Lecture 11: Somatosensation and Vestibular Sense
1/154
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
155 Terms
Somatosensation & vestibular sense
are active, and they are for action.
They are multi-sensory.
Work to provide an integrated percept of the body and its position & movements in space.
Touch:
Mechanical displacements and other physical impacts on the skin.
Proprioception
muscle sense.
Somatosensation:
A collective term for sensory signals; touch, proprioception, pain and temperature, from the body: 4 (or more) different senses!
Hold a pen. What do you feel?
=> combining info from hand and arm
=> subtracting (less interesting) sensation of the pen
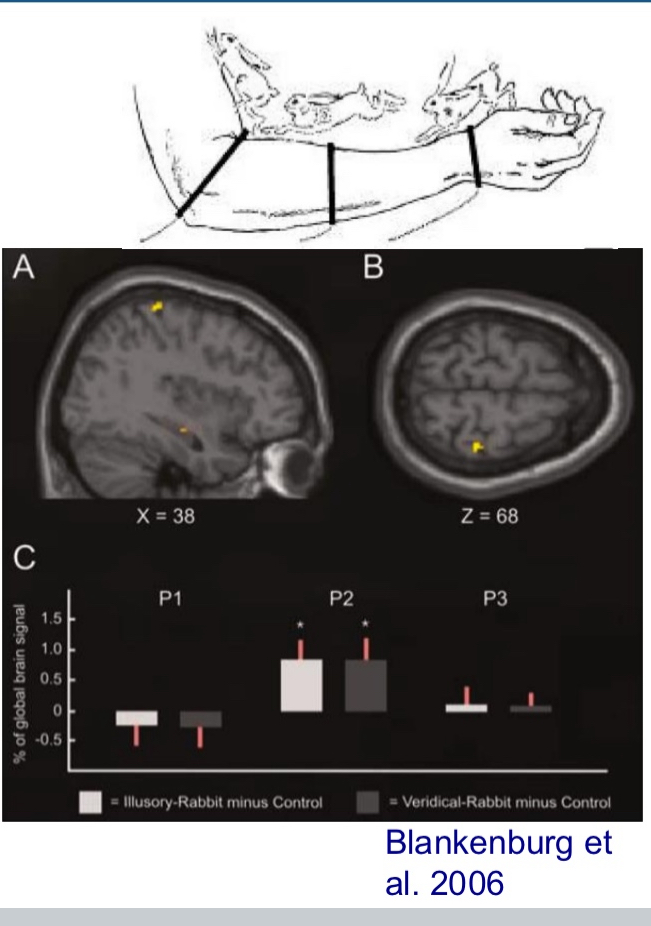
Cutaneous rabbit
2-3 separate locations stimulated multiple times in quick succession feels like a rabbit, hopping across the skin in a continuous manner.
Bayesian priors
In the rabbit illusion, the brain assumes that tactile stimuli usually move smoothly and continuously across the skin.
So when presented with fast stimuli at separate locations, it fills in the blanks to match this prior belief — hence perceiving movement where there is none.
Illusion reflected in somatosensory cortex that activates even though it shouldn’t (top down affect)
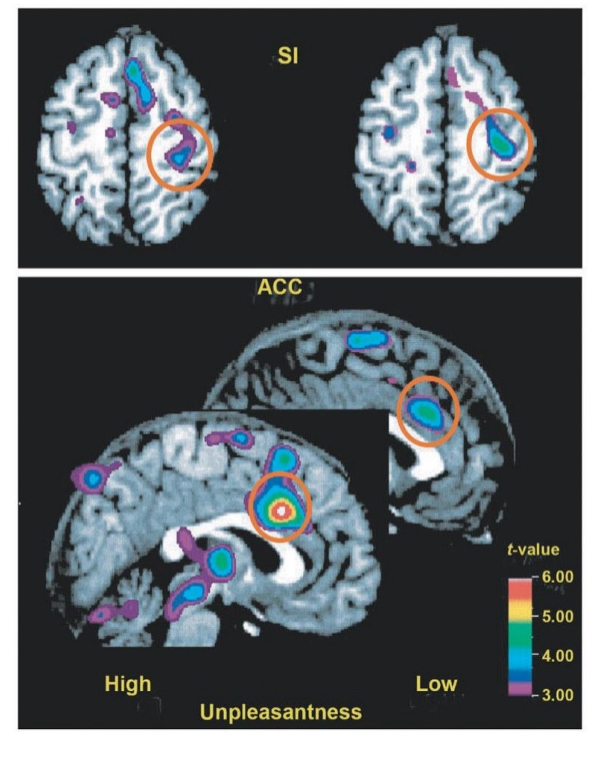
Cutaneous rabbit Investigated with fMRI
Middle location equally activated as stimulated location
This graph shows % of global brain signal in three different skin locations:
P1 = First stimulated location
P2 = Middle location (where no touch occurred)
P3 = Final stimulated location
Two conditions are shown:
Illusory-Rabbit minus Control (white bars): Real taps only on P1 and P3 (wrist and elbow), but illusion of tapping at P2
Veridical-Rabbit minus Control (gray bars): Real taps at all three locations (P1, P2, P3)
Key result:
The P2 activation in the illusory condition (white bar) is just as strong as in the real stimulation condition (gray bar).
This means the brain "believes" it was touched at P2 — even though no physical stimulus occurred there.
Somatosensory receptors have three attributes:
Type of stimulation the receptor responds to
Mechanical displacement for touch perception
Temperature
Size of the receptive field
Big or small
Rate of adaptation
Measured in Hz
Slow adaptation rate (low numbers) and high adaptation rate (high numbers)
Touch receptors:
Embedded in outer layer (epidermis) and underlying layer (dermis)
Multiple types of touch receptors
Mechanoreceptors
Meissner corpuscles
Merkel cell neurite complexes
Ruffini endings
Pacinian corpuscles
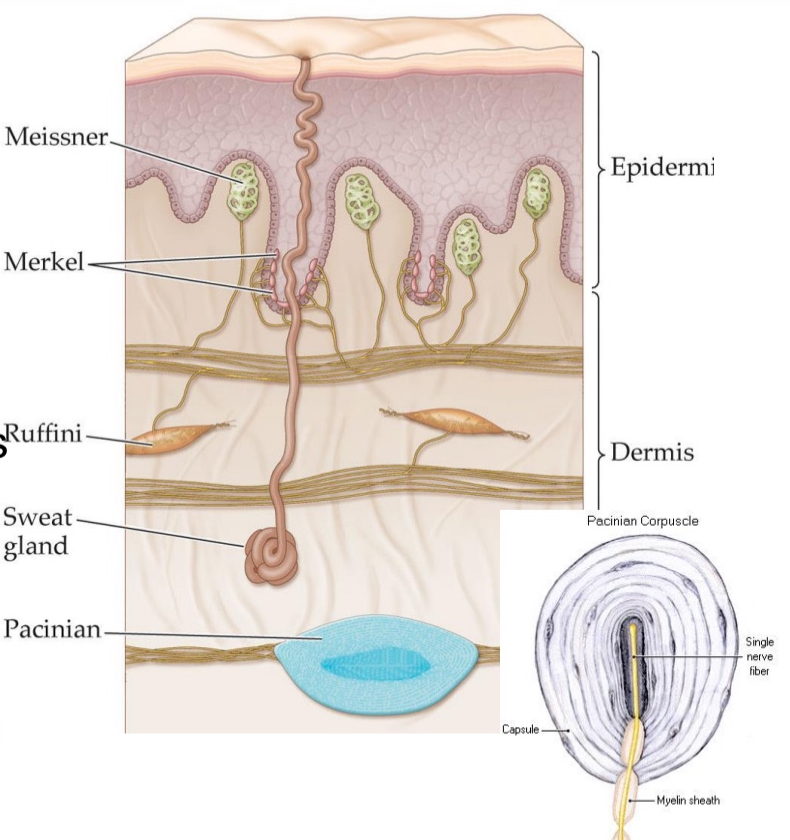
Mechanoreceptors
respond to mechanical stimulation or pressure
Messier corpuscles
Sit on top of the dermis close to surface
Merkel cell neurite complexes
Sit on top of the dermis close to surface
Ruffini endings
Deeper in dermis
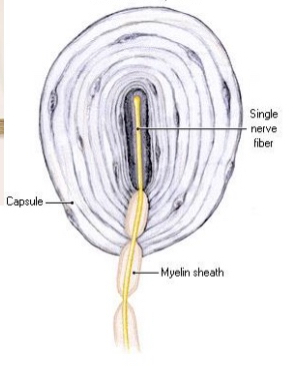
Pacinian corpuscles
Deeper in dermis
Orange part is a nerve ending but embedded in what looks like multiple areas of a onion
Mechanical impact → nerve endings will be bent and mechanical force will be absorbed by the onion structure
Very quickly adapting
Which tactile receptors are deeper in dermis
Pacinian corpuscles
Ruffini endings
Which tactile receptors Sit on top of the dermis close to surface
Merkel cell neurite complexes
Messier corpuscles
Different tactile receptor cells have different properties based on
How deep they are embedded in skin but also on morphology
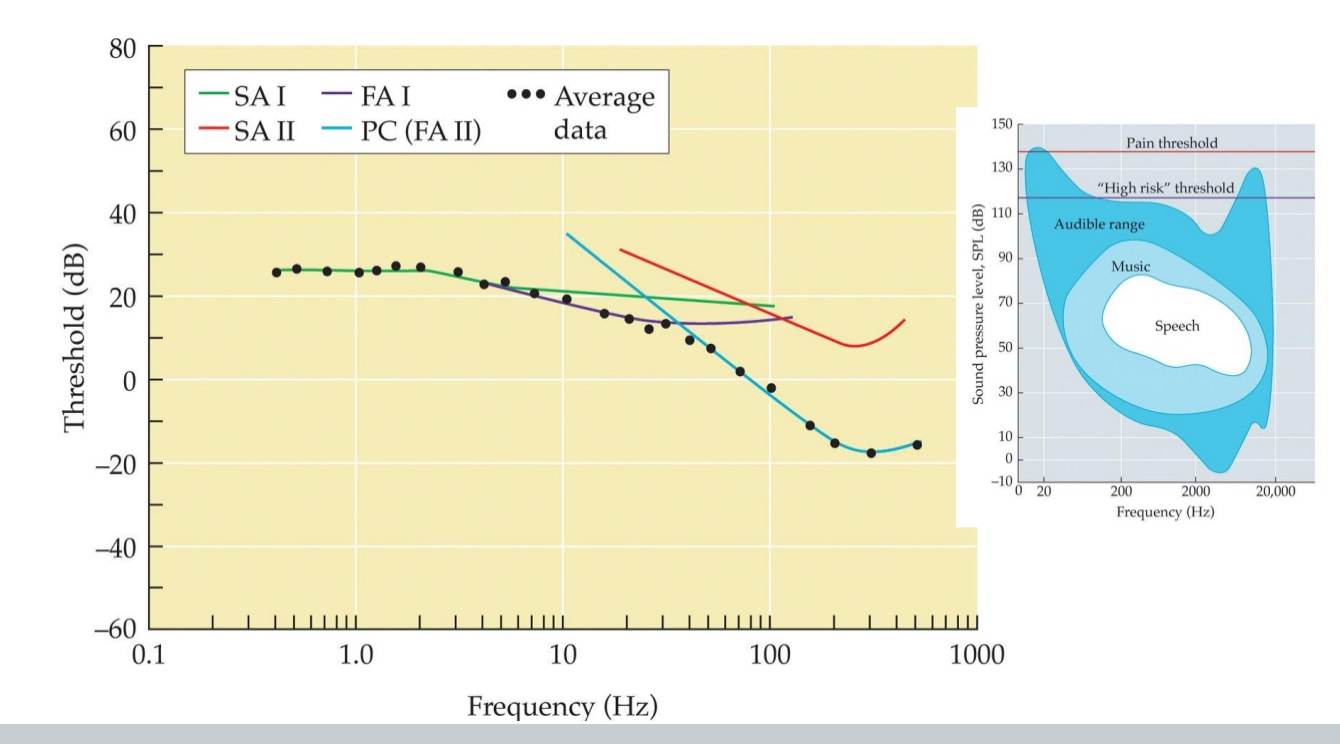
Response characteristics of 4 mechanoreceptor populations
Memorize chart
l for small recpetive field and ll for large receptive fields
FA: fast adapting and SA: slow adapting
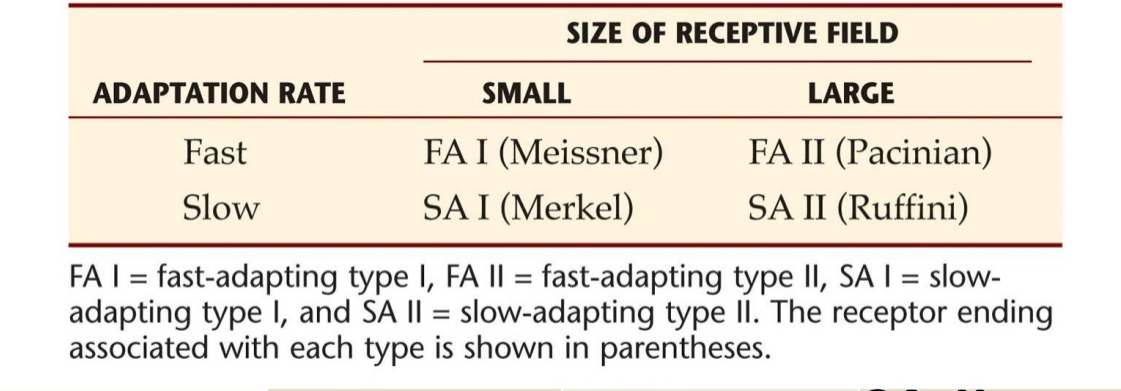
FA I:
Meissner
Good for
edge contours (tracing edges),
Braille (moving fingers over elevated surfaces
low- freq vibration (3-40 Hz)

SA I:
Merkel
Good for
local spatial discontinuities,
static texture
sustained pressure (when you hold on to something and keep touching, at some point the meissner cells stop responding but the merkel receptors continue responding)
