week 1- oral cavity, tongue, and oesophagus, stomach
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
what is the portal systemic anastomosis?
a connection (or collateral pathway) between the portal venous system—which carries blood from the digestive organs to the liver—and the systemic venous circulation, which returns blood to the heart.
Where does the geniohyoid muscle attach?
The geniohyoid muscle attaches to the chin and the hyoid bone close to the midline.
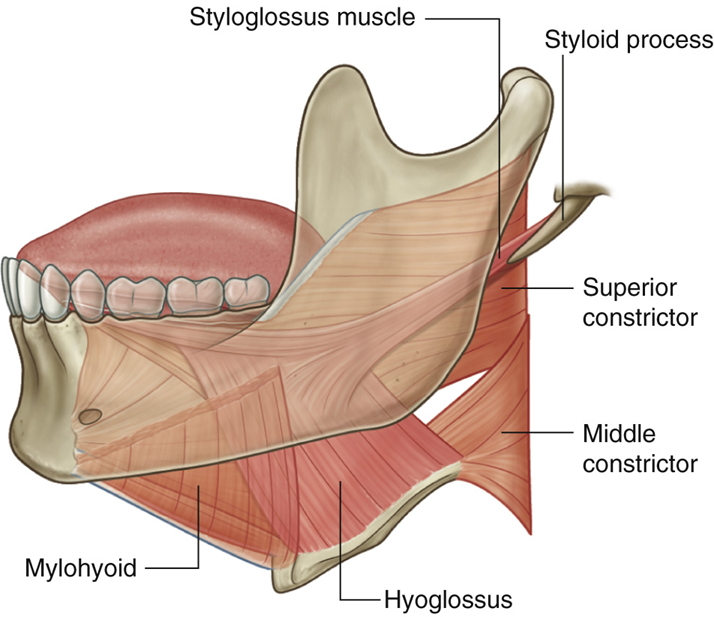
What is the action of styloglossus?
Retraction and elevation of the tongue
Which nerve provides general sensation to the anterior 2/3rd of the tongue?
mandibular nerve- (a branch of the trigeminal nerve)
what do the dental arches separate the oral cavity into?
The dental arches separate the oral cavity into the oral vestibule and the oral cavity proper
what is behind the oral cavity?
the oropharynx (the part of the pharynx that lies between the soft palate and the hyoid bone)
what are lips made AND lined with?
composed of soft tissue, lined externally by skin and internally by oral mucosa
what is the main muscle of the lips AND state its function
the orbicularis oris, acts as a sphincter for the oral fissure
what is the roof, floor and walls of the oral cavity?
roof= hard and soft palate, floor=soft tissues, incl. tongue, lateral walls= cheeks
what are cheeks composed of?
made of muscle and fascia, lined superficially with skin and deep with oral mucosa
what is the main muscular component of the cheeks?
the buccinator muscle
what supplies the foregut?
the coeliac trunk
what supplies the midgut?
the superior mesenteric artery (SMA)
what supplies the hindgut?
the inferior mesenteric artery (IMA)
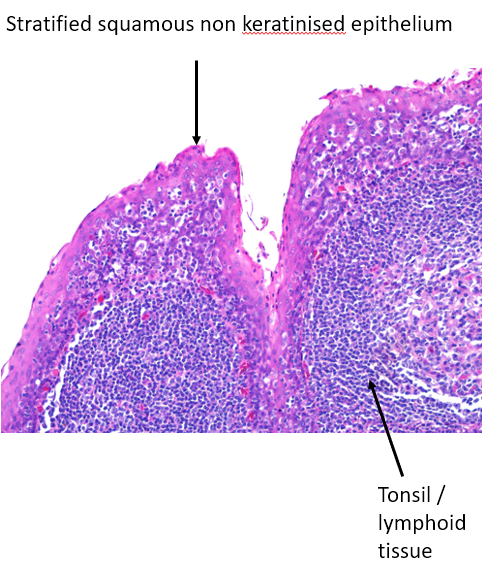
what type of epithelium is the oral mucosa, and what is it supported by?
(thick) stratified squamous epithelium. Supported by lamina propria
what parts of the mouth are keratinised, and why?
gums, hard palate and the upper surface of the tongue. Because these are the areas subject to the MOST friction (wear and tear)
what are the features of the Free Vermilion Border (transitioning area between skin and oral mucosa on the lips)?
stratified squamous, highly vascularised, large collection of free nerve endings (sensitive), no sebaceous glands
what are the features of the oral mucosa?
(thick) stratified squamous non-keratinised epithelium,
what are teeth made of, and what produces the components?
enamel produced by ameloblasts, dentine produced by odontoblasts and pulp cavity
why is the tongue specialised?
to allow manipulation of food, to undergo speech, and sensory function for taste
what is found in the anterior 2/3 of the tongue, and what is instead found on the posterior 1/3?
the papillae are found on the anterior 2/3 and lymphoid tissue is found on the posterior 1/3
what are papillaes and their functions?
papillae are small visible bumbs which house the taste buds, and are therefore needed for taste, touch, mechanical function.
what are the 4 types of papillae?
fungiform, filiform, circumvallate, foliate (few in humans)
what type of epithelium is each type of papillae (excluding foliate)?
Filiform= keratinised stratified squamous epithelium
Fungiform= Non-keratinised stratified squamous epithelium, but very vascularised
Circumvallate= Non-keratinized stratified squamous
what glands produce saliva?
parotid, sublingual and submandibular glands
what are the functions of saliva?
protective
digestive
lubrication
alkaline environment to protect the enamel
facilitates taste
starts the digestive process (Salivary amylase)
what are the functional units of salivary (secretory) glands?
