Understanding Apraxia: Types and Assessment Techniques
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
130 Terms
Apraxia
The inability to perform a voluntary act even though the motor system, sensory system, and mental status are relatively intact.
Face-tongue Apraxia
The inability to efficiently produce or imitate movements involving the face, tongue, mouth, jaw, or palate on command.
Ideomotor Apraxia
Apraxic patients are often unaware of their deficits and may do an act automatically that they cannot do on command.
Constructional Apraxia
A form of apraxia where the patient has difficulty in constructing or drawing objects.
Technique to test Face-tongue Apraxia
Ask the Pt to protrude the tongue and move it up, down, right, and left and lick the lips.
Technique to test Ideomotor Apraxia
Ask the patient to demonstrate a sequence: how to use silverware, thread a needle, strike a match and light a candle, and use a key to lock and unlock a lock, or use scissors or other tools.
Common Causes of Apraxia
Left hemisphere lesions, particularly in Broca's area (inferior frontal gyrus).
Distinction between Apraxia and Other Motor Deficits
Impairment in performing learned, skilled movements on command while still being able to perform them automatically in a natural context.
Pyramidal Lesions
Frequently associated with stroke, Alzheimer's disease, or Parkinson's disease.
Cerebellar Lesion
The Pt with a cerebellar lesion retains the ability to perform an act but cannot perform it smoothly.
Basal Motor Nuclei Lesions
Involuntary movements or rigidity impede down the act, but the sequence of the act remains possible.
Formal Criteria to Distinguish Apraxia
The Pt's motor system is sufficiently intact to execute the act, the Pt's sensorium is sufficiently intact to understand the act, the Pt comprehends and attempts to cooperate, the Pt's previous skills were sufficient to perform the act, and the Pt has an organic cerebral lesion as the cause of the deficit.
Patients struggle with tasks such as
Blowing a kiss, sticking out the tongue, puffing cheeks, whistling, and licking lips.
Aphasia
Usually the patients with ideomotor apraxia also have aphasia.
Both hands affected
Both hands are usually affected, although the lesion is unilateral.
Praxia
Ability to execute a voluntary act.
Praxis
Action, as in practice.
Apraxia definition
Inability to act.
Constructional Apraxia
the inability of patients to copy accurately drawings or three-dimensional constructions (Russell, et al., 2010).
Technique to test Constructional Apraxia
Ask the Pt to copy geometric figures (a cross, interlocking pentagons, or clock face) or construct them out of matchsticks.
Right Parietal Lobe Damage
more severe impairment in spatial perception (e.g., neglecting one side of space, distorted drawings).
Left Parietal Lobe Damage
more impairment in motor planning (e.g., difficulty sequencing steps of a drawing).
Face tongue Apraxia
Left Frontal Lobe.
Broca's area
Premotor Cortex.
Ideomotor Apraxia
Left Parietal Lobe, Premotor Cortex, Supplementary Motor Areas (sometimes).
Somatosensory System
A network of neurons and specialized receptors that allows for the perception of touch, pressure, temperature, pain, and proprioception.
