CNA Chapter 7: Basic Nursing Skills
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
94 Terms
what might residents moving into a long-term care facility may be experiencing?
fear
uncertainty
anger
loss of health, mobility, independence, family, friends, pets, and plants
what are guidelines for admission for new resident?
•Prepare the room before the resident arrives.
•When resident arrives, note the time and resident’s condition.
•Introduce yourself, giving your position. Address the resident by his formal name.
•Do not rush the admission process. Make sure the new resident feels welcome.
•Explain daily operations in the facility. Offer a tour. Introduce resident to everyone.
•Handle personal items with care and respect. Honor resident preferences when setting up the room.
•Observe the resident for anything that is missed during admission.
•Let residents adapt to their new homes at their own pace. However, signs of confusion or depression should be reported to the nurse.
what are steps for admitting a resident?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door. If the family is present, ask them to step outside until the admission process is over. Show them where they can wait. Let them know approximately how long the process will take.
5.If part of facility procedure, do these things:
•Measure the resident’s height and weight.
•Measure the resident’s baseline vital signs. Baseline signs are initial values that can then be compared to future measurements.
•Obtain a urine specimen if required.
•Complete the paperwork. Take an inventory of all the personal items.
•Help the resident put personal items away. Label personal items according to facility policy.
•Provide fresh water.
6.Show the resident the room and bathroom. Explain how to work the bed controls and the call light. Show the resident the telephone, lights, and television controls.
7.Introduce the resident to his roommate if there is one. Introduce other residents and staff.
8.Make sure resident is comfortable. Bring the family back inside if they were outside.
9.Place the call light within the resident's reach.
10.Wash your hands.
11.Document the procedure using facility guidelines.
what are steps for transferring a resident?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Collect items to be moved onto the cart. Take them to the new location. If the resident is going into the hospital, they may be placed in temporary storage.
5.Help the resident into the wheelchair (or onto a stretcher if one is used). Take him to the to proper area.
6.Introduce new residents and staff.
7.Help the resident to put personal items away.
8.Make sure that the resident is comfortable.
9.Place the call light within the resident’s reach.
10.Wash your hands.
11.Report any changes in resident to the nurse.
12.Document the procedure using facility guidelines.
what info may a nurse review with a resident who is being discharged?
•Doctor or physical therapy appointments
•Home care or skilled nursing care, if it will be provided
•Medications
•Ambulation instructions
•Medical equipment needed
•Medical transportation
•Restrictions on activities
•Special exercises
•Special dietary requirements
•Community resources
what are steps for discharging a resident?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Measure the resident’s vital signs.
6.Compare the checklist to the items there. If all items are there, ask the resident to sign.
7.Put the personal items to be taken onto the cart and take them to the pick-up area.
8.Help the resident dress and then into the wheelchair or onto the stretcher if used.
9.Help the resident to say his goodbyes to the staff and residents.
10.Take resident to the pick-up area. Help him into the vehicle. You are responsible for the resident until he is safely in the vehicle and the door is closed.
11.Wash your hands.
12.Document the procedure using facility guidelines. Include the following:
•The resident’s vital signs at discharge
•Time of discharge
•Method of transport
•Who was with the resident
•What items the resident took with her (inventory checklist)
define vital signs
measurements—temperature, pulse, respirations, and blood pressure— that monitor the functioning of the vital organs of the body.
what vital signs do NAs monitor and report?
•Temperature
•Pulse
•Respiratory rate
•Blood pressure
•Pain level
what must be reported to the nurse regarding vital signs?
•Resident has a fever.
•Respiratory or pulse rate is too rapid or too slow.
•Resident’s blood pressure changes.
•Pain is worsening or unrelieved.
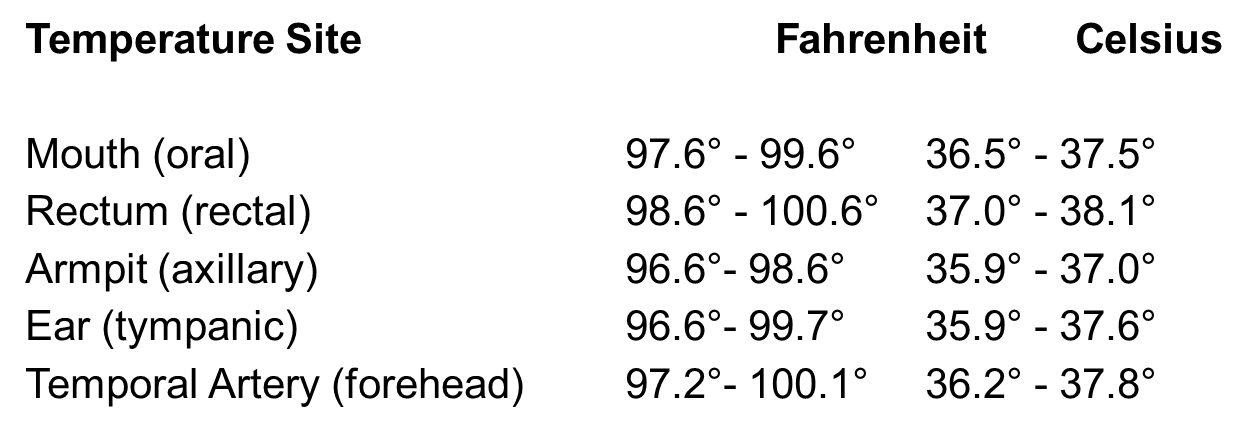
what are ranges for adult vital signs?
