(final) Chronic illness
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
44% of adults (20+) have at least 1 of 10 common chronic conditions
Hypertension: 25%
Osteoarthritis: 14%
Mood / Anxiety Disorders: 13%
Osteoporosis: 12%
Diabetes: 11%
Asthma: 11%
COPD: 10%
Ischemic Heart Disease: 8%
Cancer: 8%
Dementia: 7%
How likely are we to develop chronic condition
Most of us are likely to develop at least one chronic condition that may lead to our death.
Chronic conditions account for ⅔ of Canada’s health spending.
Chronic conditions are more common among lower-income Canadians, women, and seniors
The Initial Response to chronic illness
Shock → an acute stress reaction
Anxiety, anger
Lower sense of control
Secondary appraisal
Emotion-focused coping
Some have denial
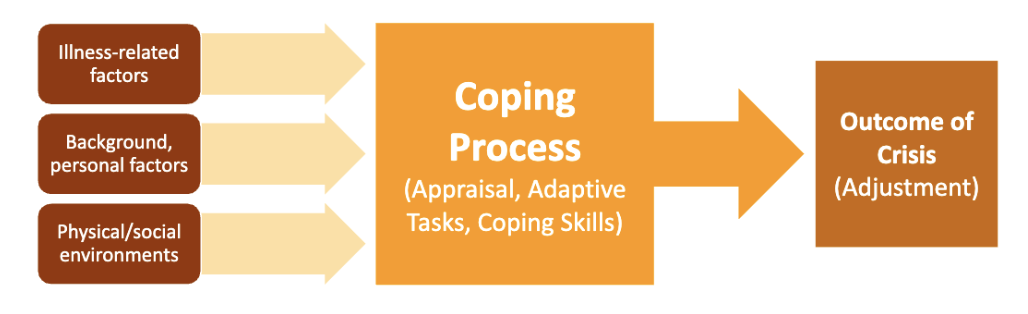
Crisis Theory
Describes factors that influence how people adjust/cope after first learning they have a chronic illness.
Illness-related factors, background/personal factors, physical/social factors
→ coping process: Appraisal (perceived meaning of the illness), adaptive tasks, coping skills
→ adjustment (poor adjustment is linked to self-blame, catastrophizing)
People who are ill must address 2 types of adaptive tasks:
Tasks related to the illness or treatment (3)
Coping with the symptoms/disability of illness.
Adjusting to hospital environment, procedures, treatments.
Developing good relationships with practitioners.
People who are ill must address 2 types of adaptive tasks: Tasks related to general psychosocial functioning (4)
Controlling negative feelings, having positive outlook.
Maintaining satisfactory self‐image, sense of competence.
Preserving good relationships with family/friends.
Preparing for an uncertain future
Coping Strategies for Chronic Health Problems
Denying or minimizing the seriousness (can be beneficial early on).
Seeking info
Learn to self-administered care to gain control.
Setting realistic, limited goals.
Get support
Be prepared for unexpected/stressful events
Gaining a manageable perspective, often by finding a sense of "purpose" or "meaning"
Major life-long adaptive tasks for successful adjustment (3)
Directly continuously manage disease (ex. taking meds regularly, maintain healthy lifestyle)
Minimizing physical limitations & disability (ex. use aid device)
Preserve as much positive functioning as possible (ex. socially engage)
Most useful coping strategies for cancer patients
Social support/direct problem solving (talk to someone abt it)
Distancing (shift focus on illness to smth else): Reduce stress (BUT Passive escape: Decrease psych well-being)
Positive focus (“I learned smth”)
Cognitive and behavioral avoidance (distraction, drinking)
Maladaptive coping for cancer patients
Rumination (exacerbates symptoms)
Interpersonal withdrawal
Avoidant coping (denial) → more distress, exacerbates symptoms (less adherence)
Denial in cancer patients (3 kinds)
Denial of diagnosis (very common)
Denial of impact (outcomes) — MOST common form of denial: Lower lifespan
Denial of emotions
Impacts on psychological functioning, not physical or social functioning depend on the form of denial
Ppl who blame themselves for their chronic illness have…
Higher depression and distress
Lower QoL
Impact of Depression on chronic illness
Helplessness, hopelessness
May be delayed as patients try to understand implications of condition; physically debilitating; direct impact on symptoms.
Shorter survival time for cancer
How can depression complicate medical evaluations?
It could have arisen due to a hospital stay or the treatment process.
Does decreasing depression help with cancer survivability?
Yes, by interventions like good hospice care, even a year earlier
Why do Cancer patients experience challenges in relationships?
Physical difficulty, feel awkward, embarrassed, stigmatized
Other people avoid them due to feelings of vulnerability, worrying they might say the wrong thing, or break down emotionally.
What factors lead to stigma for cancer patients?
