Neurological Disorders Associated with Cognitive Impairment
1/183
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
184 Terms
Neurological Model of (oral) communication: Four ordered steps or levels in their neurological model of oral communication.
-ideation
-symbolization
-translation
-execution
Neurological Model of (oral) communication: Ideation
when the concepts we wish to express are generated
Neurological Model of (oral) communication: impairment at the ideation level will result in what?
mental-verbal dysfunction (or mental confusion, dementia, DOC, delirium)
Neurological Model of (oral) communication: Symbolization
when these concepts are put into a symbolic system congruent with the rules of the speaker's language;
Neurological Model of (oral) communication: Impairment at the level of symbolization will result in what?
aphasia
Neurological Model of (oral) communication: Translation
when these linguistic units or symbols are translated into neuromotor commands that result in the innervation of the motor nerves.
Neurological Model of (oral) communication: Impairment at the level of translation with result in what?
apraxia of speech (AOS)
Neurological Model of (oral) communication: Execution
the actual movements of the speech mechanism.
Neurological Model of (oral) communication: Impairment at the level of execution will result in what?
dysarthria
Frontal lobe functions of cognition
-reasoning
-planning
-language
-long-term memory
-impulse control
-problem solving
-emotions
-judgement
-motor function
-initiation
-social/sexual behavior
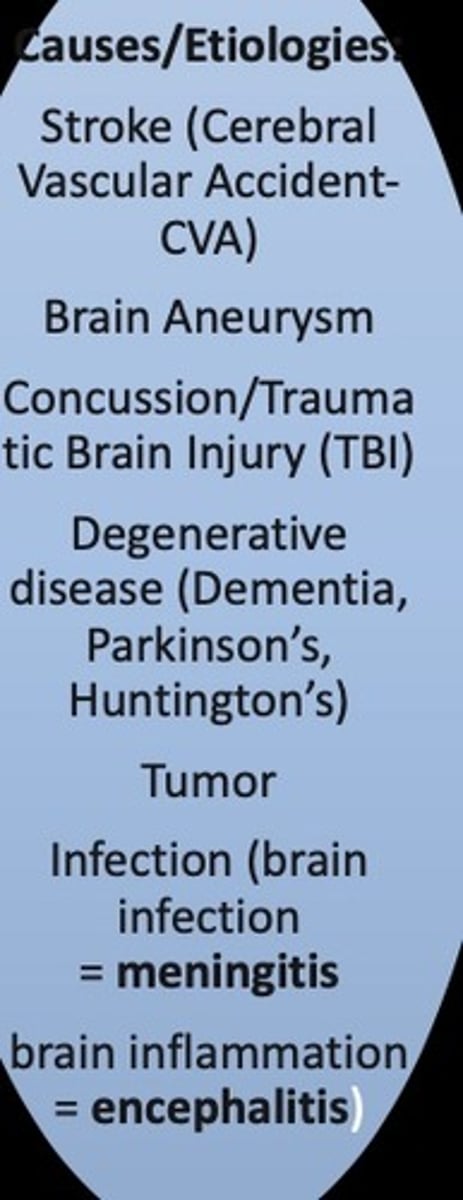
Neurological disorders associated with cognitive impairments
-ABI
-Degenerative conditions
-Others: MS, depression, delirium, and more
ABI
An acquired brain injury (ABI) is an injury to the brain that is not hereditary, congenital, degenerative, or induced by birth trauma. Essentially, this type of brain injury is one that has occurred after birth.
-The injury results in a change to the brain’s neuronal activity, which affects the physical integrity, metabolic activity, or functional ability of nerve cells in the brain. An acquired brain injury is the umbrella term for all brain injuries.
Two main categories of ABI
-traumatic- injury caused by external force
-non-traumatic- injury not caused by external force
ABI: TBI/mTBI
concussion (falls, car accident, injury/trauma)
Traumatic ABI causes
falls, assaults, MVA, sports and rec, AHT/SBS, GSW, work- related, physical abuse/violence, military actions
Traumatic ABI: 2 primary mechanisms
Impact and inertia ( coup/contra-coup)
Coup-contra-coup
Coup (initial injury)-contra-coup (brain bouncing back) : acceleration deceleration injuries (common to have frontal and occipital; or both temporal). A pattern of injury
3 major neurological causes of death and disability
-TBI
-Dementia
-CVA
Traumatic ABI: 2 subcategories
open (penetrating) and closed (non- penetrating) head injuries
Non-traumatic ABI causes
-CVA (ischemic/embolic or hemorrhagic)
-Infectious disease
-Seizure disorders
-Electric shock
-Tumors
-Metabolic disorders (insulin shock, kidney function)
