Lecture 13 Pelvis and Pelvic Viscera
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
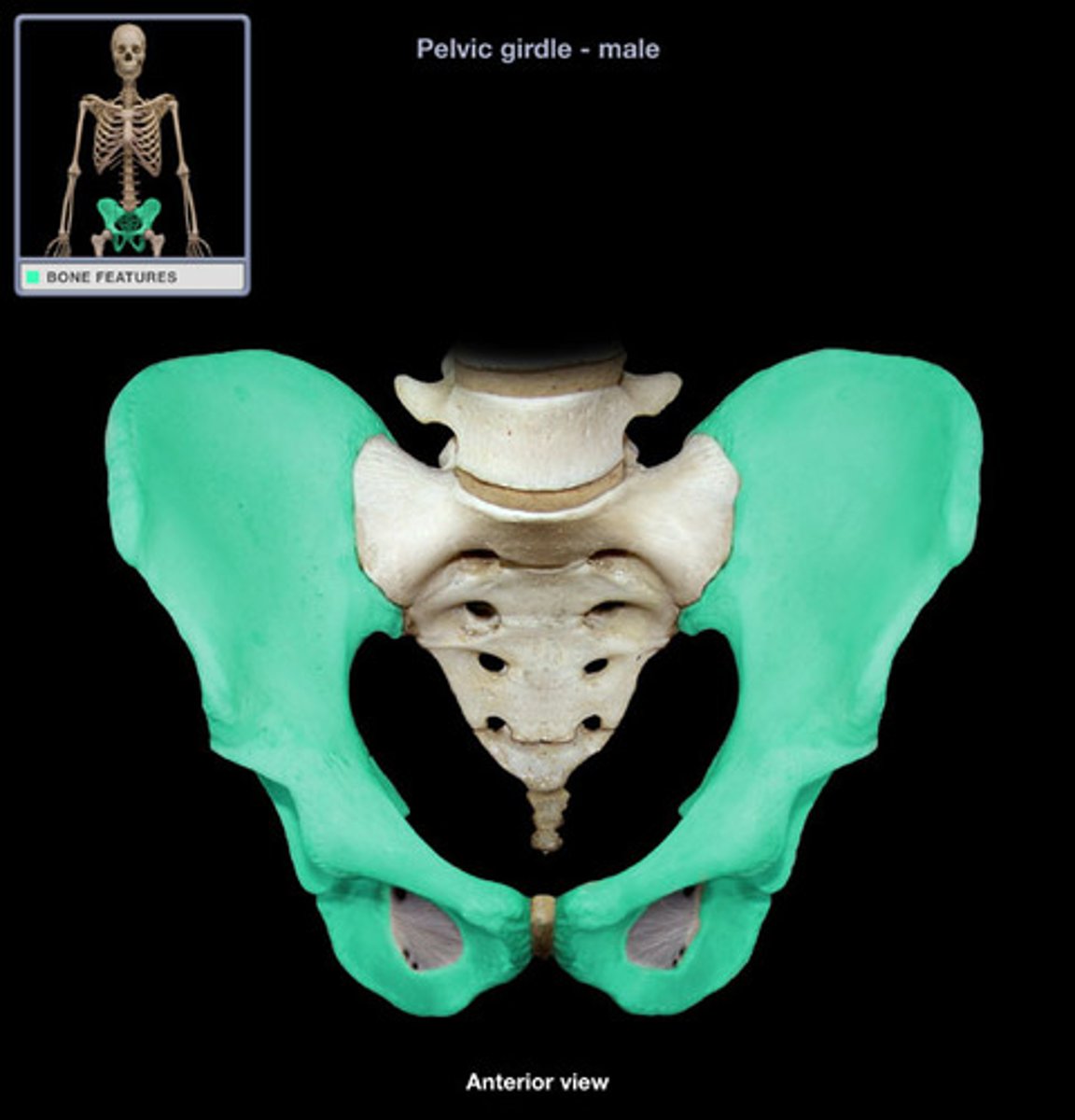
Pelvic girdle
-Protects the pelvic viscera and the inferior abdominal viscera
-Allows for passage
-Attachment for external genitalia
-Attachment for muscles that form the pelvic floor
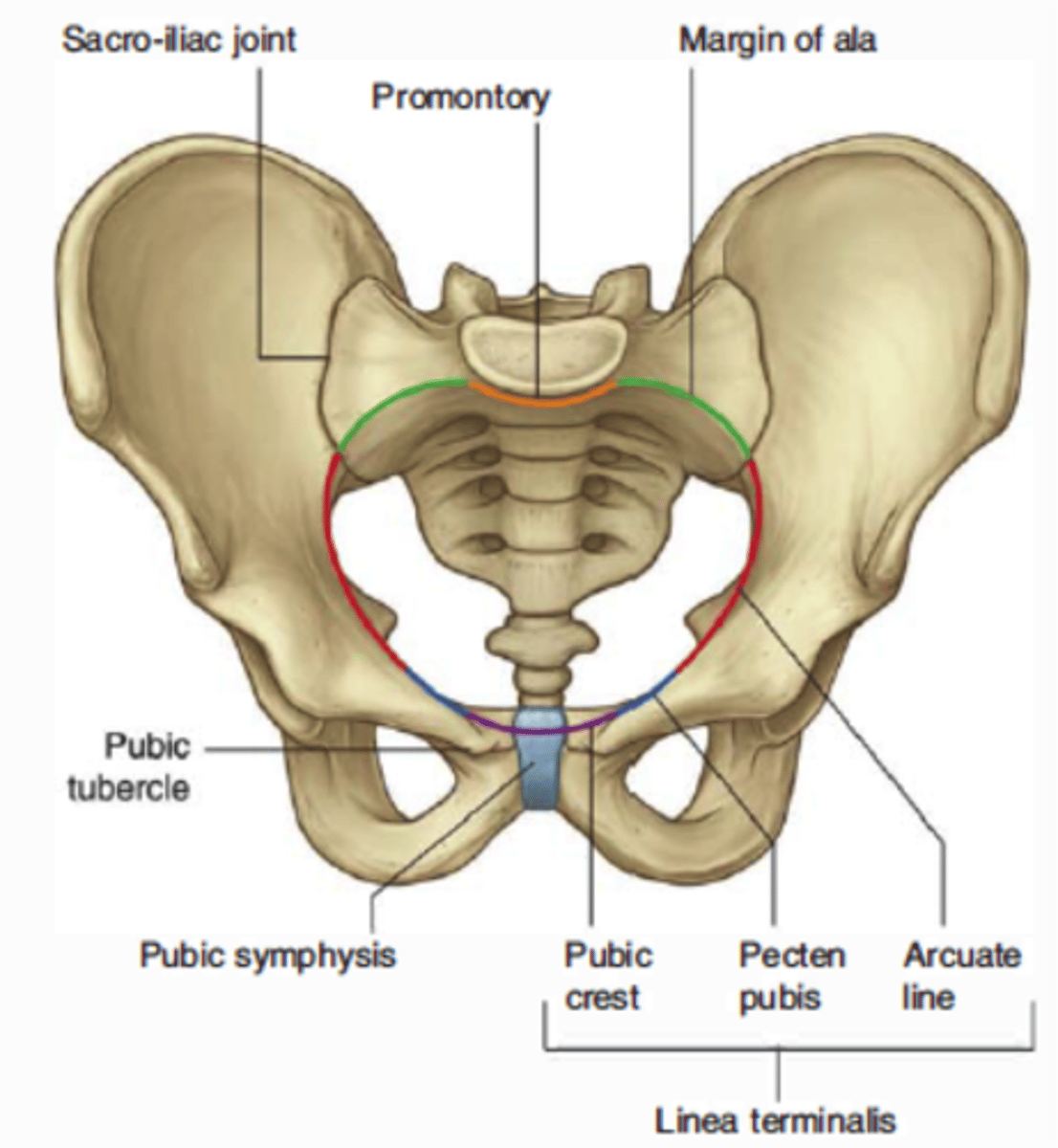
Pelvic inlet boundaries
-Sacral promontory (posterior)
-Arcuate lines (lateral)
-Pubic symphysis (anterior)
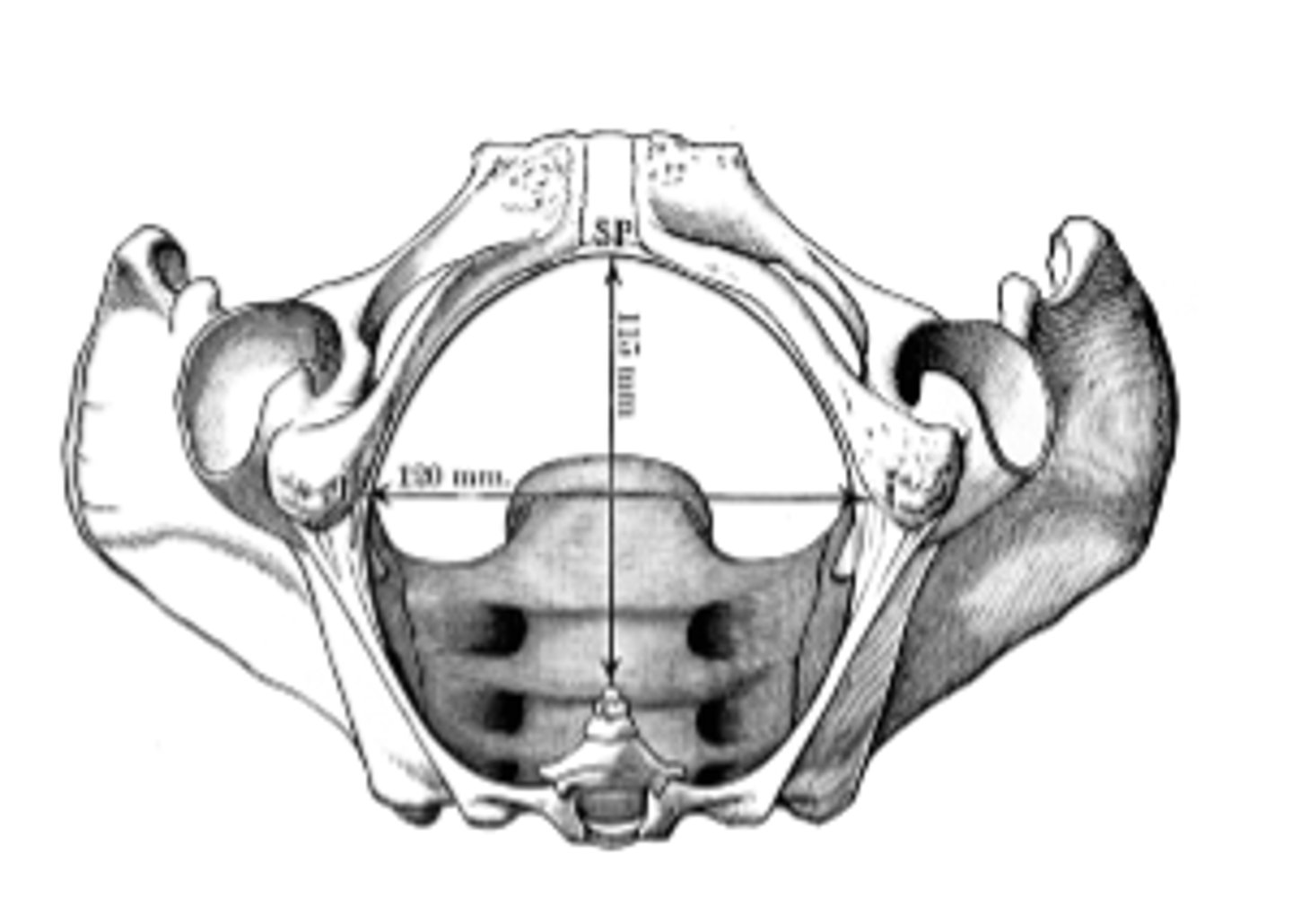
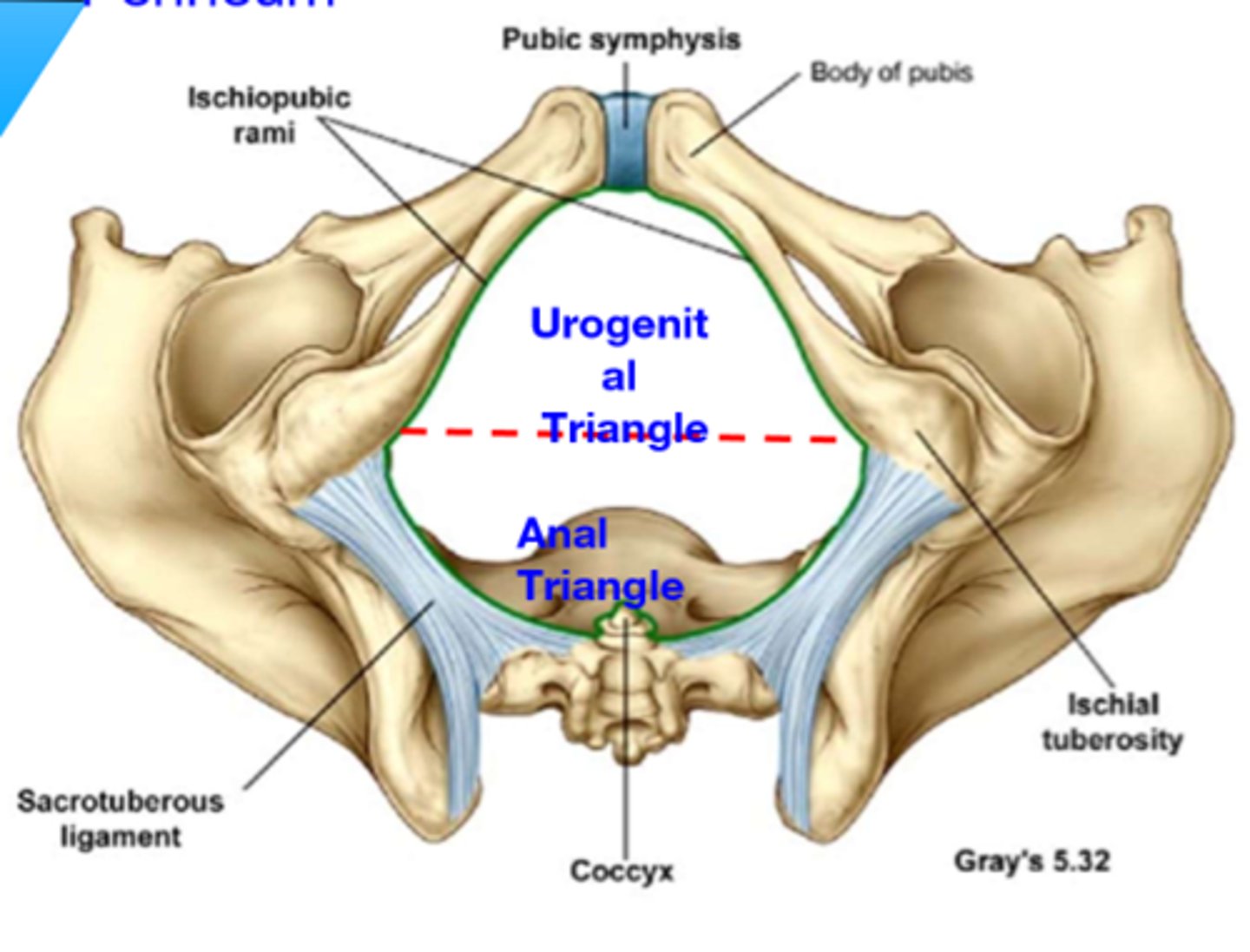
Pelvic outlet boundaries
-Tip of coccyx (posterior)
-Sacrotuberous ligament (posterolateral)