Acini (secretory unit) and ducts
what are the components of salivary glands (major and accessory salivary glands)?
salivary duct
serous and/or mucinous glands (i.e. acini) [depending on whether it produces serous fluid or mucous, or both]
where are Myoepithelial cells located in salivary glands and what is their function?
positioned between acini (secretory cells) and the basement membrane of the acini. Their primary function is to contract and expel saliva from the acini and ducts in response to stimulation
what is the histology of the oropharynx?
what layers make up the mucous membrane of the GI tract (OESOPHAGUS), and what are the 3 functions it can have depending on the region and function of the tract?
epithelia, lamina propria, muscularis mucosae
functions= absorbative, secretory, protective
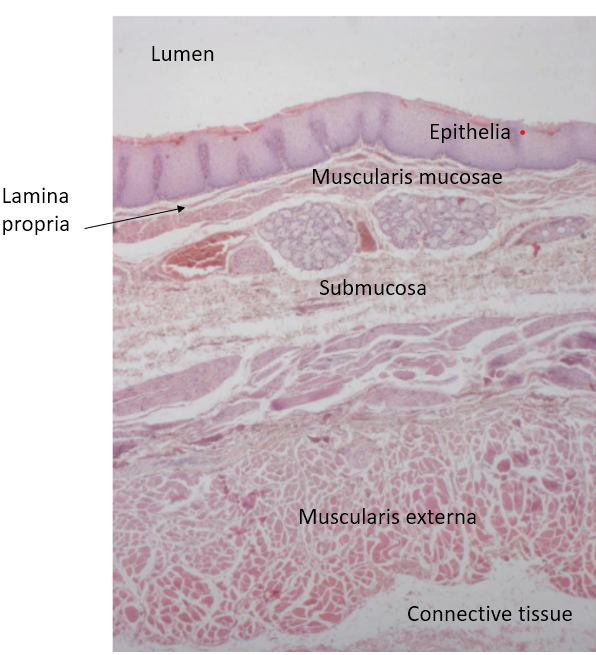
what are the 2 layers of the muscularis externa of the oesophagus, and what is their function?
inner circular and outer longitudinal of muscularis externa. Peristalsis
what’s the role of the muscularis mucosae in the transport of the bolus (HINT-different from the muscularis externa’s role)
it helps the epithelia to grip onto the food by “changing” its shape
what type of glands are found in the submucosa layer of the oesophagus, and what is their functions?
serous-mucous glands, their secretions help lubricate the oesophagus and the food, to help it move down
How does the class of epithelium lining the oesophagus reflect the function of the organ?
The epithelium lining the oesophagus is non-keratinized stratified squamous epithelium, and its structure is a direct reflection of the oesophagus’s primary function: conducting food from the mouth to the stomach while withstanding mechanical stress.
what histological change happens in Barrett’s oesophagus?
the epithelium of the lower oesophagus undergoes metaplasia , i.e. it converts to a columnar cell which is mucus-secreting
what appearance in a biopsy would signify Barrett’s oesophagus?
If you are to see glandular epithelium in an oesophageal biopsy
A 40-year-old man with chronic gastro-oesophageal reflux undergoes biopsy. Columnar epithelium with goblet cells is found in the distal oesophagus. What is this likely to represent?
Barrett’s oesophagus
A patient presents with dry mouth. A biopsy is taken from a minor salivary gland in the oral cavity. What is the predominant epithelial type of the ducts of a salivary gland?
simple columnar
which 2 areas of the GI track are under voluntary control?
upper oesophageal sphincter (swallowing)
external anal sphincter (defecation)
where does the innervation of the GI tract, especially the muscularis externa, mainly come from?
the Myenteric Plexus
where are Interstitial cells of Cajal found?
in the muscularis externa of the GI tract, especially between the inner circular and outer longitudinal muscle layers, near the myenteric plexus
what’s the function of Interstitial cells of Cajal?
Pacemaker function. They generate Basic Electrical Rhythm (BER)
what does the Basic Electrical Rhythm (BER) determine?
it determines how often an area of the gut can contract (peristalsis) . They set the timing and direction of smooth muscle contractions
Variations in Basic Electrical Rhythm (BER) [created by ICCs] determine directionality, what does that mean? and which region has the higher BER and which the lowest?
it means that regional differences in the frequency of BER help establish the forward movement of contents through the GI tract. Higher BER in proximal intestine than in distal intestine.
what does the Enteric Nervous System include?
2 major plexuses:
Myenteric plexus - primarily regulates mobility
Submucosal plexus - Controls secretion, local blood flow, and absorption
what does the Enteric Nervous System mediate?
it mediates the Reflex activity in the absence of CNS input (interprandial period)
what extrinsic factors is the Enteric Nervous system influenced by? And what effect do they have?
(parasympathetic) Vagal control: Excitatory to Non-Sphincteric muscle, inhibitory to Sphincteric muscle
Sympathetic control: inhibitory to Non-Sphincteric muscle, Excitatory to Sphincteric muscle
what other Neurohormonal factors influence the Enteric Nervous System?
5 hydroxy-tryptamine (serotonin)
Motilin
(action of) Opioid receptors
what is the muscular structure of the oesophagus?
upper oesophageal sphincter, upper 1/3, is striated skeletal muscle under voluntary control.
lower oesophageal sphincter, distal 2/3, lined by smooth muscle, involuntary control via the Enteric nervous system
what are some disorders of Oesophageal Motility, that can only be diagnosed by manometry?
Achalasia- characterized by the failure of the lower oesophageal sphincter (LOS) to relax and absent or impaired peristalsis in the distal oesophagus
oesophageal involvement in Scleroderma- weak LOS, absent peristalsis, severe oesophagitis (inflammation of the oesophageal mucosa)
Jackhammer oesophagus- associated with pain on swallowing, but it is a functional swallowing
what are the 2 phases of motility of stomach and small intestine?
Interprandial Period- cleansing of gut in preparation for next meal
Fed state
what is the Interprandial (fasting) Period controlled by?