-Anoxia (near-drowning, strangulation, choking, heart attack)
-Toxins (carbon monoxide poisoning)
Three primary dimensions of injury/event/diagnosis of ABI
1. the distribution (how much of the brain was affected): focal lesions, multifocal lesions, and diffuse brain injury
2. severity
3. type of underlying pathology (cause)
Focal lesions
stroke, tumors, brain abscesses, focal trauma/penetrating injury (GSW)
Multifocal lesions
multiple, distributed occurrence, such as in MID (multiple strokes) or TBI
Diffuse brain injury
rotational OR diffuse axonal injury (DAI) TBI, hypoxia, metabolic or infectious brain issues
Types of underlying pathology for ABI
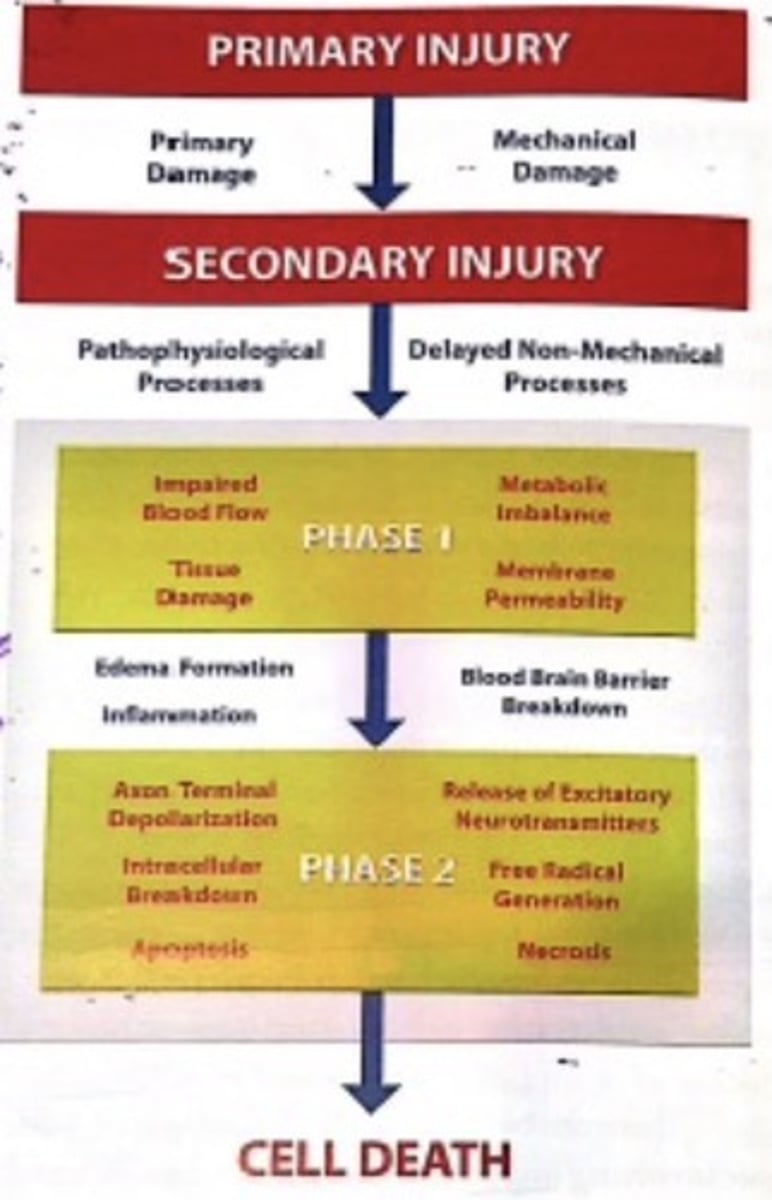
primary injury and secondary injury
Primary injury
• Primary damage
• Mechanical damage
Secondary injury
what occurred right after?
• Cascade of physiological events
• Delayed non-mechanical processes (metabolic changes, cell loss, etc)
-might not occur until weeks after primary injury
Process of primary and secondary injury
through slow breakdown of brain cells, and ultimate cell death
Consequences of ABI
-physical (include sleep)
-cognitive (include communication)
-emotional and behavioral
-ALl affected by how widespread damage is and what is the site of lesions (area of brain sustaining the damage)
Common symptoms of ABI: physical
-dizziness and balance issues
-weakness (paresis, paralysis)
-nausea, vomiting, vertigo
-headaches
-changes in vision and visual processing
-changes in hearing and auditory processing
