Special topics - Vision and FES
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
116 Terms
Where are the most refined muscles in the body?
The muscles of the eye are the most refined NM areas of the body – 1 nerve
to 6 muscle fibers in the eye (1:10 in the hand, 1:200 in the back)
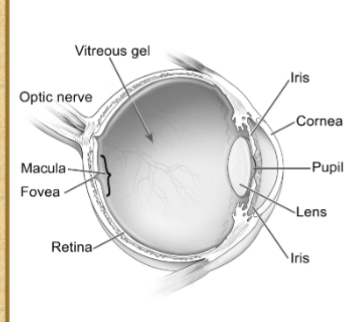
Functional Anatomy of the eye
Cornea
Lens
Iris
Vitreous gel
Retinal vessels
Retina
Optic nerve
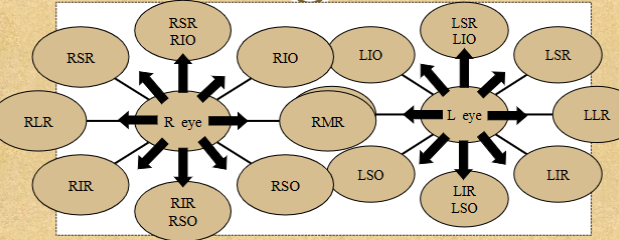
Extraocular eye muscles
Superior, inferior, lateral and medial rectus muscles and inferior, superior obliques
Allow movement in all directions of gaze and responsible for position of eye
Visual & Visual perceptual Skills (A whole list)
Acuity
Scanning, tracking/pursuits
Saccades
Visual fixation of gaze
Oculomotor control/alignment
Convergence/ Divergence (eye teaming/binocularity)
Visual attention
Depth perception
Figure ground (3)
Position in space/spatial relations
Visual discrimination – like/unlike, figure/object closure, color
Visual memory
Directionality – right/left, topographical, etc.
Contrast discrimination
‘Glare modulation’/recovery
Accommodation (3)
Awareness of visual fields
Concurrent processing of simultaneous visual stimuli – ambient vs. focal
List of Common pathologies of eye
Glaucoma
Cataracts
Macular
degeneration
Myopia
Hyperopia
Astigmatism
Diabetes/diabetic retinopathy
o Strabismus/Phoria
o CVA/TBI
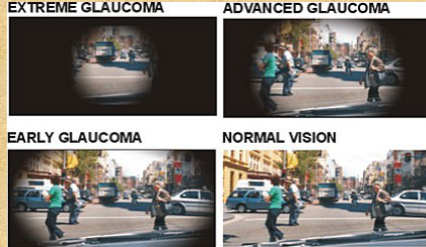
Glaucoma
increased intra-ocular pressure resulting in compression of optic nerve (producing ‘tunnel vision’).
If left untreated, can result in atrophy of optic nerve.
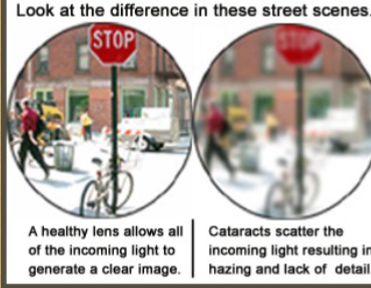
Cataracts
clouding of the lens. Decreases
acuity and contrast discrimination, however,
does not typically affect visual fields

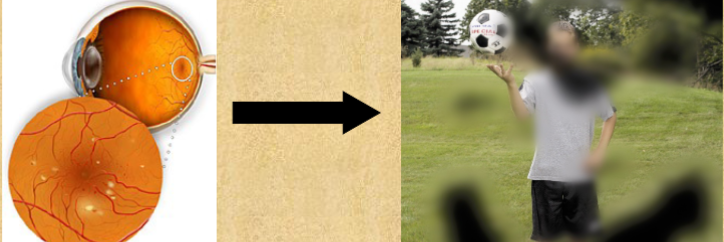
Macular Degeneration (ARMD)
– ‘wet’ vs. ‘dry’.
Degeneration of macula (portion of retina) due to
vascular changes, resulting in loss of central vision.
Myopia vs Hyperopia vs Astigmatism (Refractive errors)
Myopia – near sightedness (light rays pass through lens and are focused at a point in front of the retina)
Hyperopia – far sightedness (light rays pass through the lens and are focused at a point behind the retina)
Astigmatism - refractive error due to oval (rather than spherical) shape of eye.
What is a refeactive error?
relating to how the lens focuses the image) are treated with
corrective lenses (in therapy, this can be addressed by use of prescribed
lenses, magnification, enlarged print, changing focal distance, as well as
other interventions to maximize functional use of vision, including ensuring
adequate lighting, enhancing contrast, etc.).
Diabetic Retinopathy
Complication of diabetes. Retinal
vessels weaken, leaking blood and fluid into vitreous.
Glaucoma (pressure, creating restricted VF’s) cataracts
(clouding of the lens), retinal detachment, floaters and clouding
of the vitreous may occur.
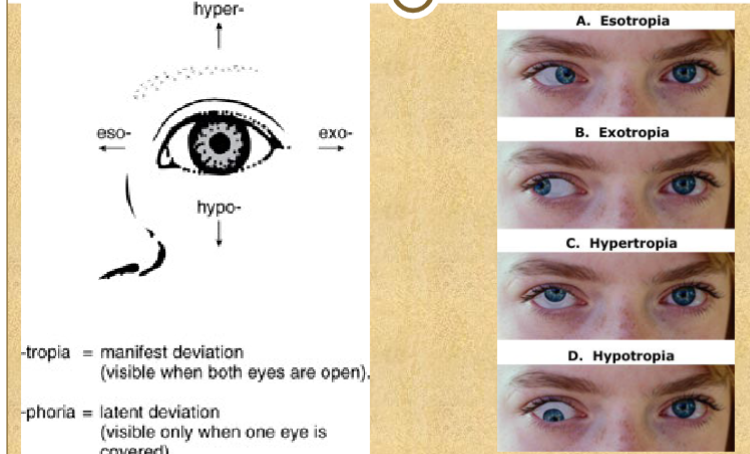
Strabismus/Phora
Misalignment of the eyes (may be
congenital, developmental or acquired). ‘Dysconjugate gaze’
Dependent upon degree of deviation, image(s) may
range from slightly ‘blurred’, to 2 distinct images
(‘diplopia’/double vision). Images may be
horizontally, vertically or diagonally displaced.