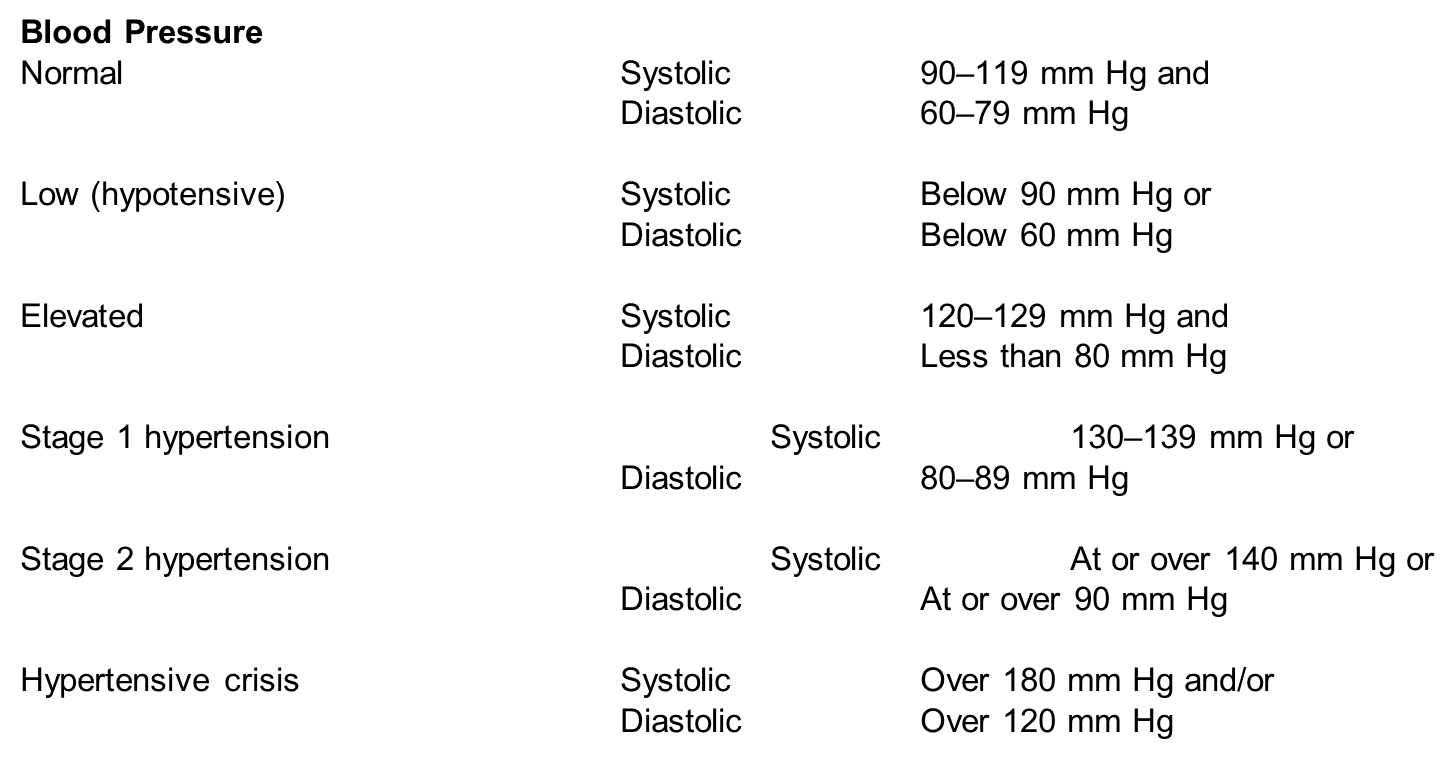
what are ranges for adult blood pressure?
Blood Pressure
Normal Systolic 90–119 mm Hg and
Diastolic 60–79 mm Hg
Low (hypotensive) Systolic Below 90 mm Hg or
Diastolic Below 60 mm Hg
Elevated Systolic 120–129 mm Hg and
Diastolic Less than 80 mm Hg
Stage 1 hypertension: Systolic 130–139 mm Hg or
Diastolic 80–89 mm Hg
Stage 2 hypertension Systolic At or over 140 mm Hg or
Diastolic At or over 90 mm Hg
Hypertensive crisis Systolic Over 180 mm Hg and/or
Diastolic Over 120 mm Hg
what facts should NAs know about body temp?
•Age, illness, stress, environment, exercise, and the circadian rhythm all affect temperature.
•There are five sites for measuring:
1.Mouth (oral temperature)
2.Rectum (rectal temperature)
3.Ear (tympanic temperature)
4.Armpit (axillary temperature)
5.•Digital thermometers are commonly used for oral, rectal, and axillary temperatures.
•Temporal artery thermometers measure heat over temporal artery with a gentle stroke or scan across the forehead.
•Tympanic thermometers are fast and accurate.
•Rectal temperatures are most accurate, but taking rectal temperature can be dangerous with some residents.
•Axillary temperatures are considered least accurate.
•Oral temperatures cannot be taken on someone who
•Is unconscious
•Has recently had facial or oral surgery
•Is younger than 5 years old
•Is confused or disoriented
• Is heavily sedated
•Is likely to have a seizure
•Is coughing
•Is using oxygen
•Has facial paralysis
•Has a nasogastric tube
•Has sores, redness, swelling, or pain in the mouth, or has an injury to the face or neck.
what are steps for measuring and recording oral temp?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on gloves.
6.Digital thermometer: Put on the disposable sheath. Turn on the thermometer and wait until the ready sign appears.
Electronic thermometer: Remove the probe from the base unit. Put on probe cover.
Mercury-free thermometer: Hold the thermometer by the stem. Before inserting it in the resident’s mouth, shake thermometer down to below the lowest number (at least below 96°F or 35°C). (cont'd)
*To shake the thermometer down, hold it at the side opposite the bulb with the thumb and two fingers. With a snapping motion of the wrist, shake the thermometer. Stand away from furniture and walls while doing so.
7.Digital thermometer: Insert the end of digital thermometer into resident’s mouth, under tongue and to one side.
Electronic thermometer: Insert the end of the thermometer into the resident’s mouth, under tongue and to one side.
Mercury-free thermometer: Put on disposable sheath if available. Insert the bulb end of the thermometer into the resident’s mouth, under tongue and to one side.
8.For all thermometers: Tell the resident to hold the thermometer in her mouth with lips closed. Assist as necessary. The resident should breathe through her nose. Ask the resident not to bite down or talk.
Digital thermometer: Hold in place until thermometer blinks or beeps.
Electronic thermometer: Hold in place until you hear a tone or see a flashing or steady light.
Mercury-free thermometer: Hold in place for at least three minutes.
9.Digital thermometer: Remove the thermometer. Read the temperature on the display screen. Remember the temperature reading.
Electronic thermometer: Read the temperature on the display screen. Remember the temperature reading. Remove the probe.
Mercury-free thermometer: Remove the thermometer. Wipe with a tissue from stem to bulb or remove sheath. Discard the tissue or sheath. Hold the thermometer at eye level. Rotate until line appears, rolling the thermometer between your thumb and forefinger. Read the temperature. Remember the temperature reading.10.Digital thermometer: Using a tissue, remove and discard the sheath. Replace the thermometer in the case.
Electronic thermometer: Press the eject button to discard the cover. Return the probe to the holder.
Mercury-free thermometer: Clean thermometer according to policy. Rinse with clean water and dry. Return it to case.
11.Remove and discard gloves.
12.Wash your hands.
13.Immediately record the temperature, date, time, and method used (oral).
14.Place the call light within the resident's reach.
15.Report any changes in resident to the nurse.
what facts should NAs know about measuring a rectal temp?
•NA must explain what he or she will do before starting.
•NA should be reassuring.
•NA must hold onto the thermometer at all times.
•NA must wear gloves.
•Thermometer must be lubricated for this procedure.
•The privacy of the resident is important.
what are steps for measuring and recording rectal temps?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Adjust bed to a safe level, usually waist high. Lock the bed wheels.
6.Help the resident to left-lying (Sims’) position.
7.Fold back the linens to expose only the rectal area.
8.Put on gloves.
9.Digital thermometer: Put on the disposable sheath. Turn on thermometer and wait until the ready sign appears.
Electronic thermometer: Remove the probe from base unit. Put on the probe cover.
Mercury-free thermometer: Hold the thermometer by stem. Shake the thermometer down to below the lowest number. Put on a disposable sheath.
10.Apply a small amount of lubricant to tip of the bulb or probe cover (or apply pre-lubricated cover).
