EXAM 1- Mirza
1/70
Earn XP
Description and Tags
Based on lecture notes and things said in class.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
How our body responds to the administration of a drug or the “drug response” is controlled by _______________________________.
drug CONCENTRATIONS (NOT DOSES)
What is pharmacokinetics (PK)?
pharmacokinetics- what the body does to a drug
will determine dose and dose frequency
What is pharmacodynamics (PD)?
pharmacodynamics- what the drug does to the body
What is the important link between PK and PD?
drug concentration at the site of action
What do the letters of ADME stand for?
EXAM QUESTION from ADME slide (didn’t specify)
A- absorption
D- distribution
M- metabolism
E- excretion
What step of the ADME PK process makes drugs more polar, ionizable, and thus more water soluble?
Metabolism
What step of the ADME PK process physically removes the drug from the body?
excretion
PRACTICE:
Which of the following is not a PK process?
a. metabolism
b. excretion
c. absorption
d. disintegration
d
The combination of metabolism and excretion is known as __________________.
elimination
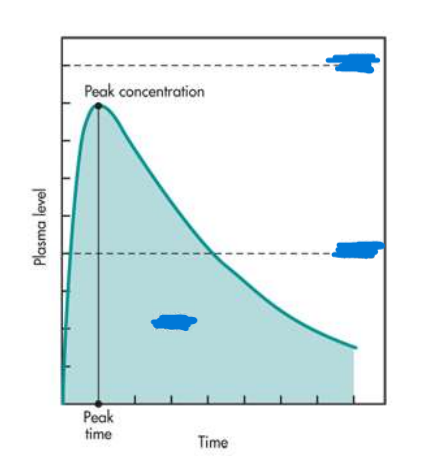
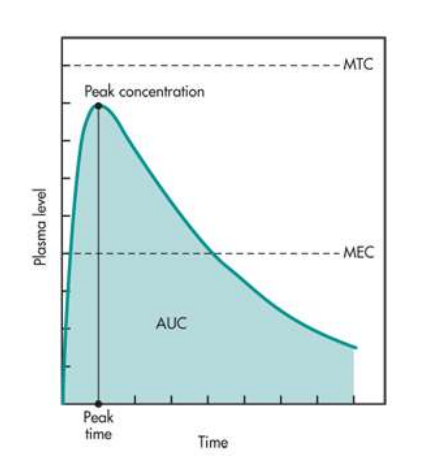
Label the graph with the following terms:
MEC
AUC
MTC
(EXAM Q on this topic)
Which of the following parameters is mostly relevant to the desired drug response?
a. dose
b. therapeutic index
c. peak time
d. plasma concentration
e. concentration at the site of action
(EXAM QUESTION)
d
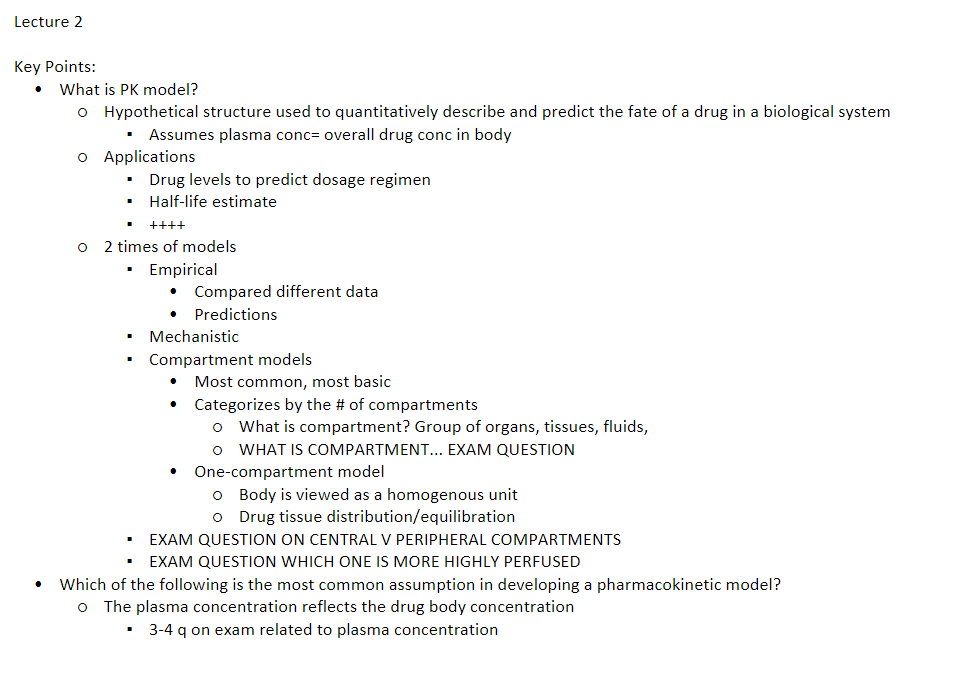
In most PK models, it is assumed that the plasma concentration = _______________________________________________?