Common types of ocular deviation
Tropia - visible when both eyes are open
Phoria- visible when one eye is covered
Developmental considerations for vision
1.Prior to 3-4 years of age, standardized testing is typically not
administered due to developing visual perceptual skills, and
requisite cognitive/linguistic skills
Functional Changes to vision as we age
Color Sensitivity - discrimination of brightness decreases with age (most notably over 60 years), diminished ability to discriminate full spectrum (decline beginning at 30 years of age)
– most notable with similar shades/hues (i.e. pastels, navy/black/dark brown)
Visual/spatial abilities – decline in depth perception and spatial abilities beginning at age 40 and progressing
Glare recovery – decreased recovery from direct or reflected glare
4. Lighting/illumination – overall, increased illumination required
Transitioning light/dark – increased time to transition from light to dark and dark to light
Visual acuity – declines with age (typically optimal late teens/early 20’s), thought to be due to diminished corneal transparency or changes in vascular efficiency in the retina'
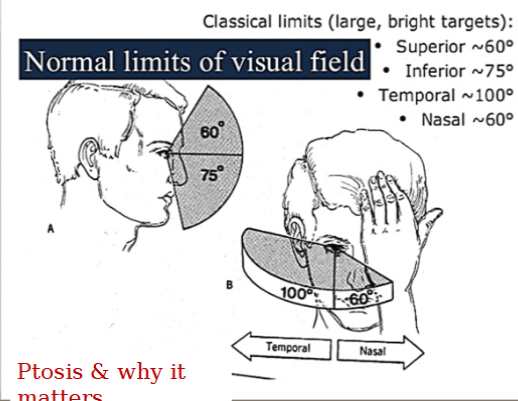
Visual fields – gradual narrowing of the visual field(s) until mid to late 50’s, more significantly during/after 60’s.
Visual Feild Screening Position
Position: Eye level, knee to knee (or within arm’s length)
• Present stimulus equal distance between you and
patient ... why??
• Finger count, static presentation (gross) vs. pen/penlight/finger, dynamic presentation
high contrast dowel vs. penlight : Visual field screening
Rod (vs. cone) cells in detection of movement and
light –
ambient vs focal vision ... choosing the right tools
Smartphone flashlight could be used for many of
these screening measures.
What’s a normal visual field?
Visual Acuity Review
NVA (near visual acuity):
Acuity near (letters)
Acuity near (symbols)
Acuity near – continuous text ... what is this and why is it important? (not just ‘print size’ – what about cadence, rate, accuracy, efficiency ... what they can ‘technically see’,nmay not be the same as what is ‘functional’)
DVA (distance visual acuity)
Acuity distance (letters)
Acuity distance (symbols) ... ways this can be modified
Acuity entered is the last line for which the patient
got > 50% correct
Visual Acuity - test eyes together or separate? Referral?
Referral for anything less than 20/40, or difference of greater than one line on eye chart between eyes
Normal: 20/12 – 20/25 (no corrective lenses to see newsprint, 1M)
Near normal: 20/30 – 20/60 (can see newsprint with glasses)
Moderate low vision: 20/70 – 20/160 (begin to experience difficulty with ADL)
Severe low vision: 20/200 – 20/400 (‘legal blindness’)
Profound low vision: 20/500 – 20/1000
Near blindness: 20/1250 – 20/2500
Total blindness: no vision and no light perception
Traditionally, ICD definition of ‘low vision’ <20/60 (20/70) best corrected acuity in better eye
Testing ocular Alignment
Position at rest (clinical
observation and corneal
reflection)
Teaming during pursuits
Cover test – strabismus
Uncover test & Alternate cover
test - phoria
Near point convergence
Why important? – functional impact/symptoms
Refer if break greater than 4 inches, recover greater than 6 inches, or if
no report of double vision
• Setting expectations (not being afraid to report blurry or double
vision)
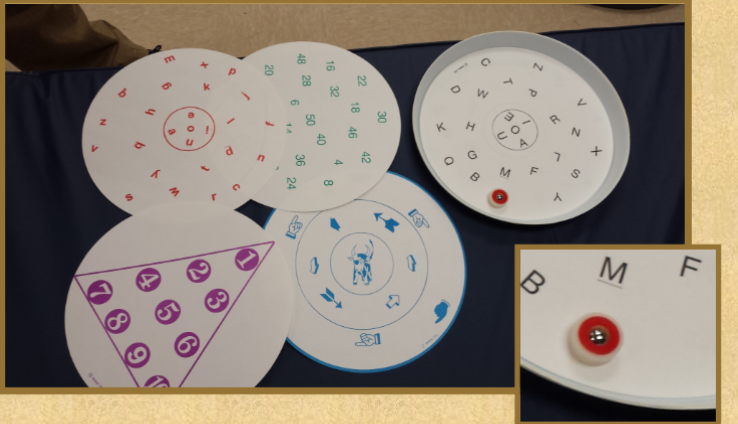
Saccadic eye movements
16” from pt, 4” either side of midline (8” apart)
5 round trips/10 fixations
Other options – 2 pens, 2 penlights

Processing Simultaneous Visual Stimuli
Why is this important functionally?