11.Separate the buttocks. Gently insert thermometer into rectum 1/2 to 1 inch. Stop if you meet resistance. Do not force the thermometer into the rectum.
12.Replace the sheet over buttocks. Hold on to the thermometer at all times.
13.Digital thermometer: Hold thermometer in place until thermometer blinks or beeps.
Electronic thermometer: Hold in place until you hear a tone or see a flashing or steady light.
Mercury-free thermometer: Hold in place for at least 3 minutes.
14.Gently remove the thermometer. Wipe it with tissue from stem to bulb or remove the sheath. Discard the tissue or sheath.
15.Read the thermometer at eye level as you would for an oral temperature. Remember the temperature reading.
16.Digital thermometer: Clean thermometer according to policy and replace it in the case.
Electronic thermometer: Press the eject button to discard cover. Return the probe to the holder.
Mercury-free thermometer: Clean the thermometer according to policy. Rinse with clean water and dry. Return it to the case.
17.Remove and discard your gloves.
18.Wash your hands.
19.Assist the resident to a safe, comfortable position. Return the bed to its lowest position.
20.Immediately record the temperature, date, time, and method used (rectal).
21.Place the call light within the resident's reach.
22.Report any changes in resident to the nurse.
what should NAs know about tympanic and axillary temps?
•Tympanic thermometers are fast and accurate.
•The tympanic thermometer will only go into the ear ¼ - ½ inch.
•Axillary temperatures are much less reliable but can be safer for confused, disoriented, or uncooperative residents, or residents with dementia.
what are steps for measuring and recording tympanic temp?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on gloves.
6.Put a disposable sheath over the earpiece of the thermometer.
7.Position the resident’s head so that the ear is in front of you. Straighten the ear canal by gently pulling up and back on the outside edge of the ear. Insert the covered probe into the ear canal. Press the button.
8.Hold thermometer in place until it blinks or beeps.
9.Read temperature. Remember temperature reading.
10.Discard sheath. Return thermometer to storage or to the battery charger if thermometer is rechargeable.
11.Remove and discard your gloves.
12.Wash your hands.
13.Immediately record temperature, date, time, and method used (tympanic).
14.Place the call light within the resident's reach.
15.Report any changes in resident to the nurse.
what are steps for measuring and recording axillary temp?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain the procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Adjust the bed to a safe level, usually waist high. Lock the bed wheels.
6.Put on gloves.
7.Remove resident’s arm from sleeve of gown to allow skin contact with the end of the thermometer. Wipe the axillary area with tissues before placing the thermometer.
8.Digital thermometer: Put on the disposable sheath. Turn on thermometer and wait until the ready sign appears.
Electronic thermometer: Remove the probe from the base unit. Put on the probe cover.
Mercury-free thermometer: Hold the thermometer by the stem. Shake the thermometer down to below the lowest number. Put on a disposable sheath.
9.Position thermometer (bulb end for mercury-free) in the center of the the armpit. Fold the resident’s arm over him chest.
10.Digital thermometer: Hold in place until thermometer blinks or beeps.
Electronic thermometer: Hold in place until you hear a tone or see a flashing or steady light.
Mercury-free thermometer: Hold in place, with the arm close against the side, for 8 to 10 minutes
11.Digital thermometer: Remove the thermometer. Read temperature on display screen. Remember the temperature reading.
Electronic thermometer: Read the temperature on the display screen. Remember the temperature reading. Remove the probe.
Mercury-free thermometer: Remove the thermometer. Wipe it with a tissue from the stem to the bulb or remove the sheath. Discard the tissue or sheath. Read the thermometer at eye level as you would for an oral temperature. Remember the temperature reading.
12.Digital thermometer: Using a tissue, remove and discard the sheath. Replace the thermometer in the case.
Electronic thermometer: Press the eject button to discard the cover. Return the probe to the holder.
Mercury-free thermometer: Clean thermometer according to policy. Rinse with clean water and dry. Return it to the case.
13.Remove and discard your gloves.
14.Wash your hands.
15.Put the resident’s arm back into the sleeve of the gown.
16.Immediately record the temperature, date, time and method used (axillary).
17.Place the call light within the resident's reach.
18.Report any changes in the resident to the nurse.
define radial pulse?
the pulse located on the inside of the wrist, where the radial artery runs just beneath the skin.
define brachial pulse?
the pulse located inside the elbow, about one to one-and-a-half inches above the elbow.
define respiration?
process of inhaling and exhaling air in and out of lungs
define inspiration
process of inhaling air into lungs
define expiration
process of exhaling air out of lungs
what should NAs know about pulse?
•Pulse is the number of heartbeats per minute.
•Pulse is commonly taken at the wrist where the radial artery runs.
•Normal rate is 60-100 beats per minute for adults.
•Normal rate is 100-120 beats per minute for small children, as high as 120-140 for newborns.
•Pulse may be affected by exercise, fear, anger, anxiety, heat, medications, and pain.
•Rapid pulse may result from fever, dehydration, or heart failure.
•Slow/weak pulse may indicate infection.
what should NAs know about respiration?
•A breath includes both inspiration and expiration.
•Normal rate for adults is 12 to 20 breaths per minute.
•Normal rate for infants is 30 to 40 breaths per minute.
•Do the counting immediately after taking the pulse.
•Do not let person know you are counting breaths.
what are steps or measuring and recording radial pulse and counting and recording respirations?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Place the tips of your index finger and middle finger on the thumb side of the resident's wrist. Locate the radial pulse.
6.Count beats for 1 full minute.
7.Keep your fingertips on the resident’s wrist. Count respirations for 1 full minute. Observe for the pattern and character of the resident’s breathing. Normal breathing is smooth and quiet. If you see signs of troubled, shallow, or noisy breathing, such as wheezing, report it.
8.Wash your hands.
9.Immediately record pulse rate, date, time, and method used (radial). Record the respiratory rate and the pattern or character of breathing.
10.Place the call light within the resident's reach.
11.Report to the nurse if the pulse is less than 60 beats per minute, over 100 beats per minute, if the rhythm is irregular, or if breathing is irregular.
define systolic
first measurement of blood pressure; phase when the heart is at work, contracting and pushing blood out of the left ventricle of the heart.
define diastolic
second measurement of blood pressure; phase when heart relaxes or rests
what should NAs know about blood pressure?
•The two parts of the BP are systolic (top number) and diastolic (bottom number).
•Normal range for systolic is below 120 mm Hg.
•Normal range for diastolic is below 80 mm Hg.
•Brachial artery at the elbow is used.
•Equipment used is stethoscope and sphygmomanometer.
•A digital sphygmomanometer may be available. If so, you will be trained in its use.
•A correctly-sized cuff must be used. The cuff must first be completely deflated.
•Never measure blood pressure on an arm that has an IV, a dialysis shunt, or any medical equipment. Avoid a side with a cast, recent trauma, paralysis from a stroke, burns or mastectomy.
what are steps for measuring and recording blood pressure manually?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Before using stethoscope, wipe the diaphragm and earpieces with alcohol wipes.