spatial deformations (<5 Hz)
FA II:
Pacinian
mechanical transients;
high freq vibration (50-700 Hz)
SA II:
Ruffini
Good for
lateral stretch (e.g., grasping)
hand shape
static force
low sensitivity to vibration

Other types of mechanoreceptors within muscles, tendons, and joints:
Proprioceptive receptors
Spindle
Receptors in tendons
Receptors in joints
Proprioceptive receptors:
Necessary to sense
where limbs are / posture
what kinds of movements are made
Spindles:
Convey the rate at which the muscle fibers are changing in length
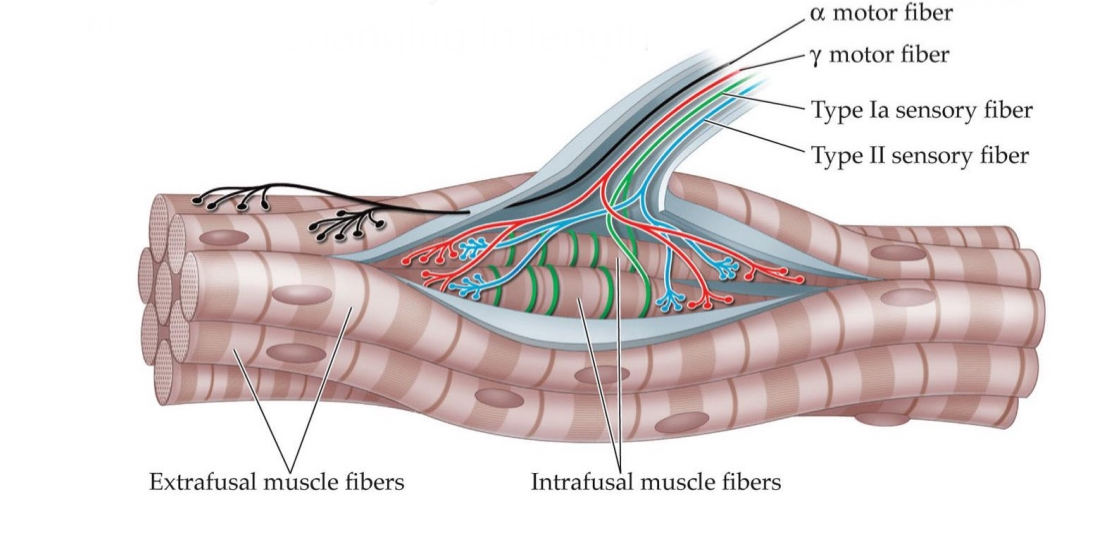
2 muscles fibers in spindles
Extrafusal muscle fibers
Intrafusal muscle fibers
4 neurons in spindle
alpha motor fibers
Delta motor fibers
Type la sensory fiber
Type ll sensory fiber
Extrafusal muscle fibers
Normal muscle fibers
When you flex muscles those are the muscle fibers being used
Intrafusal muscle fibers
Inside in the spindles, that are so thin, they can not contribute to any force
They are meant for fine tuning for Proprioceptor cells
fibers are connected to sensory neurons that detect changes in muscle length and rate of stretch.
They fine-tune proprioceptive feedback by adjusting the sensitivity of the muscle spindle, helping the nervous system precisely monitor muscle status, even during voluntary movement.
Efferent neurons in spindle
Control muscles
alpha motor fibers
Delta motor fibers
Afferent neurons in spindle
Sensory cells attached to different parts of intrafusal muscle fibers and they sense how the fibers are being stretched.
Used to estimate the length and change of length of the muscles
Type la sensory fiber
Type ll sensory fiber
alpha motor fibers
Control muscles (efferent) → contraction
Control extrafusal muscle fibers
Delta motor fibers
Control muscles (efferent) → contraction
Control intrafusal muscle fibers
Receptors in tendons
Golgi tendon organs
provide signals about tension in muscles attached to tendons
Example of Receptors in tendons
Play a role in arm wrestling. The loser usually losses very suddenly. When the loser’s hand suddenly hits the table, thats a reflex. That’s the golgi tendon organs inhibiting contraction of the muscle because their is too much tension
Receptors in joints
react when joint is bent to an extreme angle
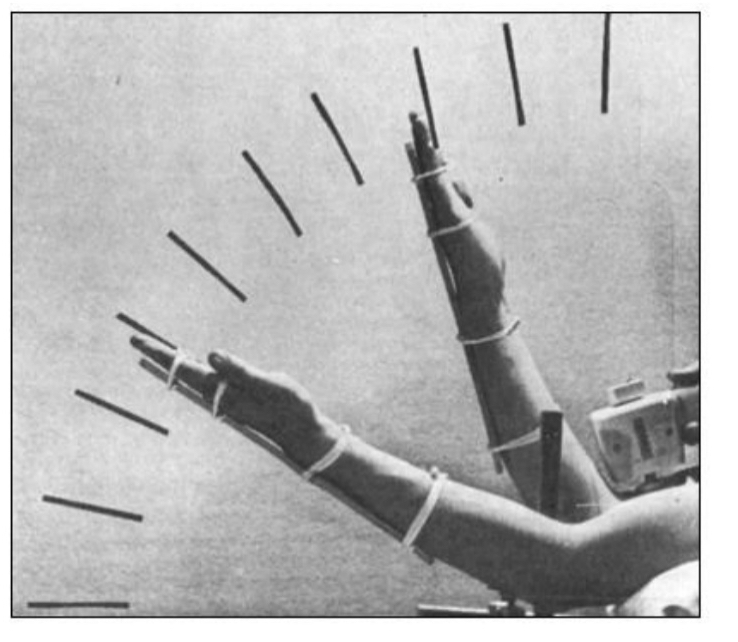
Proprioceptive illusion I
E.g., vibration of the biceps (arm perceived as being extended more than it actually is
When you vibrate the tendon of the biceps muscle, you stimulate the muscle spindles unnaturally.
This mimics the signal the brain would normally get if the muscle were being stretched (i.e., the arm is extending).
But in reality, the arm isn’t moving — the illusion is that the arm is extending or moving away from the body, even though it’s still.
The brain interprets the artificial spindle activation as real muscle lengthening, causing a false sense of movement.
Proprioceptive illusion II Somatosensory Physiology Pinocchio illusion
actually a multisensory illusion
A vibration is applied to the biceps tendon while a person is touching their nose with their finger, eyes closed.
The vibration stimulates muscle spindle receptors, just like in the first proprioceptive illusion.
This creates the illusion that the arm is extending — even though it’s not.
However, since the fingertip is still in contact with the nose, the brain tries to make sense of these conflicting signals: If the arm feels like it’s extending, but the finger is still touching the nose... then maybe the nose is growing!
The result: The person feels like their nose is getting longer — hence the name "Pinocchio Illusion."
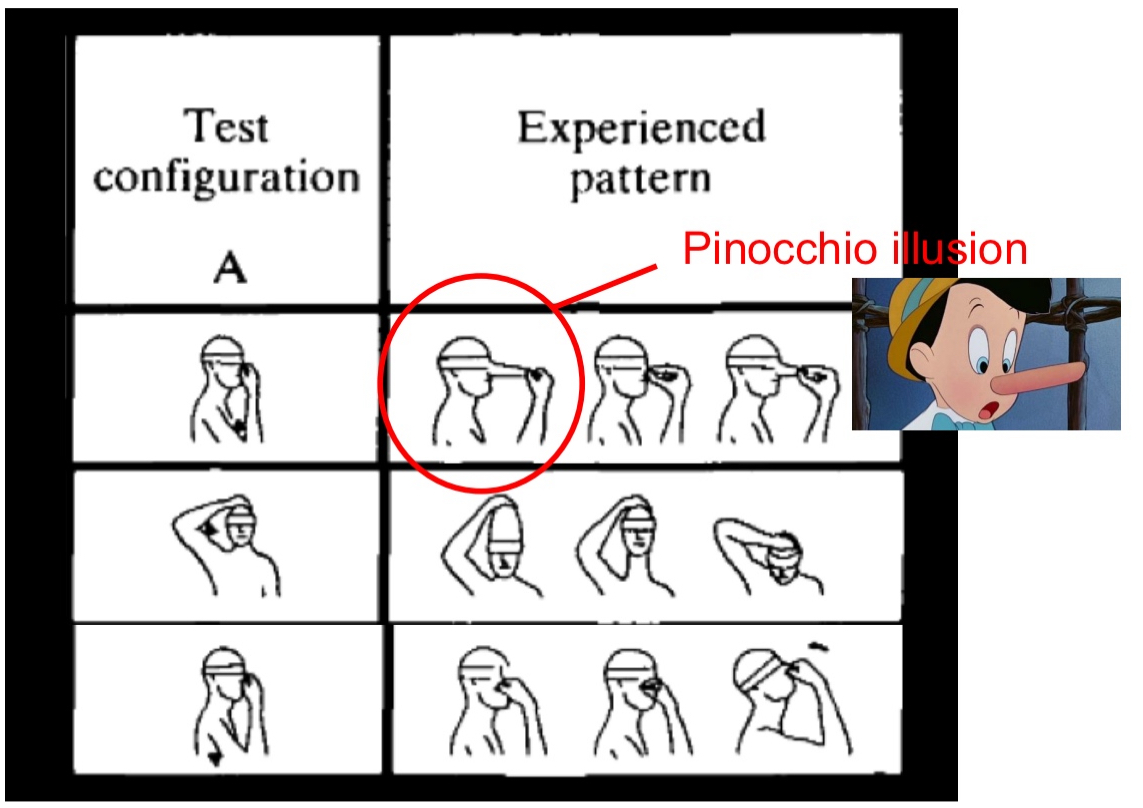
Why Is Proprioceptive illusion II Somatosensory Physiology Pinocchio illusion Important
This illusion reveals how the brain resolves sensory conflicts:
Proprioceptive input says the arm is moving,
Tactile input says the finger is stationary on the nose,
The brain blends the two, producing a bizarre but coherent body perception (a growing nose).
