ADHD notes
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
ADHD
attention deficit hyper activity disorder. a childhood-onset neurodevelopmental disorder that is characterized by developmentally inappropriate and impairing inattention, motor hyperactivity, and impulsivity.
inattentive ADHD system
They do not pay close attention to detail or often make careless mistakes
They have difficulty sustaining attention on tasks or activities. Also, they have trouble organizing tasks or activities. They tend to avoid, dislike, or be reluctant to do tasks that require sustained mental effort.
They do not seem to listen when spoken to.
They tend to lose things that are needed for tasks or activities, are easily distracted, and are forgetful in daily activities.
hyperactive symptoms
They fidget with or tap their hands or feet, or squirm in their seat. They run about or climb when it is not appropriate. They tend to leave their seats in situations where they should be seated. They are unable to play or do activities quietly.
They talk excessively and blurt out answers before a question has been finished. They have difficulty waiting their turn, and they tend to interrupt or intrude on others.
hyperactive or impulsivity type
6 or more hyperactive or impulsive symptoms with a few inattention symptoms.
inattentive type
6 or more inattention symptoms with few hyperactive/impulsive symptoms.
combined type
The most common type of ADHD with 6 or more symptoms from either category.
diagnosis
A clinical assessment is taken with a very detailed clinical history of the patient's life. The Data is gathered from parents, teachers, and other caregivers using a behavior rating scale and an interview. Afterwards, if the patient meets the criteria for ADHD, then a type is given to them along with how severe it is.
criticism of diagnostic criteria
circular reasoning, lack of explanatory power, and accuracy of the diagnostic criteria
circular reasoning
There is no diagnostic criterion for ADHD, like biomarkers or brain scans, only symptoms.
lack of explanatory power
There is no rationale for why the criteria and definition of ADHD are symptoms of ADHD.
accuracy of the diagnostic criteria
The diagnostic criteria are somewhat vague and subjective.
prevalence of ADHD
70-80% heritability and 20-30% environmental
genetic risk factors
Risk is 5-10 fold higher in 1st degree relatives of children with ADHD compared to the general population. Twin studies have heritability estimates of 70-80%. There are single-nucleotide polymorphisms and copy number variants that are associated with an increased risk of ADHD.
prenatal and perinatal factors
Exposure to drugs and other stressors has been correlated with increased risk for ADHD. Low birthweight and prematurity are also a risk.
eniverionmenal toxins
environmental toxins
Exposure to chemicals such as lead, Zinc, organophosphate pesticides, and polychlorinated biphenyls during pregnancy or at a young age has been identified as a possible cause and risk factor
dietary factors
Certain dietary deficiencies, such as a deficiency in zinc, magnesium, and polyunsaturated fatty acids, have been associated with increased risk for ADHD. However, this data supports correlation, not causation.
psychological factors
Low income, family adversity, or harsh/hostile parenting have been correlated with increased risk for ADHD. This does not support causation.
underlying causes
A common finding is thinning of cortical brain regions, especially in the Prefrontal Cortex, which is involved in planning complex cognitive behavior.
default mode network
Communication between the medial prefrontal cortex, lateral temporal cortex, posterior cingulate, and lateral temporal cortex. This area of the brain is most active in passive tasks such as daydreaming. It is believed that in individuals with ADHD, this network is overactive.
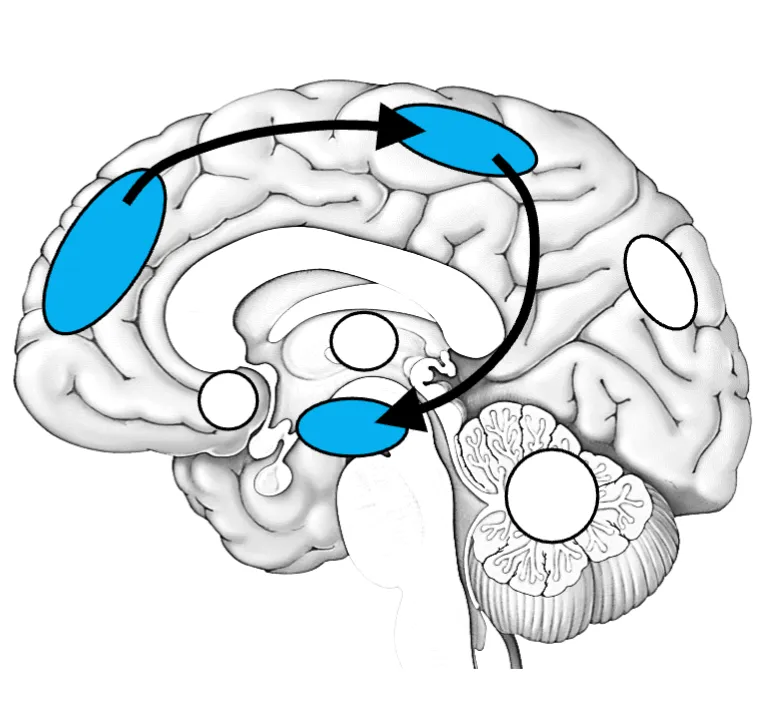
frontospatial network
Communication between the prefrontal cortex and the nucleus accumbens allows us to switch smoothly between tasks and pick out relevant information from our environment. This network may be underactive in individuals with ADHD. This could contribute to hyperactivity, impulsivity, and distractibility.