6.Ask the resident to roll up his sleeve so that the upper arm is exposed. Do not measure blood pressure over clothing.
7.Position the resident’s arm with his palm up. The arm should be level with the heart. The legs should not be crossed.
8.With the valve open, squeeze the cuff. Make sure it is completely deflated.
9.Place the blood pressure cuff snugly on the resident’s upper arm. The center of the cuff with sensor/arrow is placed over the brachial artery (1-1½ inches above the elbow, toward inside of the elbow).
10.Ask the resident to remain still and quiet during the measurement.
11.Locate the brachial pulse with your fingertips
12.Place the earpieces of the stethoscope in your ears.
13.Place the diaphragm of the stethoscope over the brachial artery.
14.Close the valve (clockwise) until it stops. Do not overtighten it.15.Inflate cuff to between 160 mmHg to 180 mm Hg. If a beat is heard immediately upon cuff deflation, completely deflate cuff. Re-inflate cuff to no more than 200 mm Hg.
16.Open the valve slightly with the thumb and index finger. Deflate the cuff slowly.
17.Watch the gauge. Listen for the sound of the pulse.
18.Remember the reading at which the first pulse sound is heard. This is the systolic pressure.
19.Continue listening for a change or muffling of pulse sound. The point of a change or the point at which the sound disappears is the diastolic pressure. Remember this reading.
20.Open the valve. Deflate the cuff completely. Remove the cuff.
21.Wash your hands.
22.Record both the systolic and diastolic pressures. Record the numbers like a fraction, with the systolic reading on top and the diastolic reading on the bottom (for example: 110/70). Note which arm was used. Use RA for right arm and LA for left arm.
23.Wipe the diaphragm and earpieces of stethoscope with alcohol wipes. Store equipment.
24.Place the call light within the resident's reach.
25.Wash your hands.
26.Report any changes in resident to the nurse.
what are steps for measuring and recoding blood pressure electronically?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain the procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident’s privacy with a curtain, screen, or door.
5.Ask the resident to roll up his sleeve so that his upper arm is exposed. Do not measure blood pressure over clothing.
6.Position the resident’s arm with his palm up. The arm should be level with the heart.
7.Make sure the cuff is completely deflated. Place the blood pressure cuff snugly on the resident’s upper arm. The center of the cuff with the sensor/arrow is placed over the brachial artery (1–1½ inches above the elbow, toward the inside of the elbow).
8.Ask the resident to remain still and quiet during the measurement.
9.Turn on the blood pressure machine and press the start button.
10.When the measurement is complete, the reading will be displayed on the screen and the machine may beep. The cuff should deflate.
11.Remove the cuff.
12.Wash your hands.
13.Immediately record both the systolic and diastolic pressures that are displayed on the screen. Note which arm was used. Use RA for right arm and LA for left arm.
14.Store equipment.
15.Place the call light within the resident’s reach.
16.Wash your hands.
17.Report any changes in the resident to the nurse.
what should NAs know about pain?
•It is as important to monitor as vital signs.
•It is uncomfortable and an individual experience.
•It is important to take complaints of pain seriously.
•NAs should observe and report carefully since care plans are based on their reports.
•NAs must ask questions to get accurate information.
•Pain is not a normal part of aging.
what are some signs of pain to observe for and report?
•Increased pulse, respirations, and blood pressure
•Sweating
•Nausea
•Vomiting
•Tightening the jaw
•Squeezing eyes shut
•Holding or guarding a body part tightly
•Frowning
•Grinding teeth
•Increased restlessness
•Agitation or tension
•Change in behavior
•Crying
•Sighing
•Groaning
•Breathing heavily
•Rocking
•Pacing
•Repetitive movements
•Difficulty moving or walking
how should NA reduce pain?
•Report complaints of pain or unrelieved pain immediately.
•Gently position the body in proper alignment. Use pillows for support. Help with changes of position if the resident wishes.
•Give back rubs.
•Ask if the resident would like to take a warm bath or shower.
•Help the resident to the bathroom or commode or offer the bedpan or urinal.
•Encourage slow, deep breathing.
•Provide a quiet and calm environment. Soft music may distract the resident.
•Be patient, caring, gentle, and responsive.
what should NA know about measuring weight and height?
•Resident will be weighed repeatedly during his or her stay, and any change in weight should be reported immediately.
•A pound is a unit of weight equal to 16 ounces. A kilogram is a unit of mass equal to 1000 grams; one kilogram equals 2.2 pounds.
•Some residents will be weighed on a wheelchair scale. The weight of the wheelchair may need to be subtracted from a resident’s weight.
•Residents may need to be weighed on a bed scale.
•There are 12 inches in one foot.
what are steps for measuring and recording weight of an ambulatory resident?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Make sure resident is wearing nonskid shoes that are fastened before walking to scale.
6.Start with scale balanced at 0 before weighing the resident.
7.Help the resident to step onto the center of the scale. Be sure she is not holding, touching, or leaning against anything.
8.Determine resident’s weight. Balance the scale by making the balance bar level. Move the small and large weight indicators until the bar balances. Read the two numbers shown (on the small and large weight indicators) when the bar is balanced. Add these two numbers together. This is the resident’s weight.
9.Help resident to safely step off scale before recording weight.
10.Wash your hands.
11.Immediately record the resident’s weight in pounds (lb) or kilograms (kg), depending on facility policy.
12.Place the call light within the resident's reach.
13.Report any changes in resident to the nurse.
what are steps for measuring and recording height of an ambulatory resident?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Make sure the resident is wearing nonskid shoes before walking to scale.
6.Help resident to step onto scale, facing away from the scale.
7.Ask resident to stand straight if possible. Help as needed.
Pull up the measuring rod from the back of the scale. Gently lower the rod until it rests flat on resident’s head.
9.Determine the resident’s height.
10.Help resident off scale the before recording height. Make sure the rod does not hit resident in the head while doing so.
11.Wash your hands.
12.Immediately record the resident’s height.
13.Place the call light within the resident's reach.
14.Report any changes in resident to the nurse.
define restraint
a physical or chemical way to restrict voluntary movement or behavior
define restraint-free care
an environment in which restraints are not kept or used for any reason
define restraint alternatives
measures used in place of a restraint or that reduce the need for a restraint
why were restraints used in the past?
•Keep person from wandering
•Prevent falls
•Keep person from hurting self or others
•Keep person from pulling out tubing
what should NA know about restraints?
•Restraints are now generally used only as a last resort.
•Restraints can only be used with a doctor’s order.
•It is against the law for staff to apply restraints for convenience or discipline.
what are problems from restraint use?
•Pressure ulcers
•Pneumonia
•Risk of suffocation
•Reduced blood circulation
•Stress on the heart
•Incontinence
•Constipation
•Weakened muscles and bones
•Muscle atrophy (weakening or wasting away of the muscle)
•Loss of bone mass
•Poor appetite and malnutrition
•Depression and/or withdrawal
•Pressure ulcers
•Pneumonia
•Risk of suffocation
•Reduced blood circulation
•Stress on the heart
•Incontinence
•Constipation
•Weakened muscles and bones
•Muscle atrophy (weakening or wasting away of the muscle)
•Loss of bone mass
•Poor appetite and malnutrition
•Depression and/or withdrawal
what are restraint alternatives?