It’s called a multisensory illusion because it involves integration of both touch and proprioception — not just one sensory system.
Example for Pinocchio illusion without proprioceptive stimulation
This version mimics the Pinocchio illusion but doesn't involve vibrating the muscle or stimulating proprioceptors.
Setup:
The person closes their eyes.
An experimenter pulls gently on the person’s nose while simultaneously stroking their hand (e.g., finger).
The person feels the touch on their hand and the tug on the nose, but their eyes are closed — so the brain lacks visual input.
What Happens:
The brain tries to integrate the tactile sensations.
Because the touch on the hand is felt as movement, and the nose is being tugged, the brain constructs a false interpretation:
"My hand must be staying still… so my nose must be moving or growing!"
This creates a mild illusion similar to the Pinocchio effect, where the nose feels longer than it really is — but no vibration or proprioceptive muscle stimulation is involved.
Proprioceptive illusion III
Press the backs of your hands against the inside of a door frame for 30 seconds—as if you’re trying to widen the frame—and then let your arms down; you’ll feel something odd. Your arms will float up from your sides, as if lifted by an external force. Scientists call this Kohnstamm phenomenon, but you may know it as the floating arm trick. Now, researchers have studied what happens in a person’s brain and nerve cells when they repress this involuntary movement, holding their arms tightly by their sides instead of letting them float up
Proprioceptive illusion III Happens because
Proprioceptive Receptors are getting tired
Arm floats up because brain thinks there is an imbalance of how you feel your body posture
Imbalance of the sensors and brain tries to reestablish equilibrium → arm floats up
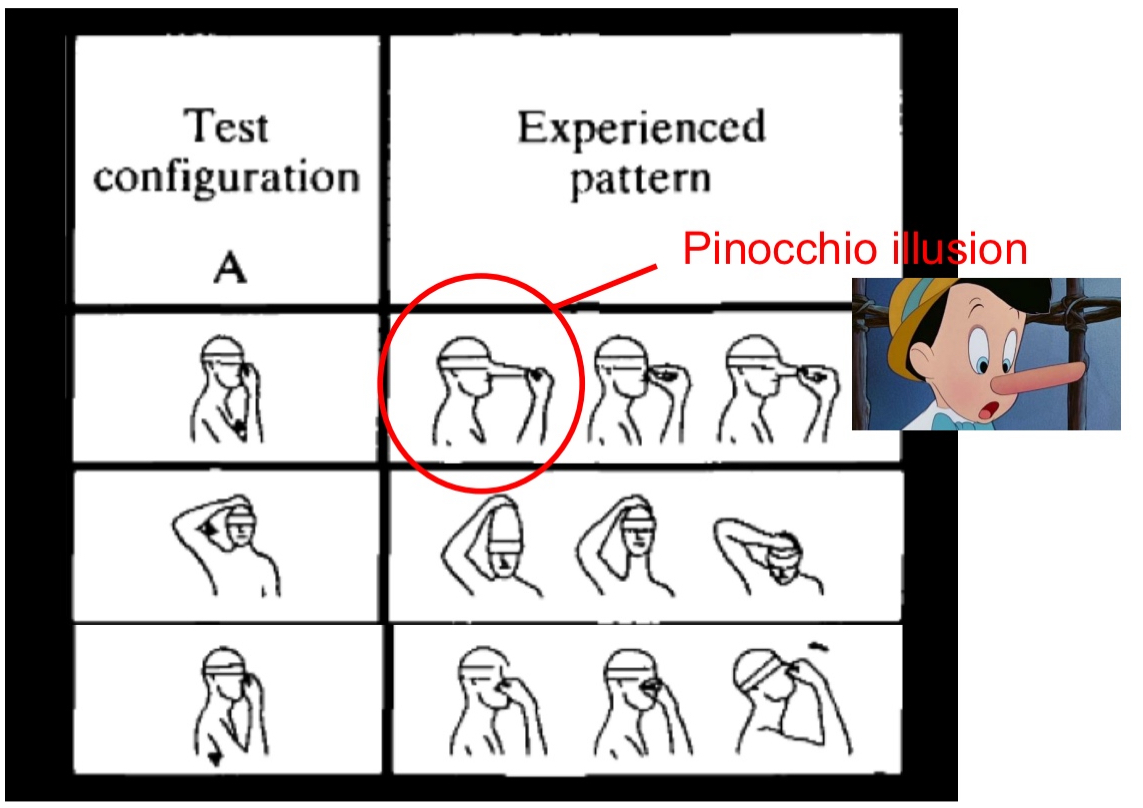
Thermoreceptors:
Sensory receptors that signal information about changes in skin temperature
Warmth fibers, cold fibers
No receptors for something in between. Gap is at body temp so about 37ºC.
We don’t need to sense that everything is ok, we need receptors to tell us if something is too cold (initiate shiver) or if something is too hot (initiate sweating)
Body is consistently regulating internal temperature
Thermoreceptors kick into gear when you make contact with object warmer or colder than your skin
Capsaicin
Capsaicin is the active compound found in chili peppers that gives them their spicy or hot sensation or pain
Capsaicin
the active compound found in chili peppers that gives them their spicy or hot sensation or pain
At what temp do cold receptors react
Peak at 25ºC
At what temp do warm receptors react
Respond to higher temps at 45ºC
Why no receptors in between warm and cold thermoreceptors
No receptors for something in between. Gap is at body temp so about 37ºC.
We don’t need to sense that everything is ok, we need receptors to tell us if something is too cold (initiate shiver) or if something is too hot (initiate sweating)
We don’t need receptors at 37ºC → everything is ok
Nociceptors:
Sensory receptors that transmit information about noxious stimulation that causes damage or potential damage to the skin
Two types of fibers
A-delta fibers
C fibers
2 phases of pain
Sharp pain
Throbbing pain
A-delta fibers:
Wider in diameter than C fibers
strong pressure, heat; myelinated ➔ fast
C fibers:
pressure, heat, cold, chemicals; unmyelinated ➔ slow
Benefit of pain perception:
Sensing dangerous objects
Congenital analgesia
Leprosy (Hansen’s disease)
Congenital analgesia
is a rare genetic condition in which a person is born unable to feel physical pain.
Usually die at early age because they can’t protect themselves
Leprosy (Hansen’s disease)
People with leprosy lose the ability to feel pain due to damage to nociceptive fibers and sensory neurons, similar to congenital analgesia in effect, though acquired rather than genetic
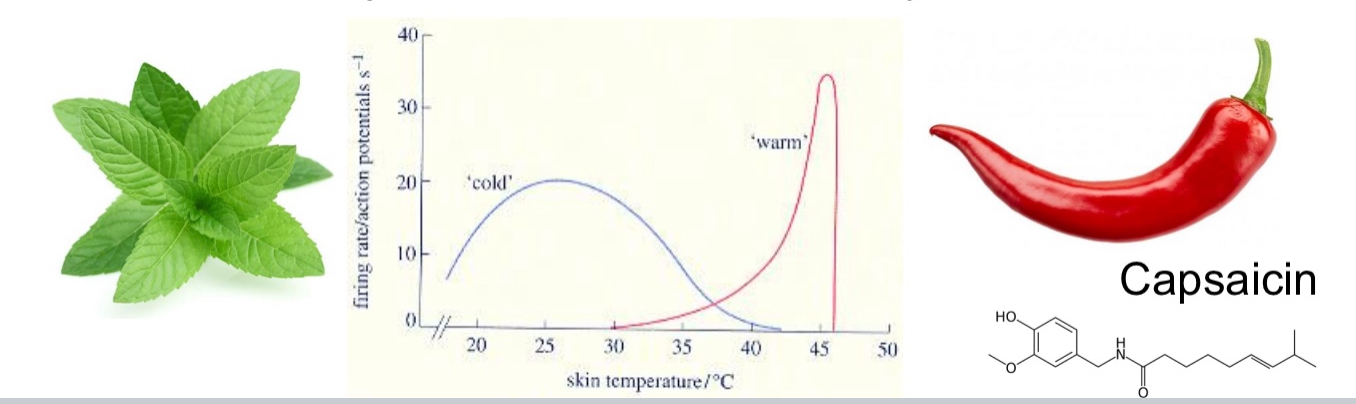
Somatosensory Pathways
Pathways: up to 2 meters long
Information must pass through spinal cord
Axons of various tactile receptors combine into single nerve trunks
Several nerve trunks from different areas of body
Once in spinal cord (via dorsal root ganglion): 2 major pathways
Spinothalamic (slower)
Dorsal column-medial lemniscal (faster)
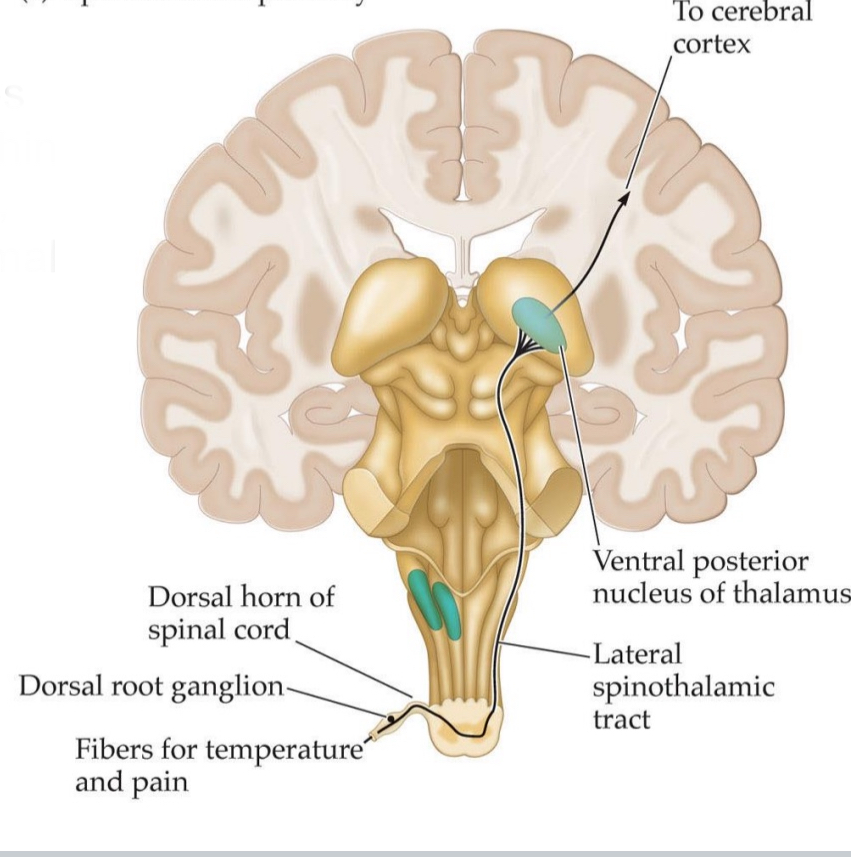
Spinothalamic pathway
synapses multiple times within spinal cord: slow, nociception, thermal information
Nociceptor in the periphery (e.g., finger)
Specialized free nerve endings (pain receptors) detect noxious stimuli (mechanical, thermal, or chemical).