The Migrating Motor Complex (MMC)
What is the Interprandial period, and how how often does it occur?
is a cyclic contraction sequence, that acts to cleanse stomach and intestine. It occurs every 90 minutes.
what are the 4 phases of the Interprandial period?
I : prolonged period of quiescence (lack of any motility)
II: increased frequency of contractility
III: a few minutes of peak electrical and mechanical activity
IV: declining activity merging to phase I
what is the Interprandial regulated by?
by the hormone Motilin
what is Motilin and what effect does it cause when triggering the Migrating Motor Complex (MMC)?
a polypeptide hormone, produced by M cells in small intestine. It is secreted at 90mins intervals. it cleanses the gut by initiating phase III of the MMC and it stimulates contractions of Gastric Fundus and enhances gastric emptying
what are the 3 functions of the stomach?
acts as a reservoir for large volumes of food
fragments food into smaller particles and mixes them with gastric secretions
empties gastric contents into Duodenum at a controlled rate
How can gastric accommodation of the gastric fondus and body of the stomach happen when volume increases WITHOUT increase in pressure?
due to Receptive Relaxation (neurophysiological reflex where the smooth muscle of the proximal stomach relaxes in anticipation of incoming food.
how does Gastric mixing occur?
muscle layers of upper stomach contract weakly. The contents form layers based on density, with fats floating to the top and emptying last.
How do gastric contractions happen and where are the strongest and where the weakest?
they occur due to Basal Electrical Rhythm arising from Interstitial cells of Cajal (ICCs/pacemaker cells) in the middle of the stomach. the contractions are the most powerful in the distal stomach (pylorus) than the proximal (the middle of the gastric body) where they begin
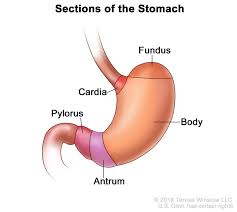
where does MAJOR mixing occur in the stomach, and what does the bolus become?
in the Antrum. the bolus becomes Chyme
what is the difference in gastric emptying between solids and liquids?
liquids leave stomach rapidly. Solids need to be regulated, as exposure of duodenum to acid can be harmful, and also to prevent over-release of insulin. Solids undergo mixing and churning with gastric juice. Food particles leave stomach when size is reduced to 2mm.
name and explain the 3 phases of meal related motility
-Cephalic: Secretory phase, Vagally mediated, sight/smell of food → increased gastric secretion (20% in this phase)
-Gastric: stomach expands. Migrating Motor Complex (cyclic pattern of contractions that clears residual contents) is suppressed and replaced by irregular and variable in amplitude contractions. The frequency and directions of these is controlled by Interstitial cells of Cajal (ICCs)., but they DON’T trigger muscle contraction, which occurs when there is neurohumoral input. ICCs generate rhythmic depolarisations (slow waves). Solids undergo mixing and churning.
-Intestinal
explain the process of Gastric emptying
•Antral pressures higher than gastric body and duodenum
•As intra-gastric pressure rises, pylorus opens up briefly
•Small amount of chyme passes to duodenum and most of gastric contents propelled back up into stomach for more settling and mixing
•Duodenal mucosa can sense acidity, osmotic pressure and presence of fats/amino acids (which cause increased pyloric pressure and reduced emptying)
(Presence of fat in duodenum inhibits gastric emptying)
what can result from Accelerated gastric emptying?
Dumping syndrome
diarrhoea
what can result from Delayed gastric emptying?
abdominal pain
vomiting
poorly controlled gastro-oesophageal reflux
malnutrition
what would be the red flags for a patient with upper GI symptoms?
•Anaemia
•weight loss
•Haematemesis
•Melaena
•Dysphagia
what is used by doctors to measure the risk of a patient having oesophageal cancer?
Edinburgh Dysphagia Score- triages patients with dysphagia (difficulty swallowing) by identifying those most likely to have oesophageal cancer
what is the MUST tool?
Malnutrition universal screening tool
What is Barium swallow test?
an X-ray procedure that uses a contrast liquid to examine the esophagus, stomach, and sometimes the upper part of the small intestine. The barium coats these organs, making them visible on X-ray images taken during fluoroscopy, a type of real-time X-ray. The test is used to diagnose swallowing difficulties and other issues like reflux and pain
what procedures are used as treatment for Achalasia?
Balloon Dilatation
Heller Myotomy (surgical repair- cutting the muscle fibers of the lower oesophageal sphincter (LES) to improve swallowing)
what is the labial franulum?
a mucosal fold (upper and lower) that connects the gingiva to the lips in the midline
name and explain the GENERAL model of cancer initiation for GI cancers, including the genes/mutations involved
Vogelstein model. Cancer is a disease driven by increased mutational load which is thought to be acquired in a linear fashion within tumour cells.
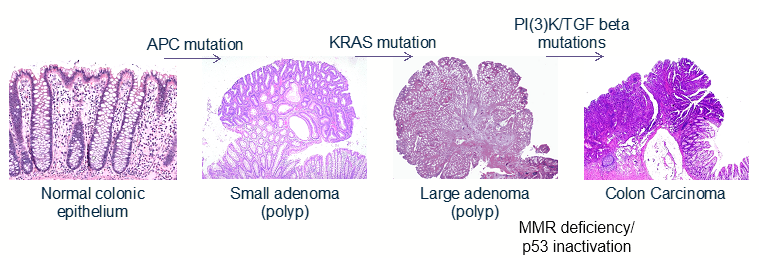
Explain APC’s role and involvement in cancer initiation
APC is a tumour suppressor that holds β-catenin in a complex along with GSK3β. When GSK3β
is phosphorylated it releases β-catenin from this complex to act as a transcription factor.
APC is the most common mutation seen in cancer and is usually the first mutation seen, and is therefore a driver mutation for many cancers
what common genes are mutated in cancer?