•Make sure call lights are within reach. Respond to call lights promptly.
•Improve safety measures to prevent accidents and falls. Improve lighting.
•Ambulate the person when he or she is restless. The doctor or nurse may add exercises to the care plan.
•Provide activities for those who wander at night.
•Encourage activities and independence. Escort the resident to social activities. Increase visits and social interaction.
•Give frequent help with elimination needs. Help with cleaning immediately after an episode of incontinence.
•Offer food or drink. Offer reading materials.
•Distract or redirect interest. Give the resident a repetitive task.
•Decrease the noise level. Listen to soothing music. Offer massages or use relaxation techniques.
•Reduce pain levels through medication. The resident should be monitored closely. Complaints of pain should be reported immediately.
•Provide familiar caregivers. Increase the number of caregivers by using family and volunteers.
•Use a team approach to meeting needs. Offer training to teach gentle approaches to difficult people.
when resident must be checked at least every 15 min, what must be done in ordered intervals?
•Release the restraint or discontinue use.
•Offer help with elimination. Check for episodes of incontinence and provide care.
•Offer fluids and food.
•Check for and report signs of skin irritation immediately.
•Check for and report signs of swelling immediately.
•Reposition the resident.
•Ambulate resident if able.
define intake
fluid a person consumes; also called input
define output
all fluid that is eliminated from the body; includes fluid in urine, feces, vomitus, perspiration, moisture that is exhaled in air, and wound drainage
define fluid balance
taking in and eliminating equal amounts of fluid
what are conversions NA should know?
1 ounce (oz) = 30 milliliters (mL) or 30 cubic centimeters (cc)
2 oz = 60 mL
3 oz = 90 mL
4 oz = 120 mL
5 oz = 150 mL
6 oz = 180 mL
7 oz = 210 mL
8 oz = 240 mL
1/4 cup = 2 oz = 60 mL
1/2 cup = 4 oz = 120 mL
1 cup = 8 oz = 240 mL
what steps for measuring and recording urinary output?
1.Wash your hands.
2.Put on gloves before handling bedpan/urinal.
3.Pour the contents of the bedpan or urinal into graduate. Do not spill or splash any of the urine.
4.Place graduate on flat surface. Measure the amount of urine at eye level. Keep the container level.
4.Note the amount on paper, converting to mL if necessary. (If the amount is between measurement lines, you may need to round up to the nearest 25 mL.) Follow policy.
5.After measuring urine, empty the graduate into the toilet. Do not splash urine.
6.Rinse the graduate. Pour rinse water into toilet.
7.Rinse the bedpan/urinal. Pour rinse water into the toilet. Flush the toilet.
8.Place graduate and bedpan in the area for cleaning or clean and store according to facility policy.
9.Remove and discard your gloves.
10.Wash your hands before recording output.
11.Immediately document the time and amount of urine in output column on sheet. For example: 1545 hours, 200 mL urine.
12.Report any changes in resident to the nurse.
define specimen
a sample that is used for analysis in order to try to make a diagnosis
define routine urine specimen
a urine specimen that can be collected any time a person voids
define voids
urinates
define hat
in health care, a collection container that can be inserted into toilet bowl to collect and measure urine or stool
define clean-catch specimen
a urine specimen that does not include the first and last urine voided; also called mid-stream specimen
what should NA know about collecting urine specimens
•NAs must wear gloves for these procedures.
•Tagging and storing specimens correctly is important.
•NAs should be sensitive to the fact that residents may find it embarrassing or uncomfortable to have others handling their body wastes.
•If an NA feels the task is unpleasant, he should not make it known. NAs must remain professional.
what are steps collecting a routine urine specimen
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain the procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on gloves.
6.Fit the hat to the toilet or commode, or provide resident with bedpan or urinal.
7.Ask the resident to void into the hat, urinal, or bedpan. Ask the resident not to put toilet paper in with the sample. Provide a plastic bag to discard the toilet paper separately.
8.Make sure the bed is in its lowest position. Place toilet paper and disposable wipes within resident’s reach. Ask resident to clean his hands with a wipe when finished if he is able.
9.Remove and discard gloves. Wash your hands.
10.Place the call light within the resident’s reach. Ask the resident to signal when done. Leave the room and close the door.
11.When called by the resident, return and wash your hands. Put on clean gloves. Give perineal care if help is needed.
12.Take the bedpan, urinal, or hat to the bathroom.
13.Pour urine into the specimen container until the container is at least half full.
14.Cover the urine container with its lid. Do not touch the inside of the container. Wipe off the outside with a paper towel.
15.Apply the label. Place the container in a clean specimen bag. Seal the bag.
16.Discard extra urine in the toilet. Flush the toilet. Rinse the bedpan, urinal, or hat if part of facility policy. Place equipment in proper area for cleaning or clean it according to facility policy.
17.Remove and discard your gloves.
18.Wash your hands.
19.Place the call light within the resident's reach.
20.Report any changes in resident to the nurse.
21.Take specimen and lab slip to the proper area. Document the procedure using facility guidelines. Note amount and characteristics of urine.
what are steps for collecting a clean-catch (midstream) urine specimen
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on gloves.
6.Open the specimen kit. Do not touch the inside of the container or the inside of the lid.
7.If the resident cannot clean his perineal area, you will do it. Use the cleansing wipes to do this. Be sure to use a clean area of the wipe or clean wipe for each stroke. See bed bath procedure in Chapter 6 for a reminder on how to give perineal care.
8.Ask the resident to urinate a small amount into the bedpan, urinal, or toilet, and to stop before urination is complete.
9.Place the container under the urine stream. Have the resident start urinating again. Fill the container at least half full. Ask the resident to stop urinating and remove the container. Have the resident finish urinating in the bedpan, urinal, or toilet.
10.After urination, provide a plastic bag so resident can discard the toilet paper. Give perineal care if help is needed. Ask resident to clean his hands with a wipe if he is able.
11.Cover the urine container with its lid. Do not touch the inside of the container. Wipe off the outside with a paper towel. Discard the paper towel.
12. Apply the label. Place the container in a clean specimen bag. Seal the bag.
13.Discard extra urine in the toilet. Flush the toilet. Rinse the bedpan, urinal, or hat if part of facility policy. Place equipment in proper area for cleaning or clean it according to policy.
14.Remove and discard gloves.
15.Wash your hands.
16.Place the call light within the resident's reach.
17.Report any changes in resident to the nurse.
18.Take the specimen and lab slip to the proper area. Document the procedure using facility guidelines. Note the amount and characteristics of the urine.
what are steps to collecting a stool specimen
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain the procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on gloves.
6.Ask the resident not to urinate when he is ready to move his bowels. Ask him not to put toilet paper in with the sample. Provide a plastic bag to discard toilet paper and wipes separately.