Cell bodies of these sensory neurons
Located in the dorsal root ganglion (DRG), which lies just outside the spinal cord.
Central axons of DRG neurons enter the spinal cord
They synapse in the dorsal horn of the spinal cord
Second-order neurons
Cross to the contralateral side of the spinal cord and ascend via the lateral spinothalamic tract, carrying pain and temperature information up through the brainstem.
Third-order neurons
These second-order neurons synapse in the ventral posterior nucleus of the thalamus (VP nucleus)
slow pathway because of so many synapses
Why is pain slow? Shouldn’t it be fast?
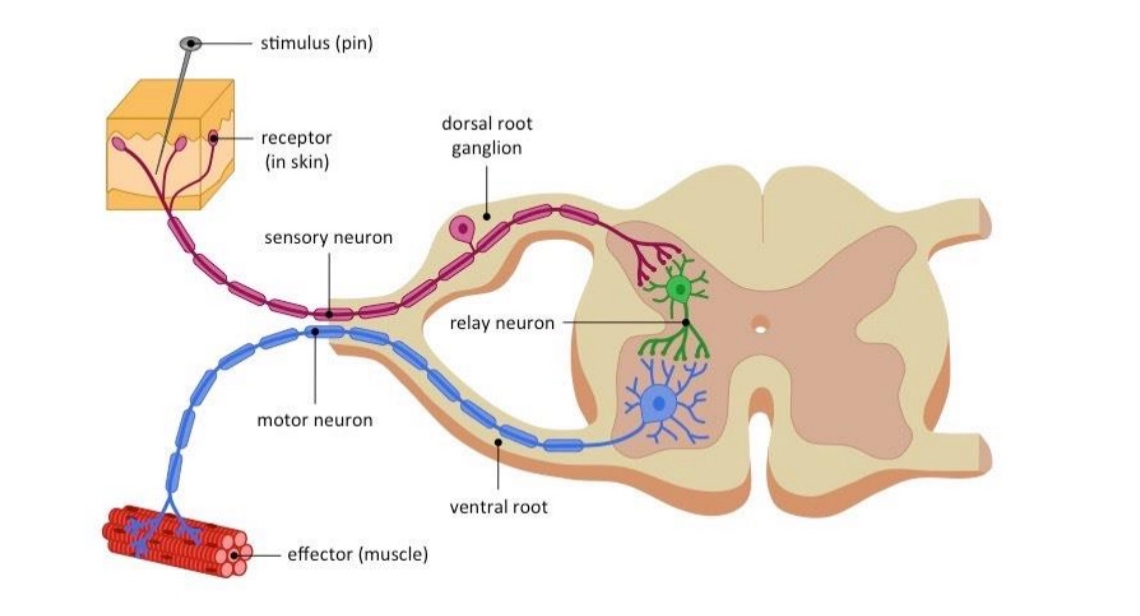
Pain reflex arc
Pain reflex arc
is an automatic, spinal reflex that helps protect the body from harm by triggering an immediate movement away from a painful stimulus—before the pain is even consciously felt.
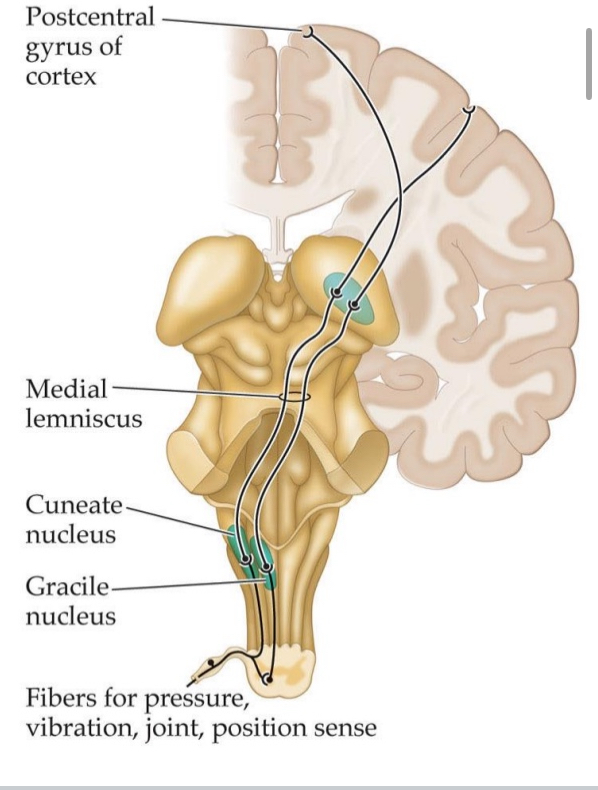
Dorsal-column-medial-lemniscal (DCML) pathway:
Fast
Synapse in medulla, near base of brain, then ventral posterior nucleus of thalamus, then somatosensory area 1 (S1), somatosensory area 2 (S2)
Fibers for pressure, vibration, joint, position sense
These are first-order sensory neurons with their cell bodies in the dorsal root ganglion (not shown).
Gracile nucleus (medulla)
Receives signals from the lower body.
First synapse of the first-order neurons.
Cuneate nucleus (medulla)
Receives signals from the upper body.
Also a first synapse site for first-order neurons.
Medial lemniscus
After synapsing in the gracile or cuneate nuclei, second-order neurons decussate (cross to the opposite side of the medulla) and ascend through the medial lemniscus.
Ventral posterior nucleus of the thalamus (not labeled directly but shown as the relay site before cortex)
Third-order neurons start here.
This is where second-order neurons from the medial lemniscus synapse.
Postcentral gyrus of cortex
The destination in the primary somatosensory cortex (S1) for conscious perception of touch, vibration, and position.
Patient with spinal cord injury might have reduced perception of touch vs. for different body sides – why?
This happens because different sensory pathways travel on opposite sides of the spinal cord.
Touch, vibration, and proprioception are carried by the dorsal column–medial lemniscal (DCML) pathway, which travels up the same side (ipsilateral) of the spinal cord as the body part sensing the stimulus. So, if the left side of the spinal cord is injured, touch and position sense will be lost on the left side of the body below the injury.
Pain and temperature are carried by the spinothalamic tract, which crosses to the opposite side (contralateral)within 1–2 spinal levels after entering. So, if the left side of the spinal cord is injured, pain and temperature sensation will be lost on the right side of the body below the injury.
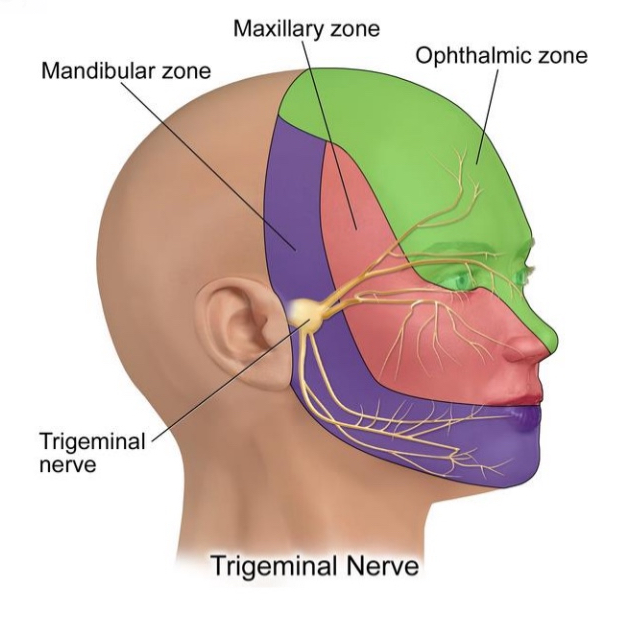
Cranial pathway:
Somatic sensation for front of the face
Trigeminal nerve (V): face, teeth etc.
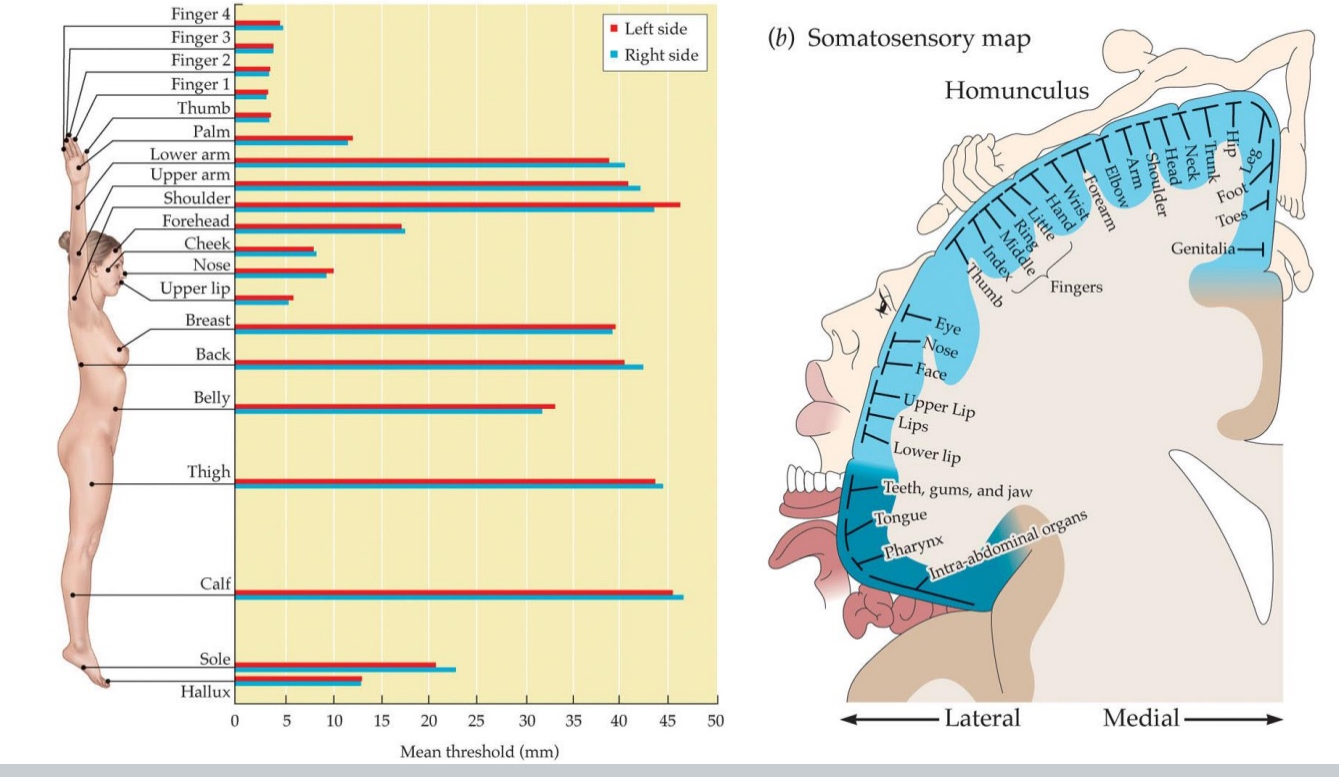
Touch sensations are represented somatotopically
Analogous to retinotopy found in vision
Adjacent areas on skin: Connected to adjacent areas in brain, called homunculus
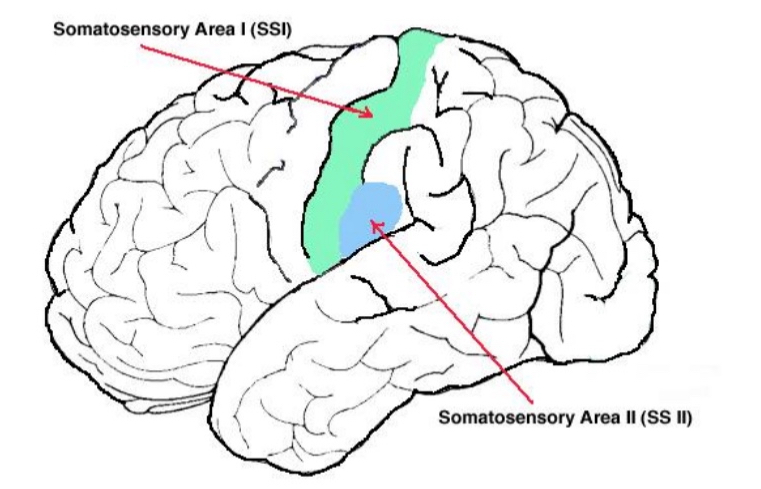
Somatosensory cortex located
in the parietal lobe of the brain, specifically behind the central sulcus.
