shit to know week 4 (a girl is tired...)
1/137
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
138 Terms
which muscle opens the eye
levator palpebrae
which muscle closes the eye
orbicularis oculi
which muscle of the eyelid may be affected in horner syndrome
superior tarsal muscle which joins the levator palpebrae → ptosis
also iris dilator muscles
which part of the eye contains the meibomian glands
tarsus
ptosis palpebrae
drooping eyelid, different causes
congenital
eyelid doesnt move when glancing down
underdeveloped affected eyelid
usually due to aplasia of oculomotor n (neurogenic) or less commonly underdeveloped levator (myogenic)
acquired
paralytic ptosis = neurogenic = oculomotor palsy
if its complete palsy then the inner ciliary muscles and sphincter papillae muscles are also affected on top of the levator
sympathetic ptosis = neurogenic, eg. due to Horner syndrome
myotonic ptosis eg. due to myasthenia gravis
traumatic ptosis
unilateral ptosis is usually a sign of x
neurogenic causes
how can you distinguish congenital ptosis palpebrae from acquired
in congenital, the upper eyelid doesnt move when they glance down
there is a risk of x in unilateral congenital ptosis
amblyopia
amblyopia
reduced vision in one eye caused by abnormal visual development early in life
why does amblyopia not occur in bilateral ptosis
because they would typically tilt their head back to see and not only one eye is affected
triad in horner syndrome
ptosis, miosis and anhidrosis
enophthalmos (eye sinking into socket) also occurs
which nerve innervates the levator palpebrae
oculomotor nerve
which nerve innervates the orbicularis oculi
facial nerve
entropion
inversion of the eyelid margin → skin touches not only the bulbar conjunctiva but also the globe
congenital
usually asymptomatic
seen commonly in asians
due to thickening of the skin and orbicularis m near the margin of the eyelid
rarely needs treatment
senile
only affects the lower eyelid
eg. due to structures supporting the lower lid becoming lax with age
cicatricial entropion
usually due to post infectious or traumatic tarsal contracture (also allergic/toxic reactions)
what may occur w/ entropion
blephorospasms due to permanent contact between eyelashes and globe (trichiasis)
there is a risk of x in entropion
corneal epithelial damage w/ superinfection which may become a corneal ulcer
disorders of the eyelid glands
hordeolum (stye)
= acute bacterial infection of the eyelid glands
painful
internal = infection of Zeis or Moll glands → more severe reaction → conjunctivitis etc may occur
external = infection of Meibomian glands = near the eyelashes
often associated with DM, acne and GI disorders
treat w/ antibiotics
chalazion
= formation of a firm nodular bulb within the tarsus (eyelid) due to chronic granulomatous inflammation due to build up of secretion from the meibomian gland
not painful, usually asymptomatic
surgical excision must be done
parts of the lacrimal system
lacrimal gland = orbital and palpebral part
meibomian glands
inferior and superior punctum lacrimale collect the fluid → enters inferior and superior lacrimal lacrimal canaliculus → into the lacrimal sac → nasolacrimal duct and out
the eye closes progressively from x to x
lateral to medial
allows tear fluid to move towards the medial conthus and then out
tear film
layer 1 → oil layer from the meibomiab glands (and sebaceous and sweat glands) → stabilises tear film, stops evaporation
layer 2 → serous layer from the lacrimal gland → protects cornea + allows for smooth surface for high quality optical images
layer 3 → mucin layer from the conjunctival goblet cells → stabilises tear film + allows for even distribution of the watery layer
also contains lysozymes, beta lysin and IgA
dacryocystitis
= inflammation of the lacrimal sac
most common disorder of the lower lacrimal system
obstruction of the nasolacrimal duct is the most common cause
acute
usually due to stenosis within the lacrimal sac → retention of fluid → infection from staph etc
usually 50-60 y/o
painful swelling
maybe malaise, fever and involvement of regional lymph nodes
diagnosis → radiographic contrast studies