-sleep disturbances
-fatigue
-seizures
-sensory issues (sound and light sensitivity, issues with taste, smell, and touch)
Common symptoms of ABI: Cognitive
-Feeling dazed or in fog
-Disorientation
-Confusion
-Difficulty concentrating
-Slowed information processing
-Difficulty learning new information
-Difficulty with memory
-Difficulty juggling multiple tasks
-Executive functions
-Difficulty with
Impulsive
-Task initiation
Common symptoms of ABI: communicative
-Difficulty understanding or producing language (aphasia)
-Slurred, weak, spastic, uncoordinated execution of speech
(dysarthria)
-Difficulty with motor programming of speech (apraxia)
-Reading fluency and/or comprehension
Writing formulation, spelling
-Social communication (turn taking, maintaining conversational
topics)
-Communicating in "socially unacceptable" ways (pragmatics)
Common symptoms of ABI: emotional/behavioral
• Irritability
• Quick to anger
•Decreased motivation
• Anxiety
• Depression
• Social withdrawal
• Does not get the"gist"of social interactions
• May comment on or react to things that seem random to others
• Behavioral changes
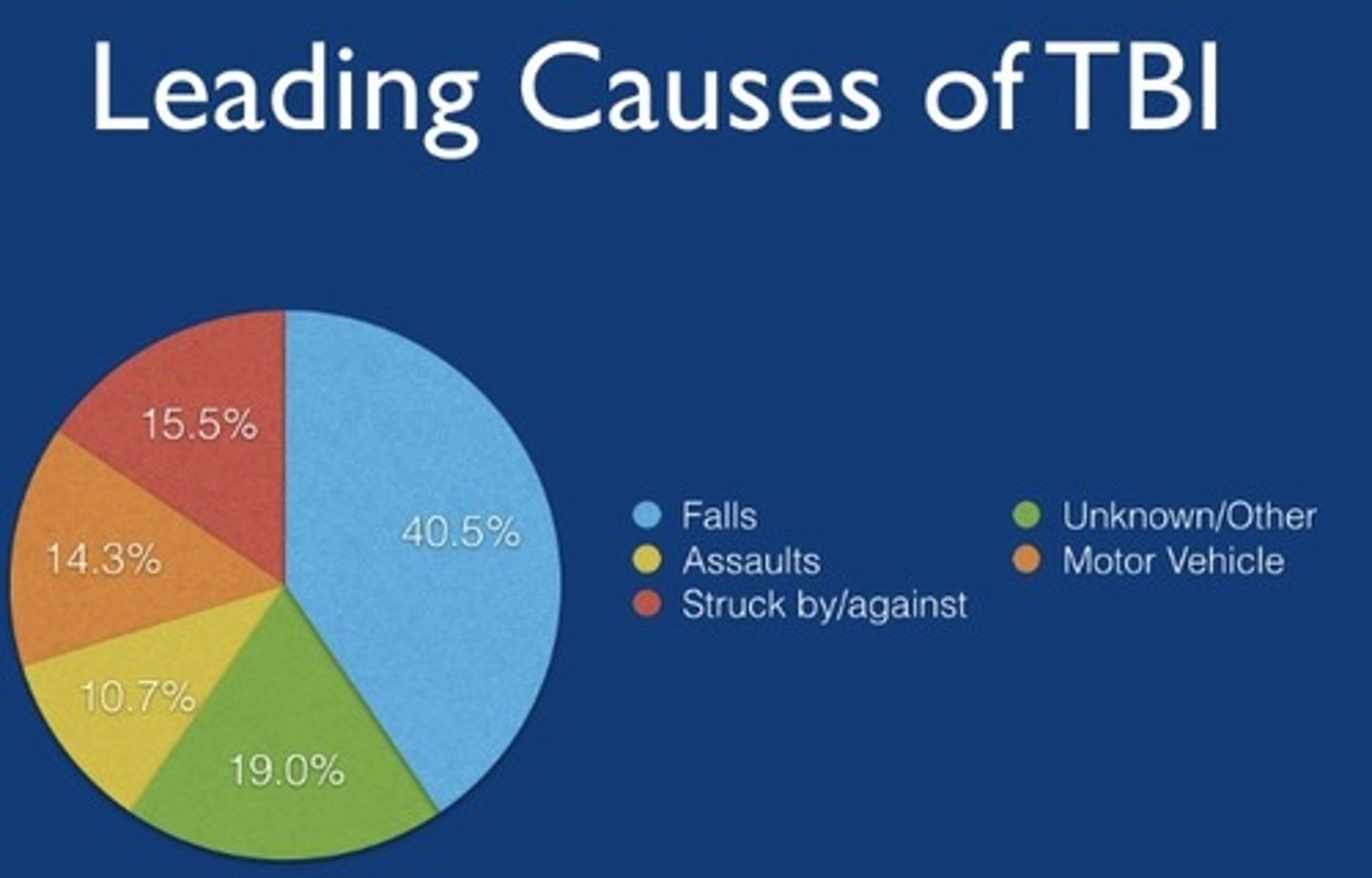
The leading causes of TBI based on the centers for disease control and prevention
• falls
• motor vehicle and pedestrian- related accidents
• collision-related (being struck by or against) events
• violent assaults
• Sport-related injuries and explosive blasts/military combat injuries (unknown/other)
The incidence of TBI refers to what?
the number of new cases identified in a specific time period.