APC, RAS and RAF (eg. BRAF and KRAS in colorectal cancer, their mutation increases cancer cell proliferation), AKT and PTEN (eg. PTEN in prostate cancer promotes tumour progression), TGFb (attracts tumour promoting immune cells, as well as stromal cells into the tumour which promotes metastasis), p53 (usually the mutation that drives a benign growth to cancer, negatively regulated by mdm2)
what is the oral vestibule
space between the lips, cheeks and dental arches (frontally when teeth are shut)
what is the buccal frenulum?
they’re mucosal folds that are observed laterally (NOT labial frenulum, which is found in the midline)
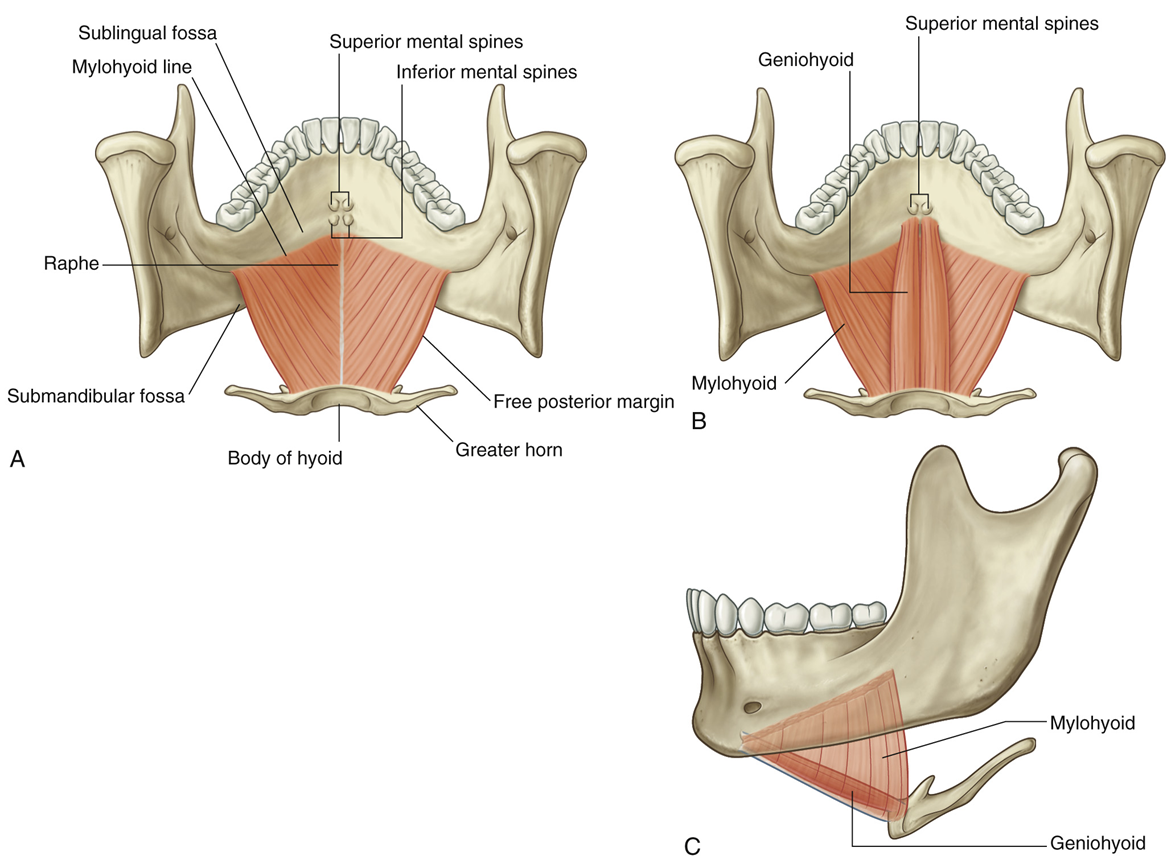
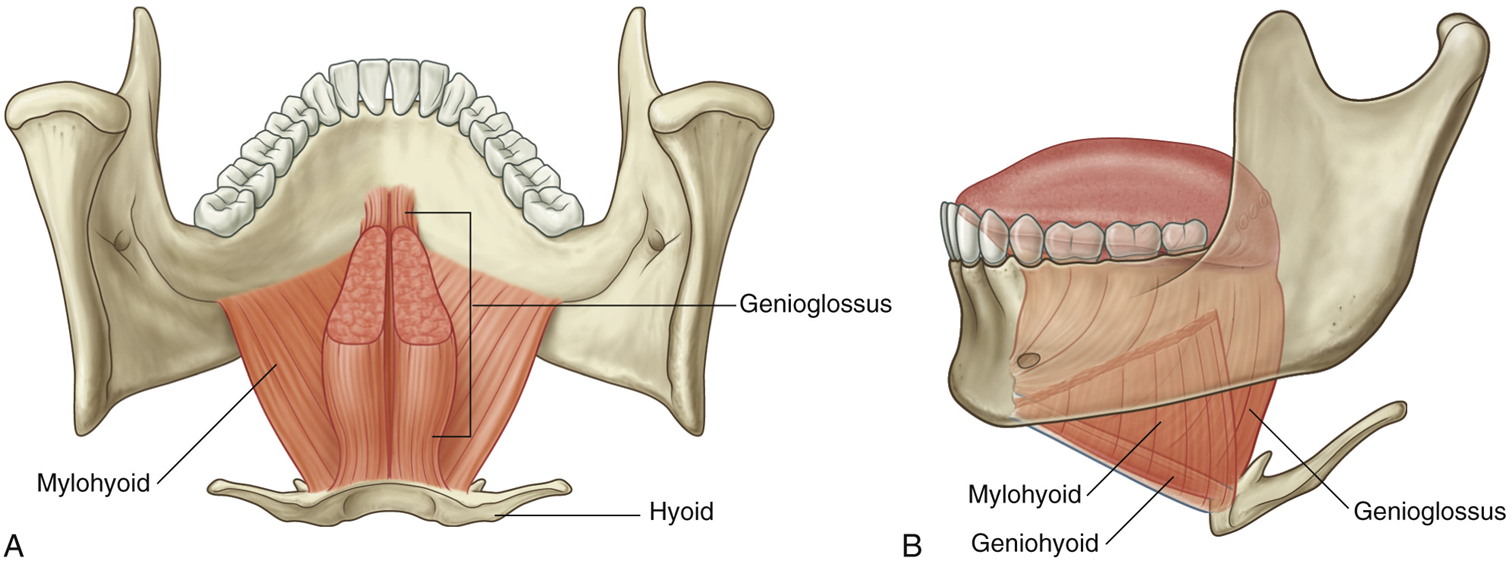
describe the floor of the oral cavity by naming its components
The floor of the mouth is formed by a muscular diaphragm created by the paired mylohyoid muscles
- These sits within the u-shape created by the mandible, attaching from the mylohyoid line of the mandible to the body of the hyoid
- The two mylohyoid muscles attach in the midline to the mylohyoid raphe
The geniohyoid muscles sit superior to the mylohyoid attaching from the inferior mental spine of mandible to the body of the hyoid
•Superior to both of these muscles is the tongue which is also a component of the floor of the oral cavity
describe the superior surface of the tongue
The anterior and posterior parts of the tongue are separated by the terminal sulcus.