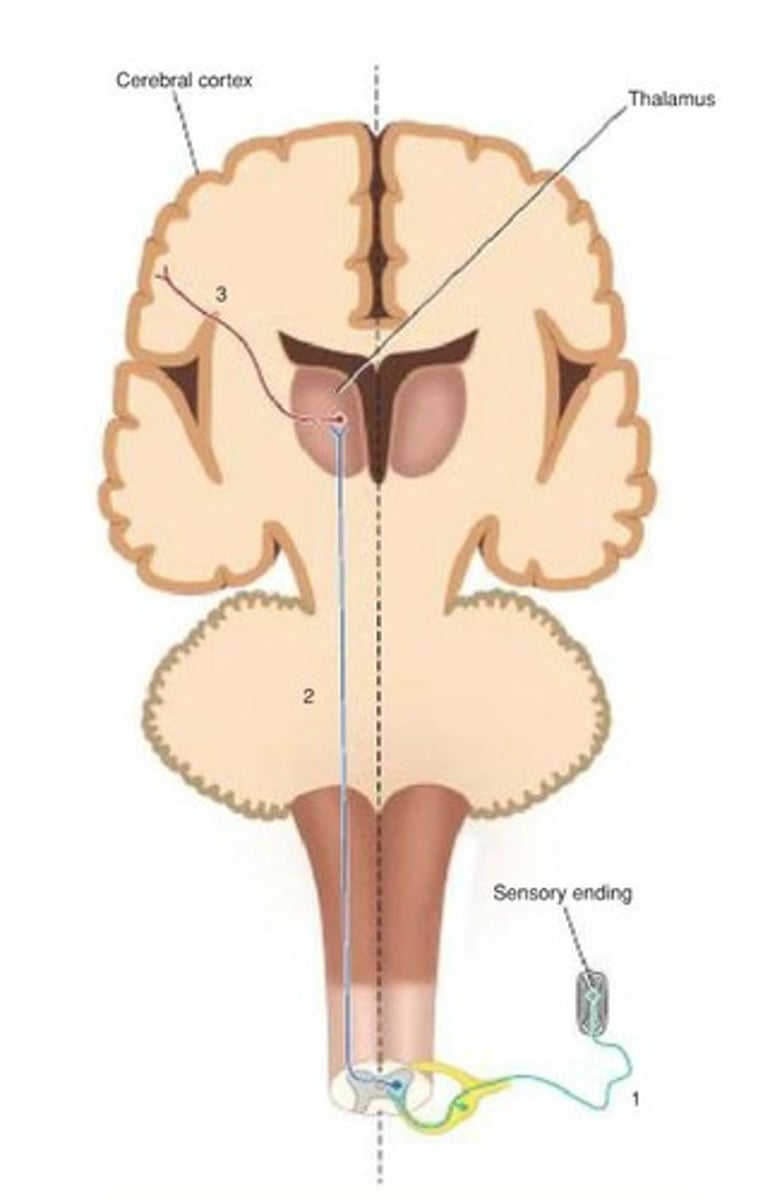
Pathway of Sensory Input
Sensory neurons enter the spinal cord → cross to the opposite side → ascend to the thalamus → projects to the somatosensory cortex.
Lower Limb Examination
A test to elicit neurological signs in the legs and feet.
Altered sensations in patients
Patients may present with altered sensations, numbness, or loss of power of a limb.
Neuropathies
Other neuropathies can occur as foot drop or 'glove and stocking'.
Full neurological examination
includes an assessment of both the motor and sensory systems of the legs.
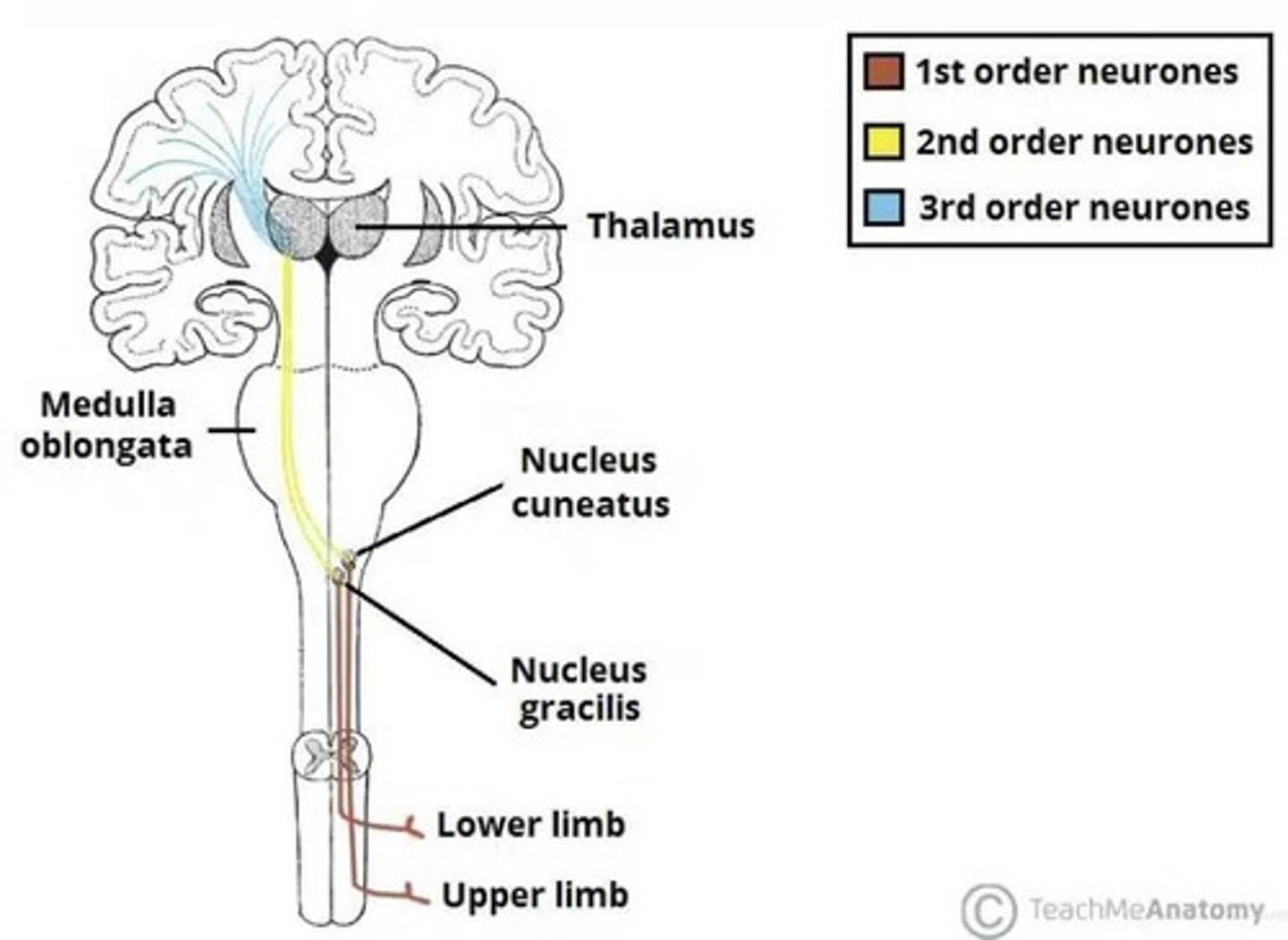
Dorsal Column Tract
also known as the Dorsal Column-Medial Lemniscus Pathway, carries fine touch, vibration, and proprioception.