-mild TBI or concussion every 21 secs.
The prevalence of TBI regers to what?
the number of individuals who are living with TBI and related deficits within a given time period
-about 13.5 million
Once an individual sustains a TBI, he/she is..
-3x more likely to have a 2nd injury and
-8x more likely to have a 3rd injury
Gender differences for TBI
TBI is more common in males and higher rates of death, but females have a worser outcome for recover
TBI due to impact
-closed injuries
-lacerations, contusions (bruises) or intracerebral hemorrhage to the brain (focal injuries)
-open injuries
TBI: Lacerations, contusions (bruises) or intracerebral hemorrhage to the brain (focal injuries)
• Can include coup-contre-coup injuries (initial blow/event, subsequent blow/event)
• Can include Diffuse Axonal Injuries (DAI) (more diffuse damage due to a shearing of axons)
Open injuries (TBI)
• Breach of meninges or skull
• Result in focal injuries (hematomas or hemorrhage)
TBI due to inertia
-non-impact injuries
-result from acceleration-deceleration forces
-can also result in coup-contre-coup injury
-can result in DAI injury
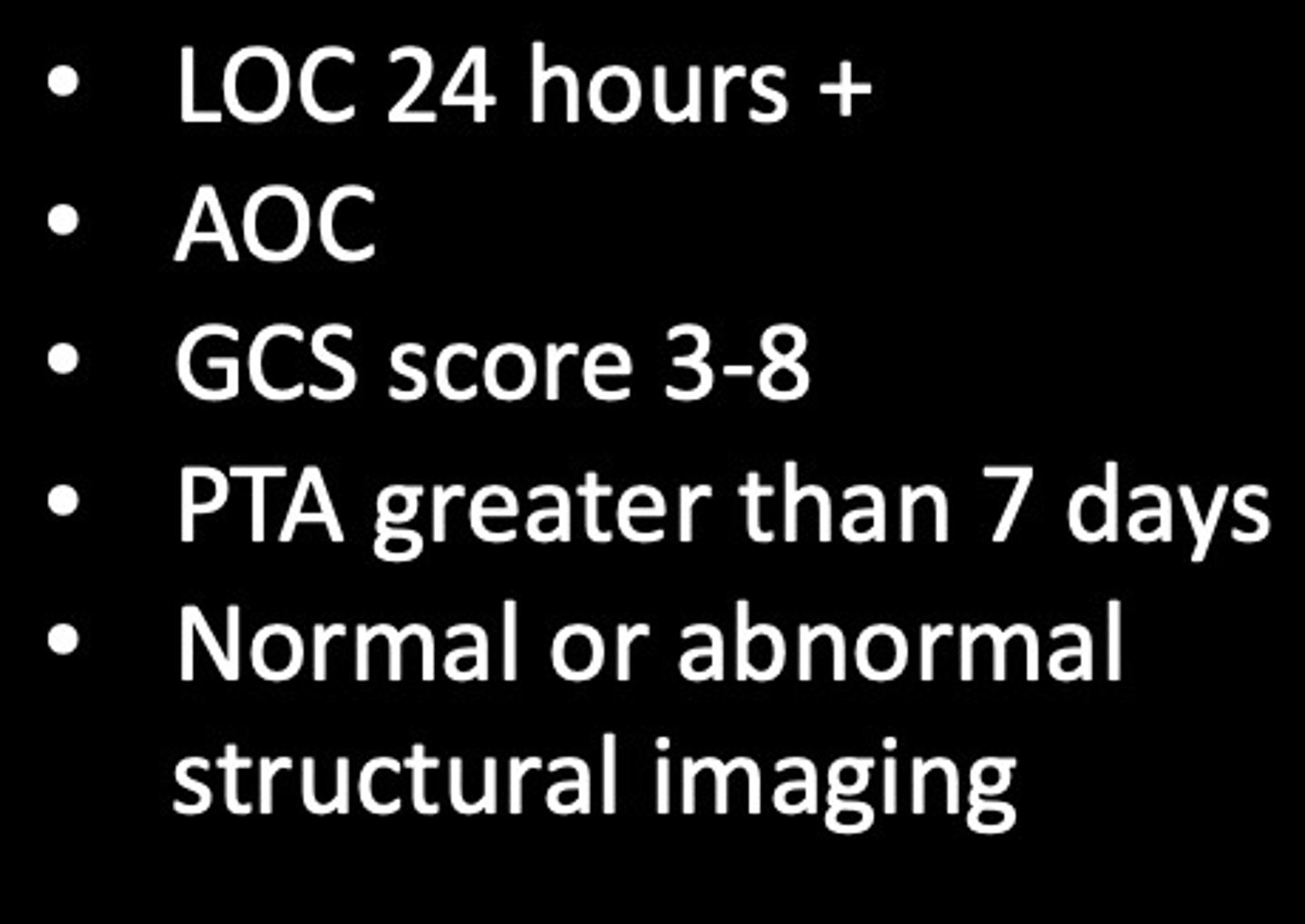
LOC
loss of consciousness
AOC
alteration of consciousness
PTA
post traumatic amnesia
GCS
Glasgow Coma Scale
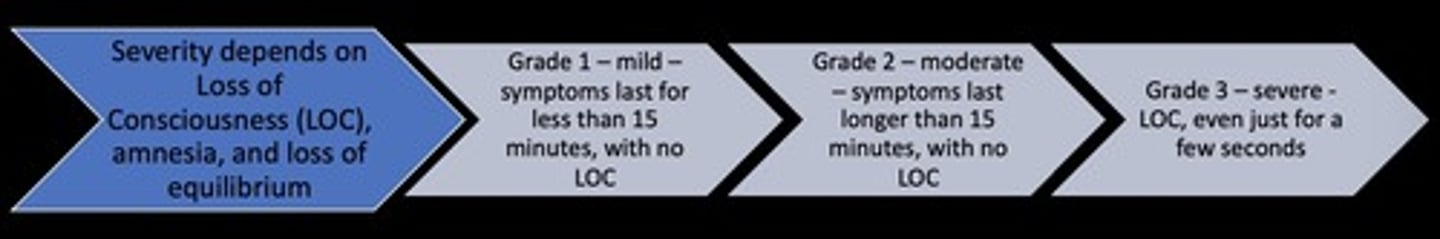
3 levels of severity of TBI
mild, moderate, and severe
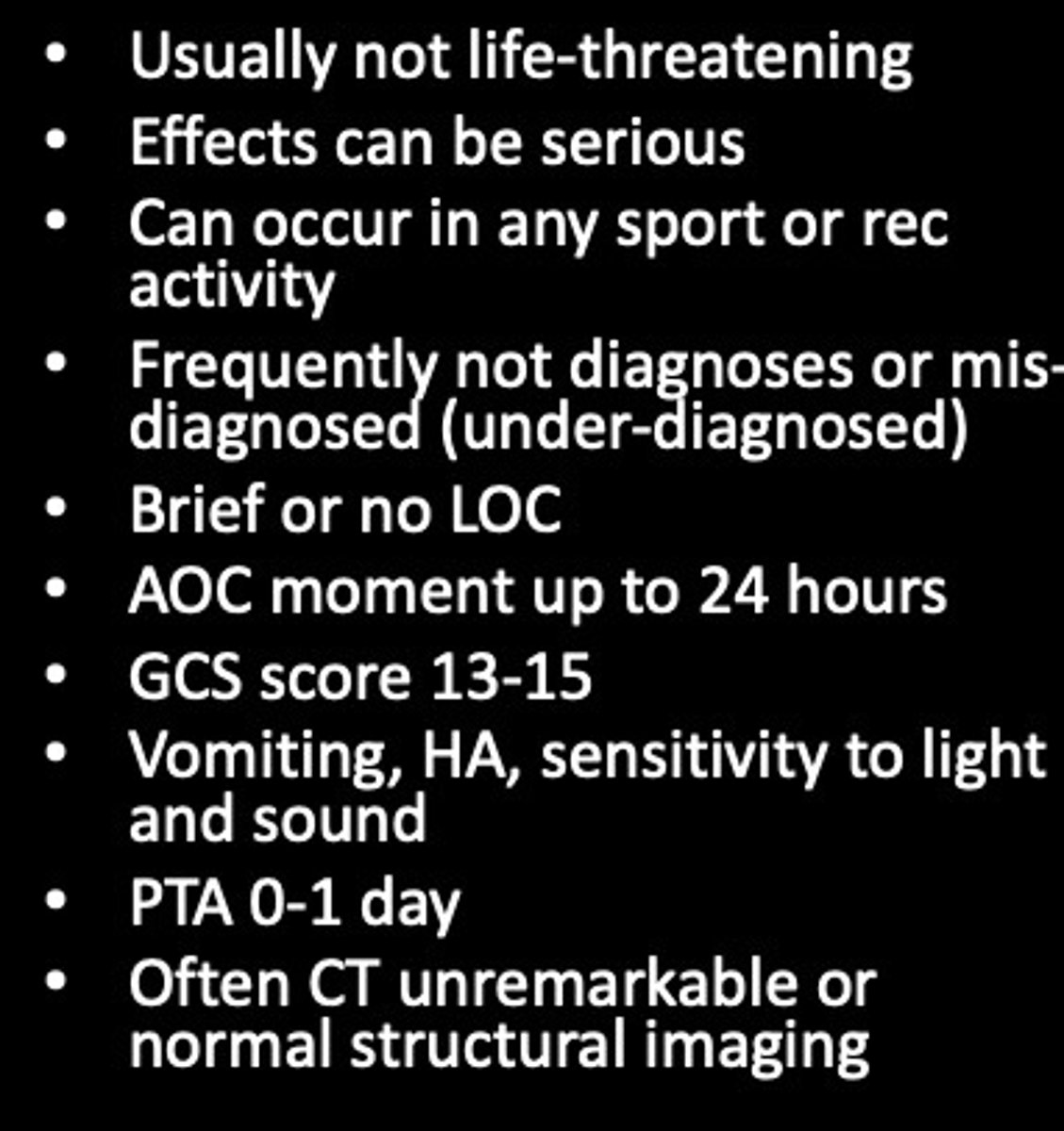
Mild -mTBI or concussion
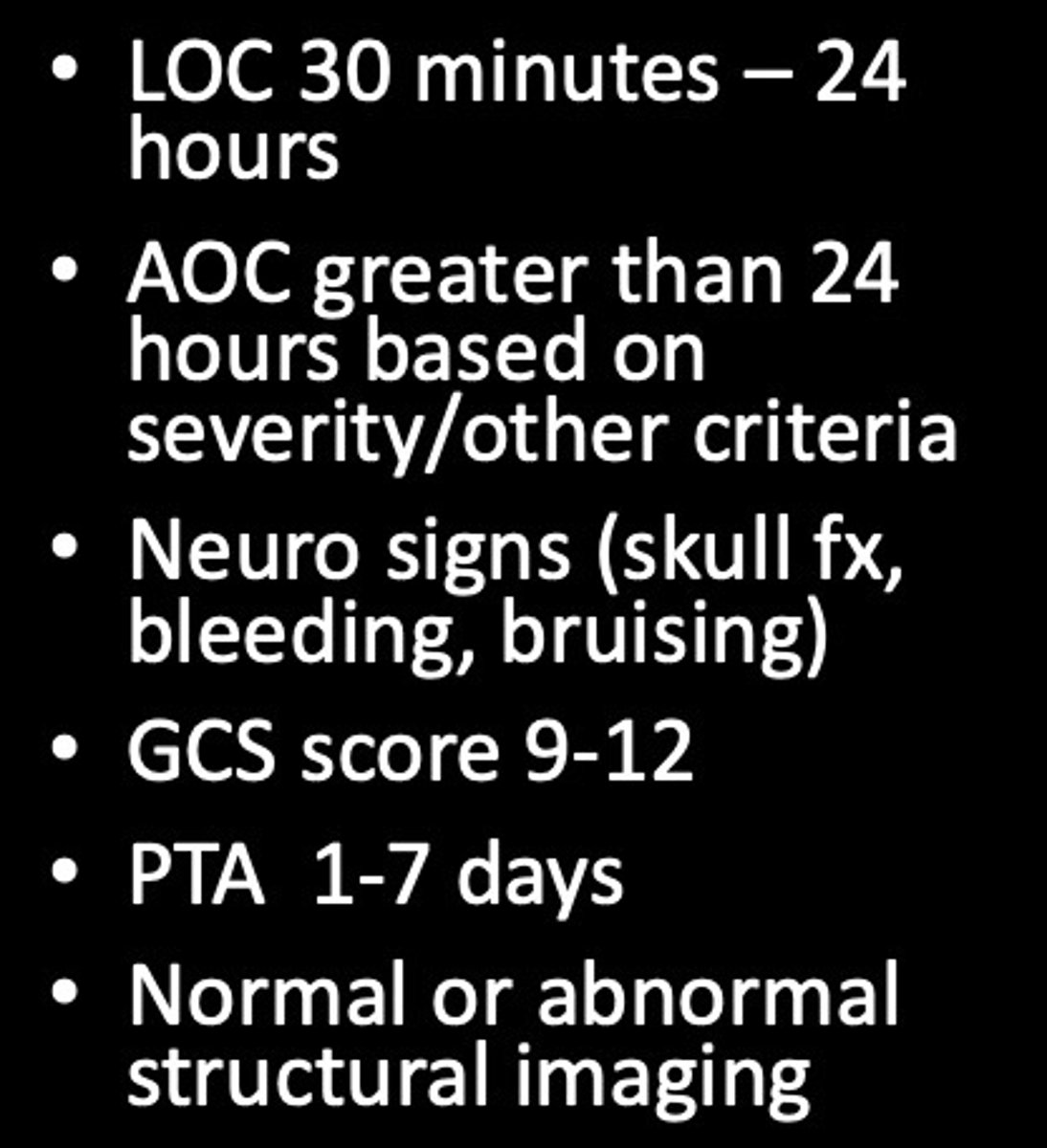
Moderate TBI
Severe TBI
Even though mTBI is classified as a "mild" TBI,...