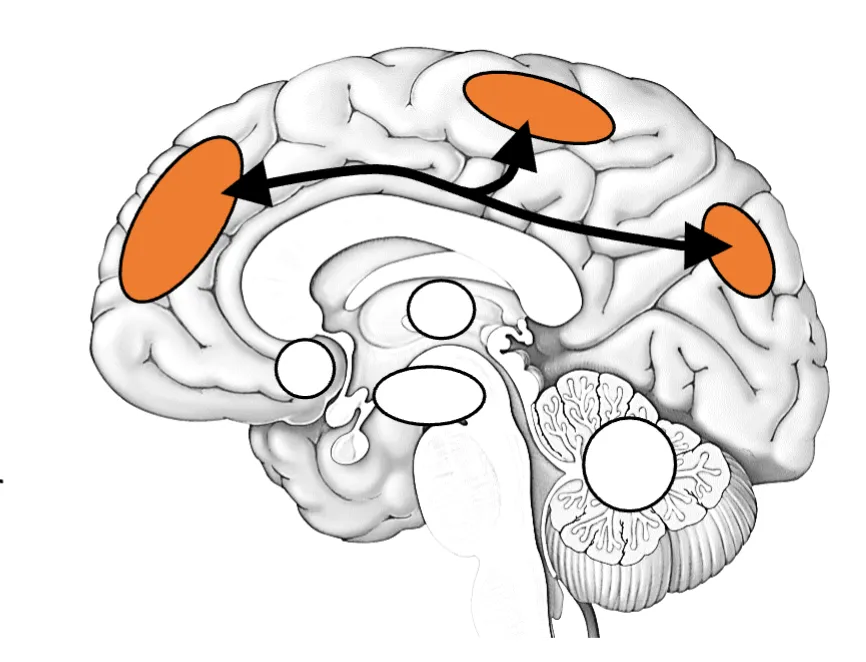
frontoparietal network
Communication between the prefrontal cortex, supplementary motor cortex, and parietal cortex. This helps sustain attention on a focused task. In individuals with ADHD, the activity is reduced, which could result in increased attention deficits.
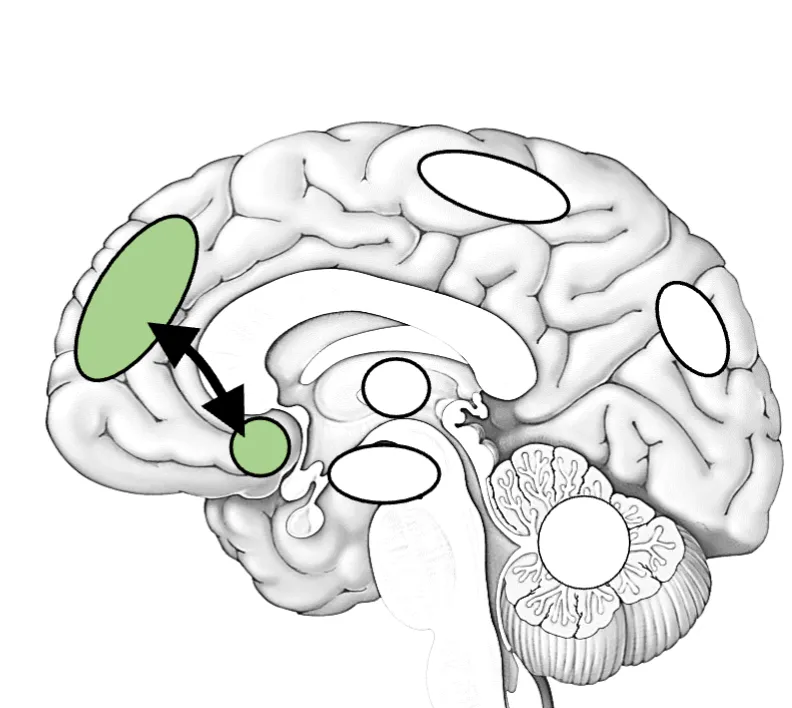
Executive function network
Communication between the Prefrontal Cortex, supplementary motor cortex, and the basal ganglia. This helps to execute focused tasks, including planning, organization, and working memory. In individuals with ADHD, this network may have a decrease in activity.
