Neurological Disorders
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
TBI
craniocerebral trauma
common causes: motor vehicle, accidents, falls, sports
TBI types
penetrating
non-penetrating
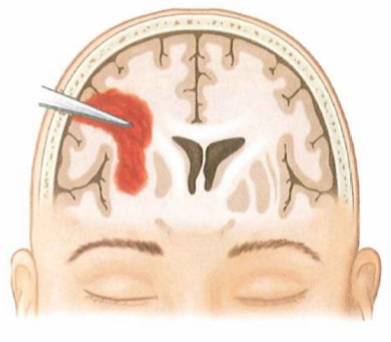
Penetrating TBI
Open head injury
foreign object breaks through skull, punctures meninges and enters the brain, pushes bone fragments into brain below fracture
Impairments often focal (localised) rather than diffuse
Non-penetrating
Closed head injury
damaged brain without open wound/penetration of foreign substance into brain
skull may be fractured but meninges intact
produces more complex symptoms than penetrating - widespread damage
Types of nonpenetrating TBI
Type 1: Nonaccelerating lesion
Type 2: Acceleration - Deceleration
Nonaccelerating lesion
restrained head hit by moving object
generally less severe consequences
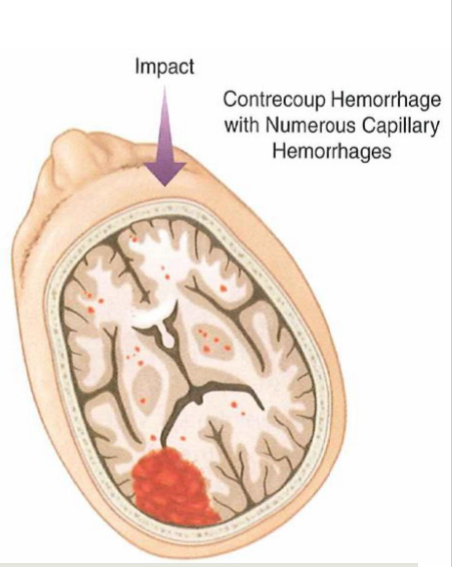
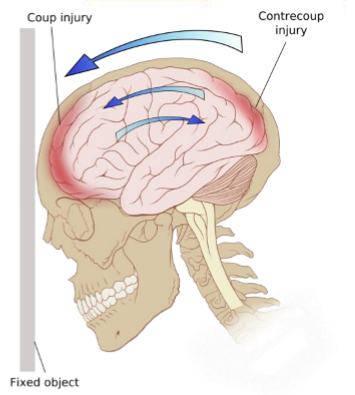
Nonpenetrating TBI
AKA Coup-Contrecoup
head set into motion by physical forces
affecting entire tissue - front and back of brain - strains - stressing/straining on white matter fibres
TBI secondary effects
intracranial hematoma (collection of blood between brain and skull)
increased intracranial pressure
seizures
infections - penetrating TBI is higher-risk
TBI neurobehavioural effects
Altered consciousness
impaired reasoning, planning and thinking skills
memory problems
confusion & disorientation
dysphagia
communication disorders
dysarthria, confused language, anomia, problems maintaining topic, impaired social interaction, lack of narrative cohesion
Altered consciousness
coma - unconscious and unresponsive to most or all external stimuli
Stupor - generally unresponsive, but pain or other strong stimulus may arouse patient for brief period
assess using glasgow coma scale
Lacunar infarcts
type of ischemic stroke
obstructions of blood flow in smaller deep arteries within the brain
occur most often in basal ganglia, internal capsule, thalamus and brainstem
signs develop slowly
Lacunae
small cavities that remain after necrotic tissue is cleared away
Transient Ischemic Attack (TIA)
= ministrokes
temporary disruptions of cerebral circulation accompanied by symptoms
symptoms resolve completely within a few mins to 24 hours
increased risk of stroke with permanent neurological deficit within 5 years
warning sign of potential strokes to come
CVA ischemia treatment
thromboembolic processes
anticoagulant drugs - reduce stroke by prevention of embolism
platelet inhibiting drugs - can reduce risk of recurrent TIAs
thromboembolytic activating agents (t-PA) = clot-busting drugs
restores blood flow by dissolving clot
carotid endartectomy
surgery removing plaque inside carotid artery
angioplasty/stenting
mechanically widening narrowed/obstructed artery
clot retrieval
CVA recovery