it can be considered also by severity as a concussion
mTBI - grades: severity of LOC
CVA
-stroke or cerebrovascular accident used interchangeably
-one of the 3 major causes of death and disability
-hemorrhage or bleed
-ischemic/embolic
tPA
clot busting medications (reduce total injury of stroke)
Strokes affectingMCA
-Left: aphasia, AOS, verbal learning impairments
-Right: visual spatial impairments, nonverbal learning impairments, impaired awareness of deficits, pragmatics, attention
Strokes affecting PCA
relatively rare, bilateral thalamic strokes can result in very severe deficits of attention, MEMORY, apathy, flat affect confabulation, amnesia) (occipital and temporal lobes)
Aneurysm effects
confabulation, disinhibition, amnesia, executive function impairments, limited awareness
Glasgow Coma Scale (GCS)
tool to assess impairment of conscious level in response to defined stimuli - used in acute care settings
Ranchos Los Amigos - Revised
Levels of Cognitive Functioning
tool
tool to assess impairment of conscious level in response to defined stimuli - used in acute care settings
-levels 1-10 (1 being the worst and 10 being the best)
What are Disorders of Consciousness D0C?
A state where consciousness of the brain has been affected caused by an acquired brain injury.
-DoC are the first 3 levels of the Ranchos Los Amigos Scale—Coma, unresponsive wakefulness (UWS), and minimally conscious state (MCS).
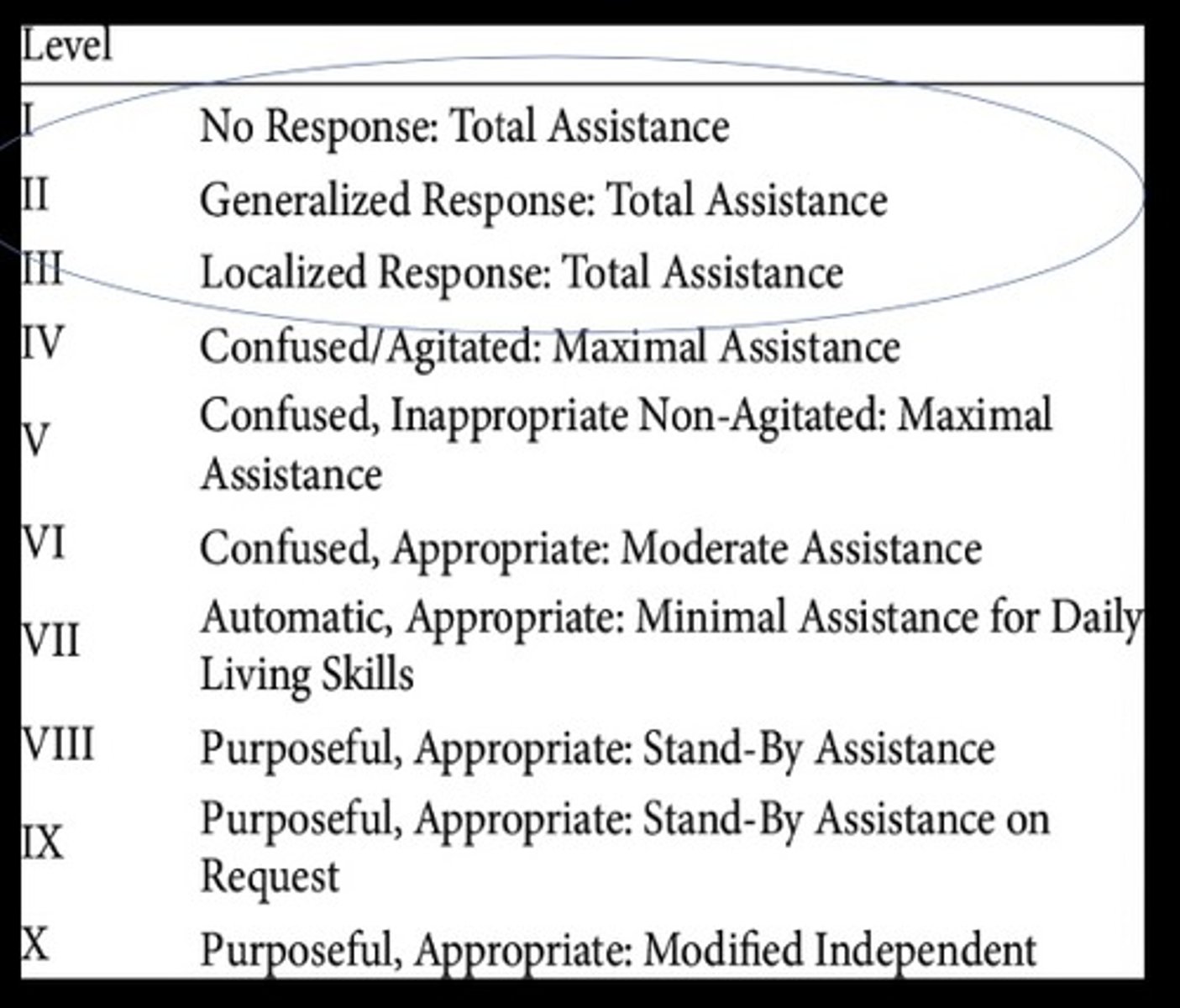
DOC I
coma
-arousal: no
-awareness: no
DOC II
unresponsive wakefulness (UWS)
-arousal: yes
-awareness: no
Doc III
minimally conscious state (MCS)
-arousal: yes
-awareness: fluctuates
Coma
• unconscious
• neither awake or asleep
• Absence of eye opening
• Absence of verbal or motor responses
• Prolonged coma is rare
• usually resolves in 2 weeks
Coma prognosis
• After 3 days, if a patient will has no pupillary or
corneal reflexes there is a negative prognosis
• After 3 days, if the patient has an absent response to noxious stimuli, that is a negative prognosis
• Traumatic brain injuries have a better prognosis than an anoxic brain injury.
