School
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
119 Terms
Diverticular Disease Diagnosis
acute is determined by examination of the stool for blood, evaluation of blood samples for anemia and signs of active infection, or inflammation, ruptured sacs using ultrasound, magnetic resonance imaging or CT scan
Once acute episode resolved, will need colonoscopy to emulate the diverticula
Diverticular Disease Pathophysiology
Diverticula: small, bulging pouches (weaken areas) that form the lining of your digestive system. (No to little symptoms from diverticula)
Common in lower portion of the body large intestine (sigmoid colon)
Diverticulosis: common and10% of people over 40 and 50% of people over 60.
More than one diverticulum is called diverticula.
Presence of diverticula is diverticulosis
Fecal matter in diverticula may promote development of infection known as diverticulitis
Chronic constipation is linked to development of Diverticular disease
Slow movements of fecal matter leads to increased, prolonged pressure on the walls of large intestine (alters structure and function)
Most people are unaware until they unaware until it leads to bleeding, infection, obstruction, ischemia of the affected area of the colon
Perforation can cause hemorrhage, abscess, sepsis and peritonitis
Prevention involves dietary alterations to prevent constipated like a diet high in fiber or low in fat
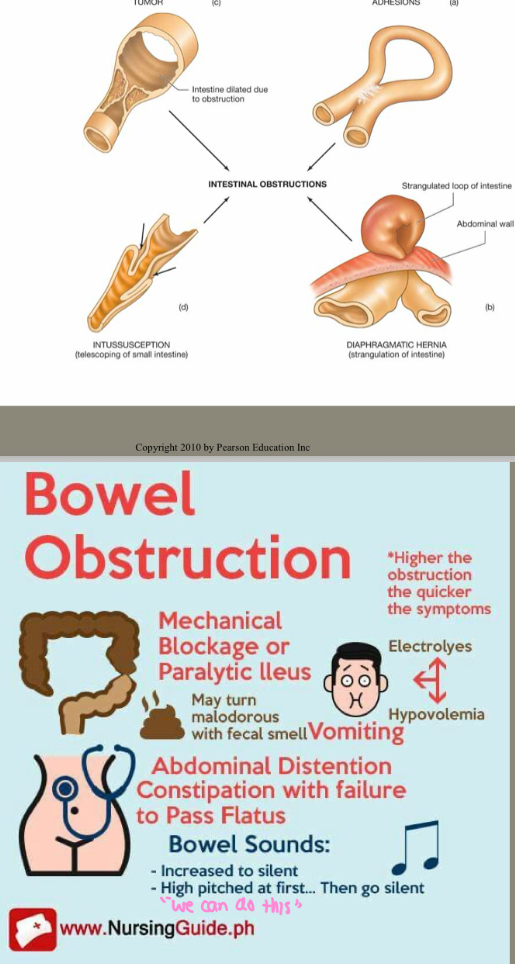
Intestinal Obstruction
Blockage prevents normal flow of intestinal contents through GI tract
Types
mechanical
Functional
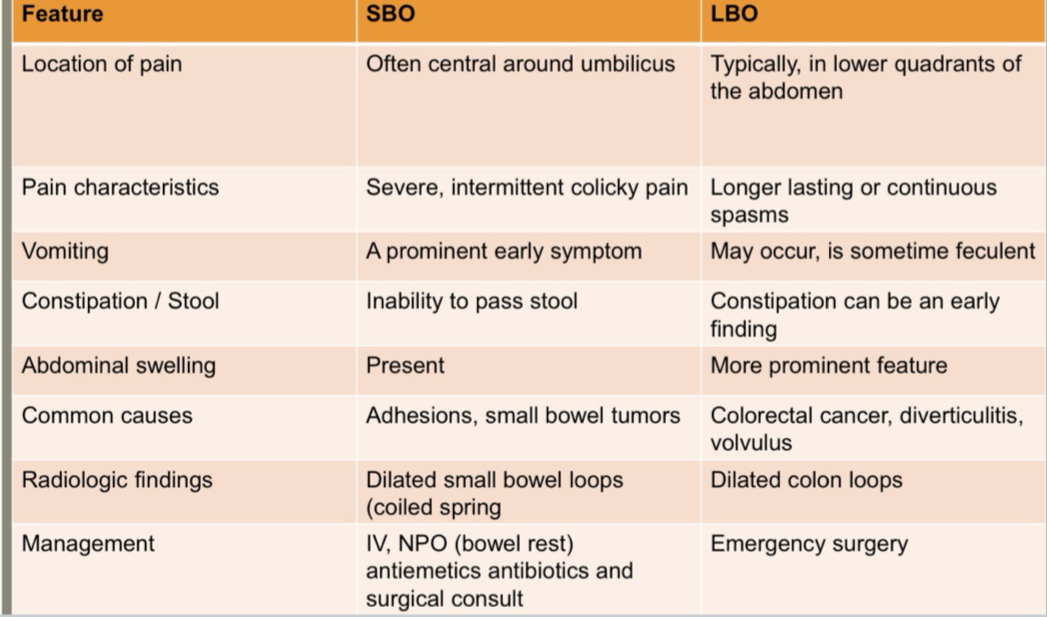
Small Bowel Obstructon (SBO)
Large Bowel Obstruction
Mechanical Obstruction
occurs when something is physically blocking the intestine
