1. Infectious & parasitic skin diseases in dogs & cats. Otitis externa
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
What are infectious and parasitic causes of skin diseases in dogs and cats?
Bacterial
Primary
Secondary
Viral
Canine distemper
Canine papillomavirus
Pseudorabies
Feline cowpox
Fungal
Dermatophytosis
Malassezia pachydermatis
Parasitic
Mites
Lice
Ticks
Fleas
What are the causes for bacterial skin infections?
Secondary infection - must treat the underlying cause!
Pyoderma/break of skin - Superficial, surface or deep bacterial infection.
Immunosuppression - by disease or glucocorticoids
Young animals
Breed predisposition: Skin folds
1. Physical examination - look for alopecia, pruritus, type of lesion.
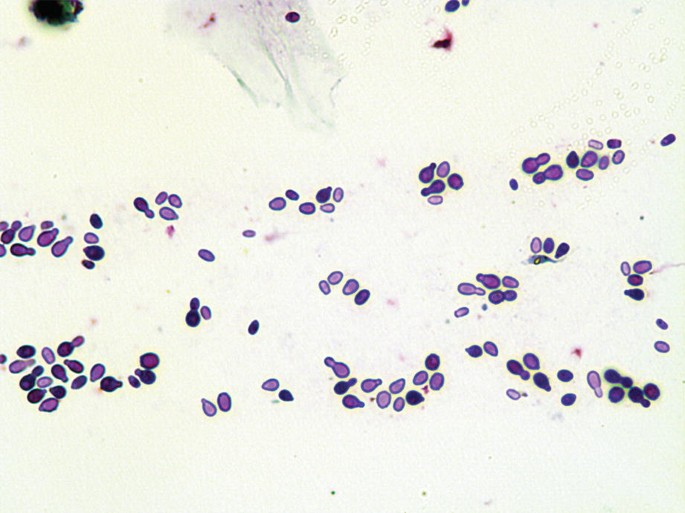
2. Cytologic examination - swab, sticky tape impression smear - Diff Quick
3. Skin scrapings (after sticky tape), cultivation, histopathology (last option)
Chlorhexidine wash (shampoos, gels, sprays)
Keep lesions dry
What are some viral causes of skin diseases?
Canine distemper
Canine papillomavirus
Pseudorabies
Feline cowpox
What is the treatment for canine distemper?
No specific treatment. Symptomatic, supportive. (interferon injections?)
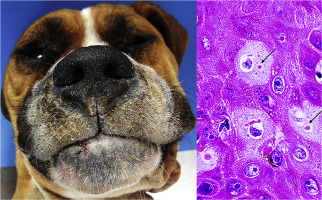
What is the causative agent of canine papillomatosis?
Canine papillomavirus-1 (DNA virus)

Spontaneous regression
Crushing (stimulates immune response to heal other growths)
Surgical removal (cauterisation, cryotherapy)


Mite detection in skin scrapings (deep or superficial)
What types of treatments are used for burrowing vs. non-burrowing mites?
Burrowing: systemic
Non-burrowing: topical
How are lice infestations treated?
Shampoo: lime sulphur, fipronil, ivermectin/permethrin also possible.
Local skin irritation, dermatitis, inflammation, swelling, ulceration, itching. Vectors of other diseases
What is the pathogenesis of FAD?
When feeding, fleas inject saliva that contains a variety of histamine-like compounds & enzymes that induce immune hypersensitivity & cause itching, erythema & papules
Intense pruritus, papulocrustous lesions on the lower back, tail head, posterior and inner thighs, restlessness, scratching, licking, rubbing, chewing, nibbling
Common secondary lesions include areas of alopecia, erythema, hyperpigmented skin, scaling, papules & broken papules covered w/ reddish brown crusts


Hypersensitivity
Immune-mediated
Cornification defects
Endocrine disorders
Foreign body, polyp, tumour.
Parasites
Bacterial infection (Staphylococcus, Pseudomonas, Proteus, Pasteurella)
Fungal/yeast overgrowth (Malassezia)
Seborrhoeic diseases → increased epidermal turnover rates → changes in otic glandular secretions → ceruminous otitis externa
Otodectes cynotis (ear mite)
Sarcoptes scabiei
Notoedres cati
Demodex canis/cati
Otobius megnini (ear tick)
What is the pathogenesis of Otodectes cynotis?
Local allergic reaction. Purulent inflammation & discharge of external ear, may perforate tympanic membrane
Massive, coffee-ground excretions in the ear canal without itching (sometimes severe pruritus).

