Psych Exam 2: Suicide, Depression, Bipolar, Addiction
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Describe what suicide is vs suicidal ideation
Suicide is the intentional act of killing oneself
Suicidal Ideation is having THOUGHTS of committing suicide.
What are risk factors of suicide: (5)
Older adults
untreated depression
no job/ finances
feel isolated/powerless
decline in physical health
lose loved ones
fam hx suicide
poor relationships at home, school, work
hx trauma/ abuse
access to lethal methods (firearms)
Warning signs of Suicide: (7)
Withdrawing from fam and friends socially
Giving away possessions
Bidding goodbye to fam/friends
Feeling like "Burden” to others
Engaging in risky behavior
Obsessively thinking/talking abt death
Hx of suicidal attempts
Inpatient hospitalization safety: (2)
One-to-One line of sight surveillance or at least monitor q15 min
Monitor and take away harmful objects
How would a person act what they have Major Depressive Disorder? (11)
Depressed mood (almost everyday)
Can’t sleep or oversleeping
Indecisive
Can’t concentrate
Suicidal ideation (always ask upfront!)
Increased or decreased MOTOR activity
Hard to feel pleasure
Increase or decreased weight
Unkempt appearance
Hard to complete ADLs
Depressed w/ psychosis
Those most at risk for depression: (7)
Females
Unmarried
Low socioeconomic class
Early childhood trauma
Fam hx of depression
Postpartum period
Medical Illness (Comorbidities→ DM, COPD, HF)
Nursing assessments for depression: (4)
Assess suicide risk ALWAYS!!
See if they have a plan/ method
Implement safety precautions
Assess severity
Plan of care for depressed client: (5)
Patient-Centered Holistic Care
consider whole person (emotional, social, financial factors that’ll affect health)
Partnership:
pts need to actively engage in tx process
go to follow up apps.
attend therapy
med adherence
Respect and Dignity
Effective communication:
clear and Empathetic!!
active listening
OEQs
Silence
Clarifying/Summarizing
Frequent check ins
Assist w/ ADLs
Anti-depressant meds: (5)
SSRIs
SNRIs
Tricyclic Antidepressants
Atypicals
MAOIs
Whens ECT therapy used? (3)
When other treatments fail (aka medications)
used for depression
bipolar
seizures
Side effects ECT: (3)
Temporary memory loss
HA
Confused
Patient education for ECT: (5)
Lasts 25 secs
NPO 4-8 hrs B4
Supine on tx table IV anesthesia and muscle relaxant
maintain ventilation
Post-procudure: awake in 10-15 mins
May sleep for 1-2 hrs after proceudre
Bipolar I Disorder describe it:
→ has had at least one time when they felt extremely energetic or “on top of the world” (that’s a manic episode)
→ and at some other point, they’ve also felt either a smaller burst of energy or a deep sadness and loss of interest (a depressive episode).
Describe Bipolar II Disorder:
→ has had at least one really low period where they felt very sad or hopeless (a depressive episode)
→ and at least one period of feeling extra happy or energetic, but not as extreme as full mania (a hypomanic episode).
may experience prolonged depression!!**********
What emotions would a person experiencing Mania show? (9)
Fellings of elation
Infalted self-esteem (cocky)
Delusions
Grandiosity (super powers)
Hyperactive
Agitated
Flight of Ideas
Accelerated speech
Easily distracted
How would a manic person ACT on a daily basis? (6)
Impulsive:
spending money, or giving away stuff
Demanding and manipulative
Distracted and bad attention span
Seeks attention
flashy dress and makeup
inappropriate behavior
Decreased sleep
2-3 hrs/day or go days w/o sleep
Neglect ADLs
nutrition (anorexia)
hydration
leads to exhaustion or risk of death
Nursing Assessment of Mania progression:
stage 1 (4)
stage 2 (4)
stage 3 (3)
Stage 1: Hypomania
Super happy, talks a lot, full of energy
Easily distracted (“Ooh shiny!”)