Adhesions, hernias, polyps, tumors
Blockage can be partial or complete
Less commmon
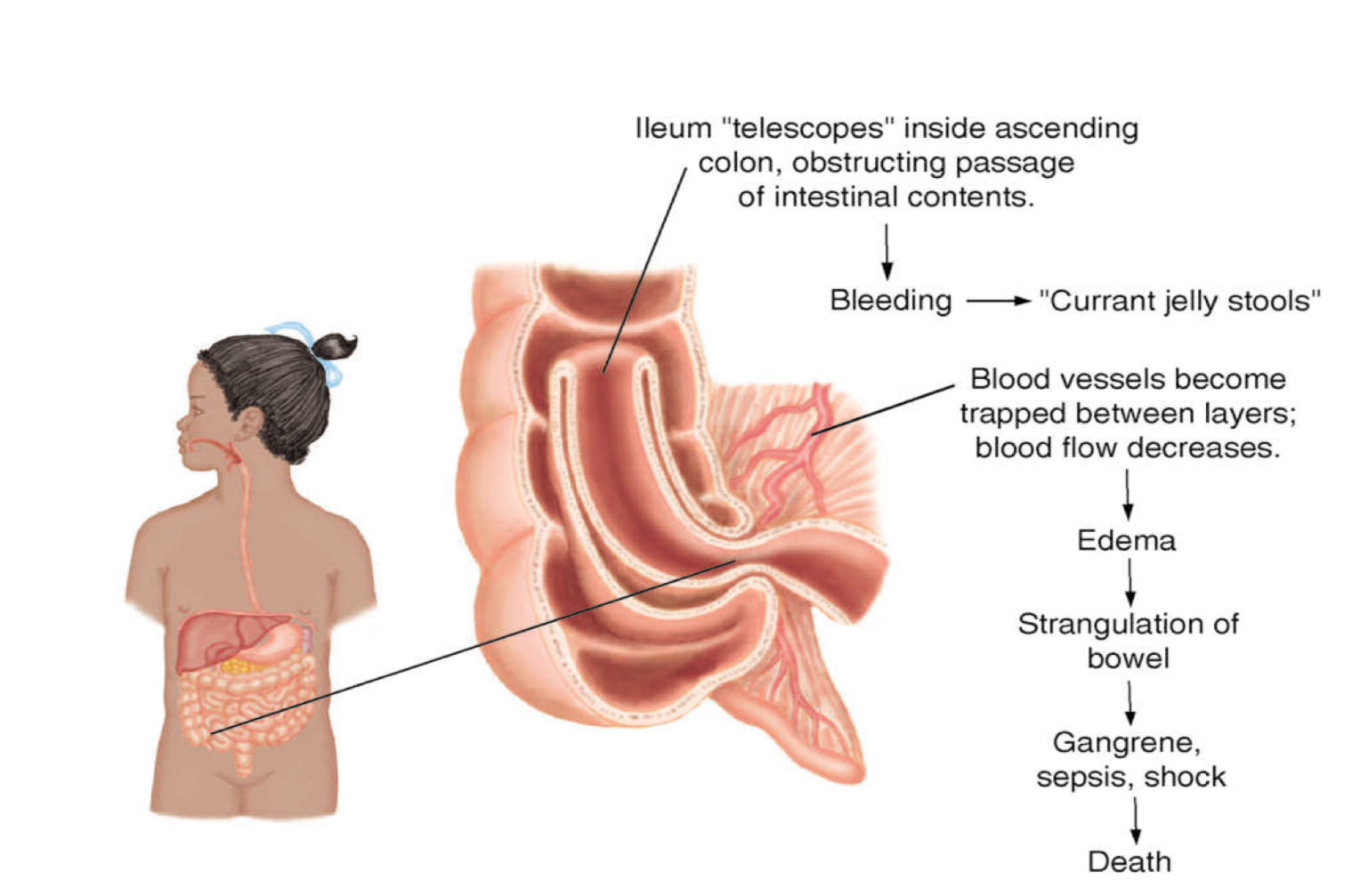
Intussusception
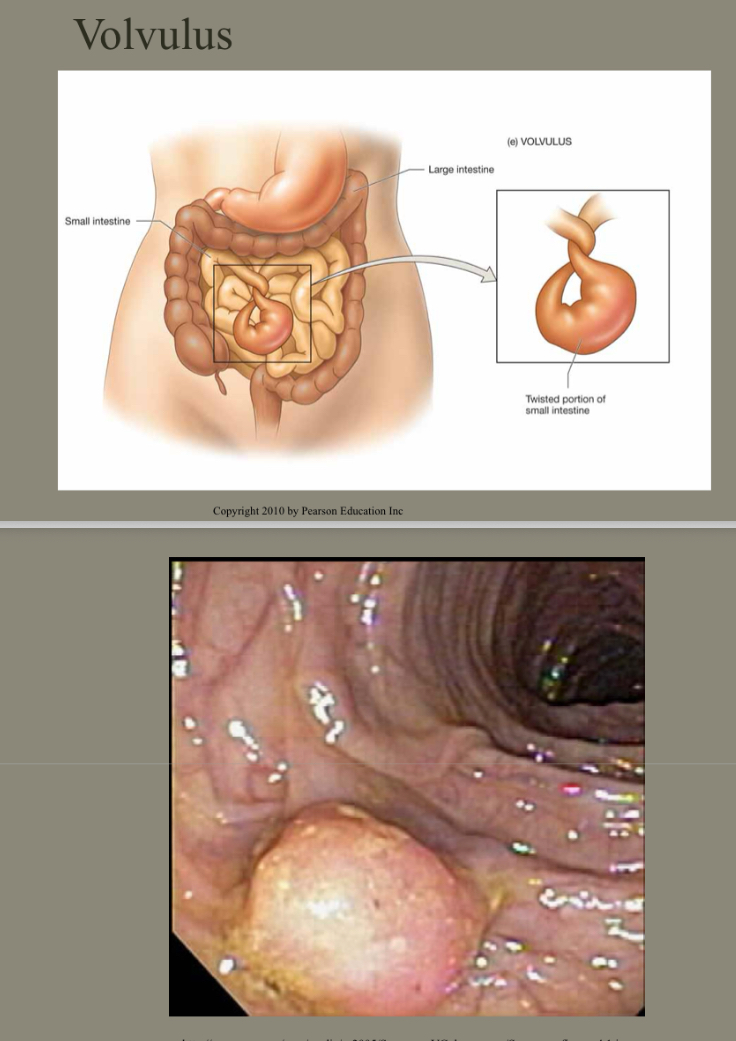
Volvulus
Fecal impaction
Functional Obstruction
Intestinal Musculature cannot propel content along the bowel
Causes
Parkinson’s
Diabetes Mellitus
muscular dystrophy
Paralytic ileus
Continuing with the previous slide
Small Bowel Obstructon (SBO)
Intestinal contents, fluid, gas accumulate above the obstruction
Peritonitis
Swelling of the peritoneum
Small Bowel Obstruction Clinical manifestations
Nausea/vomiting
Stomach contents, bile, fecal matter
wavelike cramp pain
May pass blood and mucous but no fecal matter, no flatus
Dehydration, intense thirst
Abdominal distension and pain
Large Bowel Obstruction
accumulation of intestinal contents, fluid, gas proximal to the obstruction
Serve distension and perforation can occur
Hard, board- like abdomen
Medical emergency
Large Bowel Obstruction Clinical Manifestations
develops and progresses slowly
Constipation may be only symptom
Weakness, anorexia
Vomiting fecal matter
Functional Fecal Incontinence
Repetitive voluntary or involuntary soiling (4+ years and older)
Pathophysiology
Constipation
Clinical Manifestations
Constipation, soiling once a month for at least 2 months
Diagnosis
History/ physical, diet, developmental considerations, behaviors, food allergy
Treatment:
Diet, increase fluids, mental health , scheduled time for defecation
Review: Diverticular Disease
What is the condition ?
Diverticular disease occurs when small pouches, called diverticula, form in the wall of the colon. When these pouches are not inflamed, it is known as diverticulosis, and when they become infected or inflamed, it is called diverticulitis.