start w/ local and systemic antibiotics first, maybe disinfectant compresses
drain pus
post op treatment is often needed → dacryocystorhinostomy = lower system bypass
risk of sepsis and cavernous sinus thrombosis
chronic
obstruction secondary to chronic inflammation of the connective tissue or nasal mucosa
initial characteristic = increased lacrimation
pressure causes large amounts of transparent mucoid pus to come out the punctum
no signs of inflammation
surgical intervention is the only effective treatment in most cases
neonatal
6% of newborns have a stenosis of the mouth of the nasolacrimal duct due to a persistent mucosal fold → retention of tear fluid → ideal conditions for growth of miroorganisms
might open spontaneously (massaging also helps) so monitor at first, if needed → irrigation or probing
what is the most common disorder of the lower lacrimal system
dacryocystitis
what is the most common cause of dacryocystitis
obstruction of the nasolacrimal duct, usually unilateral
dacryocystorhinostomy
lower lacrimal system bypass
keratoconjunctivitis sicca
= chronic bilateral desiccation (drying) of conjunctiva and cornea due to too little tear production, wrong composition of tear film/ accelerated tear evaporation
reduced tear production is associated w/ systemic disorders or due to atrophy of the lacrimal gland
altered tear film can be due to vitamin a deficiency, medication etc → tear film breaks up too quickly and evaporates
burning reddened eyes, excessive REFLEX lacrimation from slight environmental causes, foreign body sensation
tests → schrimer tear testing = less watery component, tear break up time = less mucin = less stability, slit lamp shows dilated conjunctival vessels
may show corneal lesions
in severe cases the tear film will contain thick mucus and small filaments from small epithelial lesions, seen with fluorescein dye
treat with artificial tear solutions
if it doesnt work → close the puncta
there is reflex … in keratoconjunctivitis sicca
lacrimation
what can happen in keratoconjunctivitis sicca
corneal lesions
how to test for keratoconjunctivitis sicca
schrimer tear testing = less watery component
tear break up time = decreased = less mucin = less stability
rose bengal → dyes dead epithelial cells and mucin
impression cytology → tests the density of goblet cells
these top 4 are used to evaluate tear formation in all cases, last 2 are mainly for KS but may also be in general
slit lamp shows dilated conjunctival vessels
in severe cases the tear film will contain thick mucus and small filaments from small epithelial lesions, seen with fluorescein dye
keratoconjunctivitis sicca occurs more commonly in …
women due to hormonal changes
aqueous humor
released by the ciliary processes → into posterior chamber → through the first resistance (pupillary resistance) ie bypassing the place where the iris and lens meet → into anterior chamber → drained by the trabecular meshwork (2nd resistance)
nourishes and protects the eye
is aqueous humour flow pulsatile
yes
production is continuous but due to 1st resistance its pulsatile flow
normal occular p
15
zonule fibres
insert into the lens from the ciliary body
the lens lies in the…
posterior chamber
cataracts
= decreased opacity of the lens
99% are acquired and 90% of the total are senile
only treatment is surgery
generalised reduction in visual acuity with starbursts around lights
how does the lens grow
centre out
so older nuclei (embryonic nucleus) is in the centre while the adult nucleus is on the periphery
zonular fibres vs suspensory ligaments
the same thing
uvea
iris + choroid + ciliary muscles
senile cataracts
nuclear/sclerotic
starts from the centre and spreads
slow progression
pressure of peripheral lens fibre production causes hardening of lens especially in the lens → nucleus becomes yellow brown ish
the refractive power increases due to compaction of older fibres and apposition of new bones → myopia and maybe diplopia
cortical
due to changes in the ionic composition of the lens cortex and the eventual change in hydration of the lens fibers = increased water content