plasma concentration = the overall drug concentration in the body
What are 3 common applications of PK models?
drug half-life estimation
drug accumulation predictions
bioequivalence studies
What are the 2 common PK models and their sub-groups? (not that important)
empirical models
mechanistic models- physiological models and compartmental models
(FOCUS ON COMPARTMENTAL MODELS!!!!!!!!!)
Empirical models are based on ________.
data
Explain physiologically based models. (a type of mechanistic model)
divide the body into 3 parts (blood/capillaries, extracellular space, and intracellular space)
describes drug uptake and disposition
useful for a NEW drug when NO data is available
What is the most common and basic PK model?
compartmental models
Compartment Models are based on ____________assumptions and ________________differential equations
linear, linear
WHAT IS A COMPARTMENT?
EXAM Q!!!!!!!!!!!!!!!!!!!!!!!!
group of organs, tissues, or fluids with similar drug distribution and drug affinity
Compartment models can further be categorized into 3 groups. What are they?
one-compartment
two-compartment
multicompartment
What’s the difference between one and two compartment models?
one-compartment: ENTIRE body is viewed as ONE unit or ONE compartment
distribution/equilibrium is instantaneous
two-compartment: body is viewed as TWO units or TWO compartments——central and peripheral compartments
distribution/equilibrium is NOT instantaneous
What organs belong to the central compartment in a two-compartment model?
EXAM Q on central v peripheral!!!!!!!!!
heart
liver
lungs
kidney
blood
What organs belong to the peripheral compartment in a two-compartment model?
EXAM Q on central v peripheral!!!!!!!
fat tissue
muscle tissue
cerebrospinal fluid
Does the central or peripheral compartment contain HIGHLY PERFUSED ORGANS?
EXAM Q on central v peripheral
CENTRAL!
Which of the following is the most common assumption in developing a pharmacokinetic model?
A. the body can be viewed as a single compartment
B. All body tissues are similar
C. All body fluids are similar
D. The plasma concentration reflects the drug body concentration
D
In the ADME PK process D stands for distribution. What is the definition of distribution?
a PK process by which a drug reversibly leaves the bloodstream to enter extracellular fluid and/or tissues
Is drug distribution equal or not equal throughout the entire body?
not equal
WHAT IS THE #1 FACTOR THAT EFFECTS DRUG DISTRIBUTION?
EXAM Q
blood flow rate
What are some other factors that effect drug distribution?
capillary permeability (BBB)
physicochemical properties of APIs (log P/lipophillicity)
plasma/tissue protein binding affinity of APIs (albumin, etc.)
In highly-perfused tissues, you see a _______ distribution. In poorly-perfused tissues, you see a _______ distribution.
In highly-perfused tissues, you see a high distribution. In poorly-perfused tissues, you see a slow distribution.
What are some examples of highly-perfused and poorly-perfused tissues?
highly- brain, kidney, liver
poorly- skeletal muscles, fat, adipose tissue
PRACTICE:
Would the liver have a fast or slow drug distribution?
fast (bc it’s a highly perfused organ)
If a drug has a higher affinity for plasma proteins/binds to them more, would the drug have a slower or faster distribution rate?
slower distribution (bc bound to proteins=cannot bind to tissues)
What is the definition of Volume of Distribution (Vd)?
the extent of drug distribution into body fluids and tissues is commonly described as the volume of distribution
Volume of distribution relates the amount of drug in the body to the measured concentration in ____________.
a. blood
b. tissues
c. plasma
d. capillaries
c
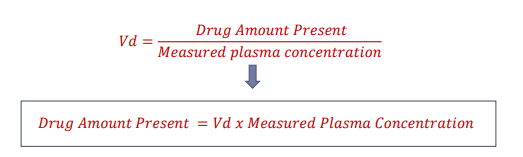
WHAT IS THE EQUATION for Vd?
must memorize, will be math problem on this
Vd= drug amount present (dose)/ measured plasma concentration (Cp)
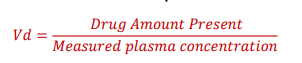
If I want to solve for the amount of drug present, how would I rearrange the Vd equation?