-Ischial tuberosities (anterolateral)
-Pubic symphysis (anterior)
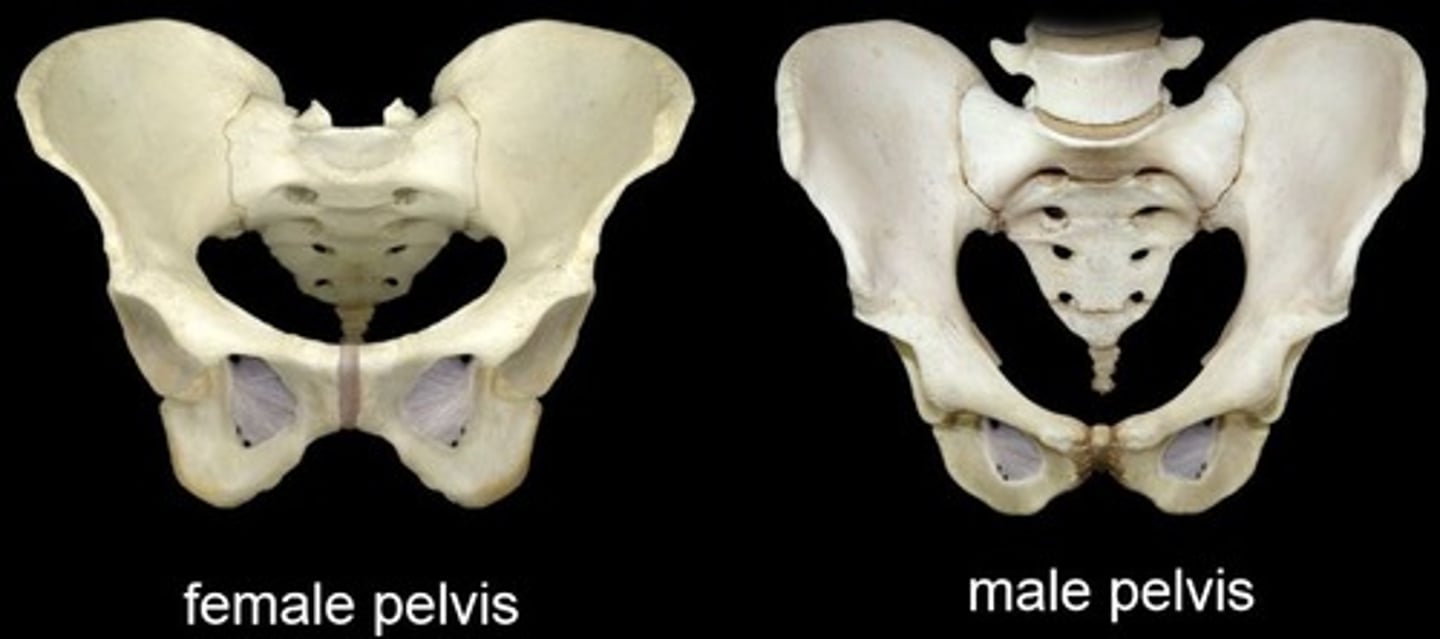
male pelvis
-heart shaped pelvic inlet
-narrow pubic arch
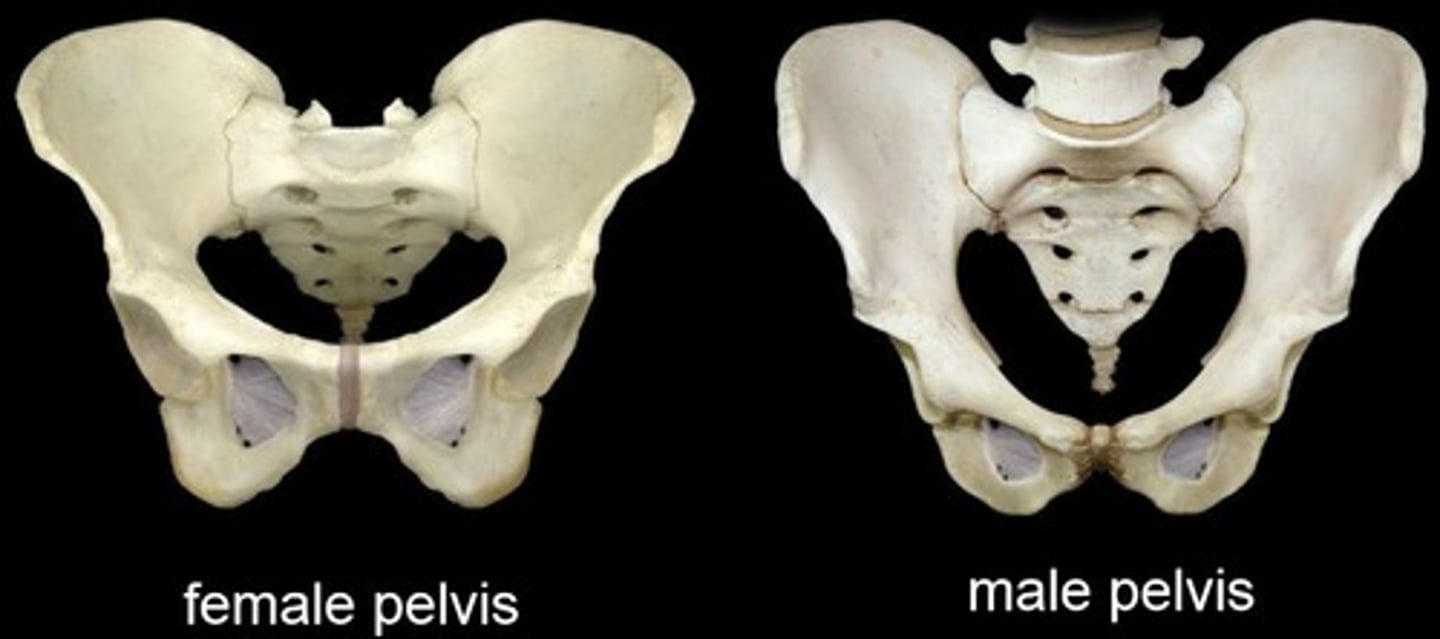
female pelvis
-more oval shaped
-shallow greater and lesser pelvis
-wide pubic arch
-larger pelvic outlet
What part of the pelvis increases during pregnancy?
the circumference of the lesser pelvis increases during pregnancy
What joints contribute to increases the transverse and interspinous diaeters?
The sacroiliac and pubic symphysis joints contribute 10-15% increase in transverse and interspinous diameters.