Presented 30-45 degrees from midline on right/left
Another option – Colored discs

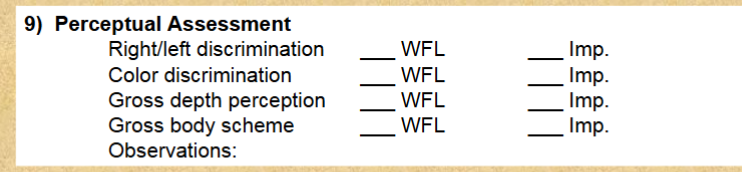
Screen basic perceptual skills during vision
Can just ask them questions
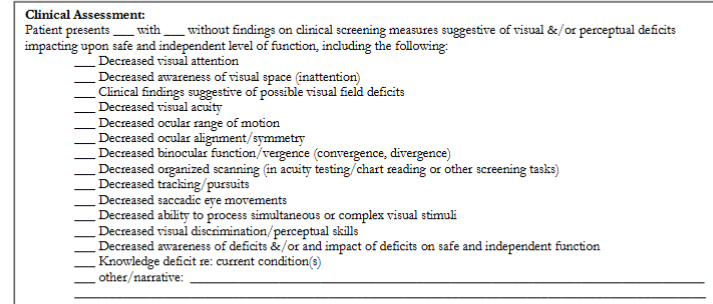
Everything a vision eval from checks (1-10)
Visual Attention
Visual Feilds
Visual Acuity
Ocular ROM and Pursuits
Ocular Alignment
Binocular Function - Vergence
Saccadic Eye Movements
Processing of Simultaneous Visual Stimuli
Perceptual Assessment
General appearance of eye and eye lids
Intervention: Visual Attention/Fixation
Bold black and white designs, blocks/patterns using bold primary colors
Incorporate movement
Place items on grids/mats with movement (transfer discs with contrast, ‘lazy susan ’with grid/mat placed on top) to facilitate fixation, incorporate visual pursuit and increase motivation
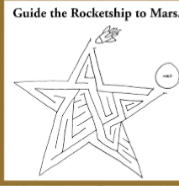
Mazes for visual fixation/attention – ease of access, variety, themes, easy to grade task
Line tracing tasks - commercially available assessments and workbooks, or create your own!
Sustained visual attention with visual perceptual skills –
puzzles in Highlights magazine, hidden object and ‘find the differences’ puzzles, workbooks and apps (great for both clinic and ‘homework’)
Intervention: Visual Feilds & Scanning
Flashlight/Laser-light Tag (Stimulating &/or increasing awareness - incorporating scanning)
Options for surfaces, positioning, AE
Variations – ‘tag’ , ‘chase’, ‘2 overlapping’, ‘jumps’
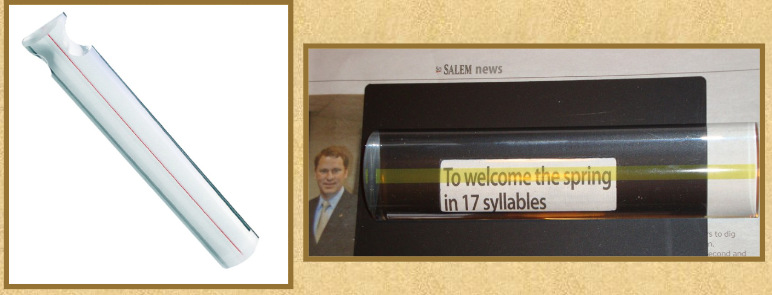
low tech adaptations for scanning text
Ruler
Bookmark
• Index card
• Reinforce visual scan across line by “‘tracing’ across line with finger
Graph paper, or turning regular (or ‘bold’ or ‘raised’) lined paper to ‘landscape’ orientation (for vertical lines) for ‘math’/banking.
Visual Fields & Scanning – Low Tech
(stimulating &/or increasing awareness – incorporating scanning)
Look for additional resources available within your department to address scanning:
1. VisAbilites Workbook
(pre-reading/reading)
2. ‘Look to the Left’
3. Resources posted in
D2L (‘worksheets’)
Visual Fields Awareness, Scanning, Ocular
ROM & Pursuits Low Tech: Vision Tube
•Inexpensive and can be used with wide range of ages, dx/conditions and can easily be graded
•Examples of ways to grade activities – supine, seated (firm surface, Dynadisc), standing (solid surface, foam mat, wobble board), with mobility, with

Visual Fields Awareness, Scanning, Ocular
ROM & Pursuits Low Tech: Marsden Ball
How can you grade the activity? (supine, seated, standing, plain ball, numbers/letters, bunt with bat/dowel, catch [both hands, one hand, alternating hands,etc.)
Inexpensive option – suspended whiffle ball with ‘Command Strip’ hook

Interventions: Ocular ROM and Pursuits
Tracking/pursuits with wands/dowels, penlights, fixator sticks or any other item – make it interactive (tell stories, make it a game, etc.) ... be creative!
These products available from Bernell/VTP
Ball games –roll, bounce or toss-pass, dribble, toss/throw to target, kick, juggle (different sizes, colors, textures, shapes)
intervention: Scanning & Tracking/Pursuits - TracKIT
Intervention: Intervention: Binocularity, Teaming and vergenge
Ball games –roll, bounce or
toss-pass, dribble,
toss/throw to target, kick,
juggle (different sizes, colors,
textures, shapes)Rebounder, or, bounce against wall
Balloon toss, ball toss, seated ‘badminton’
Addition of dual task demands ..Binocular function - Vergence: ‘Super Slider’/‘Forward Pass’/‘Zoom Ball’ – great treatment option for peds and adult populations (other benefits)
Other vergence and accommodative shifts - Intervention
‘Bulls-Eye Target’ – alternating focus between bulls-eye target in near
space, with a target in intermediate to far space.
Brock String
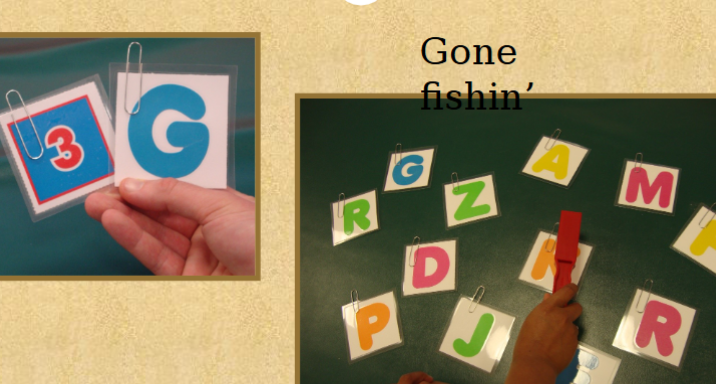
Intervention: Saccades
Remember ... saccades are a (visual) transition from one point in space to another (fixation/release/fixation)
Commercially available work books
Penlight or fixator stick exercises
Flashlight or laser light tag on wallUse scan boards, eye charts or make sheets of letter, shapes, numbers, etc. for table-top use, or posted on wall
Post-its with letter/numbers randomly arranged on wall

Intervention: Perceptual Skills
R/L Discrimination & Directionality
Remediation of reversals
Vision Intervention: Ways of Grading activites
Easel – change the plane/visual field ... also offers nice opportunity gross motor involvement and for kinesthetic input
Transition from monocular to binocular (when appropriate)