What is the relationship between Vd and plasma concentration?
when plasma conc decreases, Vd increases
when plasma conc increases, Vd decreases
(opposites)
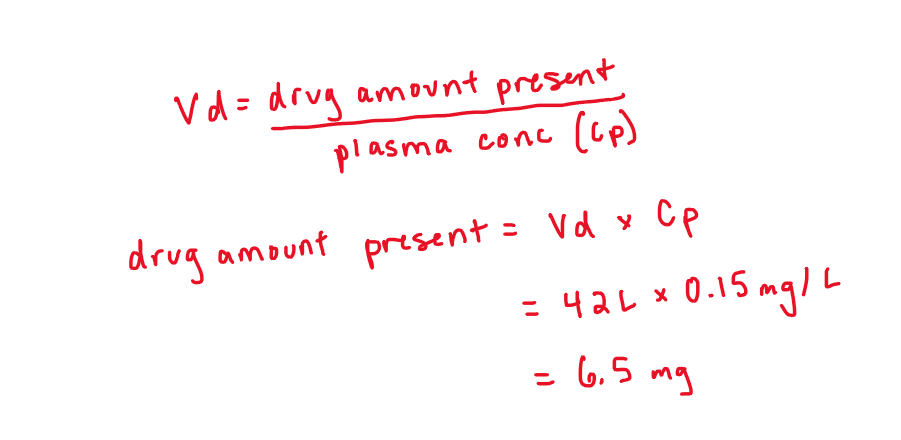
PRACTICE:
If the volume of distribution of a drug is 42 L and the measured plasma concentration (Cp) is 0.15 mg/L, calculate how much drug is in the body?
EXAM LIKE MATH QUESTION
6.5 mg
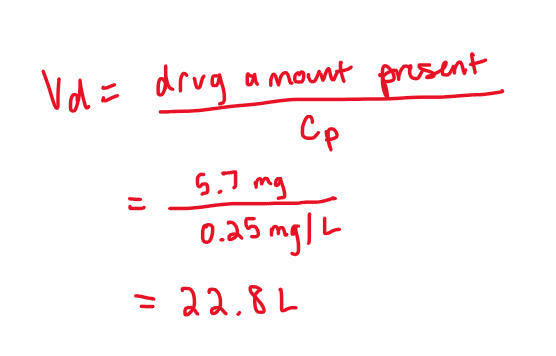
PRACTICE:
If the amount of drug in the body was 5.7 mg and the measured plasma concentration (Cp) is 0.25 mg/L, what is the volume of distribution?
EXAM LIKE MATH QUESTION
22.8 L
The amount of drug per unit of volume is defined as the:
a. volume of distribution
b. concentration
c. distribution rate
b (EXAM QUESTION ON CONCENTRATION)
Which of the following is most likely confined to the plasma?