It is primarily found on the postcentral gyrus.
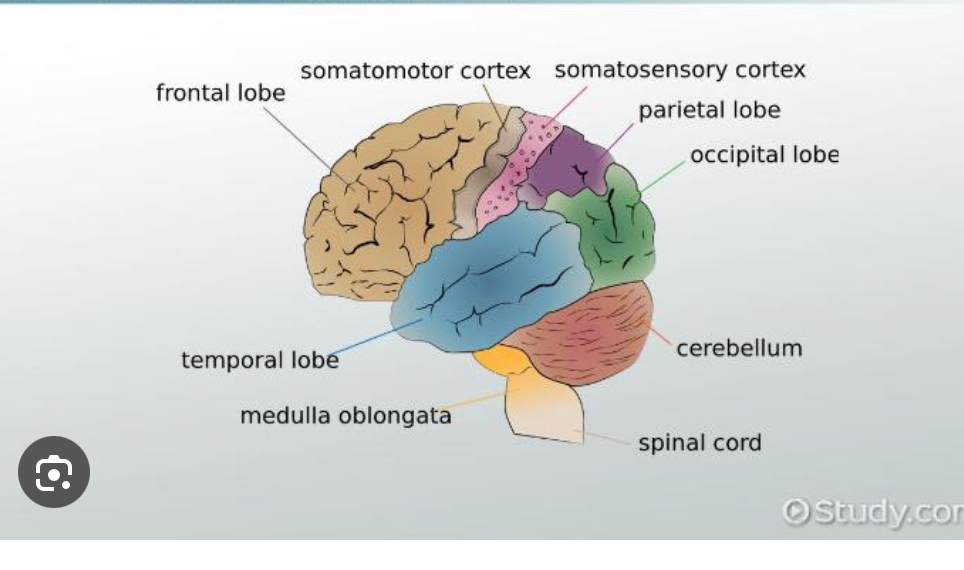
somatosensory cortex responsible for
This area is responsible for processing sensory information from the body's senses, including touch, temperature, pain, and body position
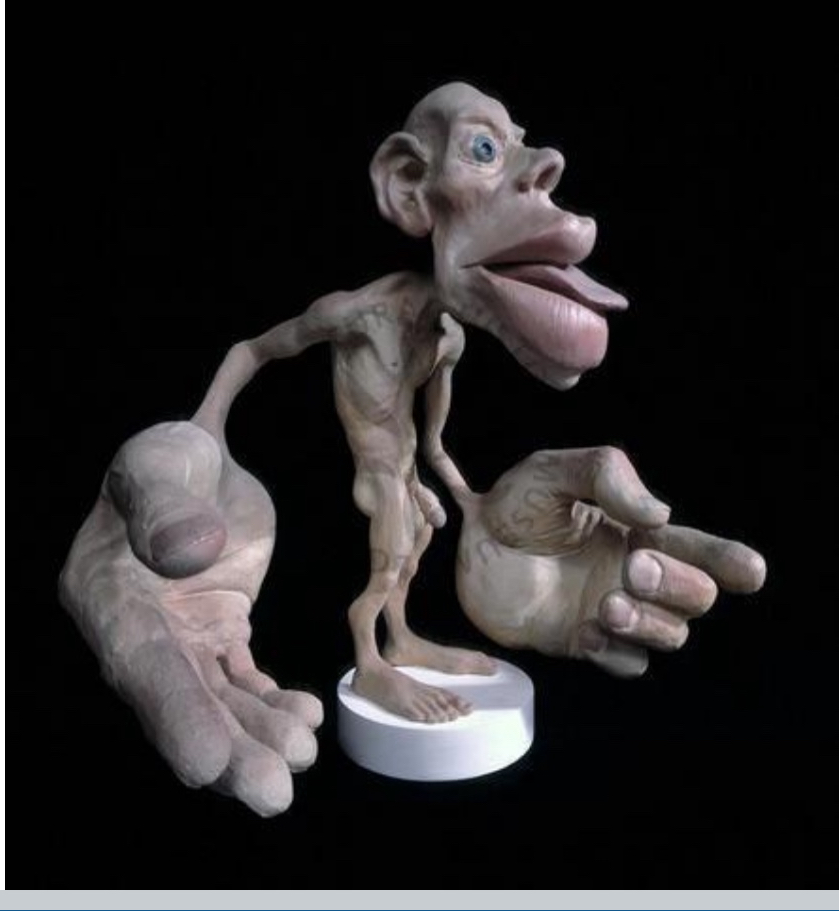
The Sensory Homunculus
Distorted representation reflects receptor density.
Brain contains several sensory maps of body, several homunculi, i.e., different subareas of S1, secondary areas as well
a visual representation of how the human body is mapped onto the primary somatosensory cortex, the part of the brain that processes touch, temperature, and pain.
It's often depicted as a distorted human figure, with larger areas representing body parts that have a greater density of sensory receptors. This means parts like the lips, hands, and feet are depicted as larger than the torso or legs, reflecting their greater sensitivity
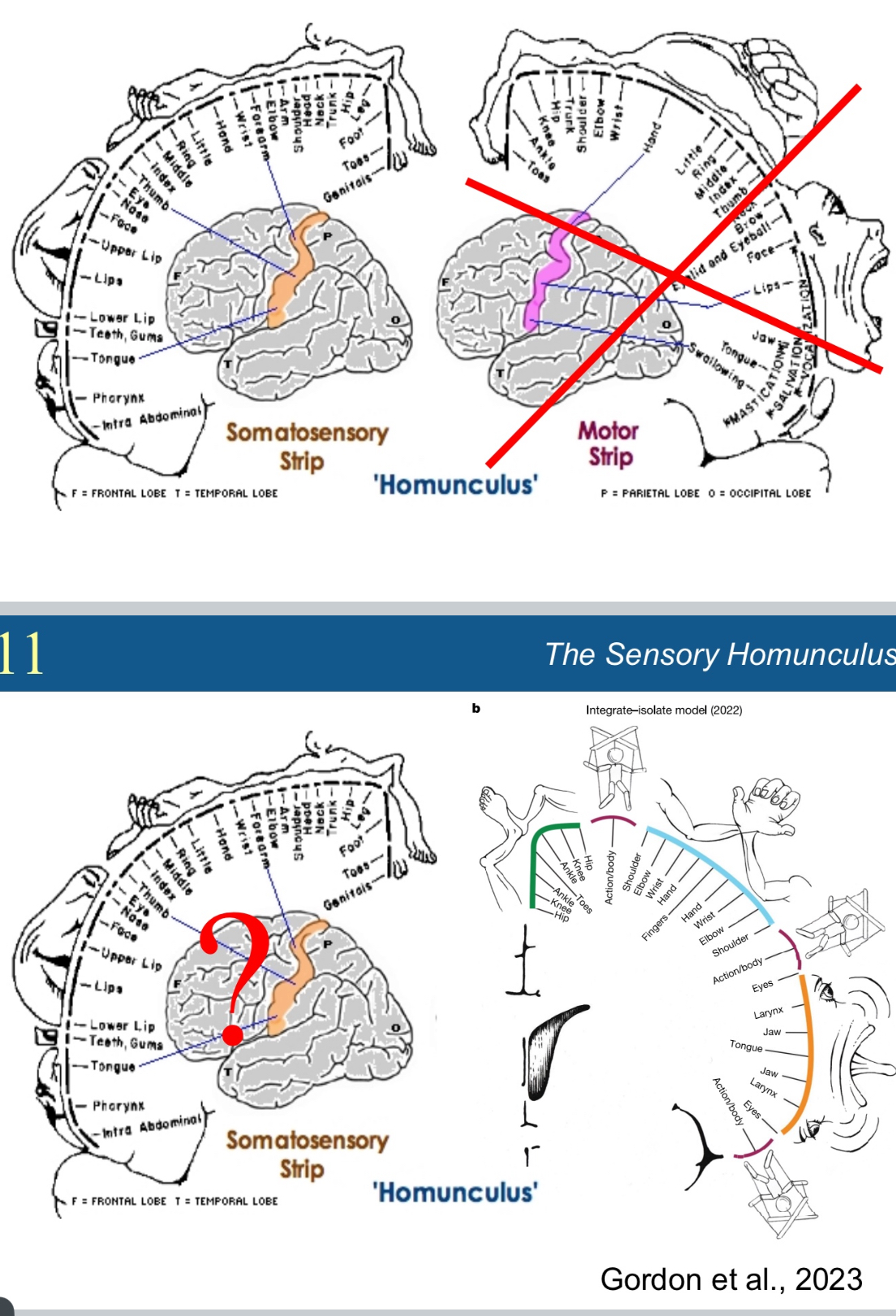
Top Half: Traditional Model
Left Brain Image: Shows the somatosensory strip (orange) in the parietal lobe, responsible for processing sensory input from the body.
The exaggerated body parts around the cortex represent how much brain area is devoted to each body region (e.g., large lips and hands = more sensitivity).
Right Brain Image (crossed out): Shows the motor homunculus (in the precentral gyrus), new research found this is wrong
Bottom Left: Question Mark Overlay
This reuses the traditional somatosensory homunculus diagram but adds a question mark, possibly asking how accurate or complete this older model is.
It implies there's uncertainty or a need to rethink the traditional sensory mapping.
Bottom Right: Gordon et al., 2023 – Updated Model
This is from a recent study (Gordon et al., 2023) proposing a revised sensory homunculus.