Superior surface of the tongue is covered in papillae that help to grip food and house tastebuds:
Fungiform – ‘mushroom’
Foliate – folds of mucosa lining posteriorly and laterally on superior surface of tongue
Vallate – largest papillae, arranged in a V-shape anterior to terminal sulcus
Filiform – only papillae that does not have any tastebuds
describe the posterior surface of the tongue
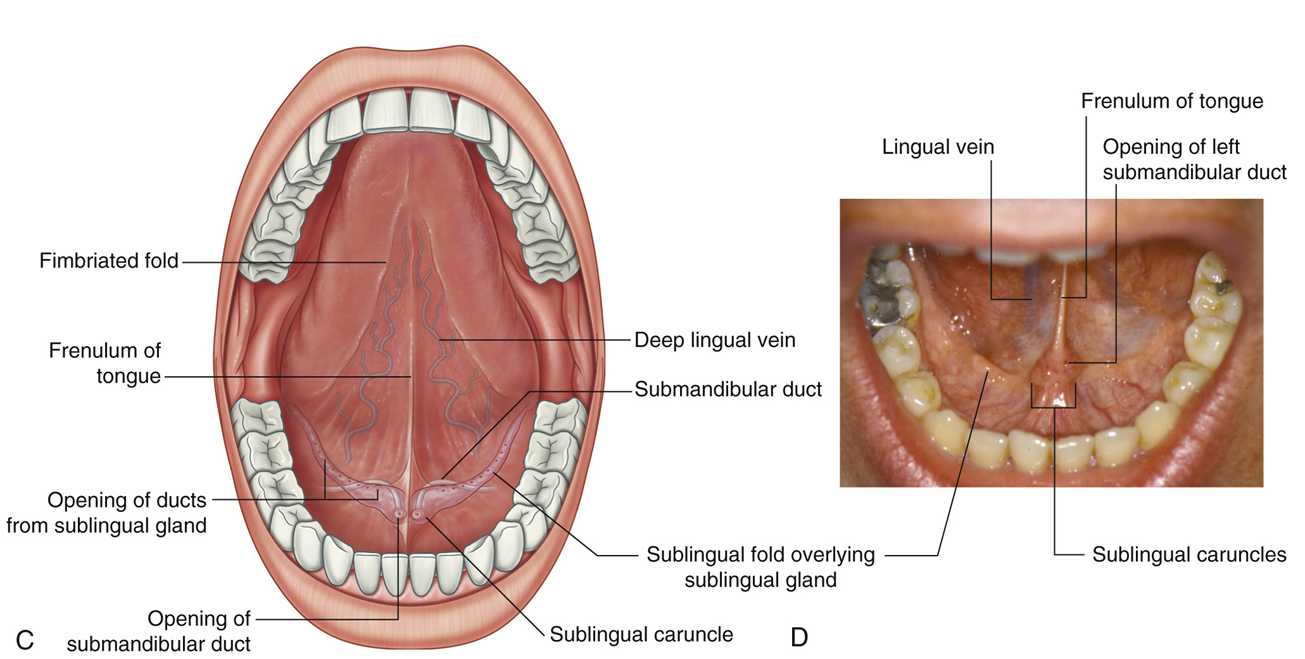
no papillae. The midline is marked by the frenulum of the tongue which extends from the inferior surface of the tongue, along the midline, and is continuous with the mucosa of the floor of the mouth
On each side of the frenulum the lingual vein can be seen as well as sublingual folds.
name and describe the intrinsic and extrinsic muscles of the tongue
the intrinsic and extrinsic muscles are separated by the sagittal septum.