What are the S/Sx?
Symptoms of diverticulosis are often mild or absent, but diverticulitis can cause left lower abdominal pain, fever, nausea, vomiting, and bowel changes such as constipation or diarrhea.
Review: Small Bowel Obstructions
What is the condition?
blockage in the small intestine that prevents the normal movement of digestive contents. Common causes include adhesions from prior surgery, hernias, tumors, or inflammatory bowel disease.
What are the S/Sx?
abdominal pain and cramping, bloating, nausea and vomiting, inability to pass gas or stool, and abdominal distention
What is the treatment?
NPO (nothing by mouth), nasogastric tube insertion for decompression, IV fluids for hydration and electrolyte balance, and pain control.
If the obstruction does not resolve or there is evidence of strangulation or perforation, surgical intervention is required to remove the blockage or repair the affected section of bowel.
Review: Large Bowel Obstructions
What is the condition?
blockage in the colon that prevents the normal passage of intestinal contents. Common causes include colon cancer, diverticulitis, volvulus (twisting of the bowel), or strictures.
What are the S/Sx?
abdominal distention, constipation or inability to pass gas, cramping abdominal pain, nausea and vomiting, and sometimes fever or signs of infection if complications occur.
What is the treatment?
fluid and electrolyte replacement, bowel rest (NPO), nasogastric decompression, and addressing the underlying cause.
Surgery may be required if there is complete obstruction, bowel ischemia, perforation, or malignancy.
Review: Functional Fecal Incontinence
What is the condition?
A small bowel obstruction is a blockage in the small intestine that prevents the normal movement of food and fluids. It can be caused by adhesions, hernias, tumors, or paralysis of the bowel.
What are the S/sx?
Common symptoms include crampy abdominal pain, vomiting, bloating, and inability to pass stool or gas.
Review of SBO and LBO
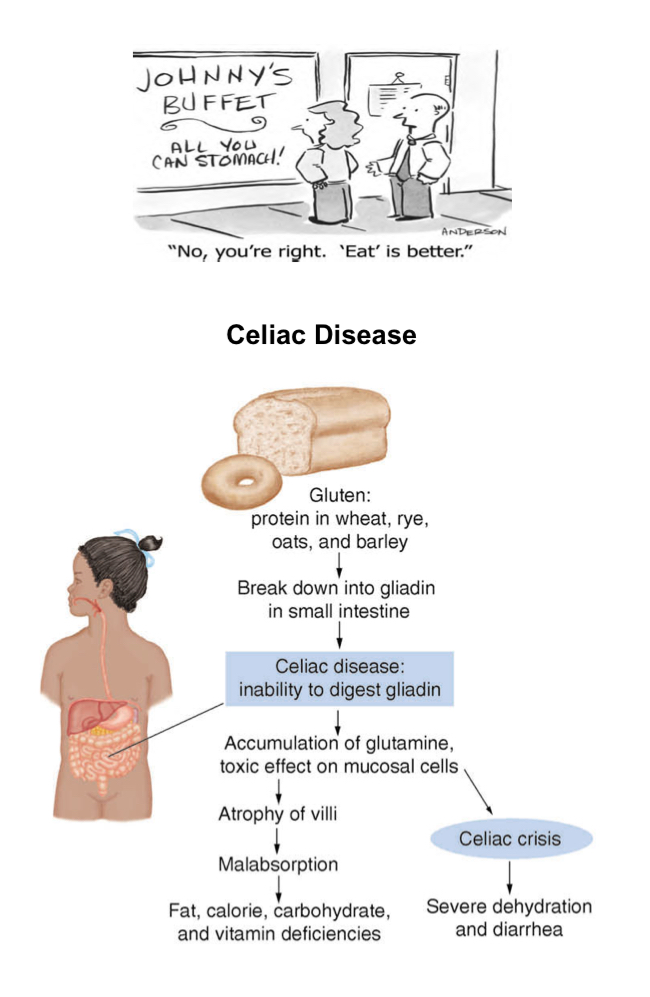
Review: Celiac Disease
Review: Mechanical Obstruction
Mobility and Functional Ability
Discuss the two types of connective tissue found in the skeletal system
The skeletal system contains two types of connective tissue: bone and cartilage. Bone provides structure, support, and protection, while cartilage offers flexibility and reduces friction in joints.
State the function of the parathyroid hormone, calcitonin, vitamin D in terms of bone formation and metabolism
Parathyroid hormone (PTH) increases blood calcium by stimulating bone resorption, calcitonin lowers blood calcium by inhibiting bone breakdown, and vitamin D promotes calcium absorption for bone mineralization.
Describe the source of blood supply to the synovial joint
The synovial joint receives its blood supply from arterial branches surrounding the joint capsule, which form a network to nourish joint tissues and maintain healthy function.