radial patterns of water filled fissures between fibres
separation of lamellae by fluid
posterior subcapsular
special forms of ^
due to formation of granular and plaque like opacities in the posterior subcapsular cortex
begins in the visual axis
leads to early rapid and severe visual acuity but dilating eye drops can help
mature cataracts
means the lens has undergone complete opacification of the cortex
diffusely white lens
risk of angle closure glaucoma
mature cataracts → increase in lens thickness → increase in resistance of pupil → angle closure glaucoma
can only see light and dark w/o surgery
hypermature/morgagni
when mature cataracts reaches the liquefecation stage → dense brown nucleus will subside and move inferiorly
fluid leaks out
can cause phacolytic glaucoma
how does cataracts affect vision
cloudy lens → increased refractive power → light scatters upon entering (sort of myopia?) → blurry image
mature cataracts has a risk of …
angle closure glaucoma
mature cataracts → increase in lens thickness → increase in resistance of pupil → angle closure glaucoma
how does the refrative power of the lens change with cataracts
increases → myopia and maybe diplopia
due to compaction of older fibres and apposition of new bones
how is congenital cataracts screened for
red reflex
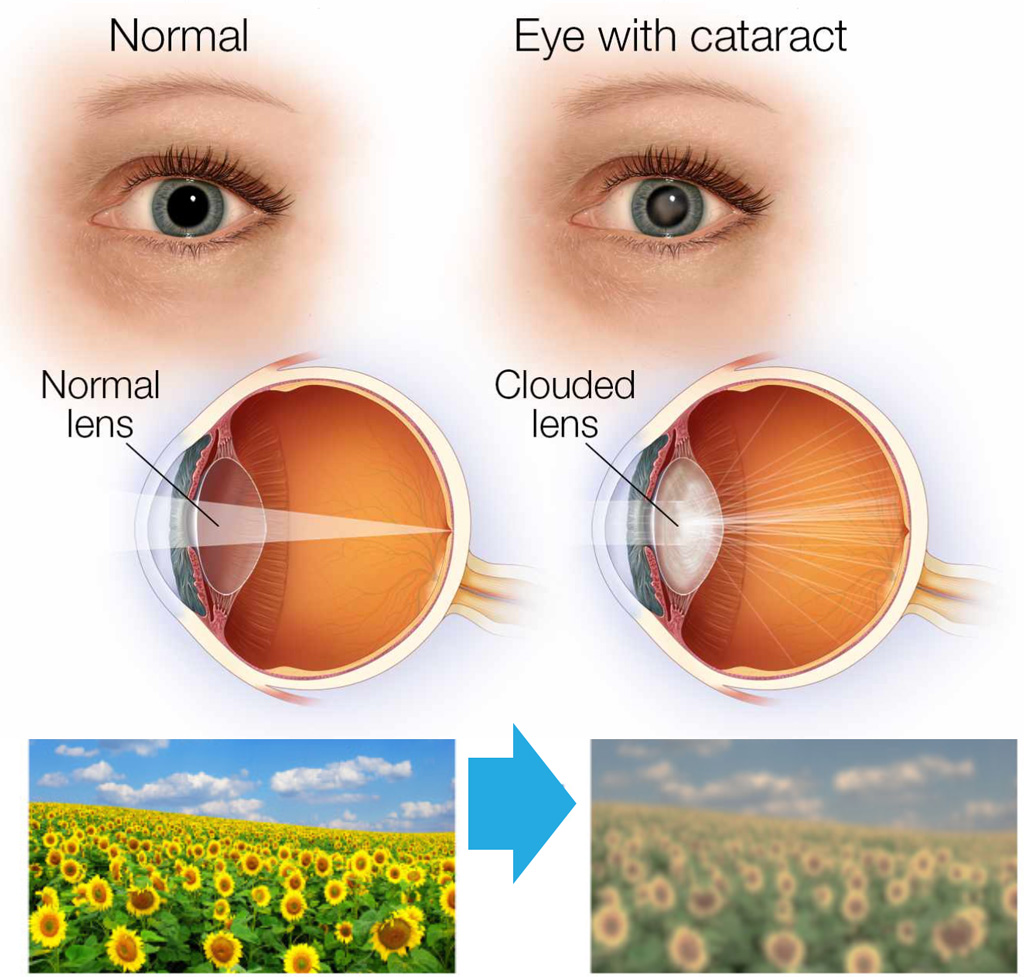
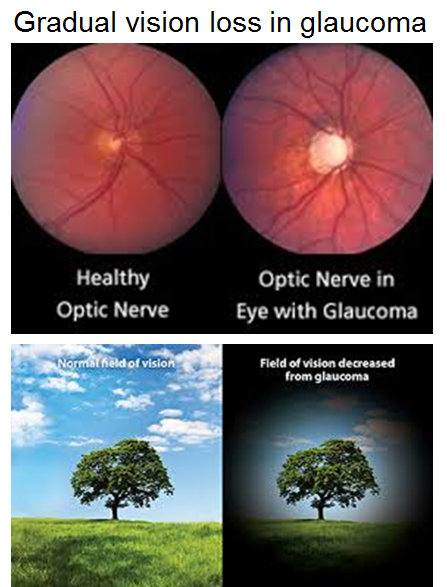
cataracts vs glaucoma vs macular degeneration
Cataracts cause a generalised reduction in visual acuity with starbursts around lights
Glaucoma causes a peripheral loss of vision with halos around lights
Macular degeneration causes a central loss of vision with a crooked or wavy appearance to straight lines
it would be like a black dot in the middle
congenital cataracts can be either x or x
hereditary or acquired transplacentally from an infection
secondary cataracts
can occur after extracapular catarct extractions bc only the anterior central portion is removed → leftover ells
treat with laser
the blind spot is
the optic cup / disc
part of the retina with highest visual quality
fovea
the fovea is within the…
macula
why does glaucoma change the optic area
glaucoma = increased intraocular pressure and decreased blood flow to the optic n → tissue atrophy and fibre death → increase in optic CUP size (+ pale discolouration)
changes in ophthalmoscopy in glaucoma
optic cup size increases → ratio to optic disc decreases
optic cup becomes brighter
optic disc becomes oval shaped
blood vessels abruptly plunge into the deep cup
cup/disc move more nasally / away from the fovea towards the midline
how does the fovea sit in relation to the optic disc
fovea is lateral/temporal to the optic disc
a visual defect in glaucoma is…
the beginning of the end
most common type of glaucoma
primary open angle glaucoma = trabecular meshwork outflow impediment
factors that increase resistance to pupillary outflow = risk of angle closure glaucoma
increased contact between the margin of the pupil and lens →
small eyes
large lens
miosis (small pupil)
posterior synechiae = adhesions between lens and iris
increased viscosity of the aqeuous humour due to inflammation or bleeding
primary open angle glaucoma
problem in 2nd physiological resistance
middle aged and elderly patients
most common glaucoma
minimal symptoms that worsen progressively
many dont experience symptoms at first → can be far advanced before noticed
maybe non specific symptoms (headache, burning eyes, blurred vision)
rings of colour around light sources at night are characteristic
intraocular p > 22
fluctuations in 24 hr pressure curve → fluctuations >5-6 mm Hg = warning sign
gonioscopy → normal and open anterior chamber angle
ophthalmoscopy → glaucomatous cupping
perimetry → visual field → peripheral loss
x is characteristic in glaucoma
rings of colour around light sources at night
introcular p over x is a warning sign for glaucoma
22
what, other than intraocular p, can be measured in glaucoma
fluctuations in 24 hr pressure curve → fluctuations >5-6 mm Hg = warning sign
gonioscopy shows…
anterior angle chamber
primary angle closure glaucoma
= problem in 1st physiological resistance =