Intrinsic muscles change the size and shape of the tongue:
Superior longitudinal / Vertical / Transverse / Inferior longitudinal
Extrinsic muscles of the tongue originate from outside of the tongue and are responsible for protruding, retracting, elevating and depressing the tongue:
Palatoglossus / Styloglossus / Hyoglossus / Genioglossus
describe the genioglossus
Superior to the geniohyoid muscles
Originates from the superior mental spines of the mandible
Inferior fibers attach to the hyoid bone while superior fibers blend with the intrinsic muscles of the tongue
Genioglossus muscles is important in protruding the tongue
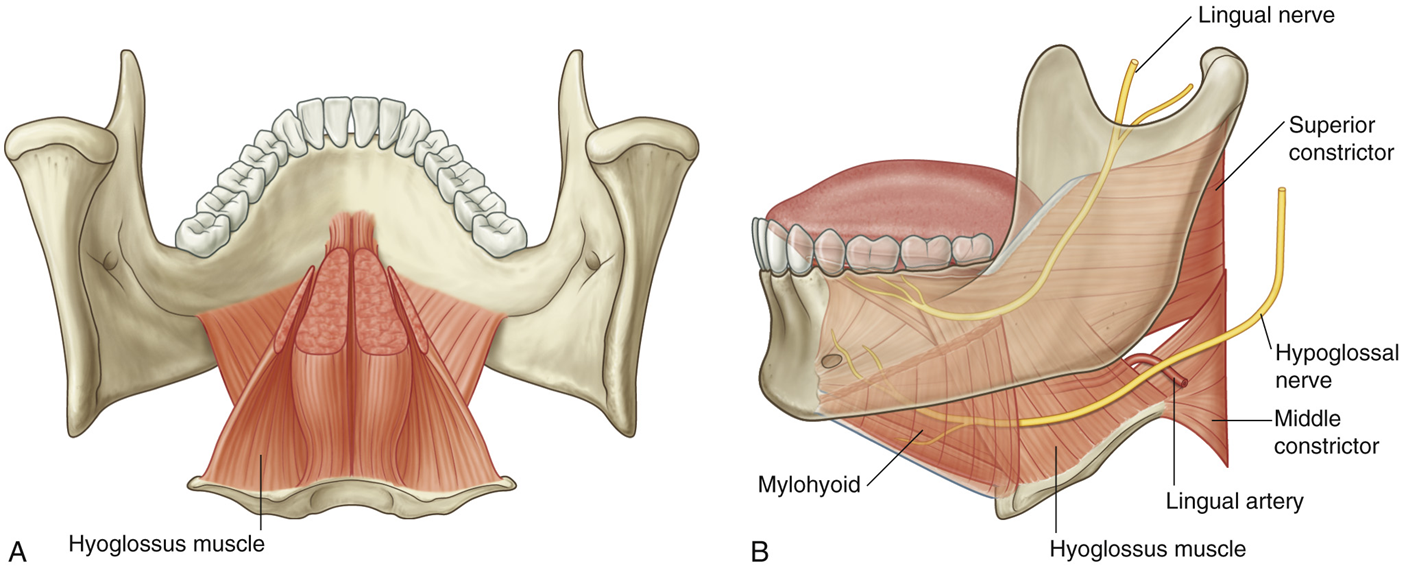
describe the Hyoglossus, and the relation in position of the lingual artery and hypoglossal and lingual nerves
Lateral to the genioglossus muscles, it originates from greater horn of hyoid and fibers blend with intrinsic muscles on the lateral aspects of the tongue
It is important for depressing the sides of the tongue.
the lingual artery, the major arterial supply to the tongue from the external carotid, enters the tongue between the hyoglossus and genioglossus muscles.
The hypoglossal and lingual nerves enter the tongue on the external surface of the hyoglossus.
describe the Styloglossus
Originates from the styloid process of temporal bone
Its fibers blend with the intrinsic muscles of the tongue and the superior fibers of the hyoglossus
Styloglossus muscles is important in elevating and retracting the tongue
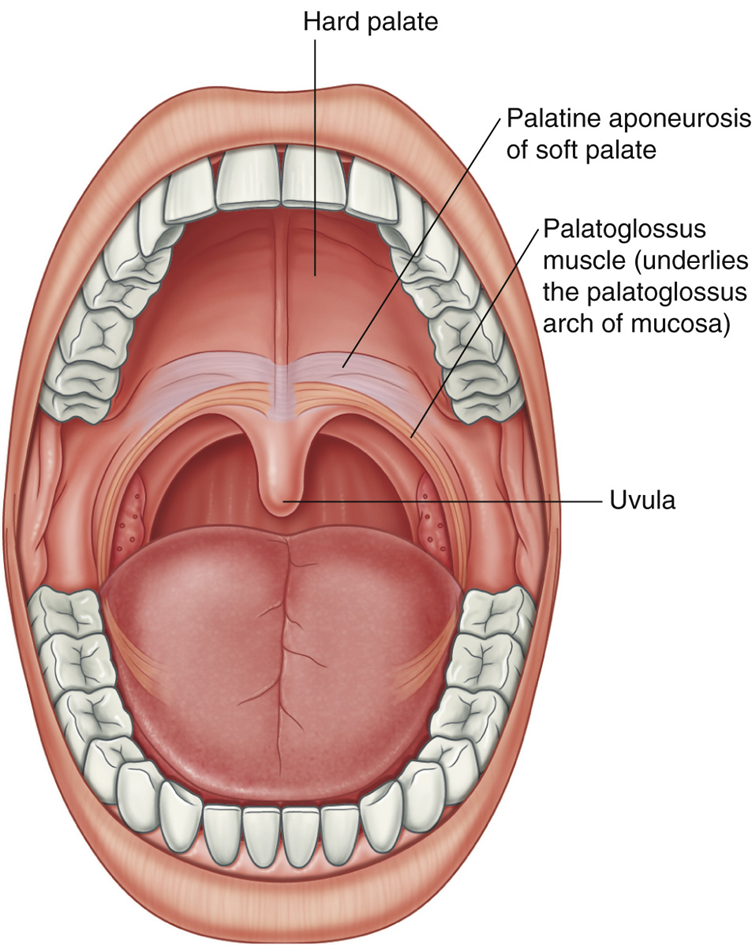
describe the Palatoglossus
The palatoglossal muscle is a muscle of the tongue AND the soft palate
Its origin is from the palatine aponeurosis, a fibrous tissue on the posterior border of the hard palate
Its fibers pass inferiorly to blend with intrinsic muscles on the lateral surface of the tongue
Elevates the root of tongue and constricts the isthmus of fauces (narrow passage connecting the oral cavity to the oropharynx)
explain the innervation to the tongue
Motor
All muscles of the tongue are supplied by the hypoglossal nerve EXCEPT palatoglossus muscle which is supplied by the vagus nerve
General Sensation (pressure, temperature, pain)
Ant 2/3 – Mandibular nerve (trigeminal)
Post 1/3 – Glossopharyngeal nerve
Special sensation (taste)
Ant 2/3 – Facial nerve via chordae tympani
Post 1/3 – Glossopharyngeal nerve
outline the blood supply of the tongue
The lingual artery is the major arterial supply to the tongue (from the external carotid)
The deep lingual and dorsal lingual veins drain the tongue (both drain into the internal jugular vein)
outline the oesophagus and the structures along its course
The oesophagus is a 20-25cm muscular tube connecting the pharynx to the stomach
2nd narrowest point of the GI tract and has several strictures along its course:
Cricopharyngeus (15cm) [not part of the esophagus; it is the primary muscle that forms the upper esophageal sphincter (UES), which sits at the junction between the pharynx and the esophagus.]