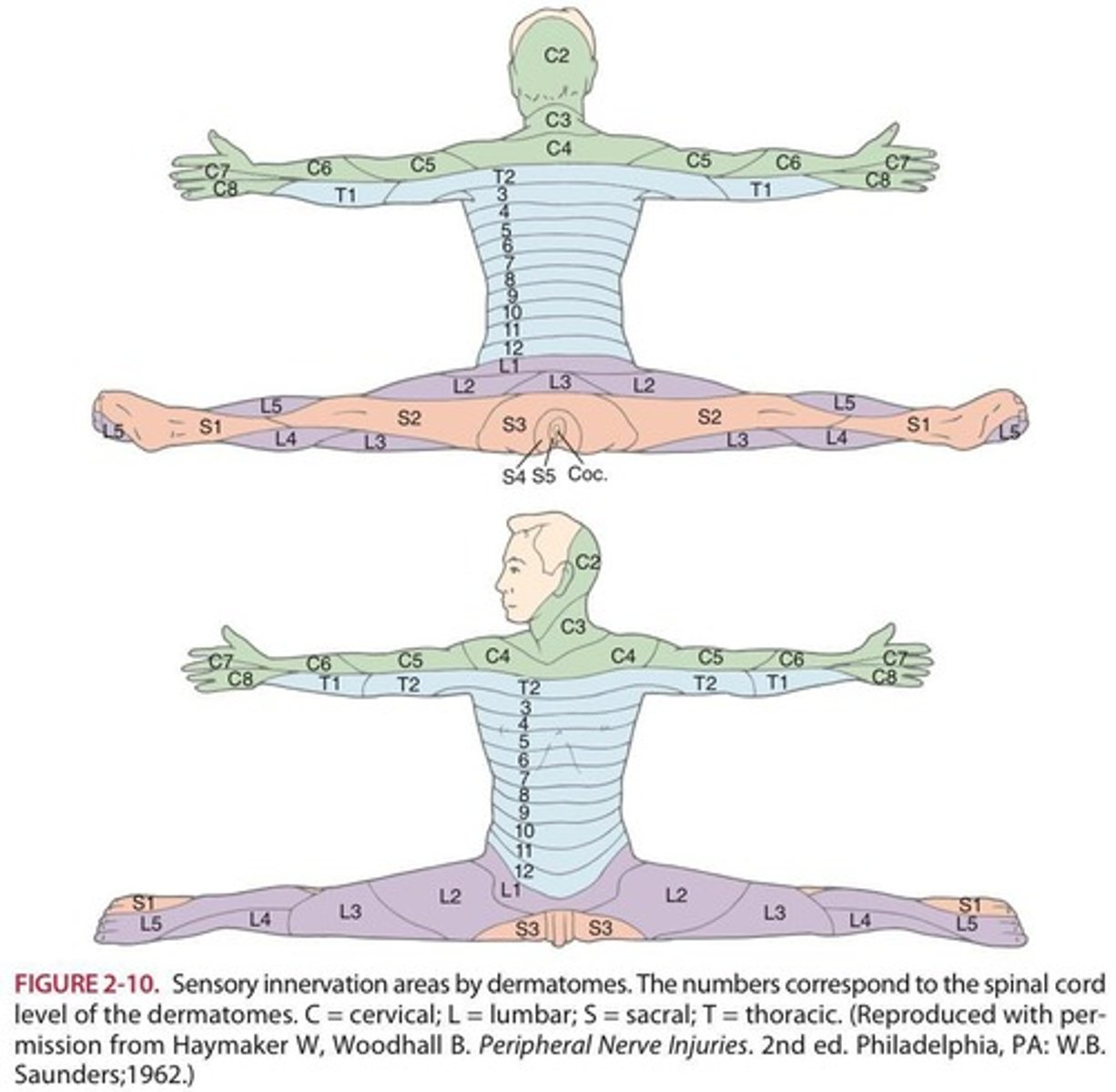
Dermatomes
specific regions of the skin where sensory information are organized.
Spatial tasks in Constructional Apraxia
Both 2D and 3D spatial tasks, such as copying geometric figures, arranging blocks in a pattern, drawing a clock face correctly, and assembling a puzzle.
Misplacement of movements
using the wrong body part for an action, like pretending to use a toothbrush with their finger instead of mimicking holding a brush.
Patients' spontaneous actions
the patient cannot do it, but they may spontaneously wave when saying goodbye to someone.
Patients' task performance
they may struggle, but they can brush their hair when actually holding a brush.
Severe spatial deficits
Right = severe spatial deficits.
Motor planning deficits
Left = motor planning deficits.
External changes detection
detects external changes.
Numbness in limbs
Patients may present with numbness.
Loss of power in limbs
Patients may present with loss of power of a limb.
Sensory input pathway
Sensory neurons enter the spinal cord, cross to the opposite side, ascend to the thalamus, and project to the somatosensory cortex.
Dermatome
Each dermatome corresponds to a spinal nerve root that supplies sensation to a particular area of the body.
Mapping
Mapping is important in diagnosing nerve injuries, spinal cord lesions, etc.
Pathway of Sensory Input
Peripheral receptors → Dorsal Columns of the Spinal Cord → synapses in the Medulla → crosses to the opposite side → Thalamus and Somatosensory Cortex.
