Pulmonary Alterations and Mechanical Ventilation Overview
1/281
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
282 Terms
Carina
A landmark that the ventilators should end about 2-3 cm above to ensure each lung gets equal volume of inflation.
Pleural Space
The area between the parietal pleura and visceral pleura that contains fluid allowing the lungs to slide during breathing.
Parietal Pleura
Membrane lining the chest wall.
Visceral Pleura
Membrane lining the lung parenchyma.
Pleural Pressure
-5 cm H20 pressure (vacuum pressure) between the pleura that helps keep the lungs from collapsing.
Alveoli
Structures where gas exchange occurs, with walls so thin that only one cell gets through at a time.
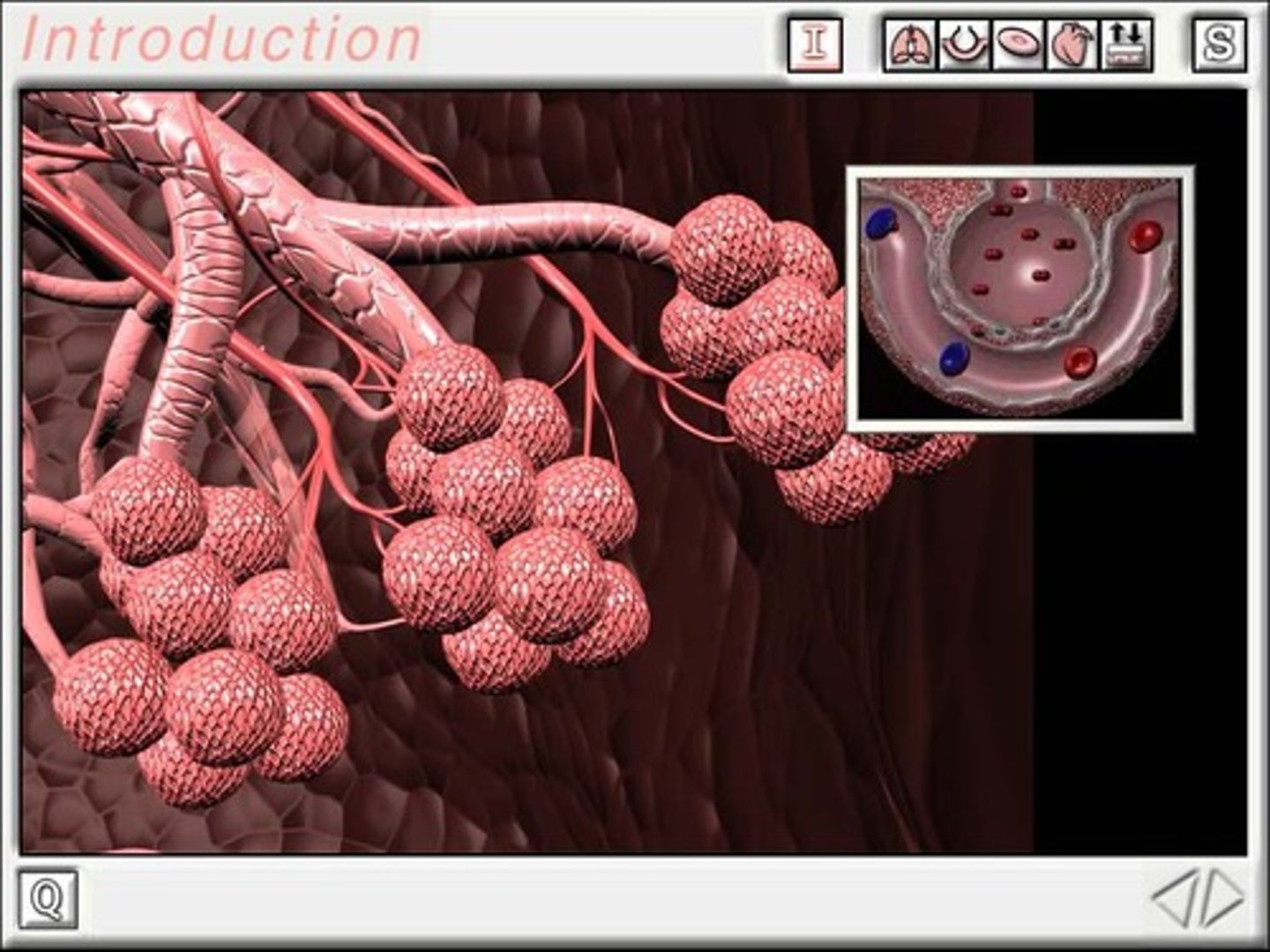
Type I Cells
Cells that make up 90% of the alveolar surface area.