What happens to the obstetrical diameter and the sacroiliac joint to permit rotation of the pelvis?
-Obstetrical diameter remains unaffected
-Sacroiliac joint loosens to permit greater rotation of the pelvis
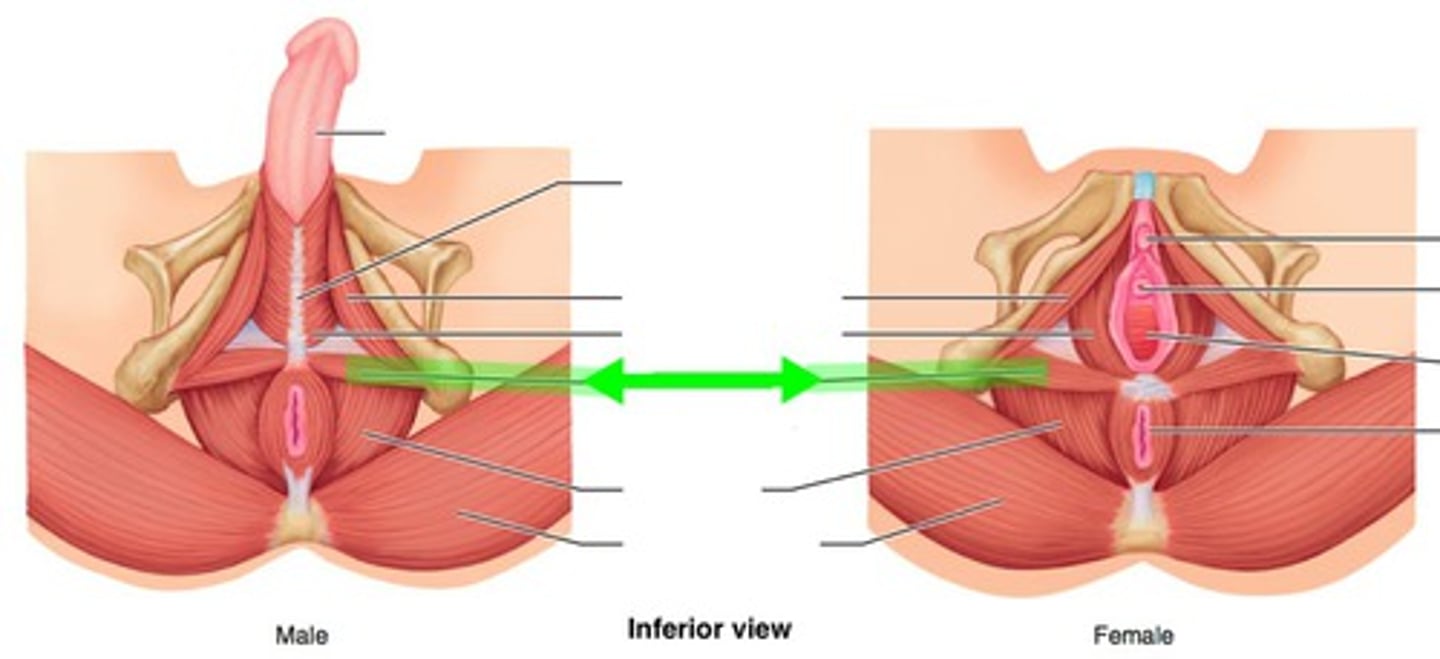
What is the perineum and its two major triangles?
The perineum is the region below the pelvic diaphragm, and it is divided into the urogenital triangle and the anal triangle.
What are the components of the female reproductive system located within the pelvis?
Components include:
-uterus
-ovaries
-uterine (fallopian) tubes
-cervix
-vagina
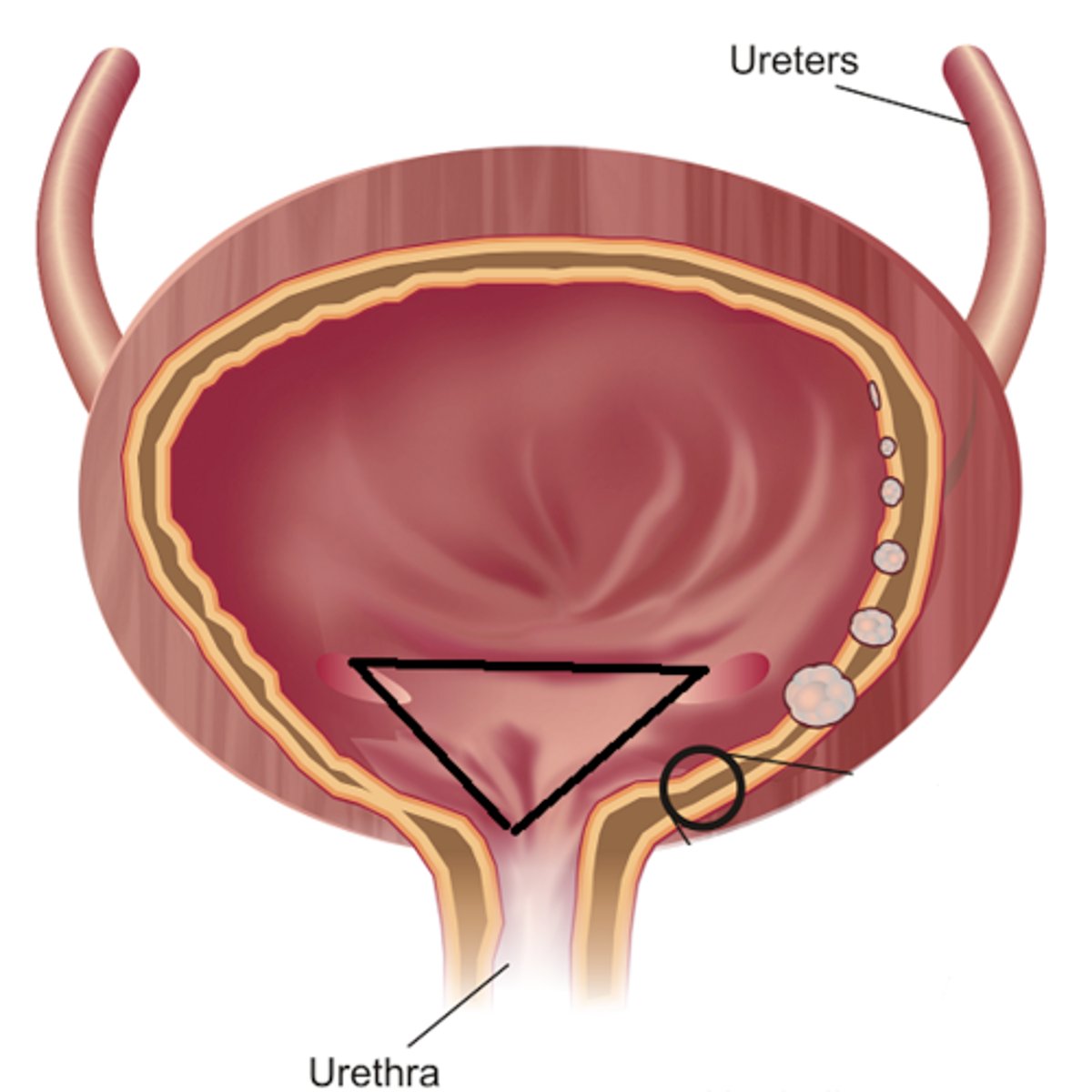
What is the trigone and where is it located?