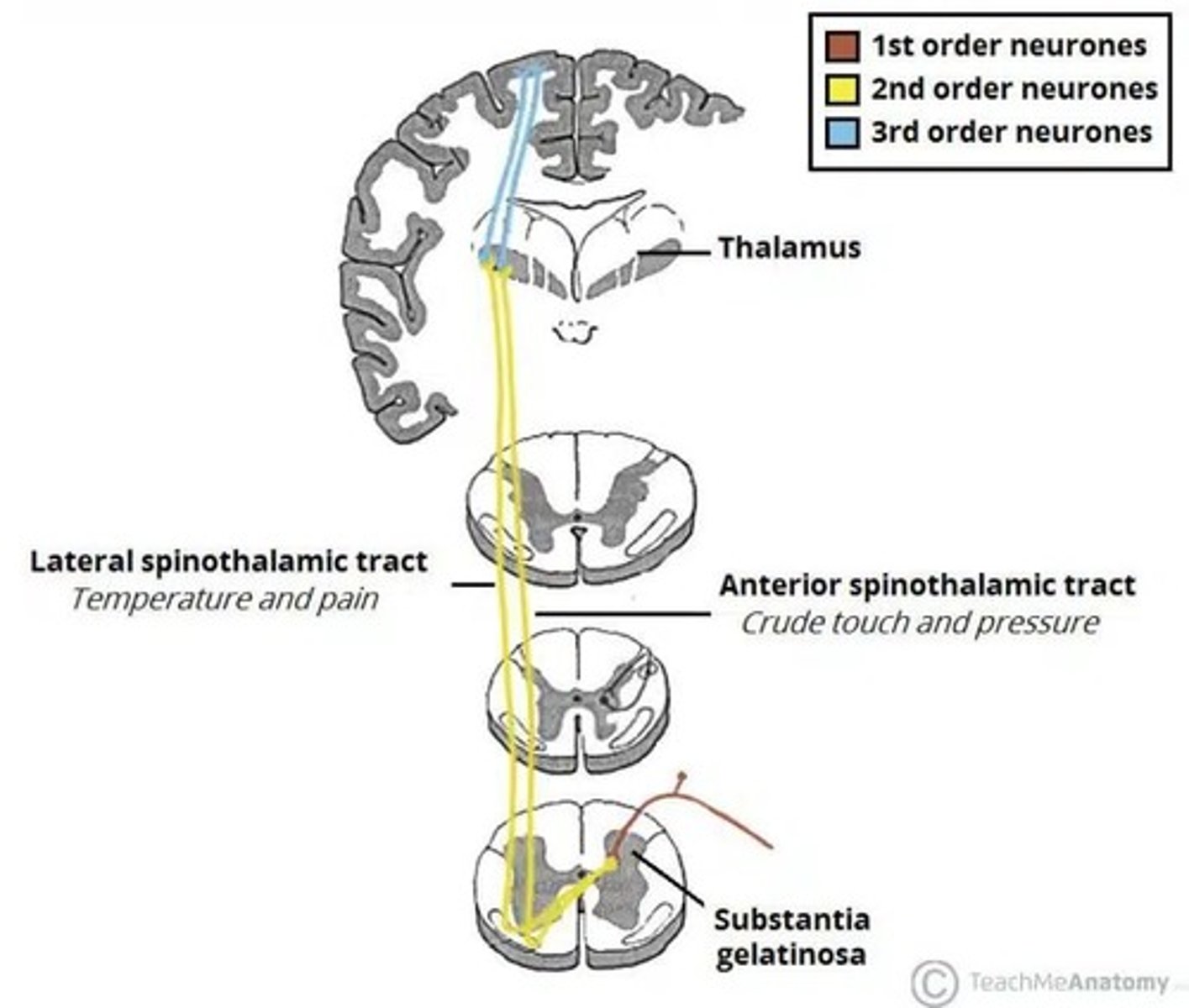
Spinothalamic Tract
Transmits pain, temperature, and crude touch.
Sensory Endings
Sensory endings are widely distributed and found throughout the body in both somatic and visceral areas.
General Procedure for Sensory Function Testing
Key points to remember when testing the sensory function of the lower extremity.
Patient Preparation
Make them feel comfortable and relaxed before beginning any test.
Eyes Closed Assessment
Ensure the patient has their eyes closed for the assessment.
Demonstrate Normal Sensation
Demonstrate normal sensation on the patient's dermatomal boundaries to minimize the risk of misinterpretation.
L1 Dermatome
Inguinal region and the very top of the medial thigh.
L2 Dermatome
Middle and lateral aspect of the anterior thigh.
L3 Dermatome
Medial aspect of the knee.
L4 Dermatome
Medial aspect of the lower leg and ankle.
L5 Dermatome
Dorsum and medial aspect of the big toe.
S1 Dermatome
Dorsum and lateral aspect of the little toe.
Light (Crude) Touch
Touch impulses ascend to the somesthetic cortex by two spinal pathways.
Abnormal Response to Light Touch
Loss of sensation, hypersensitivity or heightened sensation to light touch.
Delayed Response
Decussates at the level of entry of the dorsal root.