Change seating/standing surface
Improvement can be measured by
1. Time/speed
2. Accuracy
3. Activity tolerance
4. Fatigue
5. Test scores (standardized tests)
6. Subjective report
7. Improved level of function in ADL, IADL tasks, education-related tasks, functional mobility, etc.
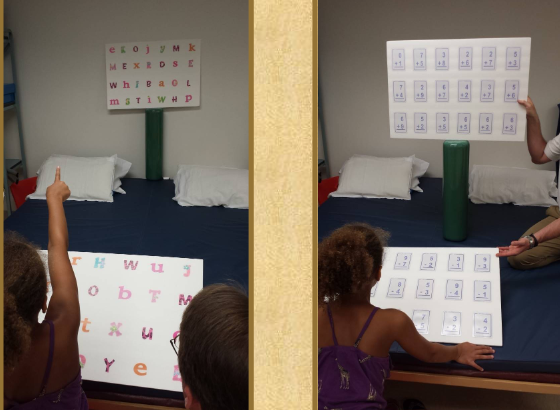
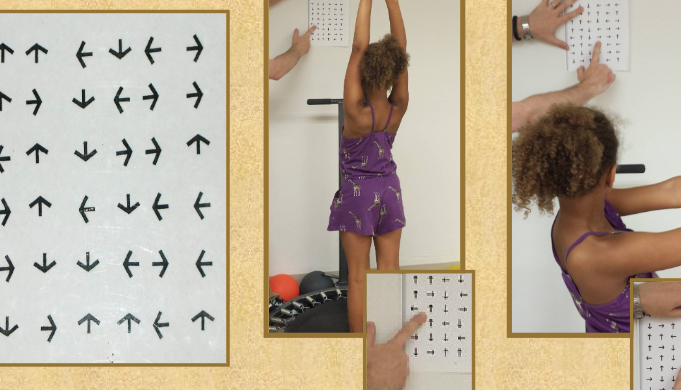
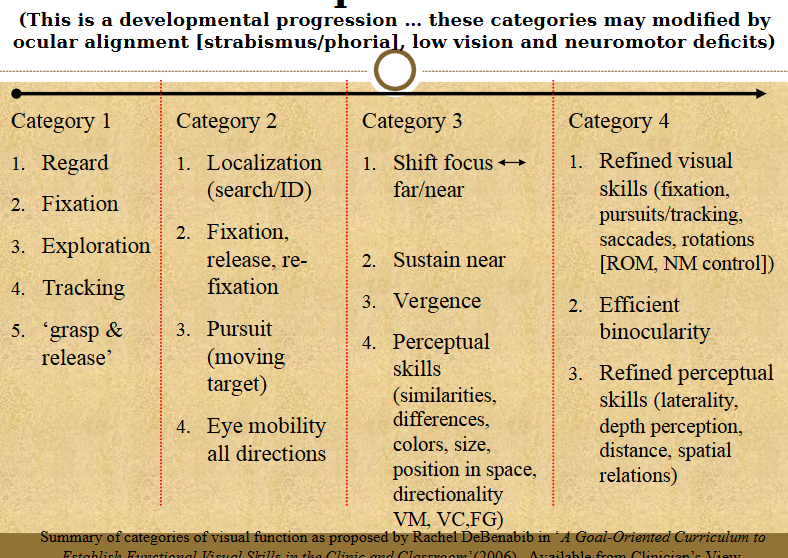
DeBenabib’s Sequence of visual skills
Intervention: Low Vision
free magnifiers
(Stand – may require pt to move magnifier, but not hold)
(Stand – may require pt to move magnifier, but not hold)

Intervention: Low Vision
free magnifiers
Binoculars, Cip on spectacles, around the neck

Intervention: Low Vision
Low vision optics/magnification - Monocular, Loupes
(Clip on or hand-held)

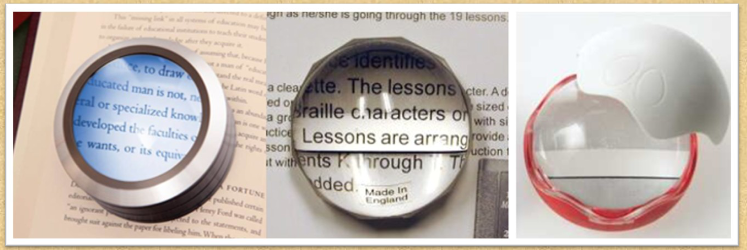
Intervention: Low Vision
Low vision optics/magnification – Globes
(magnifier sits on top of reading material and pt moves glove
magnifier over text)
Illuminated globe, globe with guideline, globe with guideline
and contrast ring
These products available from Bernell, MaxiAids and/or ILA
Intervention: Low Vision
Low vision optics/magnification – Hand-held magnifiers
Hand-held – illuminated and non-illuminated, pocket, pendant, multiple sizes/shapes,
monoculars (near and far) + ‘stand’ which are place directly on the reading material
(but still require pt to move magnifier over material)
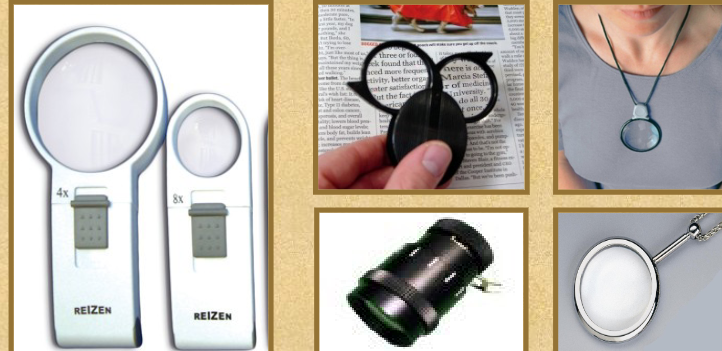
Intervention: Low Vision
Low vision optics/magnification – Hand-held
magnifiers: Strength and size may impact
reading/use (i.e. ‘spot checking’

Intervention: Low Vision
Low vision optics/magnification – Hand-held
magnifiers (Bar)
Bar with guide-line, bar with contrast line,
typoscope with bar
These products available from Bernell, MaxiAids and/or ILA
Intervention: Low Vision - HIGH TECH!