Drug | Vd (L) |
Amlodipine | 16.0 |
Ganciclovir | 1.1 |
APAP | 51 |
Ganciclovir (Why? Low Vd means it’s confined to the plasma, cannot reach tissues)
What is an IV bolus? (Prof K)
drug administration via a rapid IV injection
entire dose enters systemic circulation
What type of PK model is used to describe IV bolus doses? Describe this model. (Prof K)
uses a one-compartment model
drug distribution is instantaneous
system is “open” (means that all drugs that enters, also exits)
excretion is 1st order kinetic process
Calculating Dose Required PRACTICE:
Calculate the IV bolus dose required to achieve an initial drug concentration of 20 mcg/mL, if the Vd is 80 L. (Prof K)
1,600,000 mcg or 1,600 mg
convert 80L to mL
Use equation from Mirza’s previous pp: Plasma Concentration (Cp)= amount of drug (dose)/ Vd
Solve for “dose”
Calculating Concentration PRACTICE:
A 2-kg neonate is given a 25-mg/kg dose of phenobarbital. The estimated volume of distribution of phenobarbital in neonates is 0.9 L/kg. What is the estimated concentrated (Cp) after the administered dose? (Prof K)
27.7 mg/L
Volume of distribution and dose is in mg/kg so you need to take 2 times each to figure out the actual Vd and dose
Use equation from Mirza’s previous pp: Plasma Concentration (Cp)= amount of drug (dose)/ Vd
Solve for Cp
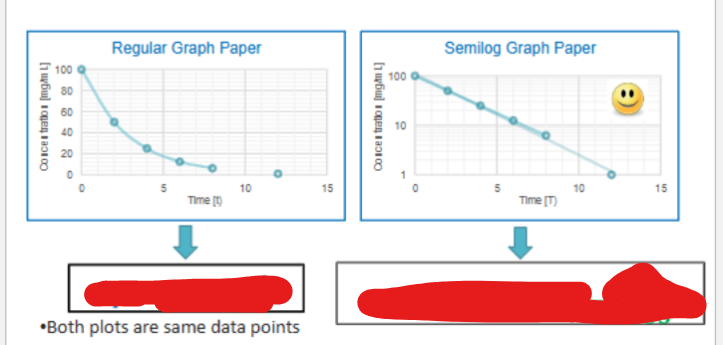
What are the first-order equations for a PK curve?
MUST MEMORIZE THESE FOR EXAM WILL NOT BE GIVEN
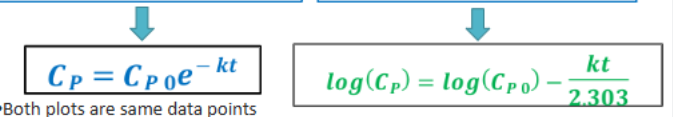
When reading a first-order process on semilog graph paper, what is the y-intercept?
Cp0
(aka the initial concentration)
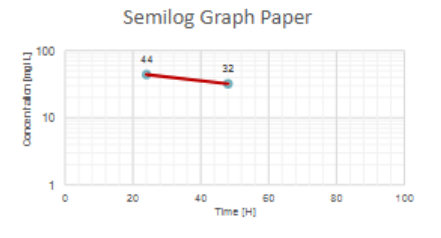
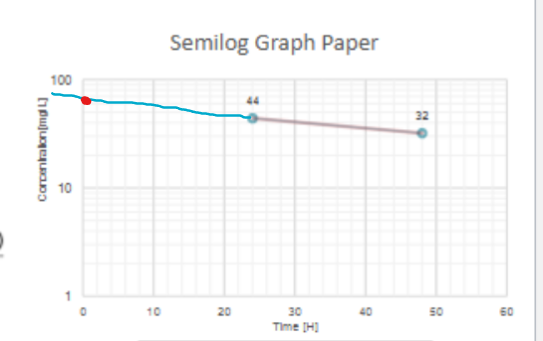
From this graph tell me long it will take for the concentration to fall from 32 mg/L to 20 mg/L
Somewhere between 17-22 hours (graph is open to interpretation)
From the already existing line between the two points, imagine it extending past beyond and see where 20 mg/L would land
Subtract the time of 32mg/L by the time for 20 mg/L
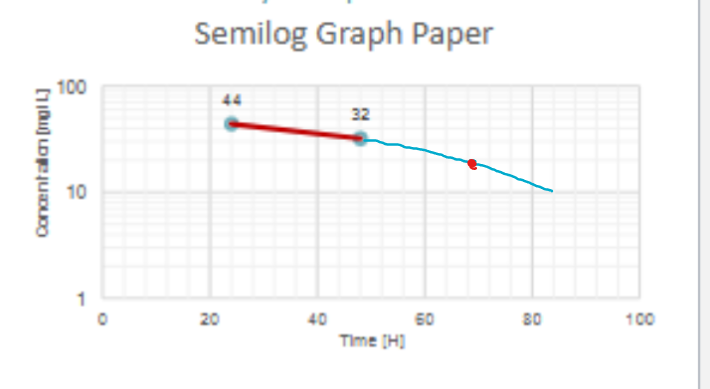
What would be Cp0? (or the initial conc)
around 60 mg/L
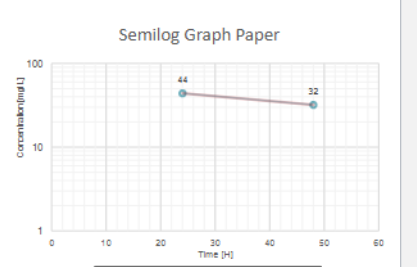
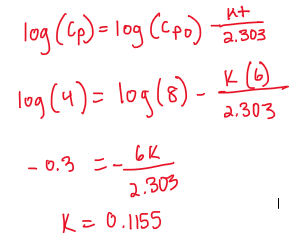
Instead of looking at a chart and determining concentrations, we can do it graphically. The following 2 concentrations were determined after administration of an IV bolus dose of a drug:
Cp (mg/L) | 8 | 4 |
T (hrs) | 3 | 9 |
___________ | _____________ | _____________ |
What is the elimination rate constant (k)?