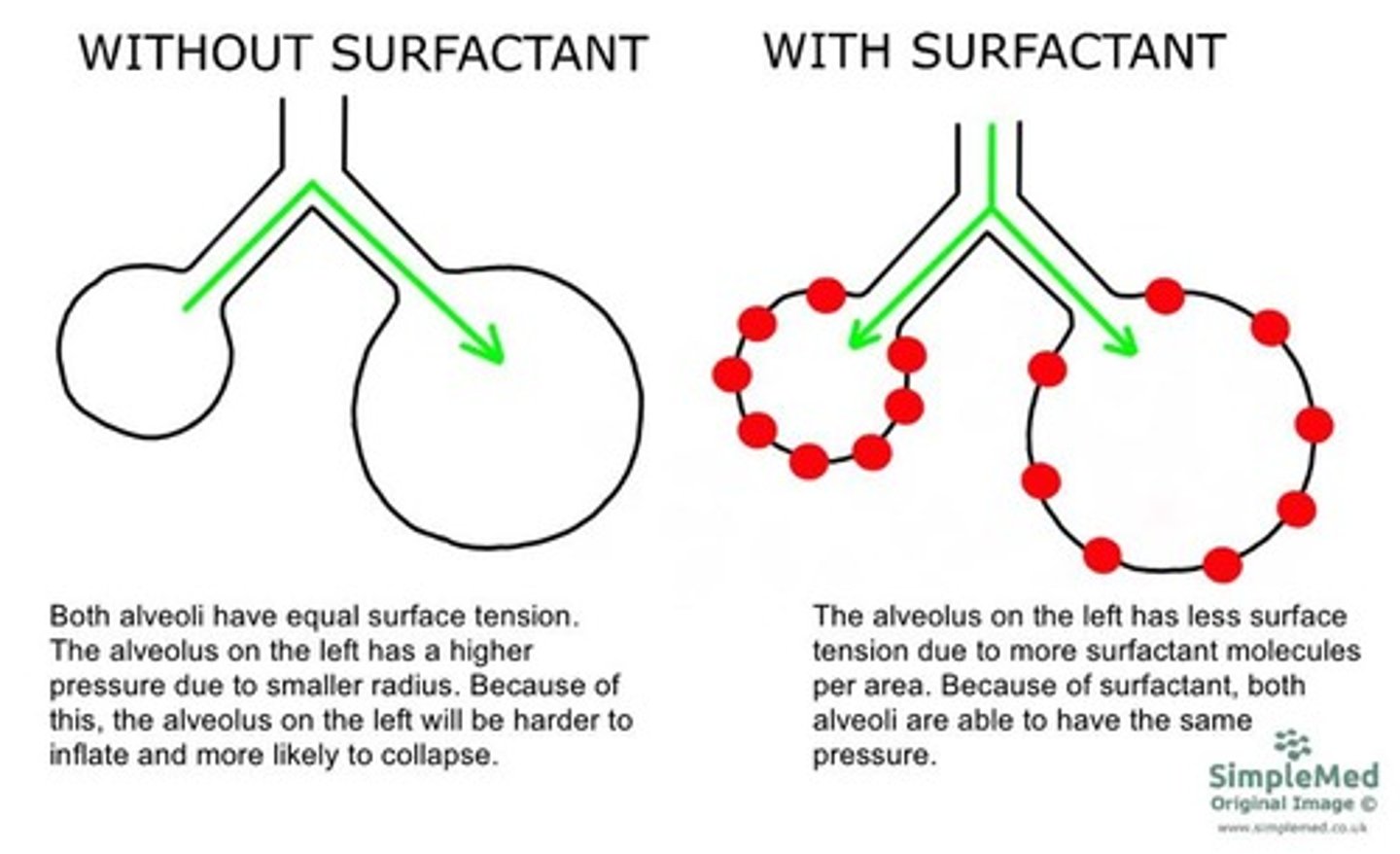
Type II Cells
Cells that produce pulmonary surfactants, decreasing surface tension in alveoli.
Pulmonary Surfactants
Substances produced by Type II cells that decrease surface tension in alveoli, making it easier to inflate them.
Ventilation
Movement of air in and out of the lungs, all the way down to the alveolar level and back out.