associated with a physically obstructed anterior chamber angle
acute episodic increase in IOP due to sudden blockage
due to widening of the pupil (eg. darkness or stress) → When the iris dilates, forces pull the iris centripetally and posteriorly causing increasing iris–lens contact, which prevents aqueous from passing between the lens and iris, through the pupil, and into the anterior chamber
iris kind of looks like 2 hills on top of the lens
increased IOP also acts on the corneal nerves → pain
may also affect the other branches of the trigeminal nerve
irritation of the vagus n may cauase nausea and vomiting
corneal epithelial oedema → decreased (peripheral) visual acuity and halos
triad → unilateral red eye w/ conjunctival or ciliary injection + fixed and dilated pupil + hard pupil on dilation
what causes an attack in angle closure glaucoma
When the iris dilates, forces pull the iris centripetally and posteriorly causing increasing iris–lens contact, which prevents aqueous from passing between the lens and iris, through the pupil, and into the anterior chamber
= episodic increase in IOP, due to darkness or emotional stress
angle closure glaucoma triad
unilateral red eye w/ conjunctival or ciliary injection + fixed and dilated pupil + hard pupil on dilation
conjunctivitis
inflammatory process involving the surface of the eye
characterised by vascular dilatation, cellular infiltration and exudation
2 categories → infectious and not (persistent irritation, allergic, toxic etc)
reddened eyes, sticky eyelids, swollen eyelids, foreign body sensation, burning sensation, photophobia and lacrimation
simultaneous presence of blephorospasm means theres corneal involvement = keratoconjunctivitis
what is present in all types of conjunctivitis
injections
if there is blephotospasm in conjunctivitis…
it means theres corneal involvement = keratoconjunctivitis
the limbus is…
the border between the cornea and conjunctiva
pinguecula
harmless, greyish yellow thickening of the conjuctival epithelium in the palpebral fissue (opening between eyelids)
usually at the limbus
due to hyaline degeneration due to ageing and sun/wind/dust exposure
treatment is not needed
pterygium
triangular fold of conjunctiva that grows from the medial portion of the palpebral fissure towards the cornea
only produces symptoms when it reaches the cornea, only then is surgery needed
tends to recur
what is the most common conjunctival change
pinguecula
in what order does light hit layers of the retina
goes to the very bottom first
1st order neuron = cones and rods
synapse
2nd order neuron = bipolar cells
synapse
3rd order = ganglion cells
synapse
4th = optic nerve
beneath the cones and rods is…
pigment epithelium (stops light from scattering) then choroid and then sclera
visual pathway
!! face foreward ok, the light that comes in from the right side of EACH eye will hit the LEFT side of EACH eye (think of diagonal lines entering through the pupil) and is therefore detected by cells on the opposite side of the light source
now
light that hits the temporal side of the eye (ie light that originally came in medially) will NOT cross at the optic chasm, light that hits the medial side will
cones and rods → bipolar cells → ganglion cells →
optic nerve
optic chiasm (medial cross, lateral not)
optic tract → due to ^…
left optic tract = left temporal fibres + right nasal fibres
right optic tract = right temporal fibres + left nasal fibres
lateral genicular body = where the optic tract ends → synapses w/ 5th neurons, then
optic radiation = new pathway = geniculocalanine tracts
fibres of the inferior retinal quadrants pass through the temporal lobe
superior quadrants through the parietal lobe
primary visual area = brodmann area 17
the macula is represented in the most … portion of the occipital lobe
posterior
how many extraocular muscles are there
4 straight
2 oblique
minimum threshold resolution
how far apart 2 objects must be for the eye to perceive them as distinct objects
what is the requirement for the eye to perceive 2 distinct objects as 2 distinct objects
at least one unstimulated cone must lie within 2 stimulated cones of the retina