Aortic arch (23cm)
Left main bronchus (28cm)
Diaphragmatic hiatus (40cm)
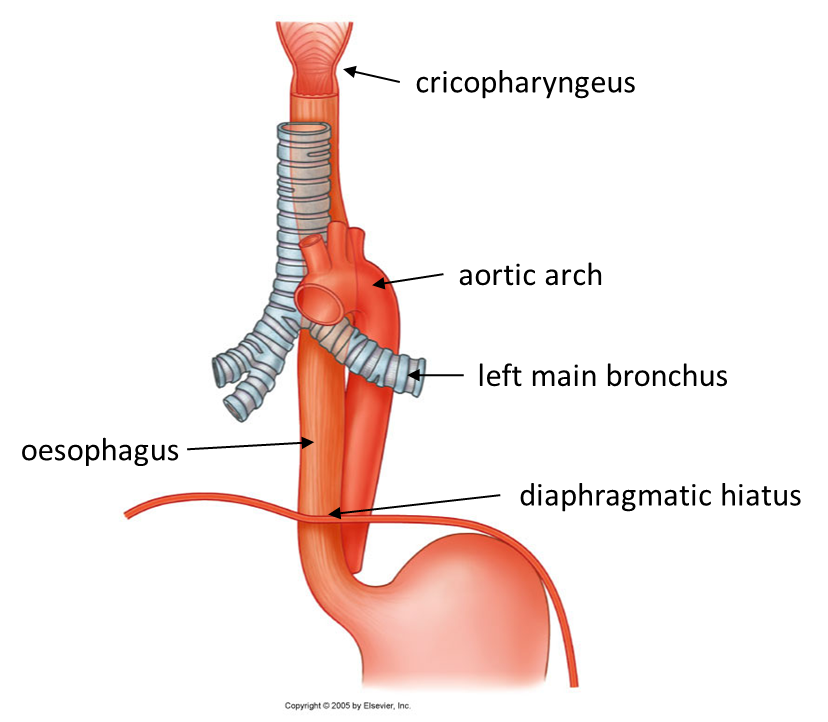
outline the blood supply and innervation of the oesophagus
Blood supply from oesophageal branches direct from the aorta
Venous drainage mostly into the azygous system
Innervation from vagus nerve plexuses
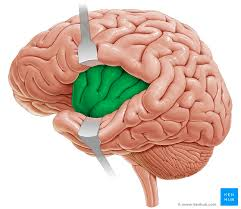
The perception of taste can be mapped to a specific region of the brain. The Primary Gustatory Cortex is located at which gyrus?
insula gyrus and inferior frontal gyrus

With Barret's Oesophagus, a precursor to oesophageal cancer, chronic inflammation can lead to cellular metaplasia, with cells changing from one type to another type.
In Barret's, stratified squamous epithelium can change to what other type of epithelium?
simple columnar epithelium
what are the 3 major salivary glands and their functions
3 major paired glands
Parotid
Submandibular
Sublingual
Produce serous, mucous, or mixed fluid
Functions:
lubrication
deglutition
digestive enzymes
aqueous solvent - taste
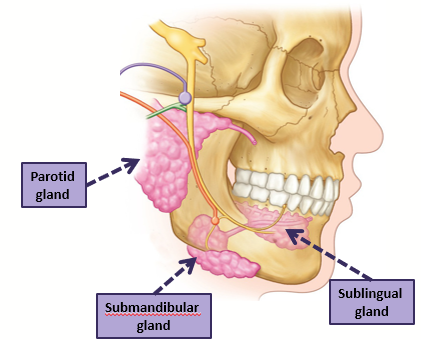
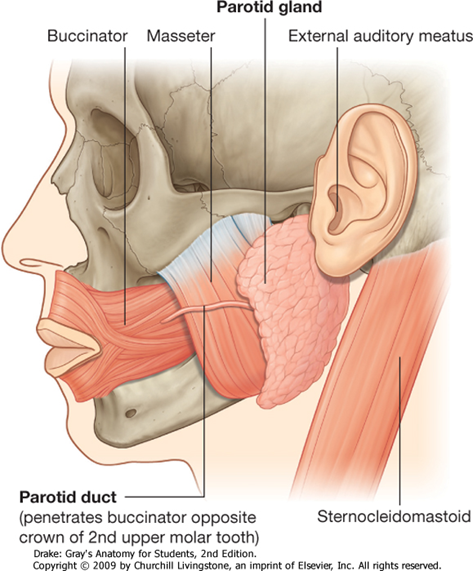
explain the parotid gland
•Largest of the salivary glands, almost entirely serous secretions, no mucus
•Enclosed in parotid sheath
•Parotid duct – pierces buccinator to enter the oral cavity near the upper 2nd molar tooth
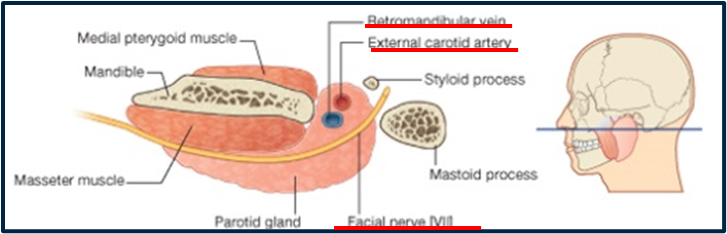
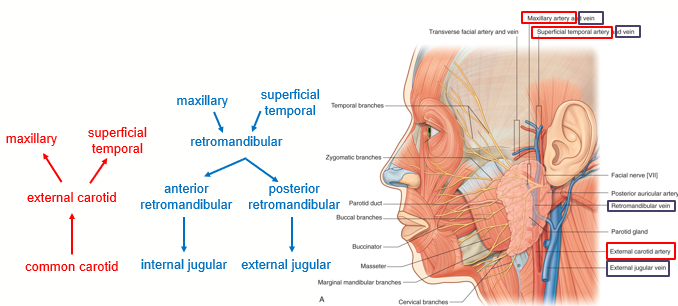
what structures are embedded in the parotid gland?