(closed circuit television/televiewer – stationary table-top units)
Stand alone unit (approximately $2,000-4,000)‘Plug and play’ using existing TV or monitor – $2,000-4,000 ... May offer greater flexibility for a wider variety of tasks since the
camera is separate from the monitor‘plug and play’ using existing TV or monitor – $200-400 (more cost-effective and portable option)
Portable electronic hand-held magnification devices - $300-1,500
App-based magnification options for smartphones and
tablets (generally, less than $5) Many offer variable
magnification, ‘lighting’,
Low Vision - Lighting
Is there such a thing as ‘too much of a good thing???
Direct lighting/‘task lighting’
Assessing lighting- is there enough, & for the specific tasks being performed in that location
Where should light be for reading/writing?
Light meter
Types of bulbs
Other inexpensive options for adding lighting in closets and in/under cabinets
“Low Vision” - Contrast
Polarized lenses with various tints to block UV and increase contrast – avoiding dark lenses – more to come on wrap-
around shades in a few minutes!
Acetate sheets for contrast
Other common examples of contrast use – reading, marking
steps/entries and thresholds, grab bars, door frames, counters/cabinets, place setting, etc!‘Low vision’ – contrast: railings and grab bars
Duct Tape on cabinets
Colored cutlery
Stairs
Tactile info from a rail
Vision Interventions: Glare reduction
‘Polar shields’ (outdoors)
Transitions lenses
Tinted lenses (indoors)
Windows
Table and counter surfaces
Flooring
Low vision’ – Sampling of Household Low Vision AE/AD
Television and computer screen magnification
Phones – large button, one touch dial, Braille, speakerphone, flashing LED
Low vision timers
Low vision watches – bold face with large numbering + digital ‘talking’
watches (can also be set to remind of medication routines)
Large print thermostats dials
Marking dots, paint, ‘hi marks’ for tactile identification
‘therapist on a shoe string’ – ‘puff paint’ from fabric store, and ‘bump dots’
Low Vision - Adaptive Equipment
Color identifiers
Tactile marking systems for clothing
Label readers
Magnified syringe guides (or ‘click’/dial insulin pens) and large print screen blood glucose meters
Magnified/illuminated tweezers and clippers (important for safe nail care with diabetics)
Large Print screen and talking thermometers and BP monitors
Talking pill bottle base
Pillboxes with large print, raised numbering with
voice or alarm medication schedule reminders
Large print on bottle tops
Organizational strategies (consistent location, by time of day, by location taken, etc.)
Large print pill box or electronic pill box, alarm on watch, or radio plugged into timer (as reminder), etc.
Decrease visual clutter + Inc contrast + Large print
Black and white cutting boards
Finger gaurds
Desk top/hand held readers
High contrast keyboards
Remote controllers (Less and larger buttons)
LV board games, cards, puzzles
REFERAL OPTIONS FOR VISION
What is the difference between the
Family physician,
Optometrist
Ophthalmologist,
Neuro-Ophthalmologist,
Behavioral (Developmental)
Optometrist,
Neuro-Optometrist,
Low Vision Optometrist,
How do I decide who is the
most appropriate to refer to?,
and
Who refers? (a ‘trick’y
question)
Vision Team members
Optometrists (and specialties)
Ophthalmologists (and
specialties)
PT
OT
ST
COVT
COMS
CLVT
CVRT
Social Work
Psychologist
Specialty Certification options for OT
CLVT
SCLV - AOTA
Why are we addressing FES - statics
1/3 of hospitalized patients may experience difficulty to swallow related
to pathology of mouth, pharynx or esophagus
• Up to 70% of patients in extended care setting may experience difficulty to swallow
• 50-75% of those in acute phase of recovery s/p CVA will experience some form/degree of dysphagia
60,000 Americans die each year from complications
associated with swallowing dysfunctions.
Who is at risk for swallowing issues
• By diagnosis: CVA, TBI, MS, ALS, MD, Parkinson’s, Dementia, Guillain
Barre
• By clinical presentation (refer to dysphagia signs/symptoms)
• By co-morbidities/other medical and clinical factors: GERD, pneumonia, etc.
Muscles for FES: Temporalis, Masseter, Buccinator, Orbicularis Oris
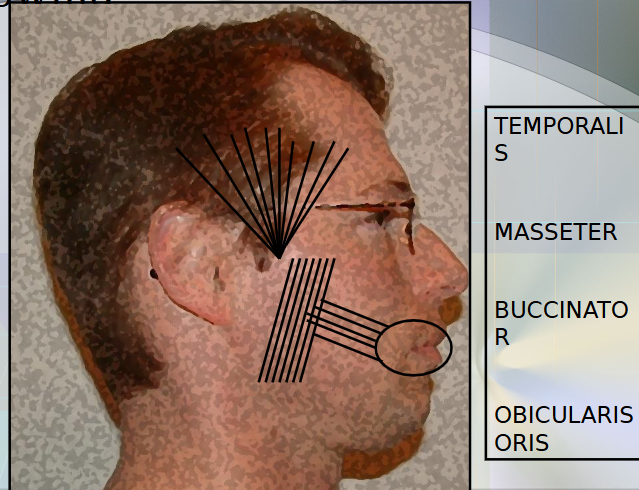
Muscles for FES:
Suprahyoid
Mylohyoids
Diagastrics
Geniohyoid
Infrahyoids
Thyrohyoid
Sterno-thyriod
Stero-hyoid
Omohyoid
Sternoclenomastiod

Anatomy FES: Anterior and Lateral Sulci
Soft palate, Uvula, Anterior and Posterior faucial arches
Pocketing
Anatomy of the Larynx

Stages of swallow
Oral preparatory stage
Oral stage
Pharyngeal stage
Esophageal
Oral Preparatory stage
lip closure, bolus is held in cupped tongue (in ‘dipper’ or ‘tipper’ position), chewing (rotary movement), velum lowers to approximate the posterior portion of the tongue
Role of types of teeth – shape and function
1. Central and lateral incisors
2. Canines
3. ‘Pre molars’ and molars
Role of Saliva in FES
• Role in bolus formation
• Impact on hygiene (residue)
• What it means as a risk factor
• ‘Xerostomia’ - dry mouth
• What can be done about it? (saliva substitute, adjustment of medications causing dry mouth, encourage fluids + recommendations during mealtime [alternating sips/bites, choosing foods with higher fluid content, use of gravies and sauces, sour/tart flavors to stimulate salivation, etc.])