Temperature/Pain Perception
Temperature and pain impulses ascend to the somatosensory cortex via the lateral spinothalamic tract.
Test for Light Touch
Ask the Pt to say 'touch' in response to each touch by a wisp of cotton.
Types of Pain
Fast - sharp and bright; Slow - dull, diffuse, stinging, or burning pain.
Analgesia
Loss of pain sensation.
Thermoanesthesia
Loss of temperature sensation.
Test for Temperature
Show Pt that you will place two stimuli up and down the trunk to discover a dermatomal loss or spinal cord sensory level around the lower limbs.
Temperature Discrimination Test
Test using different objects (warm and cold tubes or a tuning fork) applied to the legs to assess the patient's ability to discriminate temperature.
Test Procedure for Temperature
Hold the cold object to the dorsum of the hands, feet, and face, then replace it with a warm object, starting from the foot to the upper thigh.
Quantitative Testing of Touch and Pressure
Involves the use of graded monofilaments and von Frey hairs of different strengths to assess touch and pressure sensitivity.
Pain Perception Test
Involves pricking the patient with a pin while they have their eyes closed to assess their ability to feel pain.
Localization of Touch
After detecting light touch with eyes closed, the patient must place a finger on the exact site touched.
Normal Response to Sensation
Patient verbally confirms sensation when lightly touched with a wisp of cotton, with no delay or loss of sensation.
Abnormal Response to Sensation
Includes inability to detect coldness/warmth or pain, delayed pain perception, feeling stimulus only on one side, or referred pain.
Sensitivity Variation
Different areas of the skin exhibit varying thresholds for touch, with the back and buttocks being less sensitive than the face or fingertips.
Screening Purposes for Sensory Examination
Determine how far to extend the sensory examination based on patient history.
Common Pathway for Pain and Temperature Receptors
Pain and temperature receptors overlap and share a common pathway in the spinal tract, making temperature testing relevant for both.
Vibration Perception
Dorsal column pathways mediate vibration, with evidence suggesting pathways may also travel in the dorsal part of the lateral columns.
Effects of Thalamic Injury on Sensation
Sensory deficits depend on the area of thalamic injury, with interruption of pathways reducing vibratory perception.
Suprathalamic Lesions
These lesions more or less spare vibration perception.
Testing Temperature Discrimination
If the patient discriminates temperature normally and history does not suggest neurologic disease, there is no need for further pain testing.
Patient Preparation for Pain Test
Show the patient the pin to be used for pricking before asking them to close their eyes.
Testing Order for Pain
Prick the patient in each leg from distal to proximal.
Threshold for Touch
Different skin areas have different thresholds for touch, with the face and fingertips being more sensitive.
Patient Response to Coldness/Warmth
Patient feels coldness/warmth or pain upon applying the stimulus.
Equal Sensation in Legs
Patient feels the same level of stimulus in both legs.
Delayed Pain Perception
A condition where the patient experiences a delay in feeling pain after a stimulus is applied.
Referred Pain
The site at which the patient feels pain may not correspond to the site of the stimuli applied.
Vibration Sense
Involves the Dorsal Column Pathway which is related to vibration sensation.
Pallanesthesia
Loss of vibration sense due to lesion or injury in the pathway.
Reidel-Seiffer tuning fork
The most practical tool for routine clinical use in quantitative tests of vibration.
Normal Response
Usually coupled with other neurologic tests to verify diagnosis.
Vibration Sense Test
Applied to a bony prominence to assess vibration sensation.
Preparation of the Patient
Start with the Patient's eyes open and show what you will do, but perform the test with the Patient's eyes closed.
Abnormal Response
Absent or decreased vibration sensation at distal sites, delayed perception, or asymmetric response.
Test Procedure
Hold a tuning fork (128 or 256 cps) and apply it to the Patient's toenails or proximal to the nail bed.
Digital Position Sense Test
Instruct the Patient to remain relaxed while testing the position of a digit.
Reliability Monitoring
Use of varying intensities and standard anatomic sites to improve accuracy in testing for pallanesthesia.
Interpretation of Vibration Testing
Involves assessing the Patient's ability to detect vibration and reporting the position of a digit.
Aging Effect on Vibration Sense
Increases the threshold to vibration and reduces sensitivity.