k= 0.1155
Use 1st order equation and act like the first column of #’s is Cp0 (8,3) and the other column is Cp (4,9)
t is 6 because 9-3
solve for k
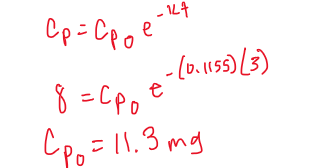
Instead of looking at a chart and determining concentrations, we can do it graphically. The following 2 concentrations were determined after administration of an IV bolus dose of a drug:
Cp (mg/L) | 8 | 4 |
T (hrs) | 3 | 9 |
___________ | _____________ | _____________ |
What is the initial plasma concentration?
Use exponential first order equation
Use one of the data points (8,3) or (4,9) to calculate the Cp0
What is half-life?
the time required for plasma concentration to decrease by 50%
Half-life is _____________ for first-order processes.
constant
What is the equation for half-life?
T1/2= 0.693/k
IF the elimination rate constant is 0.25 h-1, the percent of drug removed per hour is:
A. 0.25%
B. 1%
C. 2.5%
D. 25%
D
What is clearance?
EXAM QUESTION
a measure of the rate of removal of drug from plasma
the VOLUME of plasma completely cleared from the drug PER UNIT TIME
What are the units for clearance? What are the units for volume of distribution?
EXAM QUESTION
clearance- volume/time (ex: mL/min, L/h)
Vd= volume (ex: mL, L)
PRACTICE:
Which of the following parameters could be clearance?
a. 80L
b. 70 mg/L
c. 45 ml/h
d. 0.25 h-1
c (vol/time)
Clearance and Vd are two ___________________ parameters that determine a drug’s half-life.
EXAM QUESTION
INDEPENDENT
PRACTICE:
If CL changes from 10 to 30 L/h, what happens to Vd?
REMAINS CONSTANT. BC Vd AND CL ARE INDEPENDENT OF EACH OTHER
If CL increases, what happens to half-life?
decreases (half-life and CL have a proportional relationship)
Solve using CL= k*Vd
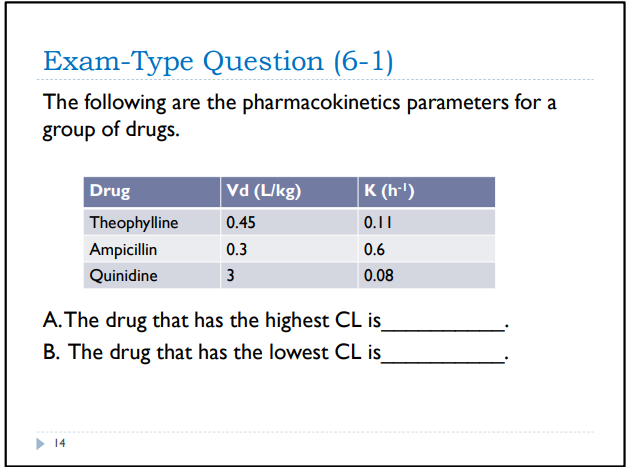
A. The drug that has the highest CL is Quinidine.
B. The drug that has the lowest CL is Theophylline.