Gets irritated fast if interrupted
Still kinda normal — just extra
Stage 2: Acute Mania
Thinks they’re unstoppable — no guilt, no limits
Acts wild or inappropriate (flirty, rude, spending sprees)
Doesn’t sleep, blames everyone else
Very labile
Stage 3: Delirious Mania
Can’t think straight — confused, panicky, maybe hallucinating
So hyper they’re exhausted, may collapse
Dangerous — might hurt self or others
Nursing Diagnosis for mania: (7)
Risk for injury
take away harmful stuff
assess SI!!
give frequent rest periods
Risk for violence
Imbalance nutrition
Disturbed Thought process
Disturbed Sensory Perception (hallucinate)
Impaired Social Interaction
Insomnia
Nursing care for Impaired social interaction in MANIC pt: (4)
Set limits on manipulative behavior/expectations of rules on unit
Dont argue****
Dont bargain/ reason w/ pt****
Decrease stimulation w/o isolating pt*****
Give positive reinforcement!
Nursing care—Mania and risk for violence: (5)
Take away harmful objects
Calm attitude
Address inappropriate behavior ASAP
first offer options then consequences follow
If restraints needed, make sure staff is nearby to help
Goal is to help pt verbalize inappropriate behaviors and demonstrate appropriate interaction skills and self-awareness
Nursing implementation for those at risk for imbalanced nutrition in MANIC pt (6)
Give high-protein, high cal foods****
bc pt is hyperactive and will neglect nutrition
Finger foods
Protein drinks
Record I/O and calorie count
No caffeinated drinks!
Help achieve 6-8 hrs of sleep w/o interruption
Meds for Mania: (3)
lithium
anticonvulsants:
lamotrigine
valproate
What do u assess/monitor for when pt is on Valproic Acid?
LIVER function!!!
LFTs q2 months
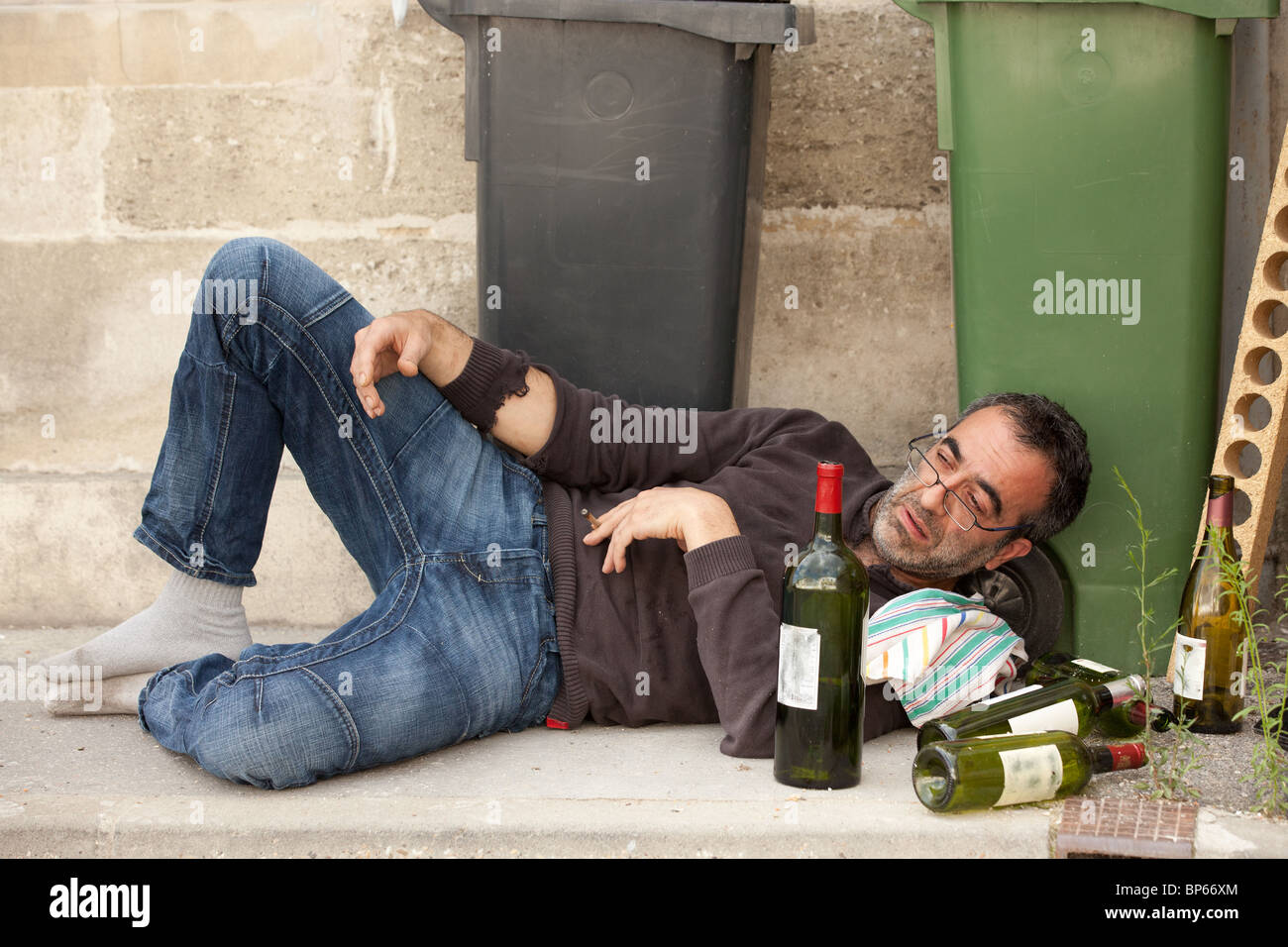
Alcohol s/s intoxication: (6)
Slurred speech
Poor coordination (stumbling, can’t walk straight)
Slow reaction time
Mood changes (happy, angry, silly, etc.)
Drowsiness or confusion
N/V
“everything slows down”
Alcohol Withdrawal s/s: (8)
Tremors or shaking (especially hands)
Sweating (high temp)
Restlessness