Skeletal System (Connective Tissue)
Bones (Rigid)
Cartilage (Flexible)
Connective Tissue Structure
Ligaments (bone to bone)
Tendons (bone to muscle)
Skeletal System Functions
framework for attachment of muscles, tendons and ligaments
Protects soft tissue and maintains soft tissue in proper position
Provides stability for the body
Maintains body shape
Acts as a storage reservoir for calcium
Contains the hematopoietic (formation of RBCs) connective tissue in which blood cells are formed (RBCs)
Classification of Bones
Long bones
found in the upper and lower extremities
Short bones
irregularly shaped bones located in the ankle and the wrist
Flat Bones
composed of spongy bone between 2 layers of compact bone
Found in areas such as the skull and rib cage
Regulation and Action of Parathyroid Hormone (PTH)
PTH triggers release of calcium from bone
Conserves calcium by the kidney
Increases calcium in the intestine by activating Vitamin D
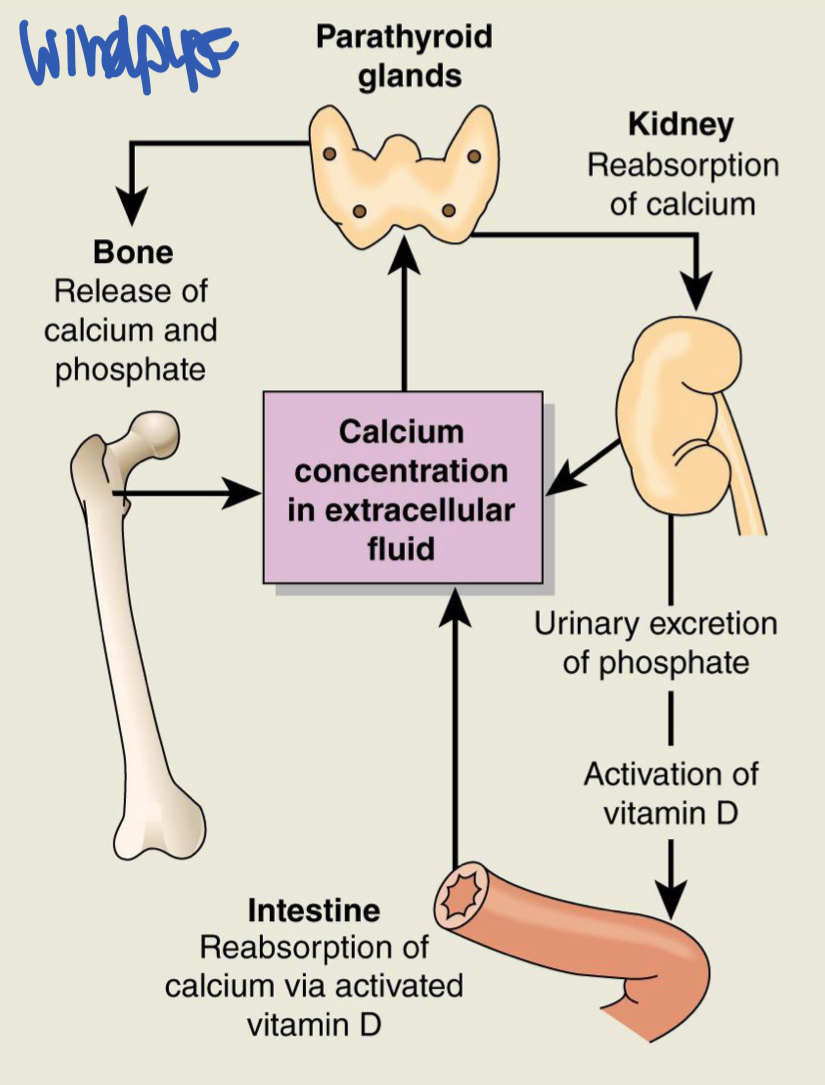
Hormonal Control of Bone Formation and Metabolism
Parathyroid Hormone
Calcitonin
Vitamin D (dairy, lentils)
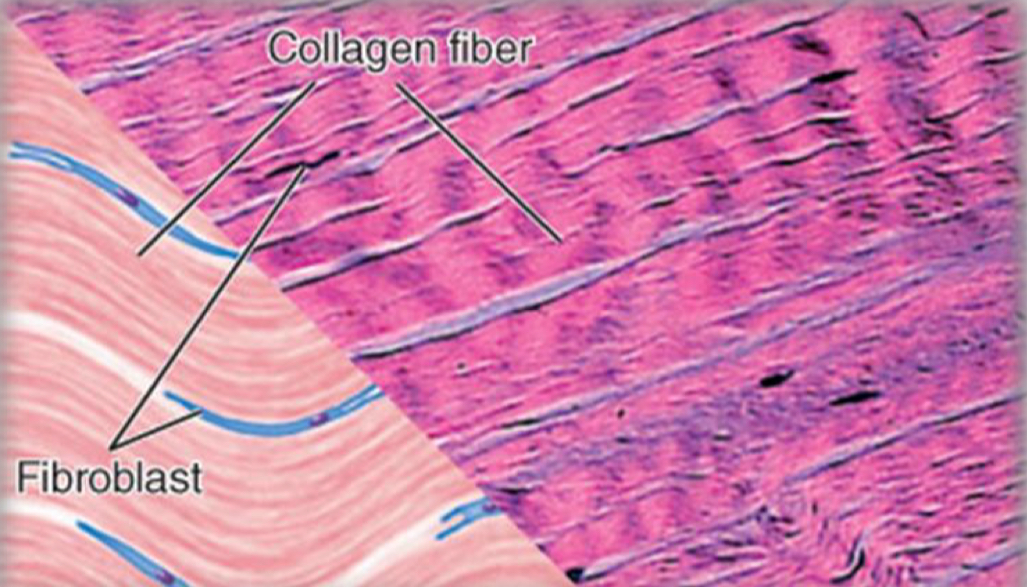
Tendons and Ligaments
Dense connective tissue composed largely of intracellular bundles of collagen fibers arranged in the same direction and plane
Limited blood supply
Composted mainly of collagen (strong ad flexible protein)
Attaches structures together
Forms scar tissues
Joints
areas where two or more bones meet
Classes of Joints
based on movement and presence of a joint cavity
Joint Nourishment Supply
Blood Vessels
direct or indirectly nourishes the majority of joint tissue
Synovial membrane has a rich blood supply
Synovial Fluid
supplies articulating cartilage
Fluid is normally clear or pale yellow and does not clot
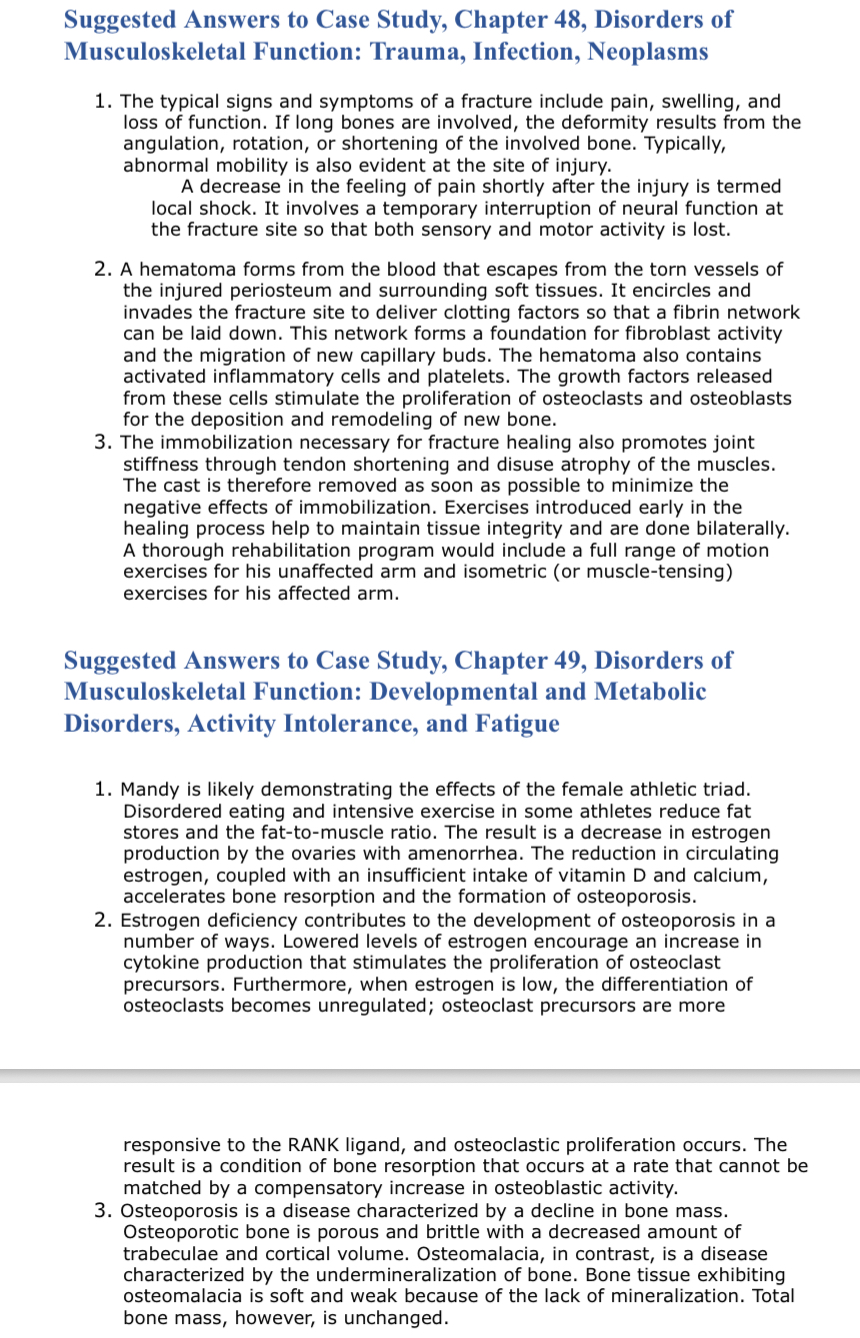
Trauma, Infection and Neoplasms Objectives
Discuss the types, clinical manifestations, and healing process of fractures
closed, open, transverse, or spiral. Symptoms include pain, swelling, bruising, deformity, and loss of function. Healing happens in three stages: inflammation, callus formation, and remodeling.