Awareness is regulated by
higher cortical areas of the brain
Unresponsive wakefulness (UWS)
-spontaneous eye opening or in response to stimuli
-formally known as "vegetative state"
-only show reflexive behavior
-preserved automatic functions
-absence of awareness
-no evidence of sustained reproducible behavioral responses to visual, auditory, tactile or noxious stimuli
-no evidence of language comp./expression
-intermittent wakefulness manifested by th evidence of sleep wake cycles
Unresponsive wakefulness (UWS) prognosis
• Often results from an injury to the thalamus
• Considered permanent (chronic) after 1 year of a traumatic event and 3 months after a non-traumatic etiology
• Fun Fact: The term vegetative state was coined in 1972. Before 1990, only 43 research studies had been completed on the vegetative state
Minimally Conscious State (MCS)
-signs of consciousness are difficult to detect because they are inconsistent and fluctuate
-patients can fluctuate between vegetative state and minimally conscious state before it stabilizes
-unable to follow simple commands, inaccurate gestural/verbal responses, intelligible verbalization, movement in relation to environmental stimuli that are not reflexive
Minimally Conscious State (MCS) prognosis
-Formal prognostics do not exist
Recovery is more favorable in those that have traumatic injuries
-20% of patients in a minimally conscious state will eventually continue to live in the community
-Recovery within 8 weeks are linked to a good functional recovery
-The earlier this behavior appears, the better the outcome
-Patients in a minimally conscious state have a more favorable outcome than a vegetative state
Emergence from DOC
1. Functional Communication as evidenced by verbal or gestural yes/no response
2. Functional use of 2 or more objects (hairbrush, cup)
Medical Management of DOC

Why is DoC Rehabilitation important?
-Patients with DoC can often be misdiagnosed in the stages of coma, UWS, and MCS
-You will see this a lot if you are working with this population
Right hemisphere dysfunction (RHD)
-distribution: usually focal lesion, can be others, less common
-severity- mild to severe
-type of underlying pathology: usually stroke, but others less common
Right hemisphere dysfunction (RHD) conditions
A range of possible conditions (any brain injury) that can cause damage to the right cerebral hemisphere
Right Hemisphere Dysfunction (RHD): characteristics
-attention and pragmatics are mostly impacted.
-language technically intact, but person seems different
-may experience left neglect (vision not acknowledging left side and not aware of the neglect; recovery is variable) or other vision problems
Does visual neglect have intact cognition
to an extent but not because attention is impacted (visuospatial skills)
Dementia (distribution, severity, underlying pathology)
-Distribution: multifocal lesions (MID), or diffuse
-Severity: mild to severe
-Underlying pathology: unknown
Dementia
A general term describing progressive deterioration of memory, intellectual ability, orientation, and behavioral appropriateness, physical skills. Repeated damage or injury to the brain can increase risk of dementia.