7.Fit the hat to the toilet or commode, or provide the resident with a bedpan.
8.Make sure bed is in its lowest position. Place toilet paper and disposable wipes within resident’s reach. Ask the resident to clean his hands with a wipe when finished if he is able.
9.Remove and discard your gloves. Wash your hands.
10.Place the call light within the resident’s reach. Ask the resident to signal when done. Leave the room and close the door.
11.When called by the resident, return and wash your hands. Put on clean gloves. Give perineal care if help is needed.
12.Using the 2 tongue blades, take about 2 tablespoons of stool and put it in the container. Without touching the inside of the container, cover it tightly. Apply the label and place the container in a clean specimen bag. Seal the bag.
13.Wrap the tongue blades in toilet paper. Put them in the plastic bag with the used toilet paper and wipes. Discard the bag in the proper container.
14.Empty the bedpan or container into the toilet. Flush the toilet. Rinse the bedpan if part of facility policy. Place equipment in the proper area for cleaning or clean it according to policy.
15.Remove and discard your gloves.
16.Wash your hands.
17.Place the call light within the resident's reach.
18.Report any changes in resident to the nurse.
19.Take the specimen and lab slip to the proper area. Document the procedure using facility guidelines. Note the amount and characteristics of the stool.
what are steps for collecting a 24-hour urine specimen?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Place a sign on the resident's bed to let all care team members know that a 24-hour specimen is being collected. The sign might read "Save all urine for 24-hour specimen."
6.When starting the collection, have the resident completely empty the bladder. Discard the urine. Note the exact time of this voiding. The collection will run until the same time the next day.
7.Label the container with the resident’s name, date of birth, room number, and dates and times the collection period began and ended.
8.Wash hands and put on gloves each time the resident voids.
9.Pour urine from bedpan, urinal, or hat into the container. Container may be stored at room temperature, in the refrigerator, or on ice. Follow facility policy.
10.After each voiding, help as necessary with perineal care. Ask the resident to clean his hands with a wipe after each voiding.
11.After each voiding, place equipment in proper area for cleaning or clean it according to facility policy.
12.Remove and discard gloves.
13.Wash your hands.
14.After the last void of the 24-hour period, remove the sign. Take specimen and lab slip to proper area. Document the procedure using facility guidelines. Make sure to include the time of the last void before the 24-hour collection period began and the last void of the 24-hour collection period.
what are steps for collecting a sputum specimen?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on mask and gloves. Coughing is one way that TB bacilli can enter the air. Stand behind the resident if the resident can hold the specimen container by himself.
6.Ask the resident to cough deeply, so that sputum comes up from the lungs. To prevent the spread of infectious material, give the resident tissues to cover his mouth. Ask the resident to spit the sputum into the specimen container.
7.When you have obtained a good sample (about two tablespoons of sputum), cover the container tightly. Wipe any sputum off the outside of the container with tissues. Discard the tissues. Apply label, and place the container in a clean specimen bag and seal the bag.
8.Remove and discard gloves and mask.
9.Wash your hands.
10.Place the call light within the resident's reach.
11.Report any changes in resident to the nurse.
12.Take specimen and lab slip to proper area. Document the procedure using facility guidelines.
define catheter
a thin tube inserted into body to drain or inject fluids
define urinary catheter
a type of catheter that is used to drain urine from bladder
define straight catheter
a type of urinary catheter that is removed immediately after urine is drained or collected
define indwelling catheter
a type of urinary catheter that remains inside the bladder for a period of time; also called Foley catheter.
define condom catheter
a type of urinary catheter that has an attachment on the end that fits onto the penis; also called Texas catheter.
what should NAs know about these guidelines when a resident has a urinary catheter?
•Wash your hands thoroughly.
•Clean the genital area at least daily.
•Keep drainage bag lower than the resident’s hips or bladder to prevent infection and let gravity allow drainage.
•Keep drainage bag off floor.
•Keep tubing straight.
what should NA observe for and report when a resident has a urinary catheter?
•Bloody or unusual-looking urine
•Bag not filling after several hours
•Bag filling suddenly
•Catheter not in place
•Urine leaking from catheter
•Resident reporting pain or pressure
•Odor
what are steps for providing catheter care?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Adjust bed to a safe level, usually waist high. Lock the bed wheels.
6.Lower head of bed. Position resident lying flat on her back.
7.Remove or fold back the top bedding. Keep the resident covered with the bath blanket.
8.Test water temperature with the water thermometer or on the inside of your wrist to ensure it is safe. Water temperature should be no higher than 105°F. Have the resident check the water temperature. Adjust if necessary.
9.Put on gloves.
10.Ask the resident to flex her knees and raise her buttocks off the bed by pushing against the mattress with her feet. Place a clean bed protector under her perineal area including her buttocks.
11.Expose only the area necessary to clean the catheter. Avoid overexposing the resident.
12.Place a towel under the catheter tubing before washing.
13.Wet a washcloth in the basin. Apply soap to the washcloth. Clean area around the meatus. Use a clean area of the washcloth for each stroke.
14.Hold the catheter near the meatus. Avoid tugging the catheter.
15.Clean at least four inches of the catheter nearest the meatus. Move in only one direction, away from the meatus. Use a clean area of the washcloth for each stroke.
16.Dip a clean washcloth in the water. Rinse area around the meatus, using a clean area of the washcloth for each stroke. With a clean, dry towel, dry the area around the meatus.
17.Dip a clean washcloth in the water. Rinse at least four inches of catheter nearest the meatus. Move in only one direction, away from meatus. Use a clean area of the washcloth for each stroke.
18.With a clean, dry towel, dry at least four inches of the catheter nearest the meatus. Move in only one direction, away from meatus. Do not tug the catheter.
19.Remove and discard the bed protector. Remove the towel from under the catheter tubing and place in proper container. Place used washcloths in proper container.
20.Place used washcloths in the proper container.
21.Empty the basin into the toilet and flush the toilet. Place basin in proper area for cleaning or clean and store it according to policy.
22.Remove and discard your gloves
23.Wash your hands.
24.Remove the bath blanket and replace the top covers.
25.Return the bed to its lowest position.
26.Place the call light within the resident's reach.
27.Report any changes in the resident to the nurse.
28.Document the procedure using facility guidelines.
what are steps for emptying the catheter drainage bag?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Put on gloves.
6.Place a paper towel on the floor under the drainage bag. Place the graduate on the paper towel.
7.Open the clamp on the bag so that the urine flows out of the bag and into the graduate. Do not let the spout or clamp touch the graduate.
8.When the urine has drained from the bag, close the clamp. Using alcohol wipes, clean the drain spout. Place the drain spout back in its holder on the bag.
9.Go into the bathroom. Place the graduate on a flat surface and measure at eye level. Note the amount and the characteristics of the urine. Empty the urine into the toilet and flush the toilet.
10.Clean and store the graduate. Discard paper towels.
11.Remove and discard your gloves.
12.Wash your hands.