It still shows body parts mapped to brain regions but adds:
Action-based groupings (e.g., “Actinobody” segments for complex movements),
Updated spatial organization of somatosensory input,
Emphasis on functional integration, not just anatomical mapping.
Brain contains several sensory maps of body, different subareas of S1, secondary areas as welll
Nowadays Brodmann Area (BA) 3 considered to be S1.
BA3a: proprioception, BA3b: touch
Dense connections from BA3b to BA1 (texture) and BA2 (size, shape, proprioception)
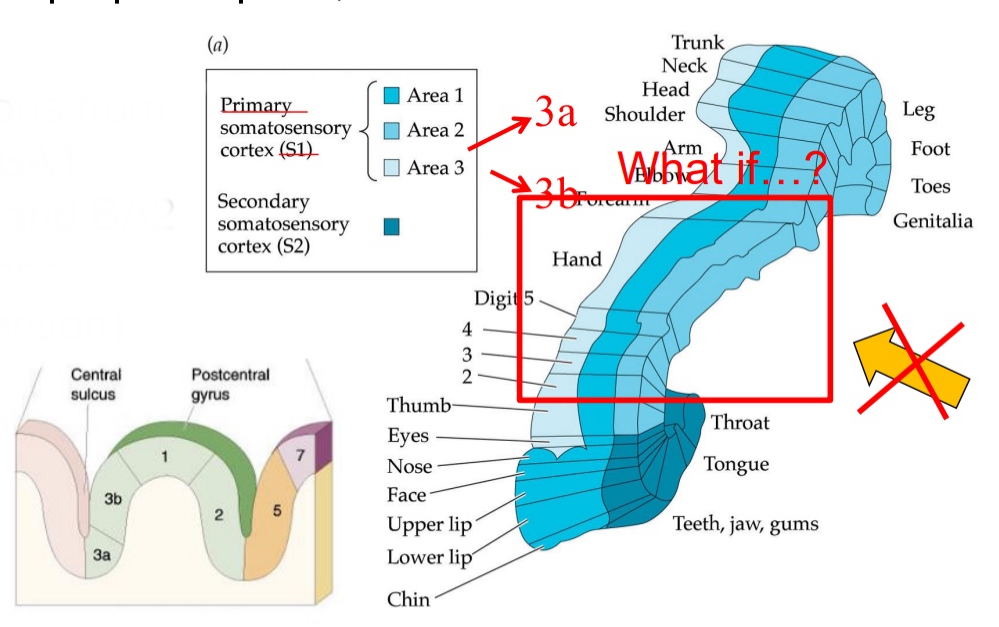
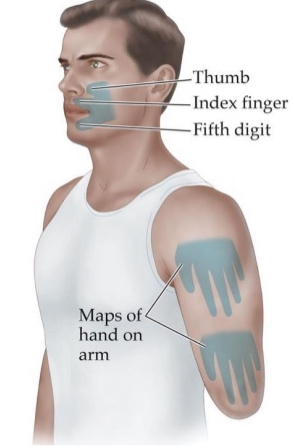
Phantom limb:
Perceived sensation from a physically amputated limb of the body
Phantom pain
If someone looses a hand, and you touch their shoulder, they’ll feel like their hand is still being touched. That suggests that those paths in S1 that used to respond to hand now respond to shoulder. But they still have the memory of being responsive to the hand
Parts of brain “listening” to missing limbs not fully “aware” of altered connections, so they attribute activity in these areas to stimulation from missing limb
Mirror “re-instates” complete body
Sometimes turn into phantom pain. If you have a cramp in foot you can stretch and get rid of it. But a person who’s foot is gone can’t do that
Mirror therapy for phantom pain
Why does mirror help phantom pain
it tricks the brain into thinking the missing limb is still there and moving normally.
A mirror is placed vertically in front of the person so that the reflection of the intact limb appears where the missing limb would be.
When the person moves their intact limb, they see the reflection and it looks like the missing limb is moving.
This visual illusion can help relieve the mismatch between what the brain expects (a working limb) and what it senses (a missing or painful one).
Pain:
Pain sensations triggered by nociceptors
Nociceptive signals arrive at the substantia gelatinosa of the dorsal horn
Responses to noxious stimuli can be moderated by cognitive, emotional and social factors
Bottom-up sensation + top-down modulation
Example: Injury during sports
Analgesia:
Decreased pain sensation while being conscious
Sports injury: endogenous opiates released in body to block transmission of pain sensations
This occurs from an evolutionary point of view because when we are physically active (running away from lion) we don’t worry about minor injury. Body cares about getting somewhere safe and ignores little pains
What do you do when you bump your head?
Rub head, apply tiny bit of pressure → touch sensation
We do this because it helps, sort of undos the pain → gate control theory
Children do this automatically, don’t need to be taught
Gate control theory:
Describes a pain transmitting system that incorporates modulating signals from the brain
Feedback circuit located in substantia gelatinosa of dorsal horn of spinal cord
Gate neurons block pain transmission
can be activated by noxious stimulation applied to another site distant from source of pain
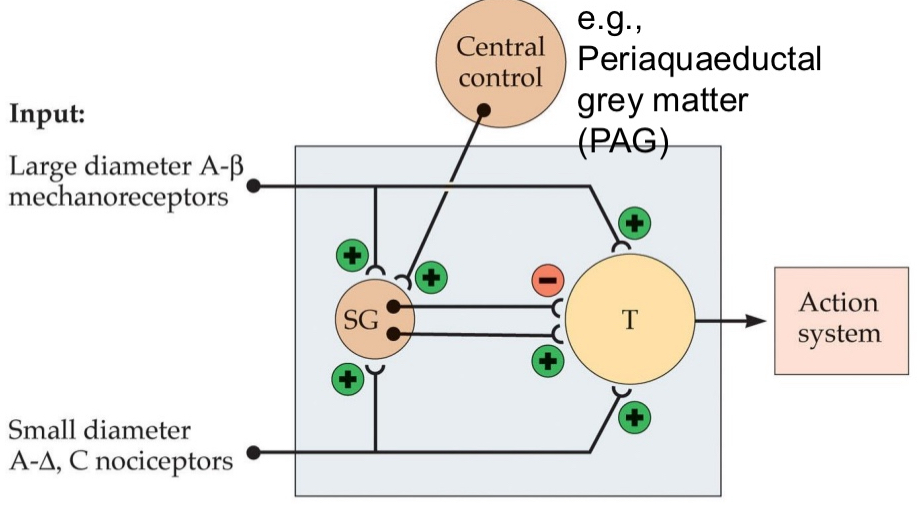
The gate in gate control theory is located in
spinal cord, specifically in the substantia gelatinosa (SG) of the dorsal horn.
How the Gate Works
Inputs:
Large-diameter A-β fibers
Carry non-painful touch or pressure information (e.g. rubbing your skin).
Excite inhibitory interneurons (green plus signs) in the SG → this closes the gate.
Small-diameter A-δ and C fibers
Carry pain signals.
Inhibit the inhibitory interneurons → this opens the gate, allowing pain signals to reach the brain.
Central Control (e.g. PAG — Periaqueductal Grey):
The brain can send signals back down to influence the gate.
Can enhance inhibition (via descending pathways) → close the gate and reduce pain.
When the Gate is Closed in Gate control theory
Less Pain
You bump your shin and start rubbing it.
Rubbing your skin activates A-β fibers — these are large-diameter fibers that carry non-painful touch sensations.
These A-β fibers activate inhibitory interneurons in the Substantia Gelatinosa (SG).
These inhibitory interneurons block the T cell (Transmission cell).
If the T cell is blocked, the pain signal cannot travel up to the brain.
As a result, you feel less pain.
This is why rubbing a painful spot makes it feel better — it’s literally “closing the gate” in your spinal cord!
When the Gate is Open in Gate control theory
More Pain
Example: You step on a nail (ouch!).
The injury activates A-δ and C fibers — these are small-diameter pain fibers.
These fibers turn off the inhibitory interneurons in the SG.
Without those interneurons, the T cell becomes active.
The T cell sends the pain signal to the brain.
You now feel sharp or burning pain — the gate is open.
The more active your pain fibers are, the wider the gate opens, and the more pain you feel.
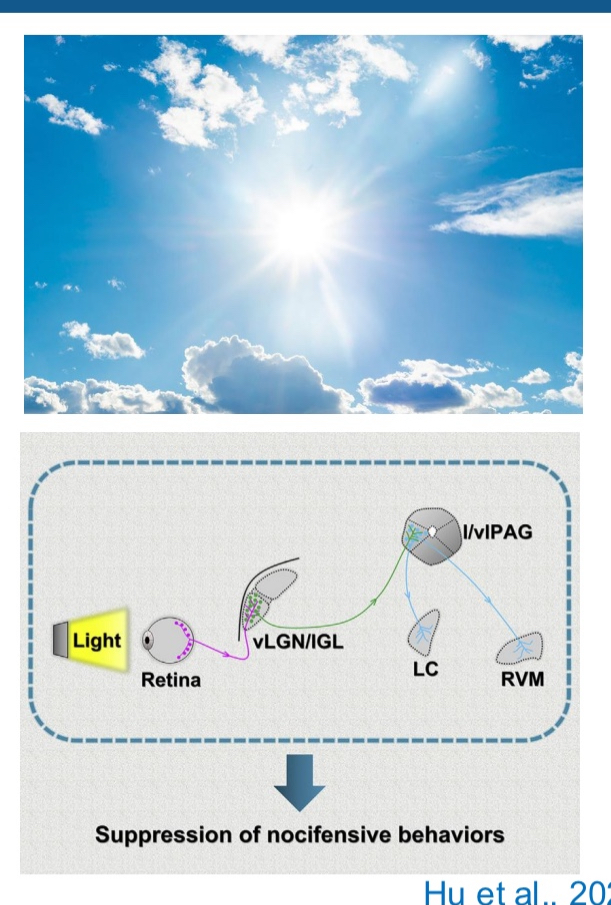
Shining light on pain Hu et al., 2022
Bright light can have antinociceptive effects
Visual pathway via portion of the LGN (ventral lateral geniculate nucleus and intergeniculate leaflet) ➔ PAG ➔ regions involved in pain regulation (locus Coeruleus, LC; rostral ventromedial medulla, RVM)
Bright light can reduce pain (antinociception):
Exposure to bright light can dampen or block pain signals — this is called an antinociceptive effect (anti = against, nociception = pain sensing).
How light reduces pain — the brain pathway:
Light is detected by your eyes, and the signal travels along your visual pathways.
Instead of going to the parts of the brain that process images, some light signals are sent to a special part of the thalamus called the ventral lateral geniculate nucleus (vLGN) and the intergeniculate leaflet (IGL).
From there, the signal is passed on to the periaqueductal gray (PAG) — an area deep in the brain that’s known for controlling pain.
The PAG then sends signals to other key pain control centers:
The locus coeruleus (LC) — involved in alertness and stress responses.
The rostral ventromedial medulla (RVM) — which can inhibit pain signals in the spinal cord.