How long should Otodectes cynotis infestations be treated?
Multiple times over 3-4 weeks to cover the whole life cycle (treatment does not affect eggs)
What are some treatment options for otitis externa?
Clean ears: ceruminolytic agents (cerumaural, dioctyl sodium succinate, carbamine peroxide). Irrigate ear with cleansing agent (warm water & isotonic/hypertonic saline)
Topical anti-inflammatory agent: corticosteroids (betamethasone, hydrocortisone)
Topical antibacterial agents: gentamicin, neomycin, enrofloxacin
Topical antifungal agents: imidazoles
Anti-parasitics: pyrethrin, ivermectin
Aminoglycoside antibiotics (neomycin, streptomycin), Macrolide antibiotics (erythromycin)
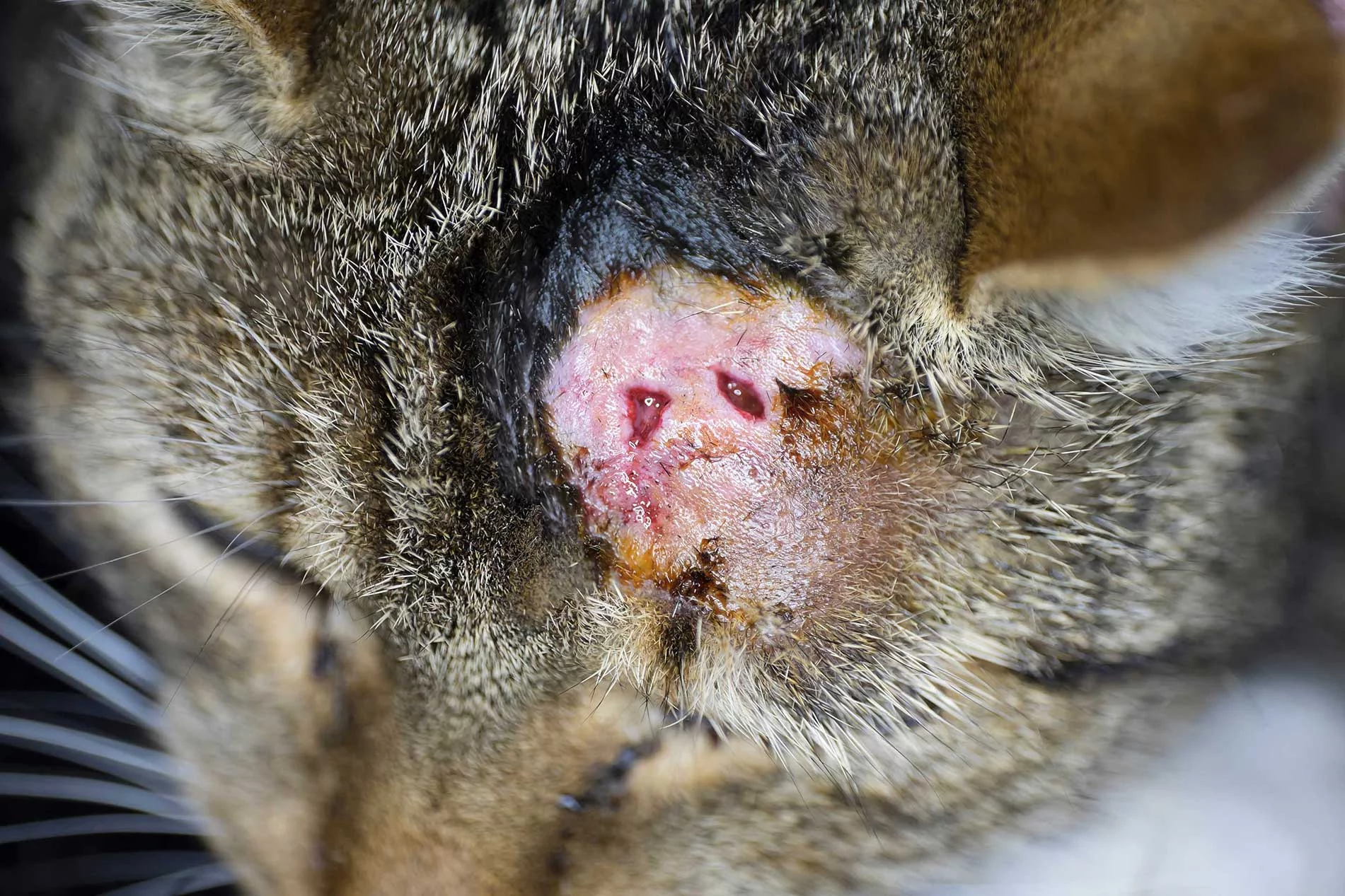
What is the difference between the clinical manifestations of sarcoptic mange and demodicosis?
Scabies is pruritic, demodicosis is not.
Does juvenile demodicosis need to be treated?
No. Self limiting as the immune system develops.
What is it called when Staphylococcus is resistant to ATB?
Methicillin-resistant
Why can corticosteroids be used in treatment of otitis externa?
To decrease irritation
What are the two skin manifestations of distemper?
Hard pad disease (nasal planum, paw pads)
Vesicles
Which skin manifestation of distemper can be associated with CNS disease?
Hard pad due to abnormal gait
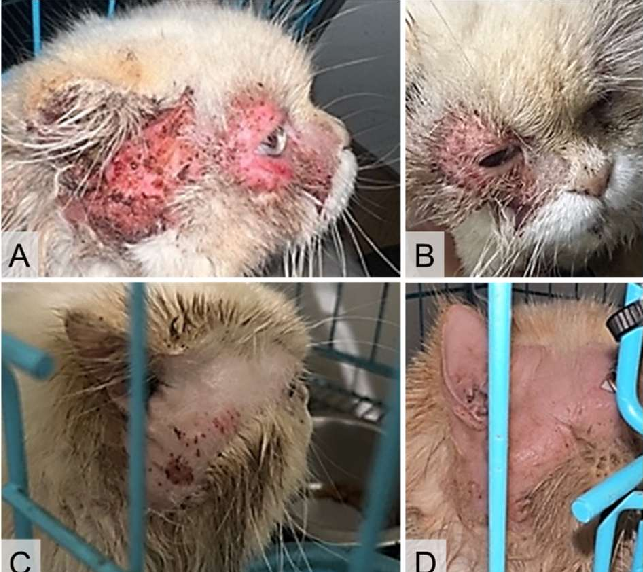
What are examples of skin manifestations involved in FIV?
Some cats with FIV develop nonpruritic, generalised, papulocrustous lesions with concurrent alopecia and scaling, which are most severe on the head and limbs.
Abscesses, skin and ear bacterial infections, and mycotic infections.