Oral Stage:
1. Tongue propels food posteriorly (anterior/posterior ‘A-P’ transit).
2. Tongue elevates anterior to posterior, forming groove in midline of tongue to hold/move bolus back to faucial arches (sensory fibers signaling next stage of swallow).
3. This stage usually takes 1-1.5 seconds.
Pharyngeal Stage:
1. Velum (velopharyngeal soft tissues/soft palate) elevate and approximate pharyngeal wall,
2. Retraction of tongue base toward pharyngeal wall
3. Pharyngeal wall contracts toward base of tongue
4. Elevation of hyoid
5. Larynx (airway) closes at true and false
vocal folds and epiglottis ‘flips’ down
6. Laryngeal superior and anterior movement
7. Upper esophageal sphincter (UES) relaxes and opens
What stage is the biggest red flag? FES
Pharyngeal Stage
Esophageal Stage:
1. UES relaxes/opens
2. Peristalsis (wave-like muscle contractions to move food)
3. LES (Lower Esophageal Sphincter) relaxes/opens, allowing food to pass into the stomach
4. This stage takes 8-20 seconds
Clinical Signs and Symptoms of Dysphagia
• Temperature spike
• Coughing or choking (& why this ‘gold standard’ may not
be as reliable as you think! – silent aspiration)
• Drooling/ difficulty managing secretions
• ‘Gurgly’/‘wet’ or ‘hoarse’/‘breathy’ vocal quality or cough
• Patient c/o
• Loss of food or liquid from mouth
• Holding food or liquid in mouth (delayed initiation of swallow)
• Multiple swallows
• Watery eyes when
feeding
• Change in
coloration
• Reflux
• Change in diet
Dehydration
• Dehydration
If a pt needs an eval for dysphagia what do you do?
Obtain orders
CHart Review
Functional mealtime observation (either before or
after swallow screen [or b/s clinical evaluation]
• Screening, or Bedside/chair side clinical evaluation of F-E-S
• ? Referral for further instrumental testing/evaluation
• Development of plan of care/treatment plan, goals and recommendations
related to aspects of
Are MD orders needed for screening
No
Screening would
typically involve chart
review and patient
observation, however,
if you are going to trial
consistencies not
currently ordered by
MD, you should have
physician order for use
of test tray in
When MUST you have MD order for FES
For
bedside/clinical
evaluation of
feeding and
swallowing
(‘bedside
dysphagia
evaluation with
test tray’), you
must have MD
order, even if you
already have OT
What to review when looking at a chart
Dx/HPI
PMH
Meds - Xerostomia as a side effect of meds
LAbs (WBCs)
• Recent procedures (intubation, supplemental or alternative feeding methods, etc)
• Reason for referral
• MD order
• Respiratory status – supplemental O2 and mode of administration, lung sounds, trach, ventilator use, intubations
• Current diet (solids and liquids)
• Any diet restrictions (special diet?)
• Any supplemental feedings? What type?
• Other testing or procedures (Barium swallow, recent/prior modified barium swallow, GI series, consults – Neurology, dietary, ST, OT, respiratory, Pulmonology, etc)
• Physical and cognitive status (from PT/OT/ST/NSG
During a clinical dysphagia eval, what are we looking at?
1. Postural assessment & trunk control
2. UE ROM, strength & G/FMC
3. Head and neck ROM, strength
4. Sensation
5. Cognition
Cardiopulmonary function
ALSO
1. ROM, sensation, praxis
(coordination), strength of lips,
jaw, tongue, mouth (oral
structures), and select observable
aspects of pharyngeal function
2. Test tray/procedures
3. Monitoring for clinical symptoms
of dysphagia
Equipment on the test tray
1. Exam gloves
2. Laryngeal mirror
3. Long cotton swabs
4. Tongue depressor
5. Thickener
6. Utensils and 2-3 cups
7. Straw (optional)
*Suction equipment and
someone trained to operate it
At least one item of each liquid consistency
At least one item of each solid consistency
Stethescope
Pulse OX
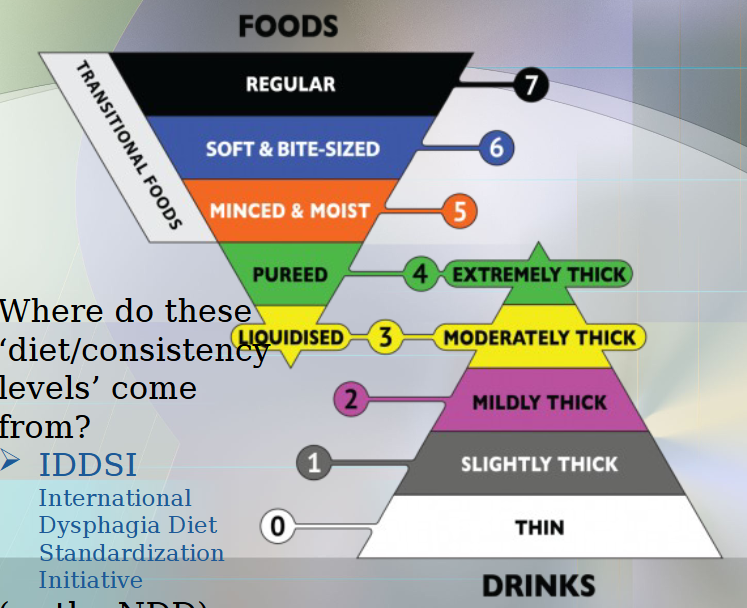
IDDSI
International Dyshagia DIet standardization initiative
IDDSI Levels
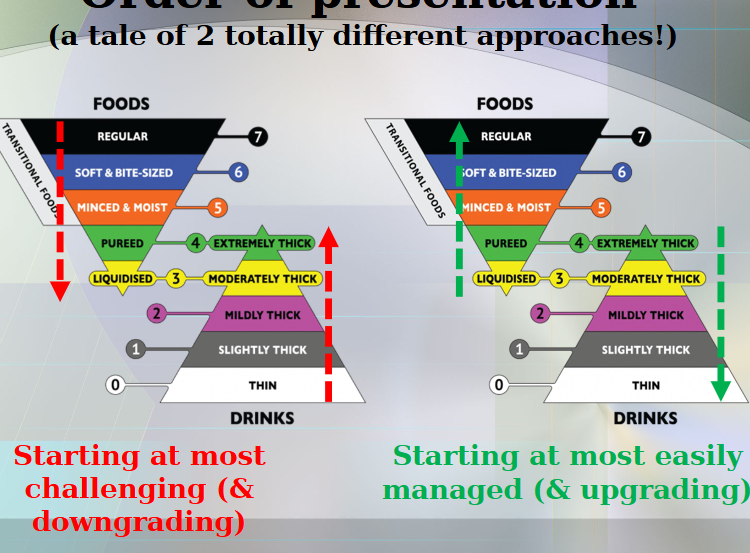
WHat is the appropriate order of presentation for FES
Effect of ice on thickened liquids
Makes it thinner bc ice melts
Useful clinical gems when eval of dysphagia
• Timing of cough as
indicator of when/where
dysphagia may be
occurring
• Type of cough as useful
clinical indicator of level
at which
penetration/aspiration
may be occurring
• Pulse-oximetry – what do
we look for ... what does it
tell us?