The trigone is a smooth triangular region of the bladder, marked by the openings of the ureters and the urethra.
-"funnel into the urethra"
What are the main components of the male urogenital system located within the pelvis?
The components include:
-bladder
-prostate
-ductus deferens
-seminal vesicles
-ejaculatory ducts
-and parts of the urethra.
What are the subdivisions of the levator ani muscle and their functions?
The levator ani muscle is subdivided into
-puborectalis (supports the rectum)
-pubococcygeus (supports pelvic organs), and
-iliococcygeus (forms part of the pelvic floor)
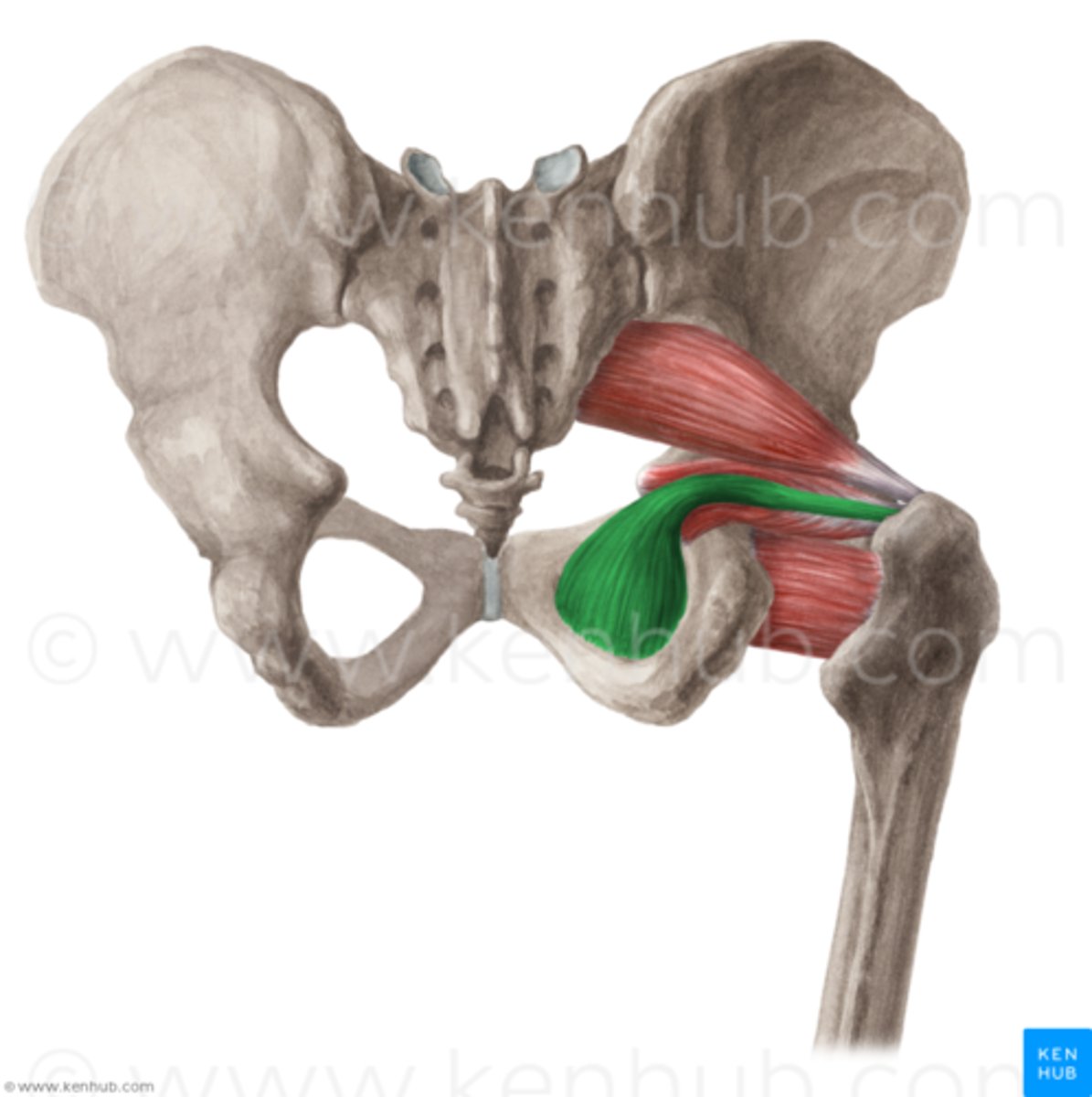
What are the muscles of the pelvic cavity?
The muscles of the pelvic cavity include:
-piriformis
-obturator internus
-levator ani
-coccygeus (ischiococcygeus)
What are the functions of the perineal body?
The perineal body acts as an important attachment point for muscles of the pelvic floor, maintaining the integrity of the pelvic diaphragm, especially during childbirth.
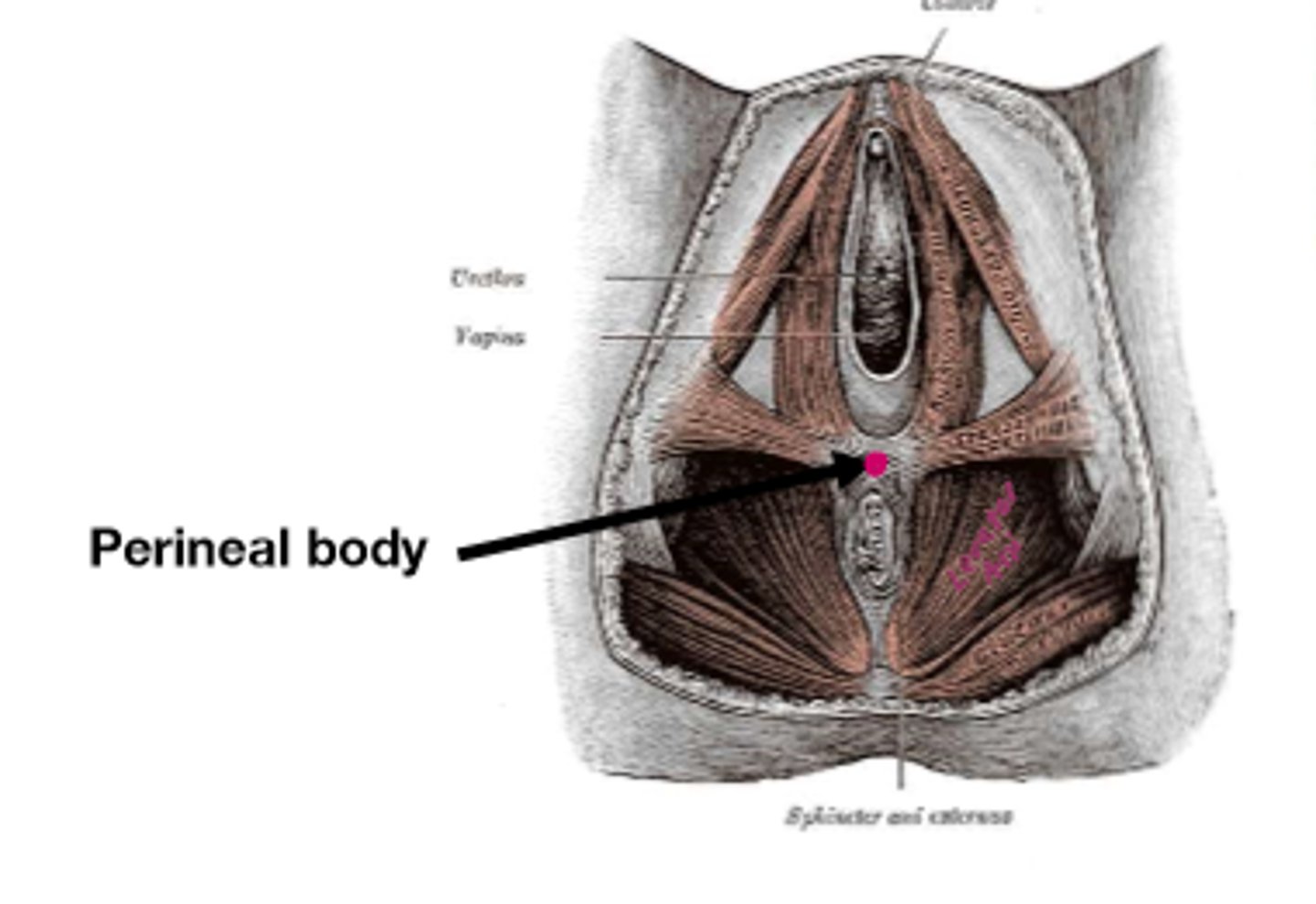
Where is the perineal body located?
located in the midline of the perineum, between the urogenital triangle (anterior) and the anal triangle (posterior).