13.Document the procedure using facility guidelines. Note the amount and characteristics of urine.
define oxygen therapy
administration of oxygen to increase the supply of oxygen to lungs
define combustion
process of burning
define flammable
easily ignited and capable of burning quickly
what should NAs know about guidelines for oxygen safety?
•Post No Smoking and Oxygen in Use signs. Do not allow smoking around oxygen equipment.
•Remove fire hazards. Report to nurse if resident does not want a fire hazard removed.
•Do not allow flames around oxygen (this includes candles).
•Do not use an extension cord with an oxygen concentrator.
•Do not place electrical cords or oxygen tubing under rugs or furniture.
•Avoid using fabrics such as nylon and wool.
•Report skin irritation from cannula or face mask.
•Do not use any petroleum-based products on resident or on any part of the cannula or mask.
•Learn how to turn oxygen off in case of fire if facility allows this. Never adjust oxygen setting.
what should NAs understand their role in caring for residents with IVs?
•NAs never insert or remove IV lines.
•NAs do not care for the IV site.
•NAs only observe the site for changes or problems and report if
•Tube/needle falls out
•Tubing disconnects
•Dressing is loose
•Blood is in tubing or around site
•Observe the site for changes or problems and report if (cont'd)
•Site is swollen or discolored
•Resident complains of pain
•IV bag breaks or fluid level does not decrease
•IV fluid is not dripping or is leaking
•IV fluid is nearly gone
•Pump beeps
•Pump is dropped
•Resident complains of pain or has trouble breathing
what must an NA not do with a resident with an IV?
•Measure B/P on an arm with an IV line
•Get the IV site wet
•Pull or catch the tubing on anything
•Leave the tubing kinked
•Lower the IV bag below the site
•Touch the clamp
•Disconnect IV from pump or turn off alarm
what should warm and cold applications be used for?
Nursing assistants may be allowed to prepare and apply warm and cold applications. NAs should only perform procedures that are assigned to them. They should never perform a procedure they are not trained or allowed to do.
Applying heat or cold to injured areas can have several positive effects. Heat relieves pain and muscular tension. It reduces swelling, elevates the temperature in the tissues, and increases blood flow. Increased blood flow brings more oxygen and nutrients to the tissues for healing. Cold applications can help stop bleeding. They help prevent swelling, reduce pain, and bring down high fevers. Applying ice bags or cold compresses immediately after an injury can stop bleeding and prevent swelling.
•Moist applications include the following:
•Compresses (warm or cold)
•Soaks (warm or cold)
•Tub baths (warm)
•Sponge baths (warm or cold)
•Sitz baths (warm)
•Ice packs (cold)
Dry applications include the following:
•Aquamatic K-pad® (warm or cold)
•Electric heating pads (warm)
•Disposable warm packs (warm)
•Ice bags (cold)
Application | Temperature | Timing | Special Considerations |
Warm Compresses | No higher than 105° | Remove after 20 mins. | Cover with plastic wrap. |
Warm soaks | No higher than 105° | Check temp. every five mins. | Observe for redness. Soak 15-20 mins. |
Aquamatic K-pad | Pre-set | Remove after 20 mins. | Tubing should not hang below bed. Check water level and refill when necessary |
Sitz baths | No higher than 105° | 20 mins. only | Fill 2/3 full. Provide privacy. |
Ice packs | Check after 10 mons. Remove after 20 mins | Fill bag 2/3 full of ice. Cover bag; watch for blisters and white or pale skin. | |
Cold compresses | Cold water with ice | Check after five mins. Remove after 20 mins | Check for blisters, redness, and white or gray skin |
what is the equipment is usually found in a resident’s unit?
•Bed
•Bedside stand
•Urinal/bedpan and covers
•Wash basin
•Emesis basin
•Soap dish and soap
•Bath blanket
•Toilet paper
•Personal hygiene items
•Overbed table
•Chair
•Call light
•Privacy screen or curtain
what are guidelines for resident’s unit are?
•Clean the overbed table after each use.
•Keep the call light within reach.
•Keep equipment clean and in good condition. Report problems with equipment to nurse or according to facility guidelines.
•Layer clothing and bed covers for warmth. Keep residents away from drafty areas. The NA should not change the temperature for the NA’s comfort.
•Remove meal trays promptly, then remove crumbs and straighten linens. Change linens if they are wet, soiled, or wrinkled.
•Restock personal supplies as needed. Keep water pitchers filled.
•Notify housekeeping department if trash needs to be emptied. Empty trash if housekeeping is not available or not on duty.
•Report signs of insects or pests immediately.
•Do not move residents’ belongings.
•Clean equipment and return it to proper storage. Tidy the area.
what problems do lack of sleep cause?
•Decreased mental function
•Reduced reaction time
•Irritability
•Decreased immune system function
what factors can affect sleep patterns?
•Fear
•Stress
•Noise
•Diet
•Medications
•Illness
•Noise in the hallway
•Sharing a room with another person
what should NAs observe for when a resident is not sleeping well?
•Sleeping too much during the day
•Eating or drinking items that contain caffeine late in the day
•Dressing in nightclothes during the day
•Eating heavy meals late at night
•Refusing prescribed medication
•Taking new medications
•Having TV, radio, computer, or light on late at night
•Pain
define occupied bed
a bed made while a person is in bed
define unoccupied bed
a bed made while no person is in bed
define closed bed
a bed completely made with bedspread and blankets in place
define open bed
a bed made with linen folded down to the foot of the bed
why is bedmaking important?
•Damp and wrinkled sheets are uncomfortable and may keep the resident from sleeping well.
•Microorganisms thrive in moist, warm places and damp, unclean bedding may cause infection or disease.
•Sheets that are not flat increase risk for pressure ulcers.
what are guidelines for bedmaking?
•Keep linens wrinkle-free and tidy.
•Wash your hands before handling clean linen.
•Place clean linen on a clean surface, such as chair or bedside stand. Do not place linen on the floor or in a contaminated area.
•Don gloves before removing bed linen.
•Look for personal items before removing linen.
•When removing linen, fold or roll linen so the dirtiest area is inside.
•Do not shake linen or clothes.
•Bag soiled linen at point of origin, and do not take it to other residents’ rooms.
•Sort soiled linen away from care areas.
•Place wet linen in leakproof bags.
•Wear gloves when handling soiled linen. Hold soiled linen away from your body. If dirty linen touches your uniform, your uniform becomes contaminated.
•Change disposable bed protectors whenever they are soiled or wet, and dispose of them properly.
what are the steps for making an occupied bed?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Place clean linen on clean surface within reach (e.g., bedside stand, overbed table, or chair).
6.Adjust bed to a safe level, usually waist high. Lower the head of the bed. Lock the bed wheels.
7.Put on gloves.
8.Loosen top linen from the end of the bed on the working side.
9.Unfold the bath blanket over the top sheet to cover the resident. Remove the top sheet. Keep the resident covered at all times with the bath blanket.
10.You will make the bed one side at a time. Raise the far side rail (if used). Then go to the other side of the bed. Help the resident to turn onto her side toward the raised side rail.