• Palpation
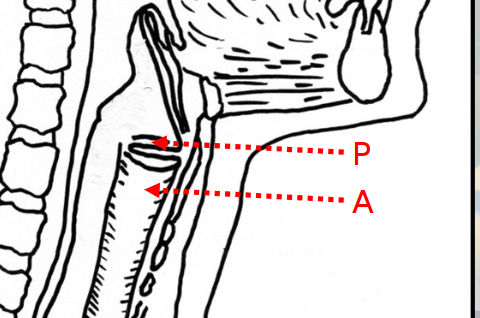
Diff b/w penetration and aspiration
Penetration happens before or at level of vocal folds'
Aspiration happens lower/ in the larynx
Overview of Basic
Compensatory
Strategies for FES
•Chin tuck – why would we use chin tuck?
•Head turn toward affected side – why?
•Combine turn with chin tuck
•Head tilt toward stronger side – why?
•Bolus size & rate of intake
•Crush meds (if able) – need MD clearance
•External pressure to the cheek – limits pocketing, provides support for bolus formation
•Lip (labial) and chin support
•Food presentation – spoon/modified spoons, ‘nosey cup’, cups that measure specific sip sizes, straw, etc
•Double/multiple effortful swallows
•Forced cough
•Alternating sips/bites
•Diet consistency – NPO, thin liquid, nectar thick liquid, honey thick liquid, pudding/spoon thick liquid, puree solids, mechanical soft solids, regular solids, crushed medication (check with MD & PDR), meds with applesauce (and another ‘trick’ for meds!)
•Tongue sweep/finger sweep
•Oral inspection with mirror (self inspection)
•Food placement – midline vs. further back on tongue vs. on the ‘stronger’ side
Thickeners
Liquid consistencies
Thin
Mildly Thick (Nectar)
Moderately thick (honey)
Extremely Thick (pudding)
Treatment strategies FES - Help w trigger swallow
Thermal Tactile stimulation - cold to faucial arch
Overview of Common Remedial/Rehabilitative/Restorative Treatment Strategies/Interventions for FES
•Sour lemon bolus
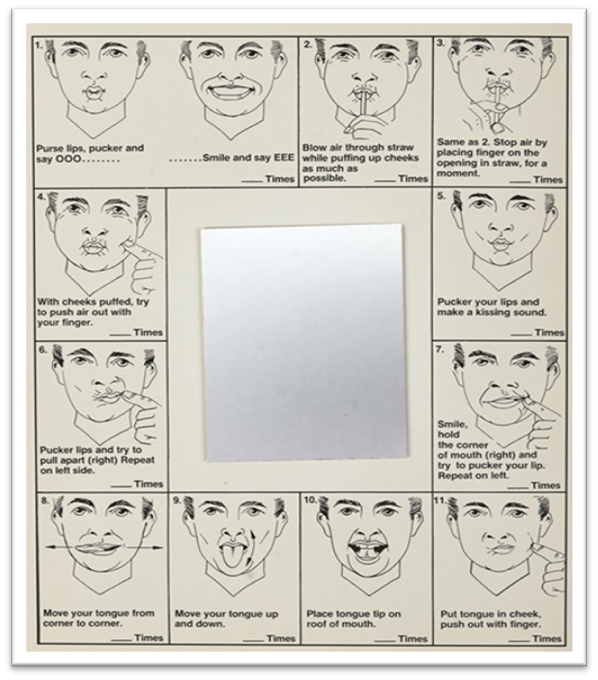
•Oral motor exercises (VHI, Oral Images, etc.)
•Mendelsohn maneuver – maintains elevation of the larynx to decrease pooling and assists to sequence swallow (see handout)
•Supraglottic and super-supraglottic swallow – assists patient with airway closure and clearing of airway (see handout)
Shaker exercise
•Laryngeal adduction and breath hold exercises (valsalva maneuver) – used to strengthen and assist with laryngeal closure. Typically done by pushing/pulling while phonating vowel sound or by taking breath and ‘bearing down”/contracting diaphragm while holding breath (consider cardiac precautions!)