where are cones concentrated the most
in the centre of the retina
this is where visual acuity is the highest
rods are more x than cones
photosensitive
emmetropia
normal eye sight
ametropia
refractive error due to incorrect ratio of axial length of eye to the refractive power of the cornea and lens
the lens refracts x and the cornea refracts x
cornea refracts more (2/3) than the lens
hyperopia / far sightedness
light rays that enter the eye meet posterior to the retina
short eyeball or deficient lens refractive power
may occur in cortical cataracts
most newborns exhibit slight hyperopia
axial hyperopia is typically congenital
shallow anterior chamber with a thick sclera and well developed ciliary muscles (to compensate)
risk of angle closure glaucoma due to shallow anterior chamber
estropia (cross eyes) may also occur because even when looking at far objects they still need to accommodate
asthenopic symptoms esp. when reading (headaches etc)
converging lenses needed (biconvex)
which, hyper or myopia, is likely to become presbyopic earlier
hyperopia since they need to accommodate for both far and close objects but accommodation decreases with age
why does estropia occur in hyperopia
because even when looking at far objects they still need to accommodate
latent hyperopia
inability to relax ciliary muscles even after having lenses due to the overuse of the muscles
myopia / near sightedness
light rays that enter the eye meet anterior to the retina
long eyeball (its just long or the anterior chamber is deep) or high lens refractive power
may occur in nuclear cataracts which may also cause diplopia
most common functional eye disorder other than age related
ciliary muscles are atrophied since theyre barely used (they can already see things up close, and to see up close the ciliary muscles contract so they dont need it → atrophy)
risk of retinal detachment and glaucoma
require ‘hourglass’ lenses
ciliary muscles in hyperopia and myopia
atrophied in myopia due to lack of use
sclera in hyperopia and myopia
well developed in hyperopia
there is a risk of x in myopia
retinal detachment and open angle glaucoma
there is a risk of x in hyperopia
angle closure glaucoma due to shallow anterior chamber
is refractive power of the lens constant
no, it changes to see close vs faraway things
done by accommodation which is due to elasticity of the lens + zonule fibres + ciliary muscles
how does the lens change shape with close vs faraway objects
thinner when things are further away = due to relaxed ciliry muscles (which actually means that the zonule fibres are under tension and taught)
relaxed ciliary muscles
zonule fibres are under tension and taught
lens is thin
faraway objects or at rest
in ametropia, is the problem usually axial or refractive
axial
amisometropia
= a difference in refractive power between the 2 eyes, usually < 4 diopters
if the difference in refractive power between the 2 eyes is > 4 diopters…
the size difference of the 2 retinal images becomes too great for the brain to fuse the 2 images together = aniseikonia
aniseikonia may lead to…
amblyopia
(also called lazy eye) is a type of poor vision that usually happens in just 1 eye but less commonly in both eyes. It develops when there's a breakdown in how the brain and the eye work together, and the brain can't recognize the sight from 1 eye
keratoconus
Conical, usually bilateral central deformation of the cornea with parenchymal opacification and thinning of the cornea
cornea thins out → cone in the centre
progressive, starts around puberty
causes myopia and astigmastism
Left untreated, in rare cases keratoconus can cause tears of Descemet’s membrane due to the continuous stretching. The entire cornea can then bulge out at this site = acute keratoconus → sudden loss of visual acuity accompanied by intense pain, photophobia, and increased tearing
Degeneration of visual acuity can usually be corrected initially with eyeglasses; hard contact lenses will be required as the disorder progresses
keratoglobus
same idea as keratoconus but is present from birth and not progressive (also rarer)
also causes myopia and astigmastism