Cognitive aspects of pain
Pain: Generally subjective experience, two components: Sensation of painful source, emotion that accompanies it
Areas S1 and S2: Responsible for sensory aspects of pain
Areas of brain that correspond to more cognitive aspects of painful experiences
experiment that used hypnosis to get people to put their hand in “different temperatures of water “
Hypnosis: Experiment with lukewarm and hot water: water was actually lukewarm, but hypnosis made them think it was hot water → painful response
Anterior cingulate cortex responded differentially to two hypnotic suggestions, by increasing or decreasing its activity
Emotional response associated with prefrontal cortex
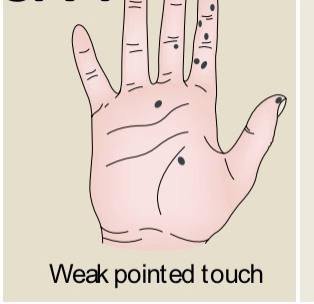
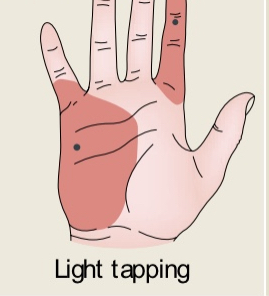
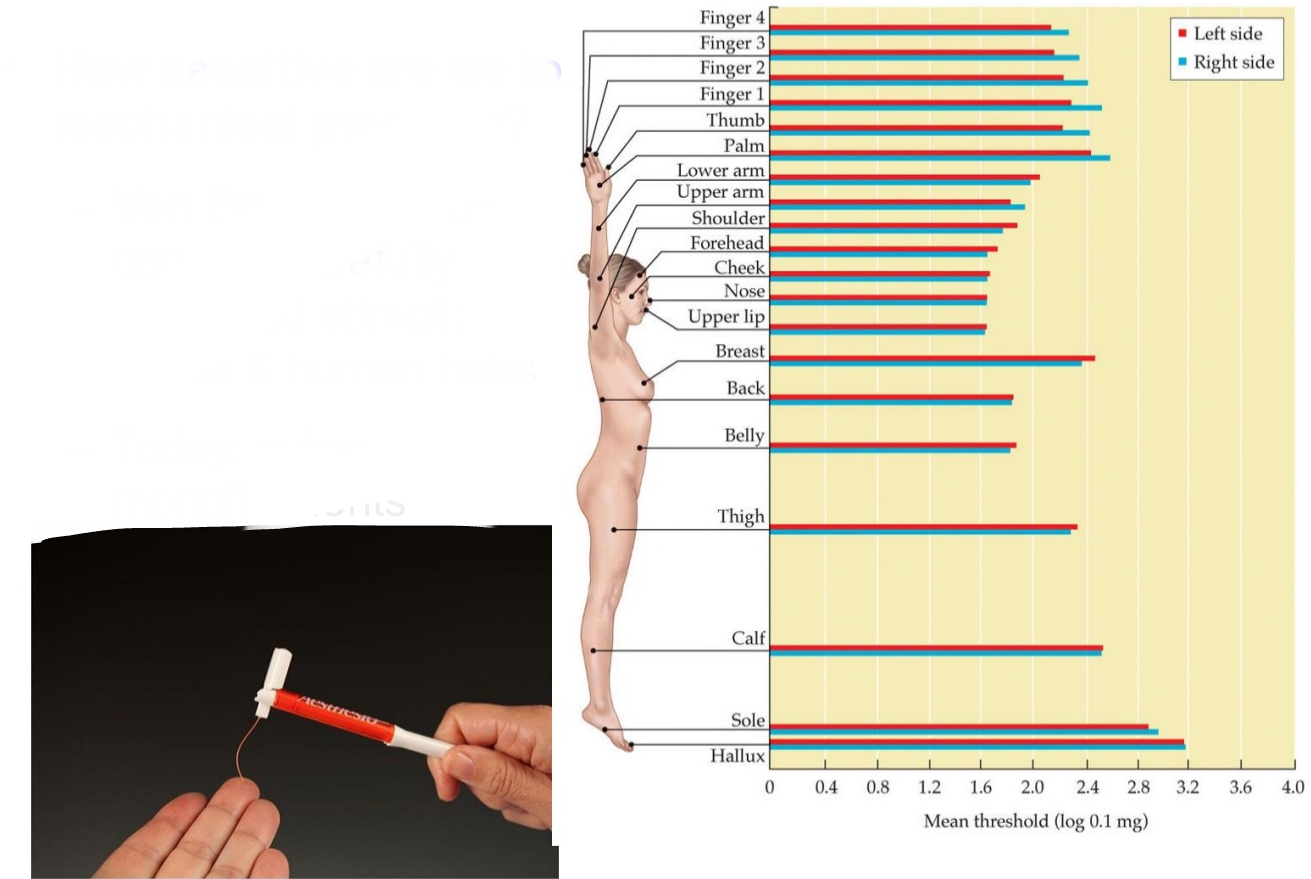
How sensitive are we to mechanical pressure?
Von Frey hair: 19th century: carefully calibrated stimuli: Horse & human hairs
Today: nylon monofilaments: no matter how much force you put on it pressure stays the same (make sure the pressure is consistent)
obviously lips have less threshold than calf
How finely can we resolve temporal details?
Look at absolute threshold not just by force applied, but also depends on frequency of vibration
Higher rates of vibration, better sensitivity, lower thresholds.
Vibration sensitivity on finger tip: Max. at ~300 Hz (~ FA II)
Only low-freq. notes can be sensed on skin (E4 ~330Hz)
How finely can we resolve spatial details?
Two point touch threshold
Two-point touch threshold:
The minimum distance at which two stimuli (e.g., two simultaneous touches) are just perceptible as separate
Ex.
If someone lightly touches your fingertip with two toothpicks that are 1 mm apart, you might feel two distinct points.
But if they do the same on your back, you might not feel them as separate unless they’re 3–5 cm apart.
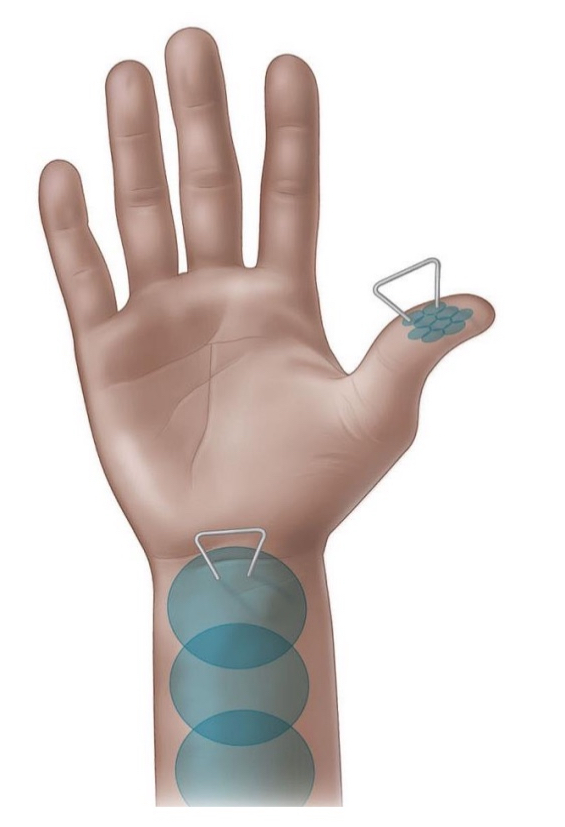
Correspondence between pattern of two-point thresholds across body & distortions of sensory homunculus
Fingers have lower thresholds than thigh
You can detect two separate touches at a much smaller distance on your fingers than on your thigh.
Two contact points will elicit different responses when
Sufficient concentration of receptors at the skin
More receptors = more detail.
Example: The lips and fingertips have a high concentration of receptors, so they can detect very fine touch differences.
Small receptive fields
Small receptive fields = more precise localization of touch.
Areas like the lips and fingers have smaller receptive fields, so even small differences in touch location are detected.
No convergence of neural processing
Convergence means multiple sensory neurons send their signals to the same neuron in the brain or spinal cord.
When this happens, the brain can’t tell exactly where the signal came from — precision is lost.
No convergence = better spatial resolution — each receptor has a direct line to the brain.
So in sensitive areas, signals stay separate and are processed individually → you feel two distinct touches.
Methodological drawbacks of 2-point threshold
Subjective: Depends on the participant's report; prone to bias or inconsistency.
Response variability: Results can vary depending on attention, fatigue, or understanding of the task.
Not purely physiological: Influenced by psychological factors, not just receptor density.
Poor spatial resolution measure: Doesn’t precisely reflect the exact size or spacing of receptive fields.
Inconsistent pressure: Manual application can lead to varying force between trials.
Low reliability: Hard to replicate results exactly across sessions or between examiners.
Haptic perception:
Knowledge of the world that is derived from sensory receptors in skin, muscles, tendons, and joints, usually involving active exploration
Exploratory procedure:
Stereotyped hand movement pattern used to contact objects in order to perceive their properties
Optimal for obtaining precise details about one or two specific properties, (e.g., to find out how rough object is: Lateral motion)
Not genetic, but not taught either, we just figure it out
Consist of
Lateral motion
Pressure
Static contact
Unsupported holding
Enclosure
Contour following
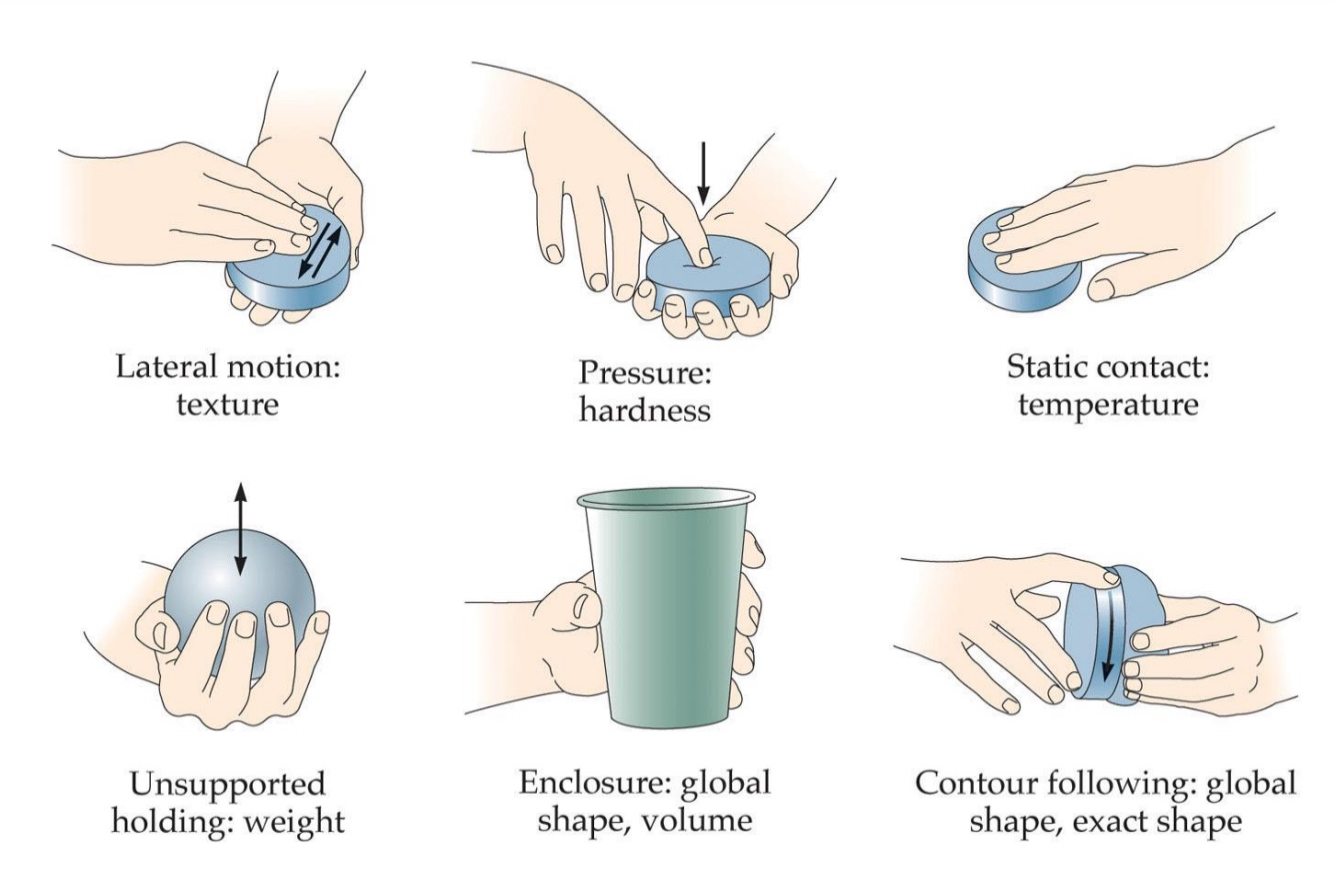
Lateral motion for
Texture
Move fingers naturally over surface

pressure for
Hardness
Poke something to test rigidness

Static contact for
Temperature
Tough surface briefly
Unsupported holding for
Weight
Carry something to see how heavy it is while moving up and down
Enclosure for
Global shape, volume
Ex. Wrap hand around cup to get a feel for its overall size
contour following
For global shape, exact shape
Trace object to get feel for it
The What system of touch:
Vision: geometric object properties
Line drawings: Easy to see; difficult to perceive haptically
Touch: perceiving material properties (cold, smooth, …)

Perception is for Action – Example: Grasping an Object
Properly lift = pull on your skin
When FA ll fire, there would be no firing if you underestimated the weight. You would start to squeeze more
Grasping involves using sensory signals to guide motor actions.