estim
Supraglottic swallow
1.Inhale and hold breath
2.Small bite or sip
3.Swallow (keep holding breath
4.Cough
5.Swallow
6.Breathe
Remedial/rehabilitative interventions FES
•Pulmonary exercises … Why?? – trunk extension & shoulder/scapular retraction/adduction with inhalation, trunk forward flexion & shoulder protraction/abduction with exhalation
•IS (‘peak flow meter’), flutter, ‘Breather’
•Inhale/cough
•Pulmonary exercises … Why?? – trunk extension & shoulder/scapular retraction/adduction with inhalation, trunk forward flexion & shoulder protraction/abduction with exhalation
•IS (‘peak flow meter’), flutter, ‘Breather’
•Inhale/cough
Remedial/Rehabilitative intervention ideas for Oral motor
• – tongue lateralization, tongue movements (praxis, strength)
•‘therapist on a shoe sting’ ideas: Life Savers
•Oral motor – lip closure and seal (‘Facial Flex’, ‘button pull’)
multi sensory facilitation/inhibition (flavor, spin, vibration, touch, pressure, texture, may also include the visual input of the prep and the auditory input )
jaw strengthening for chewing/mastication
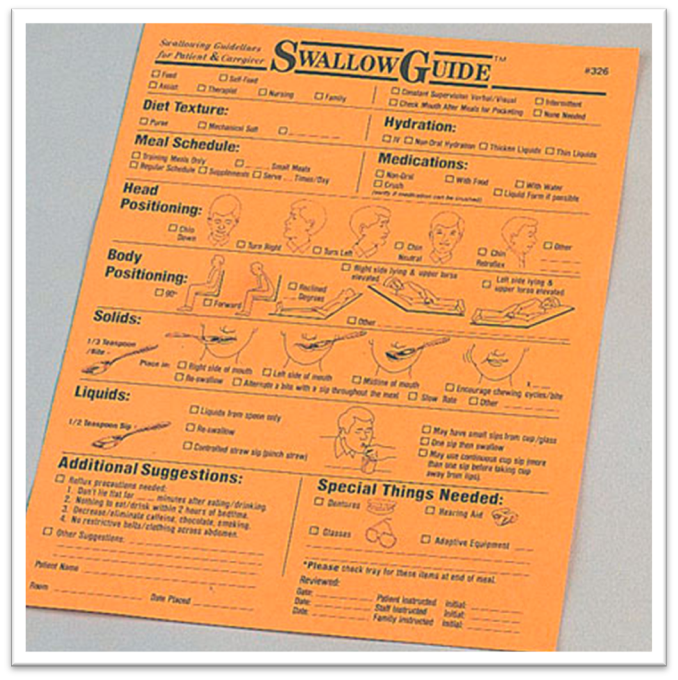
Remedial/Rehabilitative intervention ideas for pt, caregiver and staff eductaion resoruces
jaw strengthening for chewing/mastication
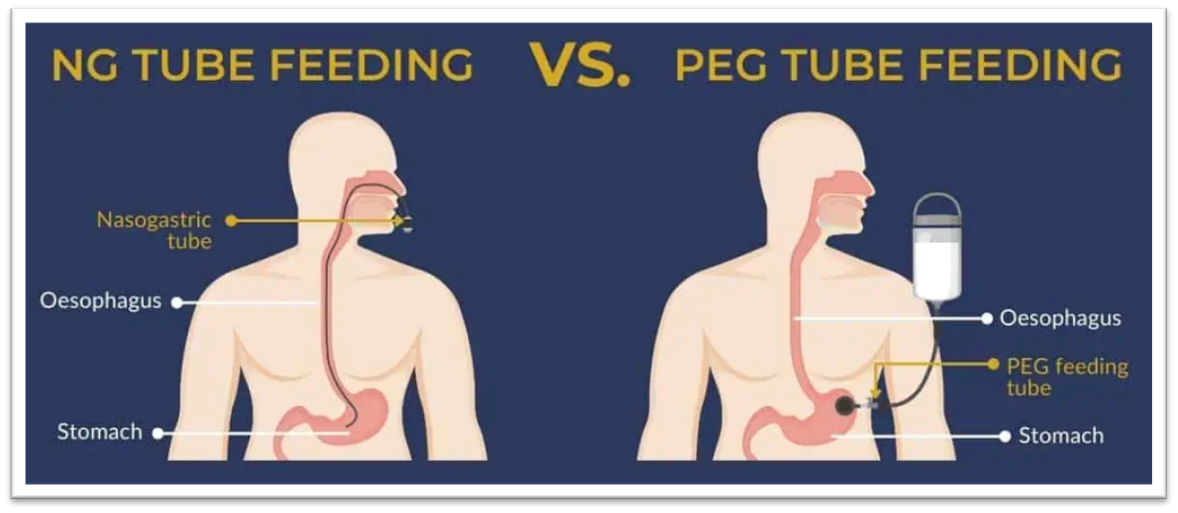
Alternative/Supplemental feeding routes
•Nasogastric tube (NG tube) – through nose, down esophagus, into the stomach. Usually short term (6 weeks or less)
•Gastrostomy (G tube) – directly placed into stomach (surgically – typically concurrent with other abdominal surgery). Usually for long-term feedings
•Percutaneous Endoscopic Gastrostomy (PEG tube) – performed under local anesthesia, functionally, same as G tube.
Additional clinical considerations
•Ways physicians think of dysphagia evaluation
1.‘Water’ tests (screenings)* … why might this be problematic?
2.Bedside evaluation with test tray
3.Instrumental evaluations* (MBS & FEES)
•Free water protocols
•Ethical issues (non-compliant patient, non-compliant family [a true story about fried chicken and Cheetos!], non-compliant staff, end of life issues, balancing nutrition/hydration with risks, informed consent)
•What can be done about purees? (power of presentation!) - MOLDS!!
•Medications – what general types and what symptoms can they produce?
•Timing of medications (Parkinson’s)
•Respiratory swallow cycle
•Can dysarthria of speech be used as indicator? (statistical correlations vs. clinical applications) - NOOOOO
One of the leading risk factors for aspiration is
Being dependent with feeding
Importance of promoting self feeding'
Staff training
Role of Oral care
Clean them out bc we dont want them swallowing gross stuff
When would you refer for an instrumental evaluation?
Things we cant see
Request a refferal
If we see any symptoms of pharyngeal stage issues we refer IMMEDIATELY (E.g. Coughing/Choking, Changes in pulse ox, during palpation not great elevation, delay in swallowing, after swallow there is gurgling, voice quality is gurgly after)
Interventions for FES if OT gains more training/experience w it
1.Everything in the ‘generalist’ category +
2.May be more involved identification and selection of appropriate interventions
3.Intervention areas may expand beyond feeding to include eating and swallowing
4.Interventions may expand to include restorative (as appropriate) in addition to compensatory
5.Train other OTs regarding F-E-S interventions
Intervention of FES as generalist
1. Address feeding (factors influencing independence with self-feeding, including sensory, motor, cognitive, perceptual, task, environment, positioning, AE, &/or compensatory strategies)
2.Collaborate with other members of the IDT (including ST) – observe precautions and carryover compensatory swallow strategies recommended by ST in OT ADL feeding sessions
3.Ensure recommended diet is observed during OT sessions
4. Monitor for s/s of dysphagia and report observations to relevant members of the IDT
Bedside Evaluation of Dysphagia
More of a speech assessment
VERY VERY LONG - 7 Pgs long
Areas of eval: Cog and communication screening, Oral motor exam, Test tray