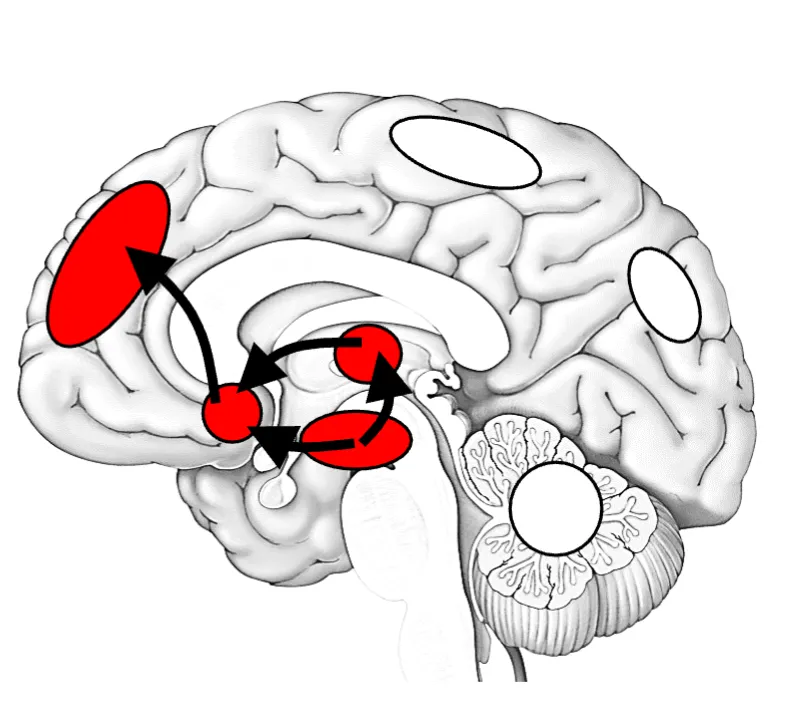
Reward network
This is where the connections between the thalamus, basal ganglia, and nucleus accumbens send information to the prefrontal cortex to make decisions about stimuli that deserve our attention. With individuals with ADHD, this network may be understimulated and have a delay in development. Hyperactivity, impulsivity, and inattention are related to this network.
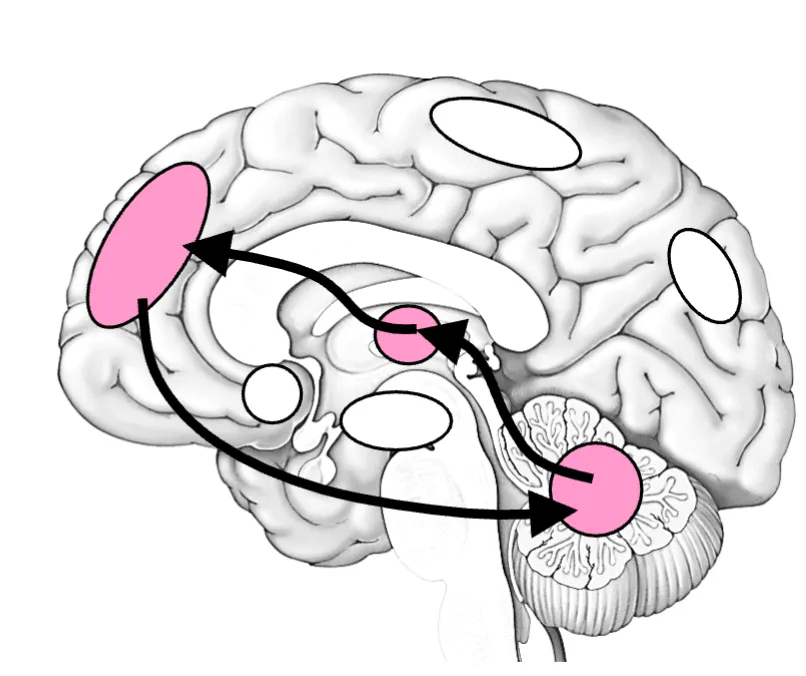
Frontocerebellar network
Communication between the prefrontal cortex, the cerebellum, and the thalamus. It is involved in moving and thinking efficiently. In individuals with ADHD, the activity of this network is reduced.
treatments
Pharmacotherapy is typically considered the first line of treatment. There are no clinical or biological predictors of response available for ADHD. Finding the optimal medication relies on educated trial-and-error. This could take several weeks.
CNS stimulants
They increase catecholamine neurotransmitters, such as dopamine, norepinephrine, and epinephrine levels by blocking dopamine and norepinephrine transporters. They are supposed to reduce patients’ need for self-stimulation. They may also help normalize structural and functional brain abnormalities
Non-stimulant medications
They are specific norepinephrine reuptake inhibitors and adrenergic receptor agonists. There is a possibility for negligible risk of abuse or misuse, and it could be particularly useful for patients at risk for substance abuse
Atomoxetine (Strattera)
norepinephrine reuptake inhibitor
Guanfacine (Tenex)
adrenergic receptor agonist
Clonidine (Kapvay)
adrenergic receptor agonist
non pharmacological interventions
Behavioral interventions that include optimized classroom management strategies, parental psychoeducation, and behavioral management techniques.