some degree of spontaneous behavioural recovery occurs during period after stroke - whether or not they have rehab
result of
diaschisis - temporary suspension of fxns of uninjured areas with rich connections with injured brain areas
reduced blood flow
edema - swelling due to extra fluid

Brain tumours
any cell type in nervous can become neoplastic (neoplasia = uncontrolled, abnormal growth of cells)
nervous system tumours rarely metastize outside CNS
systemic cancer can matastize to CNS
Types of brain tumours
neurocytomas = neuronal neoplasms (rare)
astrocytomas- most common primary CNS tumor = neoplasm from astrocytes - glioma (from glia cells - non-neuronal)
meningiomas - from meninges
schwannomas - from Schwann cells
Speech and language problems following neurological disorders
apraxia
dysarthria
aphasia
Apraxia/dyspraxia
dysfunction of motor planning in absence of muscular weakness or muscular dyfunction
muscles themselves are fine
Types of apraxia
ideomotor
oral
apraxia of speech
Ideomotor apraxia
impaired ability to carry out skillful purposeful movement in response to a verbal command
often accompanies aphasia & may be mistakenly identified as comprehension difficulty
Oral apraxia
inability to voluntarily perform nonspeech movements with laryngeal, tongue and facial muscles, in the absence of muscle weakness
Apraxia of speech
impaired ability to execute voluntarily appropriate movements for articulation in absence of muscular weakness or dysfunction
inconsistent initiation & sequencing of articulatory speech movements
often associated with Broca’s aphasia
Dysarthria
group of speech production disorders caused by oral-motor weakness, paralysis or incoordination
congenital or acquired
Not necessarily a language disorder
A disorder of motor function
Types of dysarthria
spastic
flaccid
hypokinetic
hyperkinetic
ataxic
Spastic dysarthria
associated with UMN lesions
usually bilateral lesions
speech characteristics:
imprecise consonant production
low pitch
slow speaking rate
harsh voice with strained-strangled quality
Flaccid dysarthria
LMN or motor unit lesions
Speech characteristics depend on part of motor unit & specific CN affected:
imprecise articulation
hypernasality
tongue fasciculations
voice difficulties
Hypokinetic dysarthria
Basal ganglia lesions - associated with PD
speech characteristics:
monoloudness
monopitch
decreased loudness
breathy voice
short rushes of speech
Hyperkinetic dysarthria
Basal ganglia lesions - associated with HD
speech characteristics:
excessive variation in loudness
variable rate
irregular articulatory breakdowns
involuntary movements of oral musculature
Ataxic dysarthria
cerebellar lesions
caused by damage to cerebellum & its pathways - loss of coordination
e.g., degenerative diseases, stroke, trauma, tumours, alcohol intoxity
speech characteristics may include:
excess & equal stress (scanning speech)
irregular articulatory breakdown
slow rate & prosodic changes
harsh voice quality
excessive loudness variation
Aphasia
acquired communication disorder caused by brain damage - stroke most common cause
characterised by impairment of language modalities: speaking, listening, reading and writing
not result of sensory, motor, general intellectual deficits, confusion or psychiatric disorder
Types: Broca’s, Wernicke’s, global
Broca’s aphasia
= expressive aphasia
lesion may be in Broca’s area
verbal expression
Nonfluent & effortful speech
Anomia – word finding & recalll
Poor/absent grammar
Aware of their speaking difficulties
auditory comprehension
usually impaired but comprehend spoken language better than they speak
may have difficulties understanding more grammatically complex sentences
Wernicke’s aphasia
= receptive/jargon aphasia
lesion often in Wernicke’s area
frequently no muscle weakness - typical site of lesion away from precentral gyrus
Auditory & reading comprehension
severe impairment
Verbal expression
fluent speech with abnormal content
often neologisms (made up words)
if severe – may be jargon
Not aware of their difficulties
Other disorders affecting communication
Memory problems
Sensory memory
1 st step in information processing
extremely brief (ms – 2 sec)
Responsible for holding sensory information for a very short duration after the stimulus has ended
Acts as a buffer system that allows the brain to register and process incoming sensory input before:
Decays
Transferred to short-term memory for processing
e.g., visual & auditory information storage
Working memory
= active memory
Storage and manipulation
limited capacity (~4-7 items)
Active & conscious
info must be continually acted upon
if not rehearsed memory will decay quickly
prefrontal & frontal-parietal cortex involved
Short-term memory vs working memory
Short-term:
static storage with minimal processing—remembering a new telephone number
Broader working memory:
dynamic and more relevant for understanding higher cognitive functions—doing mental maths
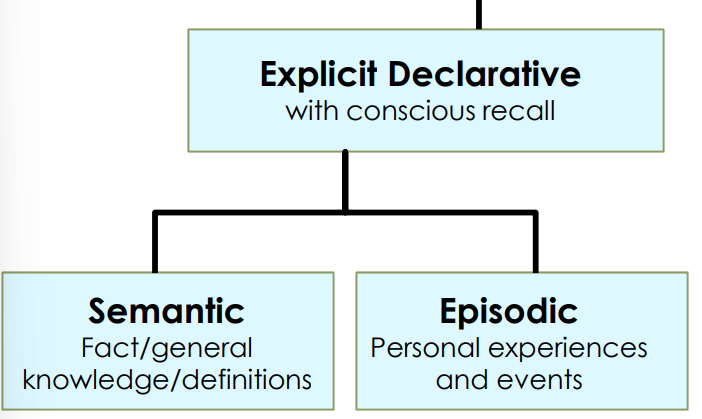
Long-term memory
relatively permanent storage of info
2 main types
declarative (explicit) memory
nondeclarative (implicit) memory
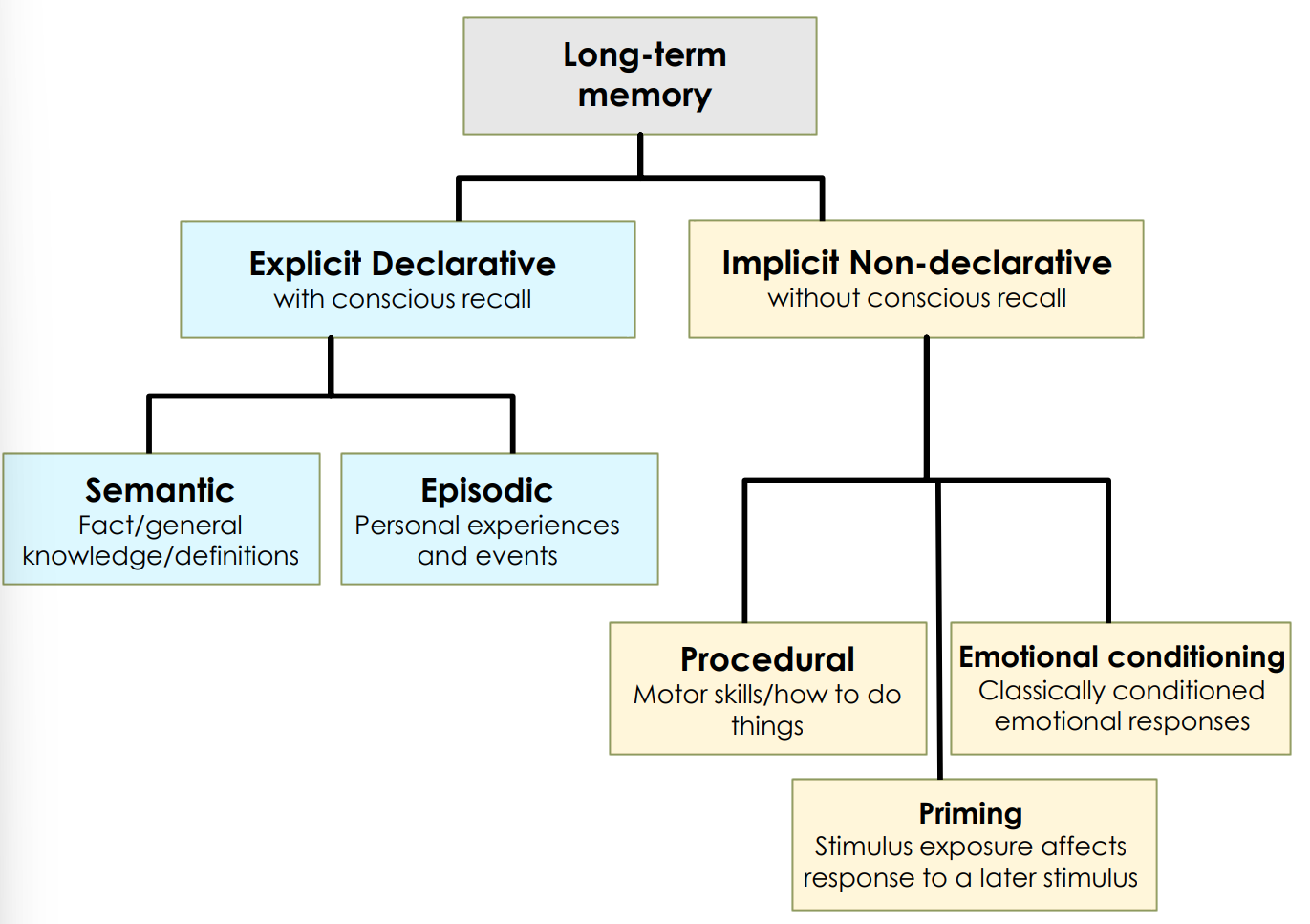
Long-term Explicit Declarative Memory
Factual info that can be declared
semantic memory
conceptual knowledge--facts, ideas, and concepts
e.g. ‘Madrid is the capital of Spain’
episodic memory
info about temporally dated episodes & events
e.g. Your first day of Uni, what you had for breakfast, specific and general events
Structures involved in Long-term Explicit Declarative Memory
medial temporal lobes, incl. hippocampus & surrounding structures
amygdala, role in emotions accompanying processing of certain memories
Long-term Implicit Nondeclarative memory