Perfusion
Movement/flow of blood to the tissues.
Diffusion
Movement of gases across the pulmonary membrane, occurring from an area of high concentration to low concentration.
Alveolar Diffusion Factors
Factors affecting diffusion include surface area, thickness of alveolar capillary membrane, partial pressure of gases, and solubility of the gas.
Solubility of Gas
CO2 diffuses across the alveolar-capillary membrane 20 times faster than O2.
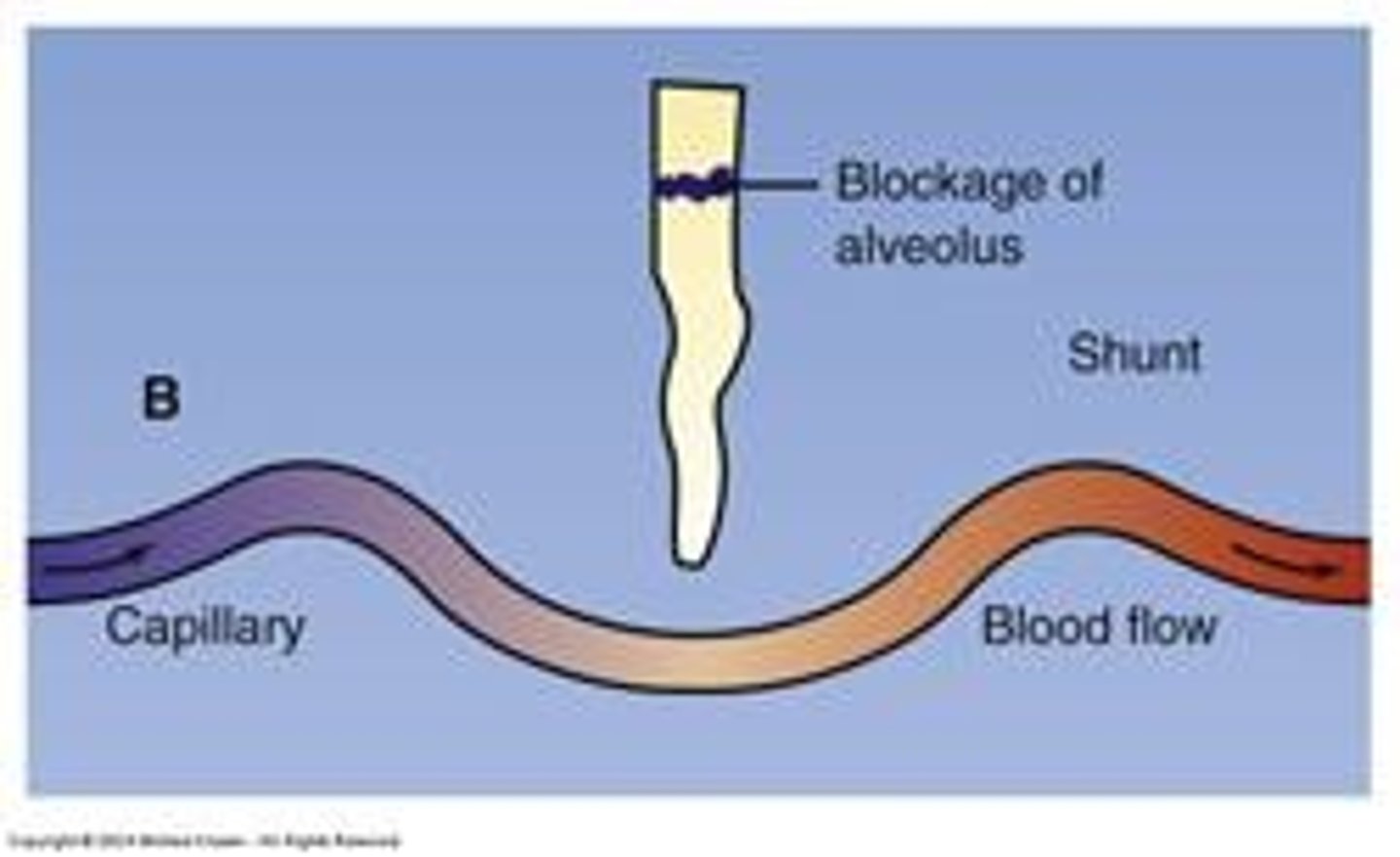
Ventilation/Perfusion (VQ)
The relationship between ventilation and perfusion in the lungs.