Differentiate the complications of fractures and musculoskeletal injuries.
poor healing, misaligned bones, infection, compartment syndrome, and fat embolism. Muscle and soft tissue injuries can cause bleeding, chronic pain, stiffness, or abnormal bone growth in the muscle.
Discuss the differences between the etiologies and manifestations of osteomyelitis
bone infection caused by bacteria spreading through the blood, nearby tissue, or trauma. Symptoms include bone pain, swelling, warmth, fever, and sometimes chronic drainage.
Describe four major causes of osteonecrosis
trauma, long-term steroid use, alcohol abuse, or blood flow disorders like sickle cell disease.
Contrast osteogenic sarcoma, Ewing sarcoma, and chondrosarcoma in terms of most common age groups and anatomic sites affected
Osteosarcoma: teens and young adults, usually in long bone ends.
Ewing sarcoma: children/adolescents, often in long bone shafts or pelvis.
Chondrosarcoma: adults 40–70, mostly in pelvis or shoulder bones.
Causes of Musculoskeletal Injuries
Blunt tissue trauma
Disruption of tendons and ligaments
fractures of bony structures
Falls most common cause of injury in patients 65 and older
Classifications of fractures
By cause:
sudden injury
Stress fractures
Pathologic fractures (osteoporosis)
Location:
proximal, midshaft, distal
Types
open or closed (through the skin)
Signs of a fracture
pain
Abnormal mobility
Deformity of the affected part
Loss of function
Swelling
Tenderness at the site of bone disruption
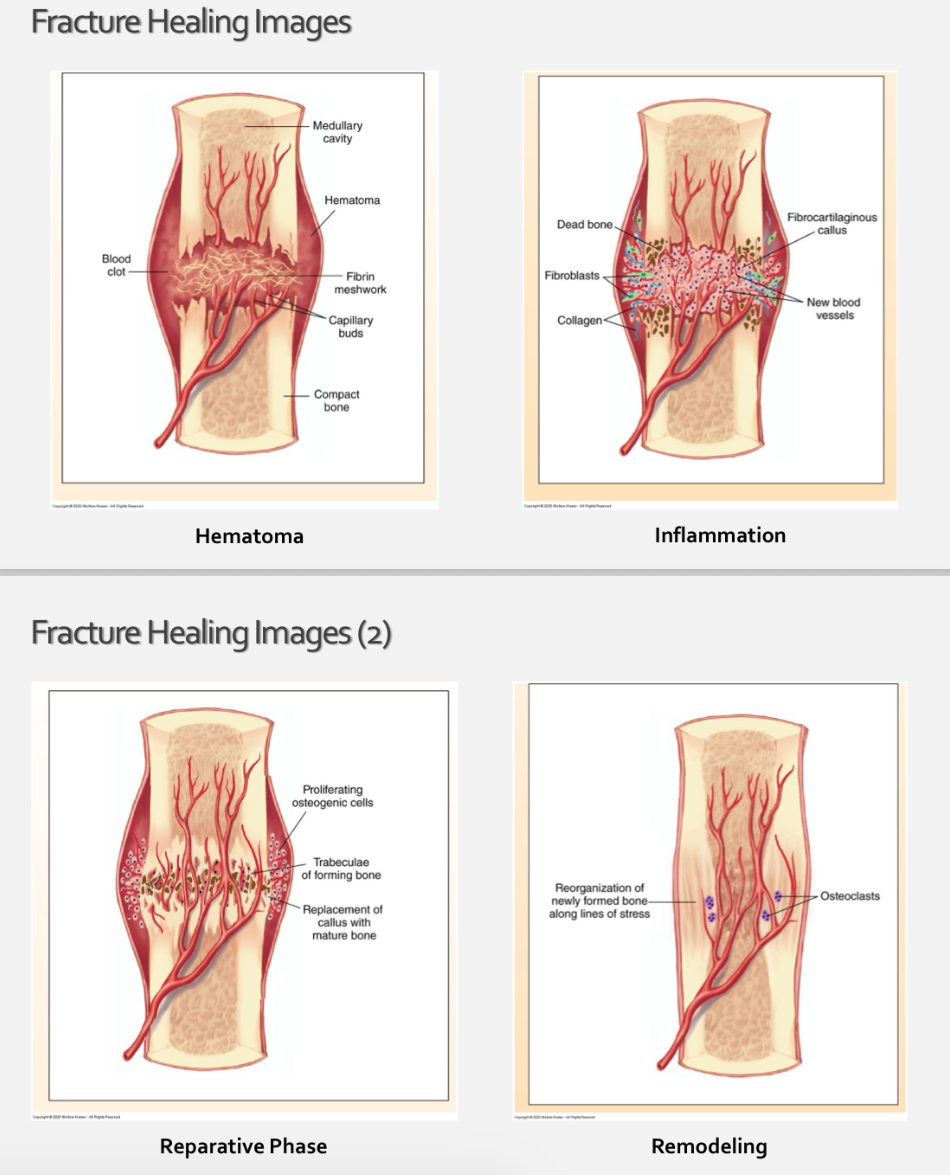
4 stages of bone healing
Hematoma formation
Days 1-5
Inflammatory phase
days 5-11
Reparative
days 11-28
Remodeling
start at day 18 and may continue for many months or years
Factors delaying bone healing
patients age (children heal faster than adults)
current medications
Debilitating disease (diabetes, rheumatoid arthritis)
Local stress around the fracture site
Circulatory problems
Coagulation disorders
Poor nutrition
Complications of Fractures
Injury from bone fragments
Pressure from swelling and hemorrhage (bleeding)
Fracture blisters, compartment syndrome
Development of emboli (clots that move)
Fat emboli an thromboembolic
increase protein for healing
Increased blood sugar makes it harder to help and suppresses osteoblasts
Compartment Syndrome
fluids are fracture blisters
Severe pain that is out of proportion to the original injury or physical findings
Fracture that swells that cuts off blood flow
Thromboemboli
clot that goes to the artery on the way to the lungs (pulmonary embolism)
Symptom: shortness of breath
Disorders
pulmonary embolism
Deep vein thrombosis ( compress devices help)
Diagnostics
venous Doppler ultrasound
Lung scan
Fat Embolism Syndrome
Long one/pelvic fracture→ fat globules entering circulation→ 1. Hypoxemia 2. Neurological abnormalities 3. Petechial rash
Doesn’t blanch
Fat Embolism Syndrome Clinical Manifestations
drowsy
Confusion
Encephalopathy
Seizures
Begins 12-72 hours after injury
First symptoms include a subtle change in behavior
Original of Bone infections
microorganisms introduced during injury
Microorganisms introduced during operative procedures
Microorganisms from the blood stream
Types of Osteomyelitis
Hematogenous Osteomyelitis
originates with infectious organisms that reach the bone through the blood stream
Chills, fever, bacteremia
Contiguous Spread Osteomyelitis
secondary to a contiguous force of infection
Direct inoculation from an exogenous source or from an adjacent extra skeletal site
Most common
Persistent fever
Increased pain at surgical site
Poor wound healing
Chronic osteomyelitis
Occur secondary to an open wound
May not have signs
Bone biopsy for diagnosis
New bone starts to form over dead bone
Osteonecrosis
causes
mechanical disruption of blood vessels
Steroids or radiation
Thrombosis and embolism
Vessel injury
Increased intraosseous pressure (compartment syndrome)
Blood flow
other cortex receives supply form surrounding blood vessels
Some sites have limited collateral circulation; interruption flow affects significant amount of bone tissue
Osteonecrosis Clinical Manifestations
varies depend on extent of infarction
Starts with pain with activity
Progresses to pain at rest