What are the components of the pelvic diaphragm?
The pelvic diaphragm consists of the
-levator ani
-coccygeus muscles.
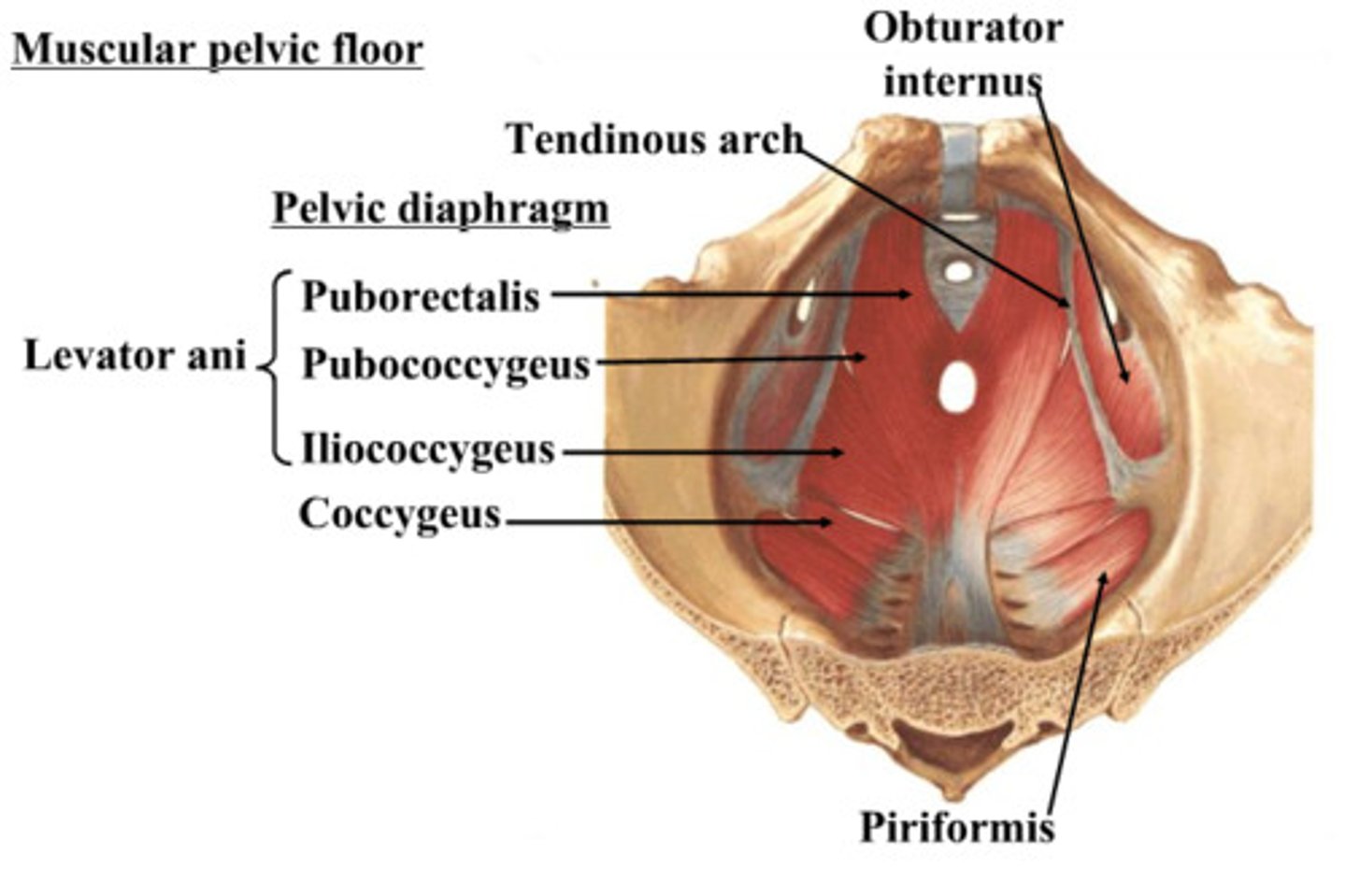
What does the obturator interus cover?
obturator foramen
What is the purpose of an episiotomy?
surgical incision that guides location and tear during birth
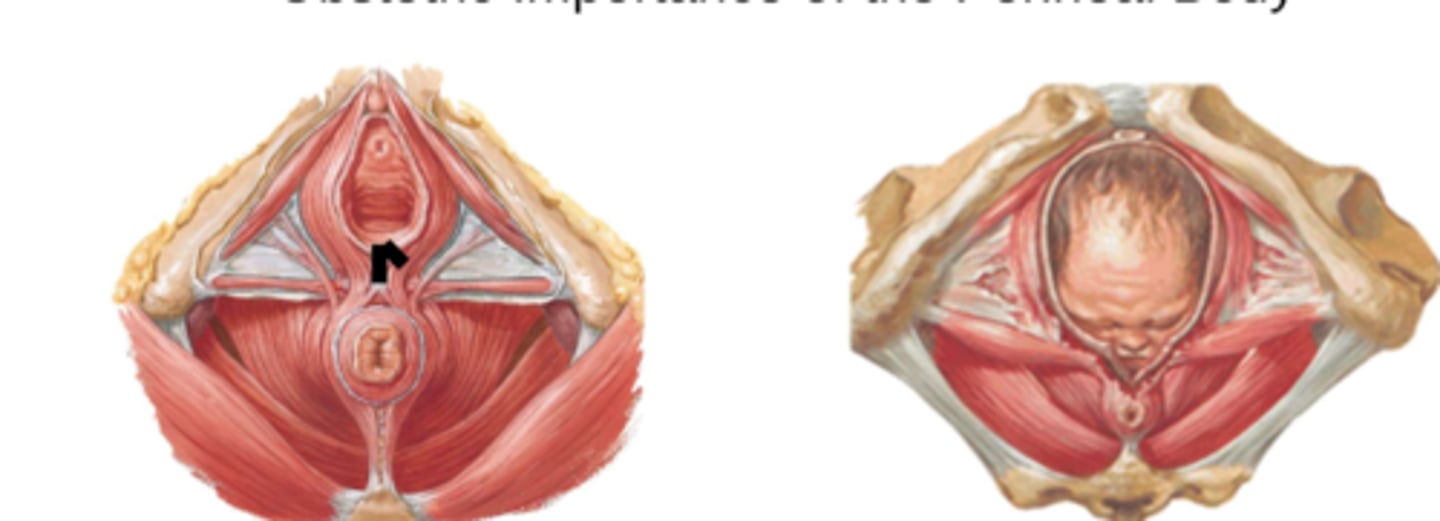
What effect does disruption of the perineal body have on the pelvic floor?
disruption of the perineal body can destabilize the pelvic floor, leading to prolapse, incontinence, and other issues related to pelvic organ support and muscle function
-pelvic floor muscle insertion site
pelvic fascia
connective tissue that occupies space between membranous peritoneum and muscular pelvic walls and floor not occupied by the pelvic viscera
-peritoneum (superior) drapes the top of pelvic organs
-floor fascia (inferior)
Median umbilical ligament
a remnant of urachus (allantois)
Describe the arterial supply to the pelvis.
The posterior division of the internal iliac artery supplies the posterior abdominal wall and gluteal region, while the anterior division supplies the bladder, reproductive organs, and pelvic floor.