Normal Unit
A state where normal ventilation (V) and normal perfusion (Q) are occurring.
Shunt Unit
A state where perfusion is greater than ventilation, causing blood to pass alveolus without gas exchange.
Causes of Shunt Unit
Conditions such as pneumonia, atelectasis, tumor, or mucus plug that lead to perfusion greater than ventilation.
Deadspace Unit
Does not participate in gas exchange
Causes of Deadspace Unit
Pulmonary embolism, Pulmonary infarction
Covid pneumonia acute respiratory distress syndrome
Condition where one lung would be whited out with fluid
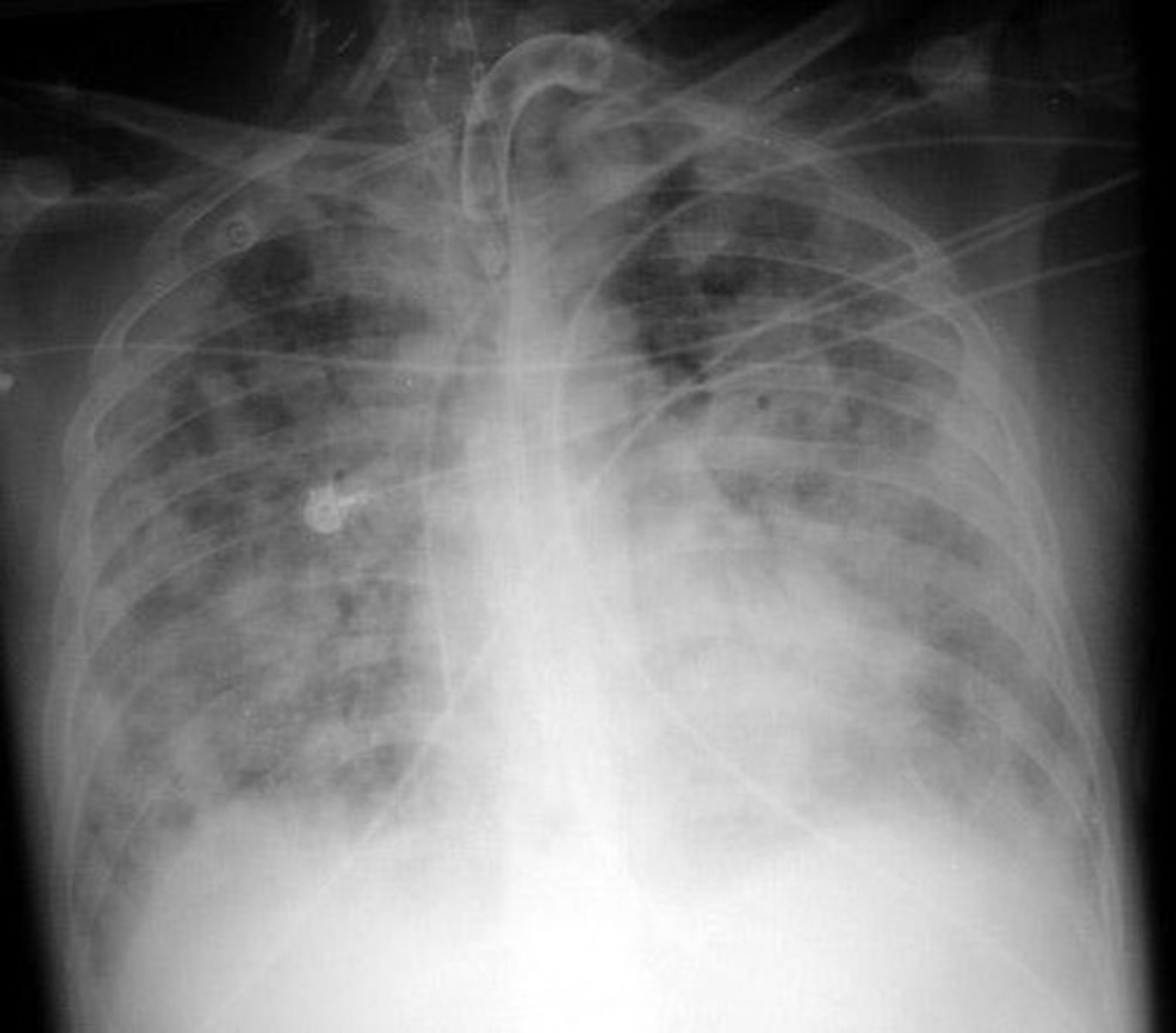
Proning
Practice that displaces fluid and increases perfusion to different areas of the lung
Oxygenation vs Ventilation
Oxygen is carried in the blood in two ways: 97% bound to hemoglobin (SaO2) and 3% dissolved in plasma (PaO2)
SaO2
Saturation of arterial blood, measured by ABGs or pulse oximetry
PaO2
Partial pressure of oxygen, only measured with ABGs
Pulse Oximetry (SpO2)
Indirect measurement of hemoglobin saturation, can give false readings
Signs and Symptoms of Hypoxemia
Tachypnea, Hyperventilation, Dyspnea, use of accessory muscles, cool skin, cyanosis, restlessness, confusion, tachycardia
PaCO2
Tells us the patient's ventilation status; adequacy of ventilation is measured by looking at the patient's PaCO2
Hyperventilation
Condition where the PaCO2 is too low, indicating the patient is moving too much air
Hypoventilation
Condition where the PaCO2 is too high, indicating the patient is not moving enough air
End-Tidal CO2 Monitor (Capnography)
Noninvasive monitor that measures the exhaled CO2 of each breath
Signs & Symptoms of Hypercapnia/Hypercarbia
Headache, drowsiness, confusion, seizures, flushed skin
Acid Base Balance
Maintain pH balance compatible with metabolic life, measured through arterial blood gases (ABG)
ABG Normal Values
pH: 7.35-7.45, PaO2: 80-100 mm Hg, SaO2: 93-99%, PaCO2: 35-45 mm Hg, HCO3: 22-26 mEq/L
pH
Normal range is 7.35 - 7.45; < 7.35 = ACIDOSIS; > 7.45 = ALKALOSIS
HCO3-
Bicarbonate, normal is 22-26 mEq/L, regulated by the kidneys
ABG Interpretation Steps