Symptoms of Bone tumor (Neoplasms)
pain
Presence of a mass
Impairment of function
Types of Malignant Bone Tumors
Osteosarcoma:
aggressive and highly malignant
Common in children and adolescents
Most common: primary bone tumor
Ewing Sarcoma:
Peripheral primitive neuroectodermal tumor (PNET)
Often in those under 20 yerars old
Chondrosarcoma
Malignant tumor originating from cartilage cells
Common in adults
Second most common primary bone tumor
Slow growing
Often painless
Treatment goals for metastatic bone disease
preventing pathologic fractures
Promoting survival with maximum functioning
Allowing the person to maintain as much mobility and pain control as possible
What tumor types would most likely metastasize
Osteosarcoma
Metabolic Disorders
Describe risk factors that contribute to to the development of osteopenia, osteoporosis, osteomalacia, and rickets, and relate them to the prevention of the disorder
Osteopenia and osteoporosis are caused by aging, low calcium or vitamin D intake, lack of exercise, smoking, excessive alcohol, and hormonal changes (especially low estrogen). Prevention includes a calcium- and vitamin D-rich diet, regular weight-bearing exercise, and avoiding smoking and excessive alcohol.
Osteomalacia and rickets result from vitamin D deficiency, poor dietary calcium, kidney disease, or limited sunlight exposure. Prevention focuses on adequate vitamin D, calcium intake, and sunlight exposure.
Discuss clinical manifestations and diagnostic criteria for osteopenia, osteoporosis, osteomalacia and rickets
Clinical manifestations:
• Osteopenia: mild bone loss, usually no symptoms, detected by bone density scans.
• Osteoporosis: fractures (especially hip, spine, wrist), loss of height, back pain, kyphosis; diagnosed by DEXA scan showing low bone density.
• Osteomalacia: bone pain, muscle weakness, difficulty walking; diagnosed by low vitamin D, low calcium/phosphate, and X-ray findings.
• Rickets (in children): bowed legs, delayed growth, skeletal deformities; diagnosed by clinical signs, low vitamin D, and X-rays showing soft bones.
Osteopenia
reduction in bone mass greater than expected for age or sex
Causes:
Decrease in bone formation
Inadequate bone mineralization (deossification)
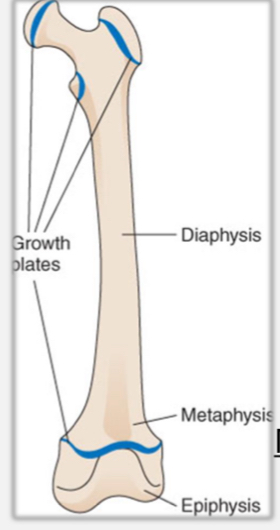
Normal bone growth
long bones grow in length, the deeper layer of cartilage cells in the growth plate multiply and enlarge, pushing articulation cartilage farther away from metaphysisand diaphysis of the bone
Osteoporosis
skeletal disorder
Loss of bone mass and deterioration of architecture of cancellous bone with an increase in bone fragility and susceptibility to fractures
Loss of mineralized bone mass causes increased porosity of skeleton
Causes
Occur as result of endocrine disorder
Aging
Risk factors associated with osteoporosis and clinical manifestations
Personal Characterstics
white
Female
Small bone structure
Postmenopausal
Family history
Hump, decrease in height, predisposition in fractures
Fractures in distal radius, fractured hip, compression fracture of vertebrae
Lifestyle
sedentary, calcium deficient, excessive alcohol and caffeine intake, smoking
Drug related
Disease related
Diagnosis of Osteoporosis
Bone Mineral density assessment
Dual energy x ray absorptiometry of spine and hip
T score:
compares your results to a healthy young adult 20-35 years old
Z score:
results to a person of same gender and age as yourself
-1.5 to -2.4 may indicate osteopenia
Less than -2.5 may indicate osteoporosis
Disorders involving softening of bones
Osteomalacia:
Inadequate mineralization of bone results from a calcium or phosphate deficiency or both
Rickets
vitamin D deficiency, inadequate calcium absorption and impaired mineralization of bone in children
Osteomalacia Clincial manifestations
affects height
Bone pain
Muscle weakness
Fractures
Rickets Clincial Manifestations
bone deformity
Lumbar lordosis
Bowing of legs
What condition results from loss of bone mass
osteoporosis
Rheumatic Disorders
Describe the pathologic changes that may be found in joint of a person with rheumatoid arthritis
autoimmune disease causing inflammation of the joint lining (synovium), leading to swelling, pain, joint deformity, and erosion of cartilage and bone.