Sense of self affected by the diagnosis
Perceived controllability and visibility of cancer
How much it interferes w daily functioning
Cancer stigma is correlated with
Problematic outcomes (depression)
Reduced cancer screening for cervical, breast, and colorectal cancer
Adaptation
Making changes to adjust constructively to life’s circumstances
Focus of coping shifting from crisis stage to dealing w more permanent changes
Successful adjustment → adaptive tasks that continue
Ex. Mastery of demands directly related to ongoing management of disease, minimize physical limitations, disability and preserving as much positive functioning as possible
Cancer survivorship
Long-term cancer survivors have higher rates of emotional distress, esp those of lower SES, single, and disabled
Evaluating Quality of Life (QoL)
Based on physical, psych, vocational, and social functioning; includes disease or treatment related symptoms
A person’s perceptions of their own health
Self-reported health (SRH) or subjective health
Emphasis on daily living
Quality of Life (QoL) is indicator of what?
Recovery/adjustment to chronic illness
Is subjective health consistent with objective health?
YES: SRH is associated with prevalence and onset of all diseases, and laboratory parameters of health
Some studies found no association with cancer
Self-reported/self-rated health (SRH) or Subjective health
Imp aspect of QoL
Use questionnaires/surveys
consistent with objective health
Is predictive of morbidity & mortality (more than objective measures and Satisfaction w Life Scale)
Predictive validity has increased over time
Is subjective health (SRH) predictive of mortality and morbidity?
YES
Even better than the actual physical health
Better than Satisfaction w Life Scale in mortality
Satisfaction with Life Scale (and what it predicts)
1 to 7
Ideal life, like conditions of life, life satisfaction, accomplishment, no regret
Predictive of morbidity (onset of chronic diseases), and mortality (less consistent than SRH)
What psychological interventions are used to manage chronic illness and disease?
Psychopharmacological
Patient & Family Education
Individual or Family Therapy
Stress Management / Relaxation
Support Groups
Why do ppl join Cancer Support Groups?
Common
Believe they can extend their lives
and they are much likely to live 1 year (but not 4 yrs) longer than ppl not in support group
Psychosocial benefits of support groups
Improved mood
Reduced uncertainty
Improved self-esteem
Enhanced coping skills
Improved QoL
Psyc factors that contribute to asthma
Stress, negative emotions, anxiety, catastrophizing → develop and worsening of asthma
High maladjustment and anxiety disorders
Social/Adherence Factors that contribute to asthma
Interpersonal conflict triggers asthma in children
Adherence to medication and avoidance of triggers (ex. smoking)
Good family support → decreased asthma-related inflammation
Psychosocial factors that contribute to epilepsy
Episodes, esp loss of consciousness → cognitive and motor impairments (limit jobs)
High anxiety and stress → increase chance/severity of seizures
Can benefit from relaxation, stress management, biofeedback
Stigma → worse adjustment, low optimism & social support
Rehab psyc goal for spinal cord injury
Gain as much physical function & independance as possible (Ex. bladder control)
Psyc factors that contribute to Spinal Cord Injury
Ppl w SCI experience depression and difficulties related to self-concept
Counselling can help w cope w permanent functional losses
Successful adaptation correlates w resilience, perseverance, tolerance, perceived competence
SCI from military are at higher risk for depression, PTSD
Social factors that contribute to Spinal Cord Injury
Face discrimination at work → limited support
Lower QoL, relationship/financial stability, emotional adjustment, sex satisfaction(helped thru edu and counselling)
Family overprotective → everyone stress out
Can benefit from Reinforcement methods (ex. Use devices to improve limb functioning, change the way they sit)
Psyc factors that contribute to Diabetes
Chronic stress and negative emotions worsen/cause diabetes
Heighten depression and lower self-efficary → less adherence to diet
Problem-focused coping → better emotional adjustment and coherance!
Social factors that contribute to Diabetes
Social support → adherence
Children w Type 1, transition of responsibility to self-care can cause family conflicts
Teen’s adherence → Self-esteem and QoL
Doctor vs patient goals differ (LT vs. day to day well being)
Psyc factors that contribute to Arthritis
Vicious cycle: pain → ↑ stress →↑ symptoms → ^ pain…
Arthritis ^ risk of anxiety & depression (does not cause onset)
Prior depression → v coping with pain
More Severe → interferes w/ daily activities + ^ helplessness & depression
Perceived control → better cope, adherence, adjustment
Helpless + catastrophizing → pain, depress
Social factors that contribute to Arthritis
Spouse’s mental well-being affects coping and adjustment
Client-centered→ better adjustment and less disturbance
More positive support → less pain, disability, depress, fatigue, better mood
Self-management program helps
Psyc outcome of Alzheimer’s
Can’t handle daily tasks and remember things → helplessness, depression
Caregivers of ppl w AD often have
Stress, lower self-efficacy, poorer health, depression
Interventions like cognitive restructuring, respite centres (nurses take care day and night to let caregivers rest) can help them