1. Evaluate the pH. 2. Evaluate the pCO2. 3. Evaluate the HCO3-. 4. Determine the primary disorder.
Correction
The process by which the same system that is affected changes to bring pH back to normal resp fixes resp issue.
Compensation
Process by which the other system changes to attempt to bring the pH back to normal- kidneys fix a resp issue.
Primary Disorder Determination
Label pH as A or B; Label CO2 as A or B; Label HCO3 as A or B; If CO2 matches the pH, label as respiratory; If the HCO3 matches the pH, label as metabolic.
Compensation Determination
If the component that does not match your pH is labeled opposite of the primary component, compensation is occurring.
Respiratory Alkalosis
Respiratory alkalosis is partially compensated because the kidneys are trying to return the pH to normal.
Partial Compensation
pH= 7.32 A; CO2 = 50 A; HCO3 = 30 B- high CO2 trying to compensate for the respiratory acidosis.
Full Compensation
pH = 7.36 Normal- slightly acidic; CO2 = 50 A; HCO3 = 33 B; Fully compensated, respiratory acidosis the kidneys are compensating for the high acid.
PaO2 Normal Range
Normal = 80-100; < 80 = hypoxemia; PaO2 < 60 = critical zone- will have major issues.
SaO2 Normal Range
Normal = 93-99%; < 90% = Critical zone.
Alkalemia
↑ pH; Too much HCO3 or Too little CO2.
Acidemia
↓ pH; Too much CO2 or Too little HCO3.
Uncompensated Respiratory Acidosis
pH 7.29 A; CO2 65 A; HCO3 24 N; PaO2 88; SaO2 86.
Partially Compensated Respiratory Acidosis
pH 7.32 A; CO2 60 A; HCO3 30 B; PaO2 78; SaO2 86.
Partially Compensated Metabolic Alkalosis
pH 7.49 B; CO2 48 A; HCO3 38 B; PaO2 88; SaO2 86.
Fully Compensated Metabolic Alkalosis
pH 7.43 N- B; CO2 54 A; HCO3 30 B; PaO2 82; SaO2 86.
Mixed Disorders
pH : 7.25 A; CO2 : 56 A; HCO3 : 15 A; PaO2 : 66 Hypoxemic; SaO2 : 91 low.
Acute Respiratory Failure
A problem of Inadequate gas exchange; Usually occurs secondary to another disorder (like resp failure caused by pneumonia, a tumor, PE, atelectasis).
Oxygen Delivery Methods
GOAL - deliver the least amount necessary.
Nasal Cannula
1-6 L/min - Low flow device delivers 21 - 44% FiO2.