Compare rheumatoid arthritis and osteoarthritis in terms of joint involvement, level of inflammation and local and systemic manifestations
Osteoarthritis (OA) is a degenerative joint disease where cartilage wears down, causing bone spurs, joint space narrowing, stiffness, and pain, usually without significant inflammation.
Describe pathologic joint changes associated with osteoarthritis
Comparison: RA often affects small joints symmetrically (hands, wrists) with high inflammation and systemic symptoms like fatigue and fever. OA usually affects weight-bearing or large joints asymmetrically (knees, hips), with mild inflammation and no systemic symptoms.
Pathologic changes in OA include cartilage loss, bone thickening, osteophyte formation, and joint space narrowing, leading to stiffness and reduced mobility.
Systemic inflammatory disease
affects 1-2% of population
Prevalence increases with age
Elderly onset for rheumatoid arthritis is 65
Rheumatoid Arthritis Characteristics
autoimmune
Extra articular
Articular
Slow (insidious) onset with systemic manifestations
Exacerbations and remissions
Only few joints for brief durations but it may get worse
RA Clincial Manifestations
fatigue
Weakness
Anorexia
Weight loss
Low grade fever
Anemia
PAIN
Diagnosis criteria for Rheumatoid arthritis
morning stiffness for 1 hour for at least 6 weeks
Swelling of 3 or more joints for 6 weeks
Swelling or wrist, metacarpophalangeal or proximal joints for more than 6 weeks in your hands
systemic joint swelling
Rheumatoid nodules
Serum rheumatoid factor (RH)
history and physical
Physical exam
ESR
Osteoarthritis
RA causes it
Degenerative joint disease
Localized or generalized syndromes
Secondary OA has known underlying cause
Congenital or acquired defects of joint,structures, trauma, infection, metabolic disorders or inflammatory disease
Pathogenesis of Osteoarthritis
progressive loss of articular cartilage
Synovitis
Osteophytes
Bone spurs
Causes of Osteoarthritis
post inflammatory diseases
Post traumatic disorders
Anatomic disorders
Metabolic disorders
Neuropathic arthritis
Heredity disorders of collagen
Age
Obesity
Osteoarthritis Manifestations
history, physical, x rays, labs
Joint pain
Stiffness
Limitation of motion
Joint instability
Deformity
What describes the primary pathophysiological process in osteoarthritis
progressive loss of articular cartilage with osteophyte formations
How Rheumatoid arthritis leads to joint deformities and reduced mobility
autoimmune
Attacks synovial joint
Chronic inflammation
Pannus formation (abnormal tissue growth)
Cartilage destruction
Erosion
Joint deformity
Compartment syndrome
increased pressure within a loved muscle compartment
Case Study
Ventilation and Diffusion
Ventilation is the mechanical process of air moving into and out of the lungs,
diffusion is the passive movement of gases across the alveolo-capillary membrane from an area of high pressure to low pressure
Acid Base Balance
Differentiate between acids and bases including ph measurements
acids are substances that release hydrogen ions
Bases are substances that acceptt hydrogen ions or release hydroxide ions
Compare the roles of buffer systems in regulation of acid base balance
buffer systems keep blood pH stable
Bicarbonate buffering system is most important, balancing acids and bases through CO2 regulation by the lungs and bicarbonate control by the kidneys
Protein buffers (albumin and hemoglobin) bind or release H+
Phosphate buffers act mainly inside cells and in urine
Identify origin of acid base disturbance
problems with the lungs or metabolism (kidney and tissues)
Respiratory disturbances: caused by changes in CO2 due to ventilation problems
Metabolic disturbances: changes in HCO3- due to kidney function or metabolic processes
Interpret acid base imbalances via arterial blood gas lab values
pH: 7.35-7.45
PaCO2: 35-45 mmHG (respiratory function)
HCO3- (bicarbonate) 22-26 mEq: reflects metabolic function
PaCO2 is abnormal: respiratory cause
HCO30: metabolic cause
Discuss common causes and clinical manifestations of metabolic and respiratory acidosis and metabolic and respiratory alkalosis
Metabolic Acidosis
Kidney failure
Decrease pH, decrease HCO3-
Rapid breathing and confusion
Respiratory acidosis
Hypoventilation (COPD)
decrease pH, increase PaCO2
Headache
Metabolic alkalosis
Vomiting
increase pH and increase HCO3-
Muscle cramping
Respiratory Alkalosis
Hyperventilation
increase in pH, decrease in PaCo2
Dizziness
Acid Base Balance
Regulation of acids and bases is critical for metabolic activities
Narrow ph range is required for function of cells, tissues, and organs
Ph 7.35-7.45