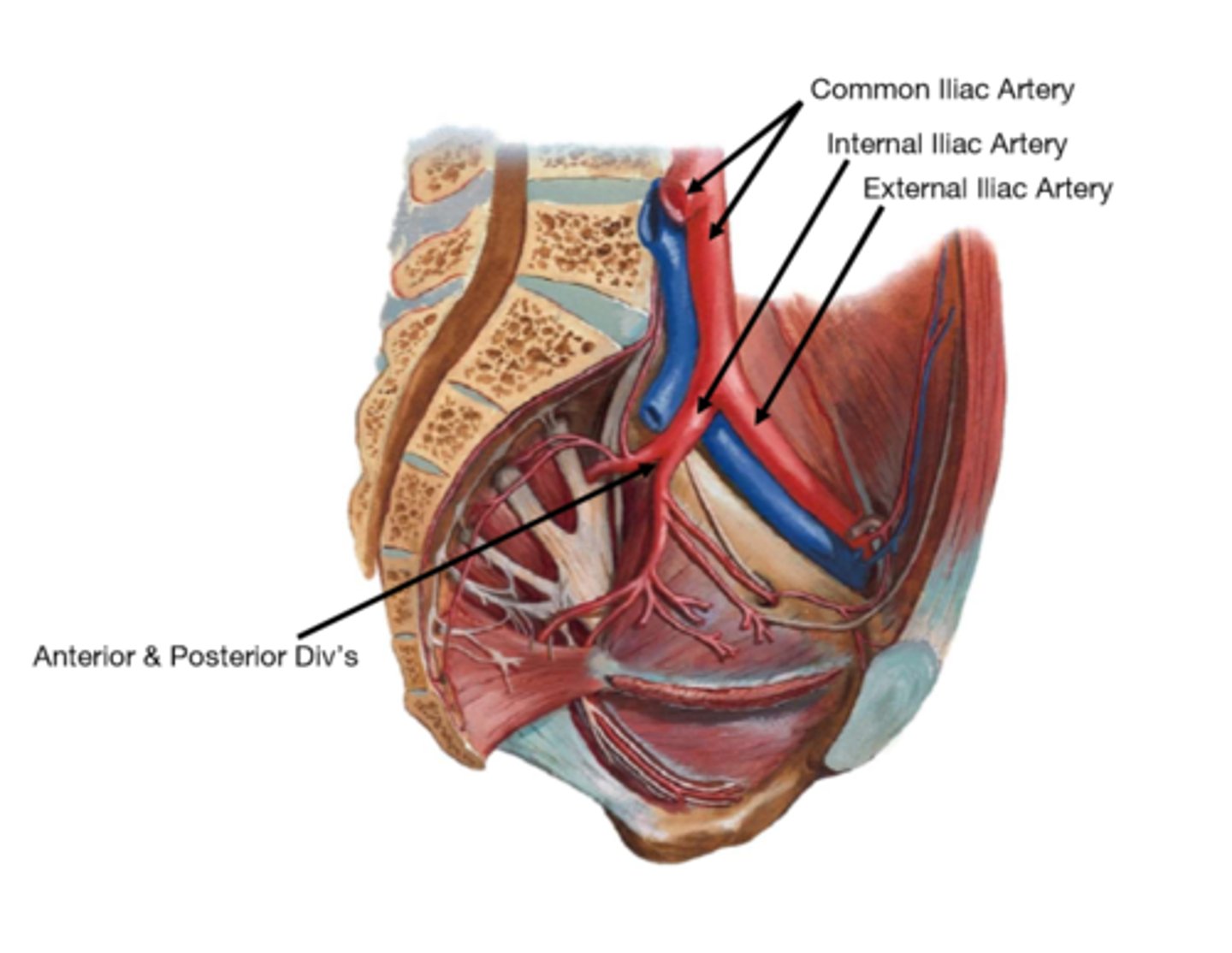
What does the posterior division of the internal iliac artery supply?
-posterior abdominal wall
-gluteal region
What does the anterior division of the internal iliac artery supply?
-bladder
-reproductive organs
-pelvic floor
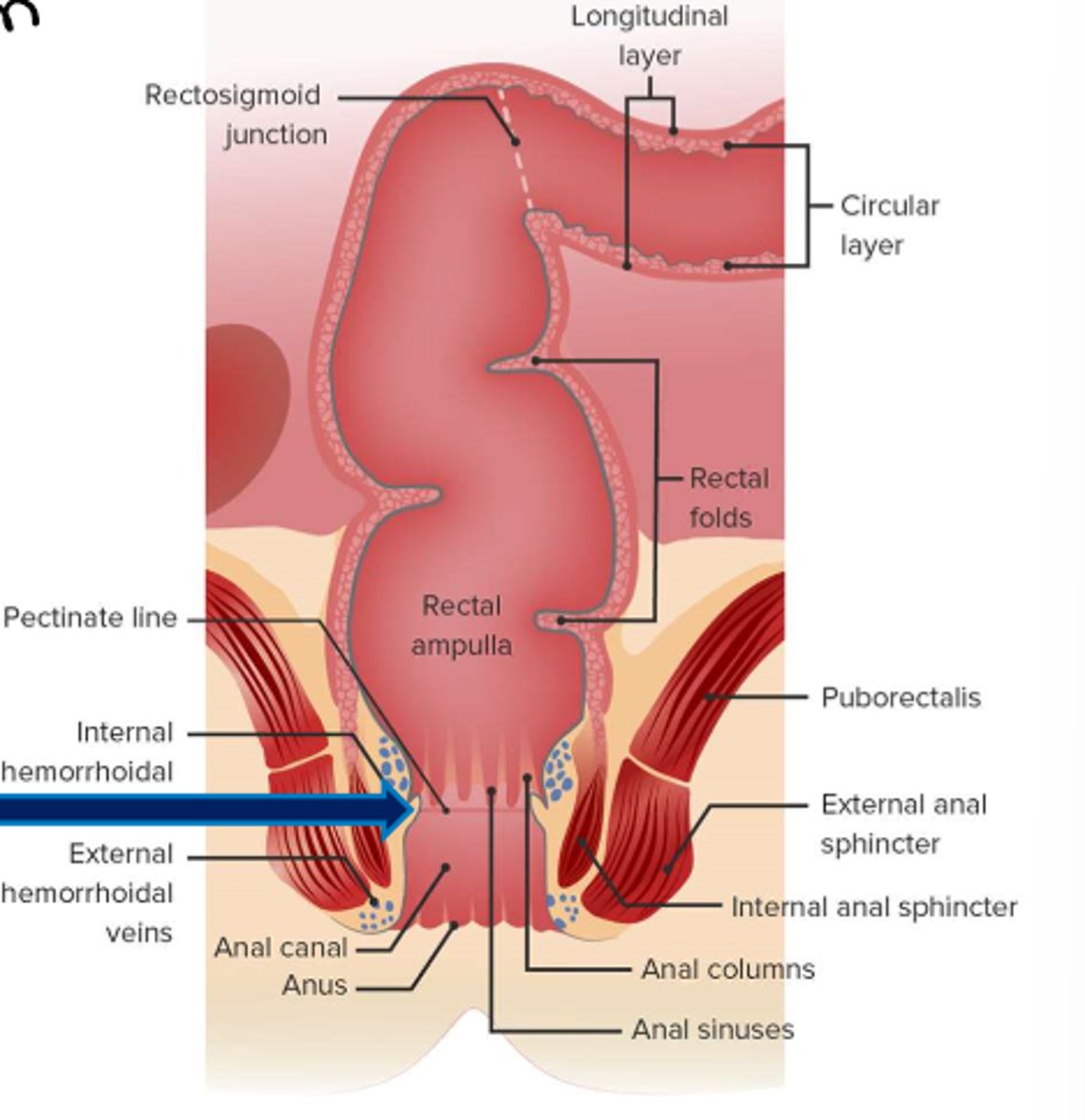
What are the anatomical divisions of the rectum?
The rectum is divided into three parts:
-the proximal portion (intraperitoneal)
-the middle portion (retroperitoneal)
-the distal portion (below the pelvic diaphragm)
What is the pectinate line and its significance?
The pectinate line separates the most distal portion of the rectum from the proximal and middle portions.
It marks the transition between
-endoderm and ectoderm
-portal vs. caval drainage
-hypogastric plexus vs. pudendal nerve innervation.
Ischiorectal fossa
fat-filled area between the pelvic diaphragm muscle and the lateral wall of the bony pelvis
-most conserved fat region in the body
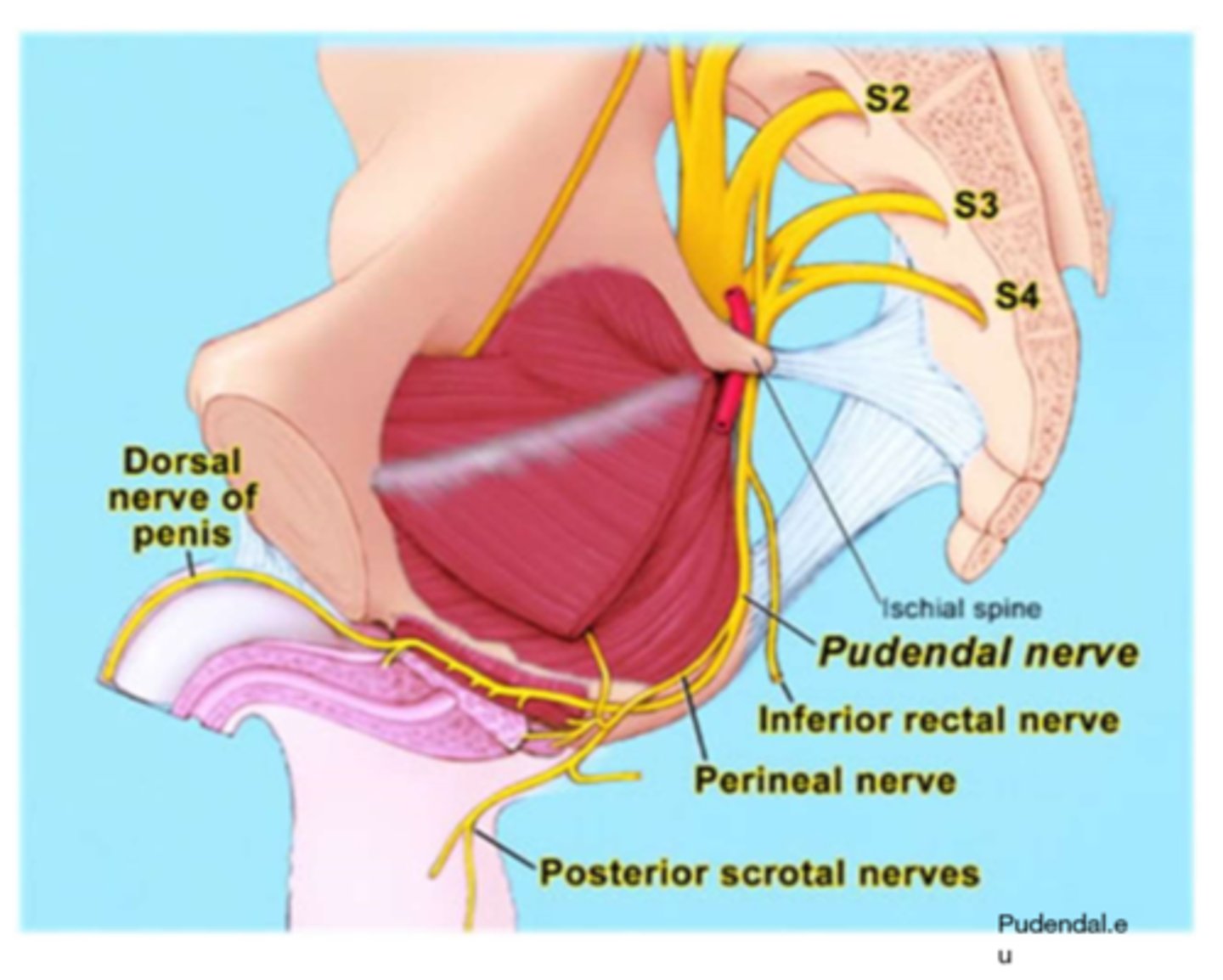
What is the significance of the pudendal nerve in the pelvis?