Fast heart rate
Seizures
HTN
Trouble sleeping
Delusions/Hallucinations
Delirium
“speeds up”

tx alcohol withdrawal (4) vs maintenance (2)
Withdrawal:
give benzos
lorazepam
anticonvulsants
valproic acid
Abstinence
N-acetylcysteine (OTC)
Maintenance:
Naltrexone: decrease alc craving
Disulfiram (Antabuse): causes unpleasant physical effects when you drink
Stimulant s/s abuse: (7)
DILATED pupils
DRY oronasal cavity
Excessive MOTOR activity
hyperactive
hypervigilance (super aware of surroundings, fight or flight mode constantly
interpersonal sensitivity
someone is easily hurt, worried, or anxious about how others see them
euphoric
-coke/crack**

Stimulant withdrawal s/s: (8)
“Crashing”
depressed/fatigue
agitated
cramps
HA
Nightmares
disoriented
cravings
lethargic
Opioid abuse s/s: (7)
“Pinpoint” pupils
Decreased RR, BP
Slurred speech
Drowsy
Psychomotor retardation (everything slowww asf)
euphoric then dysphoria
feeling great at first, then crashing afterward.
Impaired concentration, Judgement, Memory
slows down

Opioid Withdrawal effects: (9)
Yawning
Insomnia
Panic
Rhinorrhea
Diaphoresis
Lacrimation
Cramps
Muscle Aches
Chills/Fever
speeds up
Hallucinogens-what are the types? (3)
LSD
Psilocybin (magic mushroom)
Phencyclidine Piperidine (PCP, Angle dust, horse tranquilizer, peace pill)
“mind expanding drugs”
visual
flashbacks
Hallucinogen abuse s/s physical effects: (7)
Chills
Pupils DILATED-like stimulants
Increased HR, RR, BP, Temp, Blood sugar
Dizzy
Trembling/ Sweating
No Appetite
Insomnia
Hallucinogen abuse Mental effects s/s:
Heightened response to color, sounds, texture, body awareness
Distorted vision
Sense of slowed time
Magnified feelings
Fear of control loss
Paranoid
Serenity, Euphoria
Depersonalization
Derealization
Increased Libido

Self-Help groups for substance abuse:
Alcoholics Anonymous
12 step program
steps include things like admitting there’s a problem
asking for help
making amends to people they’ve hurt
committing to stay sober.
need a sponsor
personal mentor who’s been through it before.
NA basically same as AA