Procedural memory (implicit and unconscious)
broad term for several kinds of memory
e.g., motor skills, reflexes, emotional, unconscious
strengthened by repetition & practice (habit/rote)
tying shoelaces, riding a bike, multiplication tables
Structures involved in Long-term Implicit Nondeclarative memory
motor skills: caudate nucleus, putamen, motor cortex, cerebellum
emotional implicit memories: amygdala
conditioned reflexes: cerebellum
Memory disorders
amnesia
retrograde amnesia
anterograde amnesia
Amnesia
loss of long-term memory
often refers to declarative memory loss
Retrograde amnesia
loss of memories for events that occurred prior to the trauma or disease causing the memory loss (trouble accessing old memories prior to injury)
Anterograde amnesia
involves loss of memory for events following the trauma or disease (trouble making new memories)
Neuroplasticity
The ability of the nervous system to respond to intrinsic and extrinsic stimuli by reorganising its structure, function and connections
Ability to make new connections, change the way the brain functions and adjust things on the fly
Neuroplasticity can occur
during development
in response to environment
in support of learning
in response to disease
in response to therapy
Use it or lose it neuroplasticity principle
Failure to drive specific brain functions can lead to functional degradation
Use it and improve it neuroplasticity principle
Training that drives a specific brain fxn can lead to an enhancement of that fxn
Specificity neuroplasticity principle
The nature of the training experience dictates the nature of the plasticity
Repetition matter neuroplasticity principle
Repetition of a newly learned behaviour may be required to induce lasting neural changes
Intensity matters neuroplasticity principle
Induction of plasticity requires sufficient training intensity
If really want to see change need to have intensive block of training - short treatment blocks
Time matters neuroplasticity principles
Different forms of plasticity occur at different times during training
can be certain windows of times where the brain is more receptive to learning/plasticity
Saliency matters neuroplasticity principles
The training experience must be sufficiently salient/meaningful to induce plasticity
Age matters neuroplasticity principle
Training-induced plasticity occurs more readily in younger brains
younger brain - is more plastic and better able to respond to damage (advantage)
Older brains not as plastic (disadvantage) - plastic potential slightly more challenging
Transference neuroplasticity principles
Plasticity in response to one training experience can enhance the acquisition of similar behaviours
Interference neuroplasticity principle
Plasticity in response to one experience can interfere with acquisition of other behaviours
plasticity can have negative outcomes