The pudendal nerve supplies the external genitalia, perineum, and anal region. It travels through the pudendal canal and is crucial for both sensory and motor functions.
Describe the course o the pudendal nerve.
1. Originates from the sacral plexus - ventral rami of spinal nerves S2, S3, and S4
2. Exits the pelvis - through the greater sciatic foramen
3. Under the Sacro tuberous ligament
4. Re-enters pelvis - via lesser sciatic foramen
5. Runs into the pudendal canal and branches to supply sensory and motor fibers to pelvic organs, viscera, and floor.
ejaculatory duct
seminal vesicle duct joins with ductus deferens

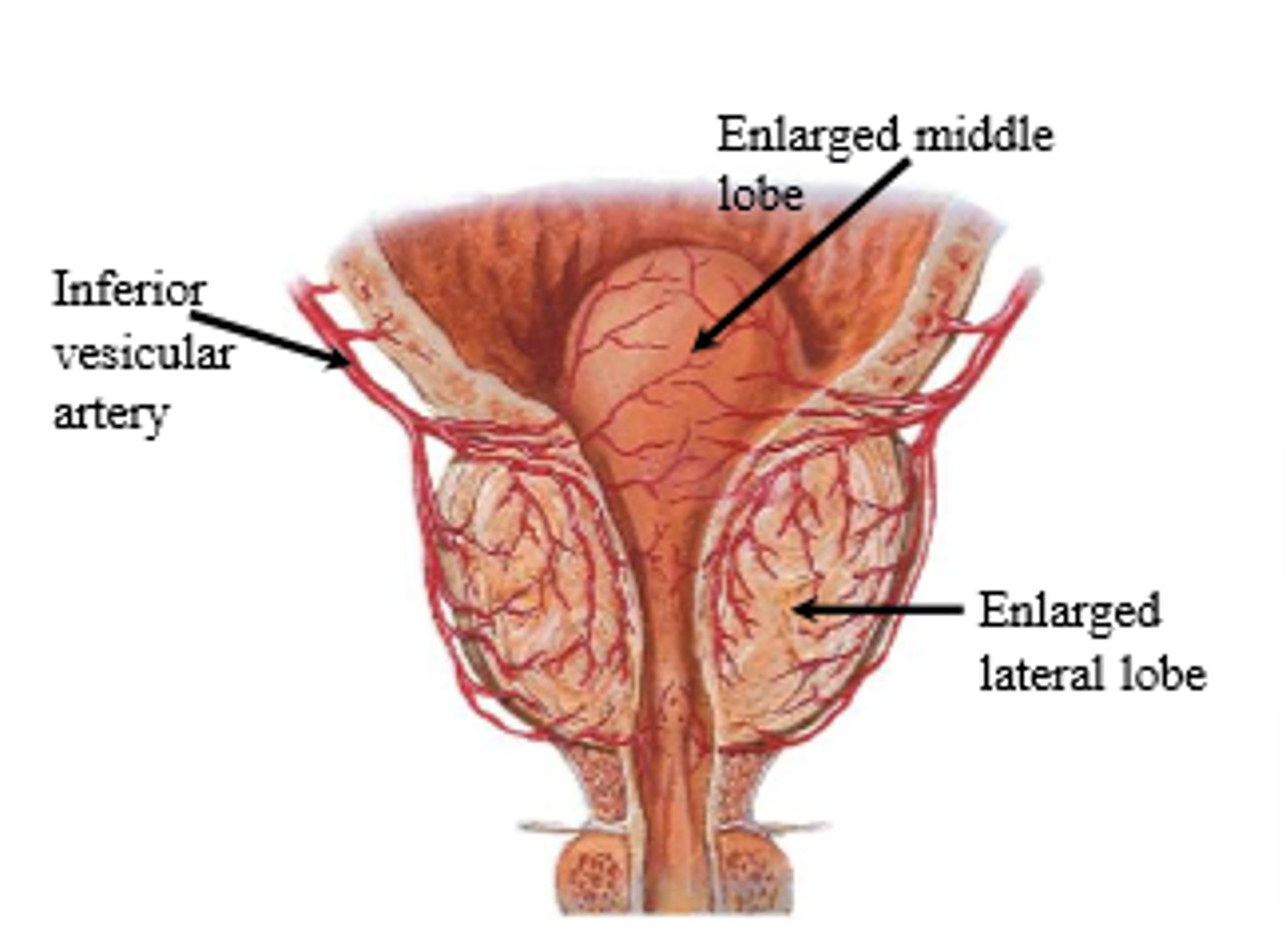
Prostate
-Right and left lobes are separated posteriorly by a longitudinal furrow.
-The middle lobe (embryonic) is subject to hypertrophy.
-2/3 of prostate = glandular
-1/3 = fibromuscular
Benign prostatic hyperplasia
benign growth of cells within the prostate gland
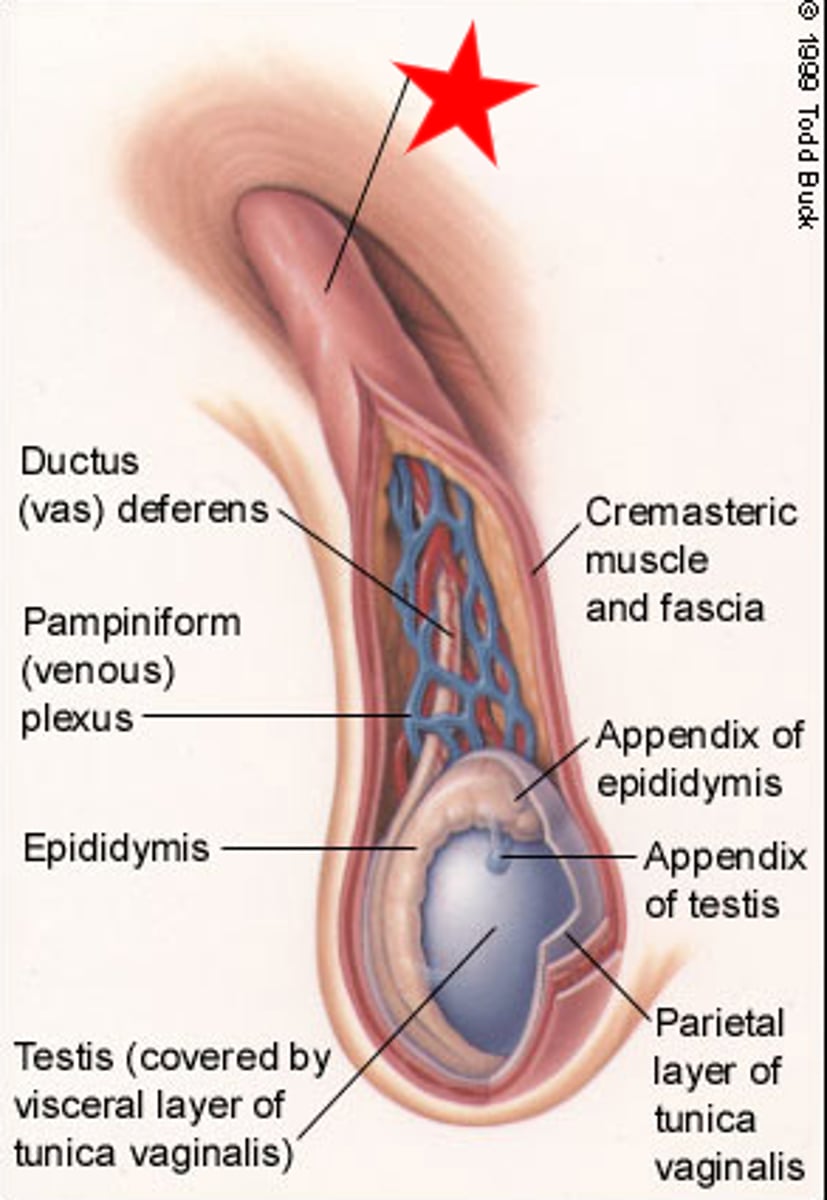
Spermatic cord
bundle of fibrous connective tissue containing the
-Ductus deferens
-Testicular artery
-Artery of ductus deferens
-Pampiniform venous plexus
-Sympathetic fibers (testicular plexus)
-Genital branch of genitofemoral nerve
-Testicular lymphatics
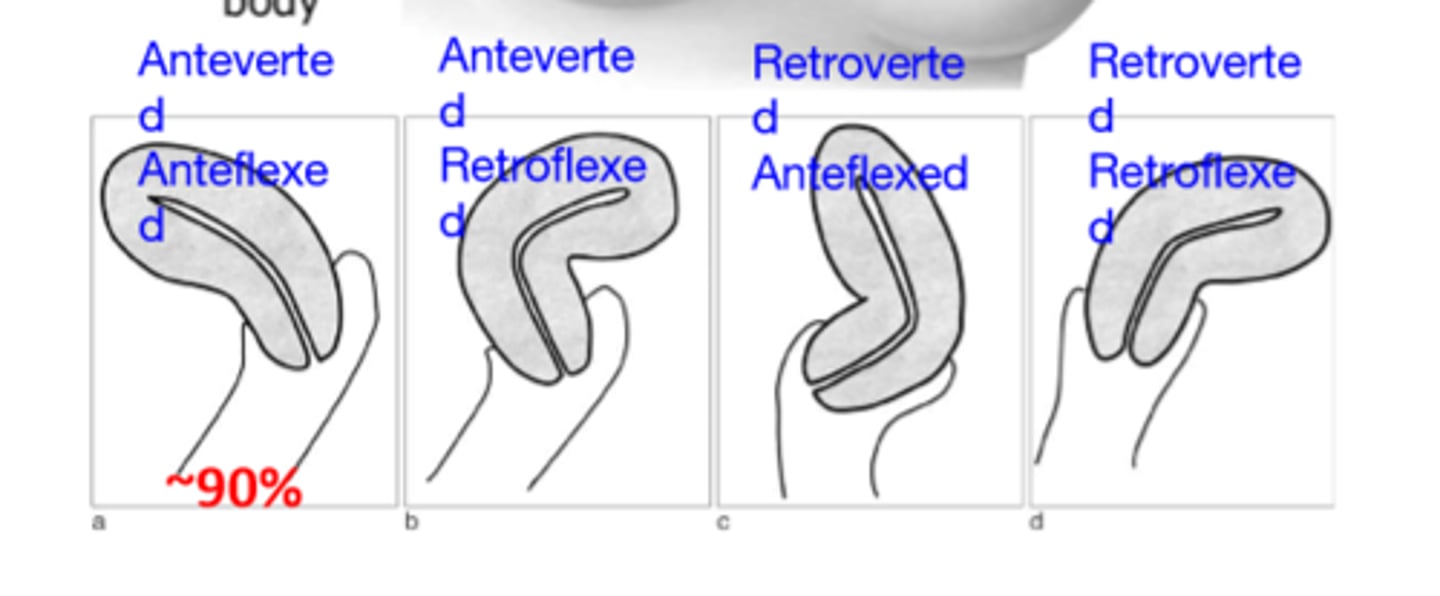
What are the different uterine positions, and which is most common?
Uterine positions include:
-anteverted and anteflexed (most common, ~90%)
-retroverted and anteflexed
-anteverted and retroflexed
-retroverted and retroflexed.
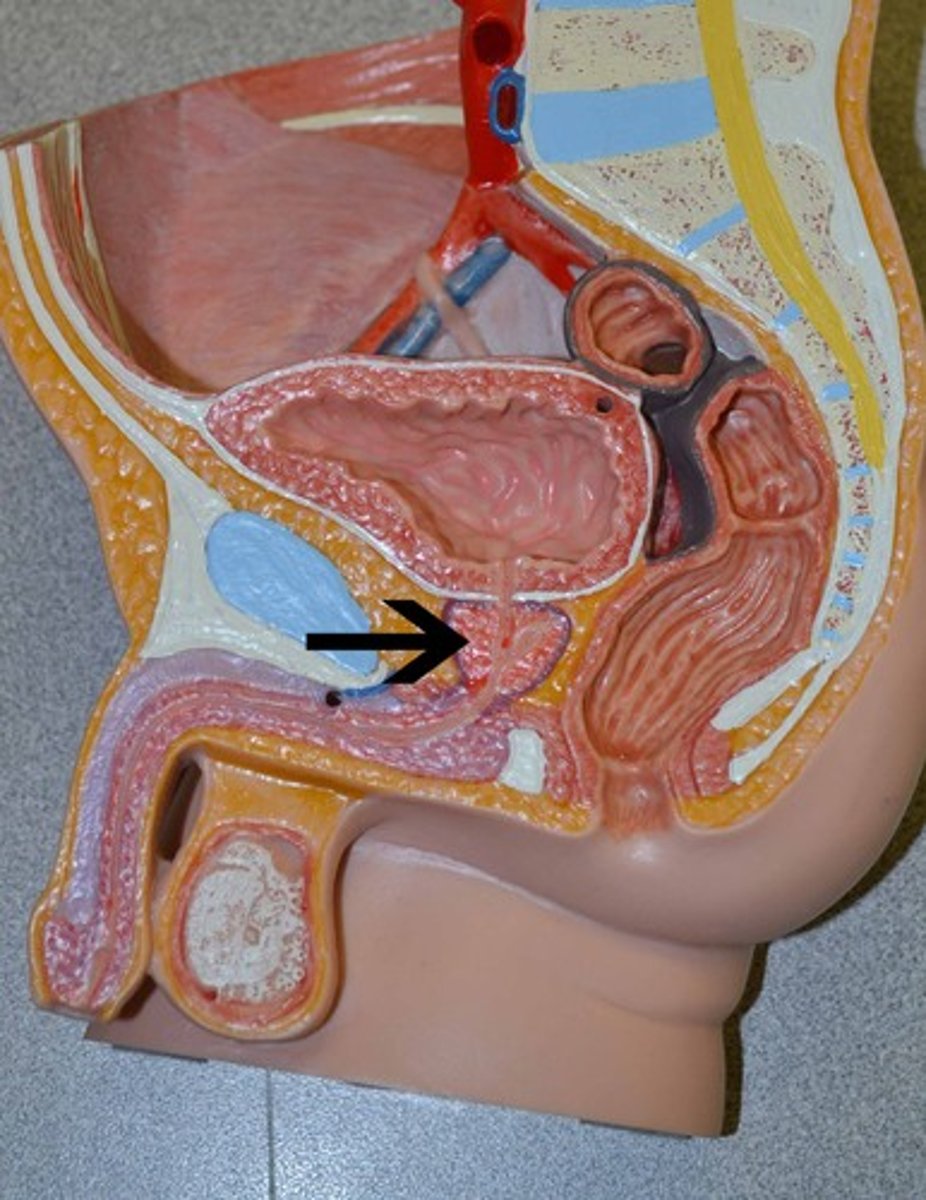
Know the anatomical relationship between the bladder and rectum.
In males: Bladder is directly anterior to the rectum, separated by the rectovesical pouch.
In females: Bladder is anterior to the uterus and vagina, which lie between the bladder and rectum, with the rectouterine pouch separating the uterus from the rectum.
Be able to trace the pathway for sperm from testis to urethra
1. Testis (seminiferous tubules) →
2. Efferent Ductules →
3. Epididymis (head, body, tail) →
4. Vas Deferens →
5. Ampulla of Vas Deferens →
6. Ejaculatory Duct →
7. Prostatic Urethra →
8. Membranous Urethra →
9. Penile Urethra →
10. External Urethral Orifice (ejaculation).
How does the ductus deferens travel relative to the ureter?