Similarities between ABI and dementia
•Both vary from mild to severe
•Both also may result in changes in emotion and personality
Mild cognitive impairment
is noticeable but is not effecting everyday life in a major way
Types of cortical dementias
-Alzheimer's disease
-Vascular dementias (VaD)
-Frontotemporal Dementias (FTD)
Cortical dementia
it is roughly true that the earliest symptoms is "cortical" dementia include difficulty with high-level behaviors such as memory, language, problem-solving, and reasoning
Alzheimer's Disease (AD
•most common - 60-70% of all cases
•(most common type; plaques and tangles throughout the brain)
Vascular Dementias (VaD)
•2nd most common next to AD of all cases (vascular - lack of bloodflow, multiple strokes, such as Multi-infarct dementia and Binswanger's)
Frontotemporal Dementias (FTD)
•Pick's disease, Primary Progressive Aphasia (PPA)*MOST CASES*, Progressive Supranuclear Palsy (PSP), Mild Cognitive Impairment (MCI)
subcortical
deeper area of the brain
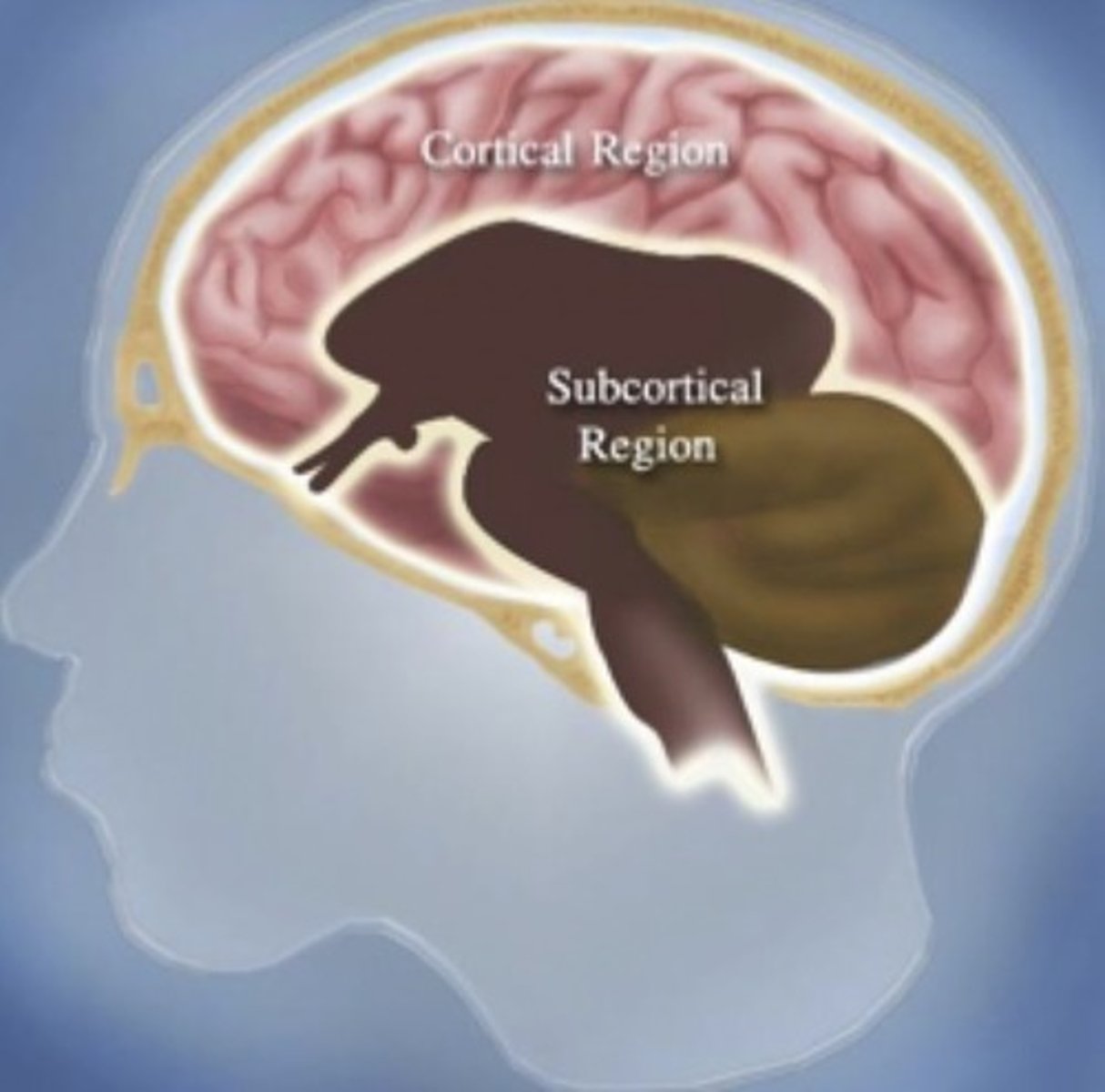
Subcortical Dementias
affecting areas of the brain beneath the cerebral cortex
-subcortical dementia
-dementia with Lewy Bodies (DLB)
subcortical dementia
is more likely to affect attention, motivation and emotionality. People with subcortical dementia often show early symptoms of depression, clumsiness, irritability or apathy. Eventually, they will also show sx of memory, problem solving and the end result is the same as the cortical dementias.
Dementia with Lewy Bodies (DLB)
•(lewy bodies are abnormal proteins found in nerve cells),
-Parkinson's Disease (PD)- 10-15%
-Huntington's Disease (HD)
-Human Immunodeficiency Virus: Dementia (HIV-D)
Mixed Dementias
-Creutzfeldt-Jakob
-Korsakoff's memory disorder
Creutzfeldt-Jakob
-rare
-fatal brain disorder resulting in failing memory, behavior changes, impaired coordination and/or visual disturbances; death within a year
-PRION disease
PRION disease
infectious protein that causes proteins to misfold leading to rapid degeneration of brain function (variant CJD is from Mad cow disease- not the same thing)
Korsakoff's memory disorder
caused by thiamine deficit- can look like dementia
-often due to chronic alcoholism but can also occur with prolonged vomiting, eating disorders and severe dietary deficiencies
Characteristics of dementia: cognitive
memory loss, mental decline, confusion in the evening hours (sundowning), disorientation, inability to speak or understand language, making things up, mental confusion, or inability to recognize common things
Characteristics of dementia: behavioral
irritability, personality changes, restlessness, lack of restraint, or wandering and getting lost
Characteristics of dementia: mood
anxiety, loneliness, mood swings, or nervousness
Characteristics of dementia: psychological
depression, hallucination, or paranoia
Characteristics of dementia: muscular
inability to combine muscle movements or unsteady walking
Characteristics of dementia: other
falling, jumbled speech, or sleep disorder