Within the parotid gland, several structures are embedded:
•CN VII – but does not innervate!
•Retromandibular vein
•External carotid artery
•Parotid lymph nodes
describe the blood supply and drainage of the parotid gland
Maxillary and superficial temporal vessels
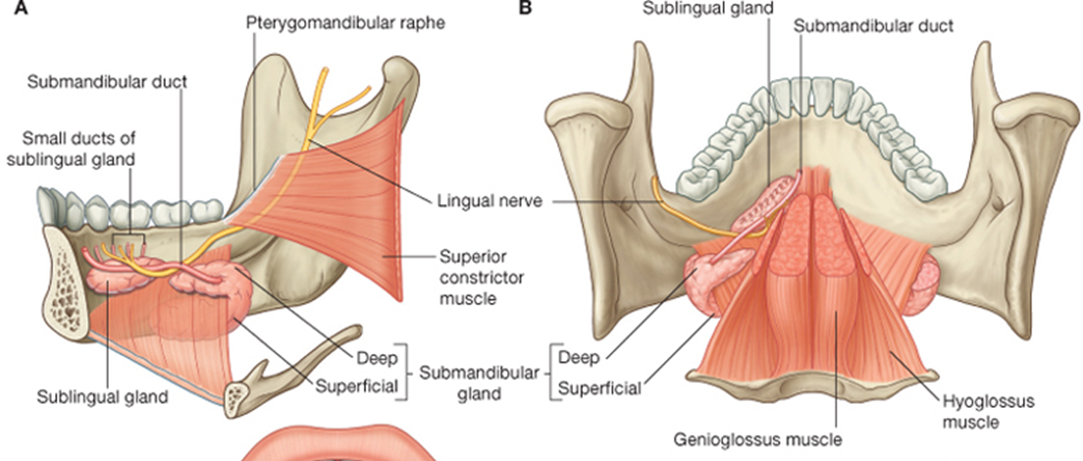
explain the submandibular gland
•Wraps around mylohyoid
•Mixed serous & mucus secretions
•Fascial sheath
•5cm duct travels between mylohyoid and hyoglossus
•Lingual nerve (CN V3) loops under the duct before it opens into the oral cavity
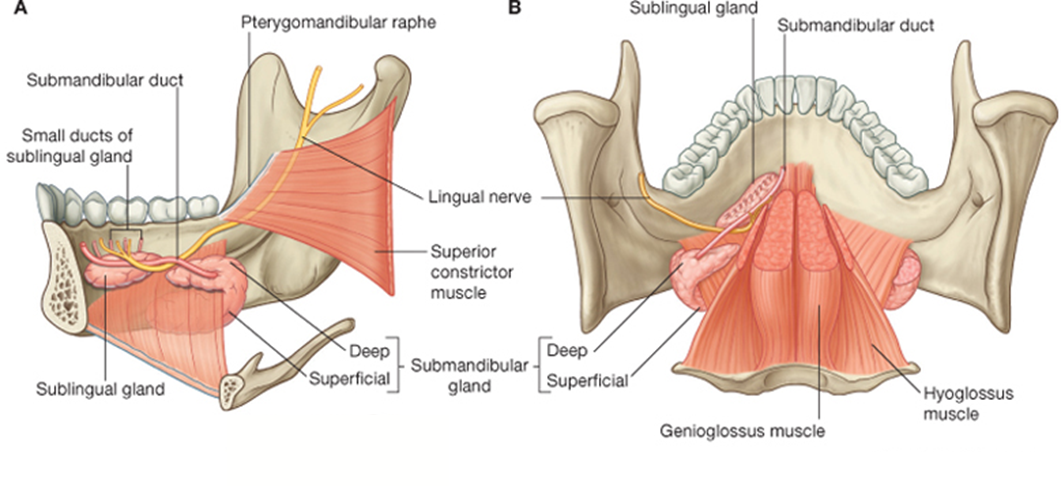
explain the sublingual gland
•Smallest of major salivary glands
•Mostly mucus, some serous secretions
•No fascial sheath
•Numerous small ducts
•Sits lateral in floor of mouth, in sublingual fossa of mandible
whare are accessory salivary glands found?
found diffusely embedded throughout the submucosa of the oral cavity:
•Buccal (cheek)
•Palatine (palate)
•Lingual (tongue)
•Labial (lip)