The crossing over of the ductus deferens and ureter happens near the posterior aspect of the bladder, just before the ductus deferens terminates at the ejaculatory duct within the prostate gland.
Where are the seminal vesicles (glands) located? How do they relate to the ejaculatory duct?
-The seminal vesicles are located posterior to the bladder and lateral to the ductus deferens.
-Each seminal vesicle combines with the ductus deferens to form the ejaculatory duct, which then passes through the prostate and opens into the prostatic urethra. These glands are essential for producing a significant portion of the seminal fluid.
Where do the ejaculatory ducts drain?
The ejaculatory ducts drain into the prostatic urethra, where their contents mix with prostatic secretions, contributing to the formation of semen that is then ejaculated.
Describe the anatomy of the prostate gland. Which lobe most often obstructs the prostatic urethra in benign prostatic hypertrophy?
-Anterior lobe: Located anterior to the urethra; mainly fibromuscular tissue.
-Posterior lobe: Posterior to the urethra and below the ejaculatory ducts; most commonly associated with prostate cancer.
-Lateral lobes (right and left): Form the bulk of the gland on either side of the urethra.
-Median (middle) lobe: Situated between the urethra and ejaculatory ducts, posterior to the bladder.
-The transitional zone of the prostate, particularly the median lobe, most often obstructs the prostatic urethra in cases of benign prostatic hyperplasia (BPH).
Outline the regions of the uterine tube. Where does fertilization usually occur?
Infundibulum:
The funnel-shaped opening near the ovary.
Contains finger-like projections called fimbriae that help to catch the ovulated egg.
Ampulla:
The widest and longest portion of the uterine tube.
This is the most common site for fertilization to occur.
Isthmus:
A narrow section connecting the ampulla to the uterus.
This region has a thicker muscular wall and helps transport the fertilized egg to the uterus.
Interstitial (or Intramural) Portion:
The segment that passes through the uterine wall and connects the uterine tube to the uterus.
This part is embedded within the uterine tissue.
-Fertilization usually occurs in the ampulla