The tactile system helps detect when and how we interact with objects.
Tactile afferents (FA-I, SA-I, FA-II, SA-II) respond to different aspects of contact and movement:
FA-I and SA-I: Contact timing, friction, and pressure.
FA-II: Transient events like lift-off and contact loss; only briefly fires.
SA-II: Skin stretch; encodes grip and load forces
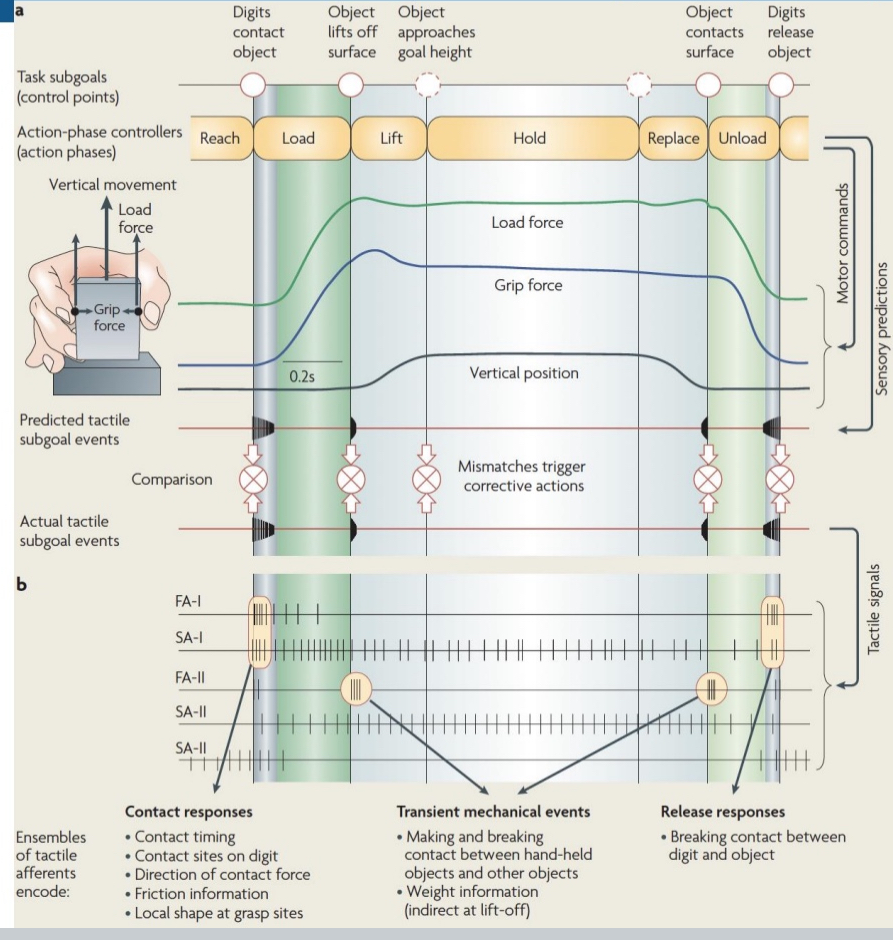
Stages of a Grasping Task (From Figure):
Reach: Hand moves toward object (no contact yet).
Load Phase:
Digits contact object (see the tactile signal spike from FA-I/SA-I).
Grip force increases to prevent slipping.
Load force begins rising (preparing to lift the object).
Lift Phase:
If the load force matches the object’s weight → lift occurs.
FA-II signals a transient spike as contact breaks with the surface.
Mismatch (object too heavy/light) triggers corrective actions.
Hold Phase:
Grip and load force plateau.
SA-II may still fire due to skin stretch.
Replace Phase:
Object approaches the target surface.
Forces begin to reduce.
Unload Phase:
Digits release the object.
FA afferents fire again during contact loss.
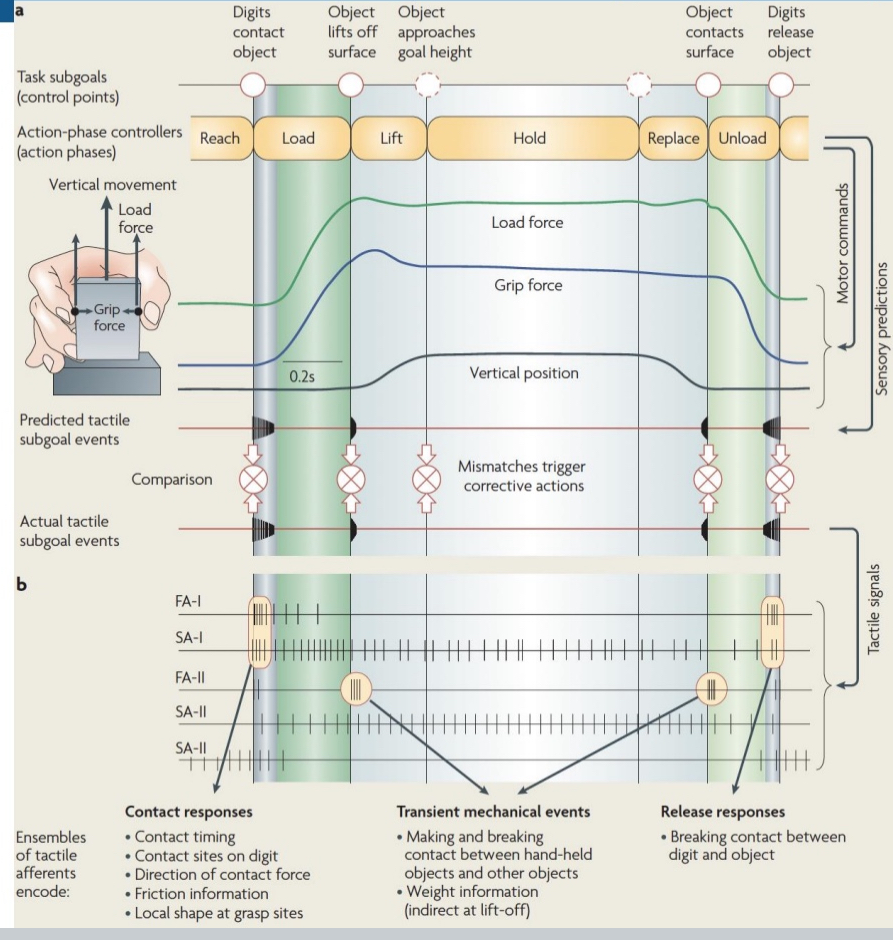
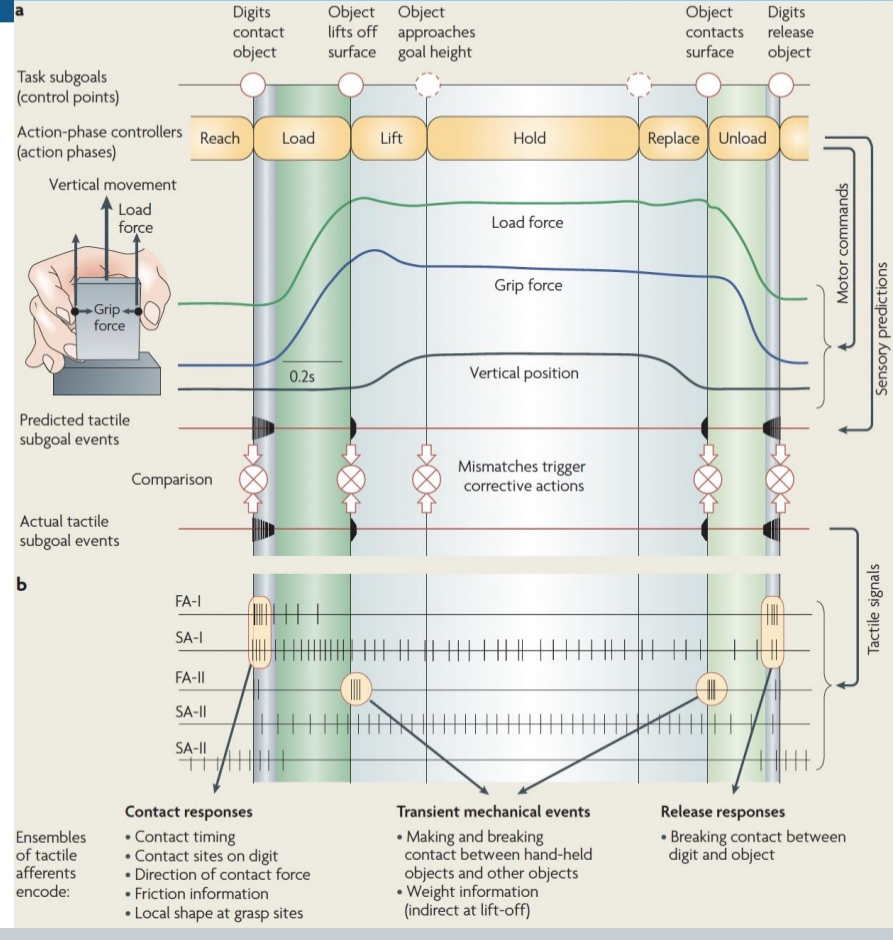
Key Concepts of graph
Grip force is modulated based on predicted weight.
If prediction is wrong (e.g., object heavier than expected), the object slips, triggering tactile feedback to correct grip.
People with anesthetized skin (no tactile input) struggle with grasping despite intact proprioception—shows how critical tactile feedback is.
Predicted tactile events are compared to actual tactile feedback.
Mismatch (e.g., slipping) activates corrections.
Tactile signals encode:
Timing and location of contact,
Direction and strength of forces,
Friction, object weight, and contact breaking.