11.Loosen the bottom soiled linen , mattress pad, and protector, if present, on the working side.
12.Roll the bottom soiled linen toward the resident, soiled side inside. Tuck it snugly against the resident’s back.
13.Place the mattress pad (if used) on the bed, attaching elastic corners on the working side.
14.If a flat sheet is used, leave enough overlap on each end to tuck under the mattress. Make hospital corners to keep the bottom sheet wrinkle-free. If a fitted sheet is used, tightly pull the two fitted corners on the working side. Finish with the bottom sheet free of wrinkles.
15.Smooth the bottom sheet out toward the resident. Be sure there are no wrinkles in the mattress pad. Roll the extra material toward the resident. Tuck it under the resident’s body.
16.If using a disposable bed protector, unfold it and center it on the bed. Tuck the side near you under the mattress. Smooth it out toward the resident. Tuck as you did with the sheet.
17.If using a draw sheet, place it on the bed. Tuck in on your side, smooth, and tuck as you did with the other bedding.
18.Raise side rail (if used) nearest you. Go to the other side of the bed and lower that side rail. Help the resident roll or turn onto clean bottom sheet toward the raised side rail. Protect the resident from any soiled matter on the old linens.
19.Loosen the soiled linen. Check for any personal items. Roll linen from the head to the foot of the bed. Avoid contact with your skin or clothes. Place it in a hamper or bag. Do noy put it on the floor or furniture. Do not shake it. Soiled linens are full of microorganisms that should not be spread to other parts of the room.
20.Pull the clean linen through as quickly as possible. Start with the mattress pad and wrap it around corners. Pull and tuck in the clean bottom linen just like the other side. Pull and tuck in the bed protector and draw sheet (if used). Make hospital corners with the bottom sheet. Finish with bottom sheet free of wrinkles.
21.Ask resident to turn onto her back. Help as needed. Keep the resident covered and comfortable, with a pillow under her head. Raise the side rail nearest you.
22.Unfold the top sheet. Place it over the resident and center it. Ask the resident to hold the top sheet. Slip the bath blanket out from underneath. Put it in the hamper or bag.
23.Place a blanket over the top sheet. Match the top edges. Place the bedspread over the blanket (if used), matching the top edges. Tuck the bottom edges of the top sheet, blanket, and bedspread under the foot of the bed. Make hospital corners on each side. Loosen the top linens over the resident’s feet. At the head of the bed, fold the top sheet over the blanket about 6 inches.
24.Remove the pillow. Do not hold it near your face. Remove the soiled pillowcase by turning it inside out. Place it in the hamper or bag.
25.Remove and discard gloves. Wash your hands.
26.With one hand, grasp the clean pillowcase at the closed end. Turn it inside out over your arm. Next, using the same hand that has the pillowcase over it, grasp the center of the end of the pillow. Pull the pillowcase over it with your free hand. Do the same for any other pillows. Place them under the resident’s head with the open end away from the door.
27.Make resident comfortable.
28.Return bed to lowest position. Leave side rails in the ordered position.
29.Place the call light within the resident's reach.
30.Take the laundry bag or hamper to the proper area.
31.Wash your hands.
32.Report any changes in resident to the nurse.
33.Document the procedure using facility guidelines.
what are steps in making an unoccupied bed?
1.Wash your hands.
2.Place clean linen on clean surface within reach (e.g., bedside stand, overbed table, or chair).
3.Adjust bed to a safe level, usually waist high. Put the bed in its flattest position. Lock the bed wheels.
4.Put on gloves.
5.Loosen soiled linen. Roll it (soiled side inside) from the head to the foot of the bed. Avoid contact with your skin or clothes. Place it in a hamper or bag. Do not put it on the floor or furniture. Do not shake it. Remove pillows and pillowcases and place pillowcases in the hamper or bag.
6.Remove and discard your gloves. Wash your hands.
7.Remake the bed. Place the mattress pad (if used) on the bed, attaching elastic at corners on the working side. If a flat sheet is used, leave enough overlap on each end to tuck under the mattress. Make hospital corners to keep the bottom sheet wrinkle-free. If a fitted sheet is used, tightly pull the two fitted corners on the working side. Finish with the bottom sheet free of wrinkles. Put on the disposable bed protector and draw sheet (if used), smooth, and tuck under the sides of the bed.
8.Place top sheet and blanket and bedspread (if used) over bed. Center these, tuck under end of bed, and make hospital corners. Fold down the top sheet over the blanket about 6 inches. Fold both top sheet and blanket down so the resident can easily get into bed. If the resident will not be returning to bed immediately, leave the bedding up.
9.Put on clean pillowcases. Replace pillows.
10.Return bed to lowest position.
11.Take the laundry bag or hamper to proper the area.
12.Wash your hands.
13.Document the procedure using facility guidelines.
what should NA know about dressings?
•NAs do not change sterile dressings, which cover open or draining wounds.
•Nonsterile dressings are for wounds that have less chance of infection.
•NAs may change nonsterile dressings.
what are steps for changing a dry dressing using nonsterile technique?
1.Identify yourself by name. Identify the resident according to facility policy.
2.Wash your hands.
3.Explain procedure to the resident. Speak clearly, slowly, and directly. Maintain face-to-face contact whenever possible.
4.Provide for the resident's privacy with a curtain, screen, or door.
5.Open the gauze package without touching the gauze. Place the opened package on a flat surface.
6.Put on gloves.
7.Remove the soiled dressing by gently peeling the tape toward the wound. Lift the dressing off the wound, angling it so that the resident cannot see the soiled side. Do not drag it over the wound. Observe the dressing for odor or drainage. Notice the color and size of the wound. Do not ask the resident to look at the wound. Discard the used dressing in the plastic bag.
8.Remove and discard your gloves in plastic bag. Wash your hands.
9.Put on clean gloves. Touching only outer edges of new gauze, remove it from package. Apply it to wound. Tape gauze in place. Secure firmly.
10.Discard supplies in proper container.
11.Remove and discard your gloves.
12.Wash your hands.
13.Place the call light within the resident's reach.
14.Report any changes in resident to the nurse.
15.Document procedure according to facility guidelines.
what should NA know about elastic bandages?
•Elastic bandages hold dressings in place, secure splints, and support and protect body parts. They may decrease swelling from an injury.
•NAs may assist with use of an elastic bandage.
•Some states allow NAs to apply and remove elastic bandages. NAs must follow facility's policy.
what are guidelines for applying elastic bandages?
•Keep area clean and dry.
•Apply snugly enough to control bleeding but make sure not to wrap too tightly, as this can decrease circulation.
•Wrap bandage evenly.
•Do not tie the bandage; use special clips.
•Remove bandage as indicated in care plan.
•Ten to 15 minutes after bandage is applied, check for signs of poor circulation; loosen if any of these signs are present:
•Swelling
•Pale, gray, cyanotic or white skin
•Shiny, tight skin
•Skin that is cold to touch
•Sores
•Numbness
•Tingling
•Pain or discomfort