High-Flow Nasal Cannula
1-60 L/min - High flow device delivers 21-100% FiO2.
Face Mask
(40-60% or 5-10 L/min).
Venturi Mask
(25-60% or 4-15 L/min) (AKA Venti mask).
Nonrebreather
(85-95% or 10-15 L/min).
Non-Invasive Ventilation (NIV)
Uses a mask that fits tightly over the mouth and nose, or just the nose (nasal pillows).
BiPAP
Positive pressure on both inspiration AND expiration; inspiratory and expiratory pressures are different.
IPAP
Inspiratory positive airway pressure - a bump on inspiration to get more tidal volume to breathe in and exhale deeply to breathe off CO2.
EPAP
Expiratory positive airway pressure - helps maintain alveoli pressure, keeps them open, and helps recruit more to assist with ventilation and oxygenation.
CPAP
Continuous Positive Airway Pressure; inspiratory pressure and expiratory pressure is the same.
V60
A bipap that uses FiO2 up to 100%.
Airway protection
Ensuring patients are alert enough to prevent silent aspiration and manage vomiting to avoid aspiration pneumonia.
Nutrition & Hydration
Breathing takes precedence over eating; patients are usually NPO or have an NG tube.
Oral care
To decrease bacteria and keep it out of the lungs.
Skin care
To prevent pressure ulcers from mask suction; Mepelex can be used on the nose.
Communication
Will be muffled; consider writing or other methods to communicate.
Endotracheal Tubes (ETT)
A tube placed in the trachea between vocal cords, preventing speech.
Intubation
The process of placing a tube in the trachea for ventilation.
ETCO2 monitor
A device that indicates correct placement of the tube by color change (purple to yellow).
Coughing
Indicates the need for suctioning or inappropriate tube placement.
Nursing Interventions for Intubation
Ensure equipment is ready, monitor vital signs, and administer medications as directed.
Mechanical Ventilation Goals
Improve ventilation, decrease work of breathing, correct inadequate breathing patterns, and improve oxygenation.
Ventilator settings
Settings that affect the amount of air moved in and out of the lungs.
Tidal Volume (VT)
The size of each breath; larger in = large out.
Rate (f)
The number of breaths per minute; easiest to change based on a patient's body weight.
Assist Control (AC)
A mode that assists or controls breaths; delivers a preset tidal volume at a preset rate.
Synchronized Intermittent Mandatory Ventilation (SIMV)
A mode that allows for both mandatory and spontaneous breaths.
Pressure Support Ventilation (PSV)
A mode that provides support during spontaneous breaths.
Assist Control
Negative deflection, triggering assisted breath.
Synchronized Intermittent Mandatory Ventilation (SIMV/IMV)
Ventilator delivers a preset volume at a preset rate that is a minimum. In between mandatory breaths, the patient can breathe spontaneously, with a pressure-supported breath.
Advantages of SIMV
Helps keep respiratory muscles active and coordinated and can be used as a weaning mode.
Pressure Support (PSV)
When on IMV or Spontaneous breathing trial, this 'boost' from the ventilator increases spontaneous breath volume and makes it easier for the patient to inspire.
Settings that Affect Oxygenation
Settings that affect oxygenation are those that increase the uptake of oxygen at the alveolar/capillary level.
FiO2 (Fraction of Inspired Oxygen)
The percentage of oxygen delivered via the ventilator, ranging from 30-100%.
Positive End Expiratory Pressure (PEEP)
Positive pressure applied at the end of expiration of ventilator breaths, increases oxygenation by preventing collapse of alveoli.
Complications of PEEP
Hemodynamic compromise due to decreased venous return, and volutrauma or barotrauma along the thin capillary membrane.
PEEP
The amount of pressure remaining in the lung at the END of the expiratory phase.
What is the percent of oxygen in room air?
Around 21%.
If a patient is at 100% FiO2, what can PEEP do?
PEEP can help recruit more alveoli and open collapsed alveoli for improved oxygenation.
Increase FiO2
Increase oxygen to correct elevated PaCO2.
Increase PEEP
Recruit more alveoli to correct elevated PaCO2.
Decrease TV
Lower volume of breath to correct elevated PaCO2.
Increase rate
Faster breathing to blow off more CO2.
Patient stops breathing
They will still receive the preset volume at the preset rate.
Weaning modality
Pressure support is used to see what the patient can do without maximum ventilator support before Extubation.