More h+ more acidic
More OH more alkaline
High pH is alkalosis
low pH is acidosis
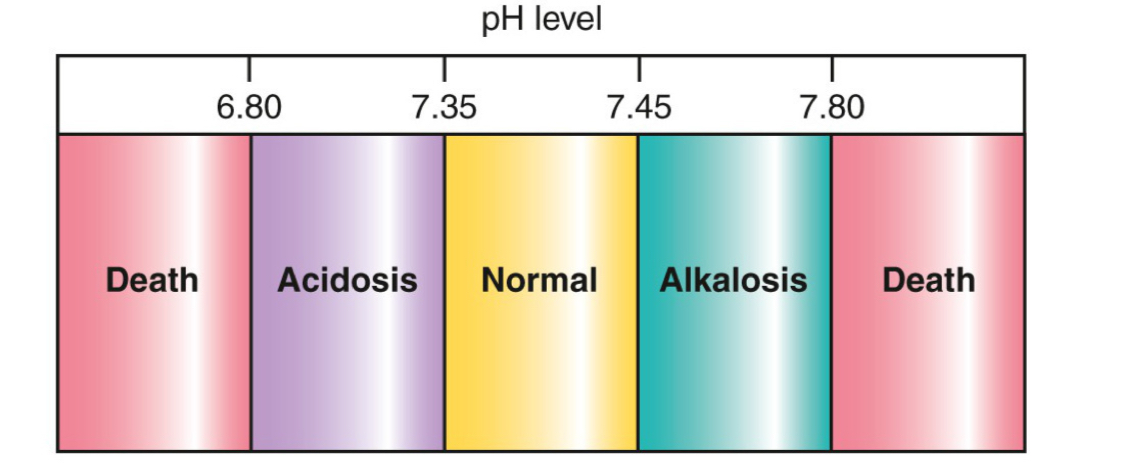
PH balance
represents negative logarithm of H+ ion concentration
PH is inversely related to H+ ion concentration
Low pH indictates high concentration of h+ ions
High pH indicates a low concentration of H+ ions
Anion Gap
Increase in anion gap= metabolic acidosis
Cation - anion
H+ cations can be exchanged with K
H⁺ increases in the blood (acidosis), H⁺ moves into cells and K⁺ moves out to maintain electrical neutrality_
Showing unmeasurable anions in plasma that replace bicarbonate in metabolic acidosis
pH regulators
Chemical buffer systems of body fluids
combine with excess acids or bases to prevent large changes in pH
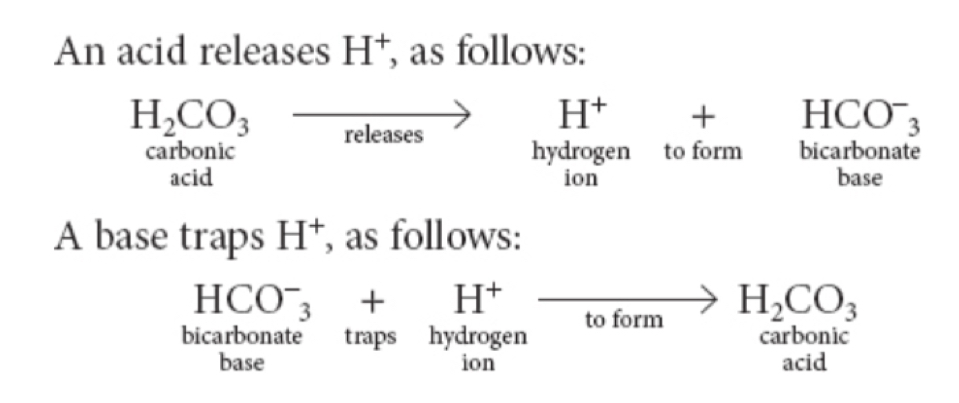
H20+CO2 < - > H2CO3 <- > H+ + HCO3-
Lungs
control elimination of CO2
Kidneys
Eliminate H+ and both reabsorb and generate new HCO3-
Bicarbonate Buffer System
most important buffering system for your body
Weak acids or bases in the body fluids exchange for strong acids or bases to help neutralize
Potassium Hydrogen Exchange System
Excess H+ can be exchanged for K+ across the cell membrane
Chemical Buffering System
largest system
Amphoteric: acid or case
Albumin: intracellular proteins and plasma globulins combine with H+ ions (It helps maintain blood pH by binding hydrogen ions (H⁺) when the blood becomes too acidic)
Example of plasma protein buffer
Respiratory Buffer System
Chemoreceptors and peripheral chemoreceptors sense changes in PaCO2 and pH
INCREASED ventilation DECREASES PaCO2
DECREASED ventilation INCREASES PaCO2
Blood gases
Rise in PaCo2
Central chemoreceptors
Rise in PaCO2, Fall in PaO2, Fall in pH
Peripheral chemoreceptors
excess H+ increased ventilation to prevent acidosis
Not enough H+ decreased ventilation to prevent alkalosis
Rapid acting
Not sufficient to completely normalize pH by itself
Renal Buffer System
3 mechanisms of action
Reabsorbs of HCO3- (bicarbonate and blood is filtering through the kidney)
Produces new HCO3-
H+ combines with phosphate or ammonia to create new HCO3- when homeostasis is reached, excess H+ is excreted
Excretes acids from protein and lipid metabolism
Phosphate and ammonia buffering systems excrete excess H+
Primary source for retaining/creating bases
Takes hour to begin adjusting pH can last days
Complements plasma and respiratory buffering systems for adjusting pH
Review
What causes changes in respirations
chemical receptors in continuous chemoreceptors and peripheral detecting changes in CO2
If there’s too many H+ ions what will the respiratory system do
Increase respirations
What does the kidney produce to neutralize acids
Bicarbonate
Acid Base Imbalances
Respiratory or Metabolic in origin
Respiratory disorders are due to an alternation in CO2
An increase in CO2= respiratory acidosis
A decrease in CO2= respiratory alkalosis
Metabolic disorders are due to an alternation in HCO3-
An increase in HCO3-= metabolic alkalosis
A decrease in HCO3-= metabolic acidosis
Arterial Blood Gas Sampling
Arterial stick performed By MD/RT/RN
Arterial puncture at radial (most of the time), brachial, femoral
Indwelling arterial catheter
Measures pH, acid-base balance and oxygenation status
Allen’s test
ABG Pneumonic
Acid Base Mnemonic (ROME)
Respiratory…Opposite
PH increases, PCO2 decreases= alkalosis
PH decreases, PCO2 increases= acidosis
Metabolic…Equal
PH increases, HCO3 increase =alkalosis
pH decreases, HCO3 decreases= acidosis
Practice 1
PH: 7.30 (acidosis)
CO2: 50 mmHg (respiratory driven)
HCO3-: 24 meq (normal)
respiratory acidosis
Practice 2
PH: 7.50 (alkalosis)
CO2: 43 mmHg (normal)
HCO3-: 28 mEq (metabolic driven)
Metabolic alkalosis
Practice 3
pH: 7.31 (acidosis)
CO2: 36 mmHg (normal)
HCO3-: 12 mEq (metabolic driven)
Metabolic acidosis
Practice 4
PH: 7.48 (alkalosis )
CO2: 28 mmHg (respiratory driven)
HCO3-: 23 mEq (normal)
Respiratory alkalosis
Metabolic Acidosis
Causes
diabetic ketoacidosis
Lactic acidosis
Drug and alcohol overdose
Acute kidney injury
Liver failure
Hyperkalemia
Diarrhea (lose base therefore acidosis)
Metabolic Alkalosis
Causes:
prolonged vomiting (losing acid because stomach has acid)
Diuretic use
Hypokalemia, hypocalcemia, hypochloremia, hypomagnesemia
Antacid abuse
Inadequate renal perfusion
Respiratory Acidosis
Causes
hypoventilation
Over-sedation (retaining extra CO2)
Brain stem dysfunction
Obstructive sleep apnea
Acute respiratory distress syndrome
COPD
Pneumothorax
Respiratory Alkalosis
Causes
Hyperventilation
Anxiety
Acute respiratory distress syndrome
Stroke
Head injury
Altered Ventilation and Diffusion
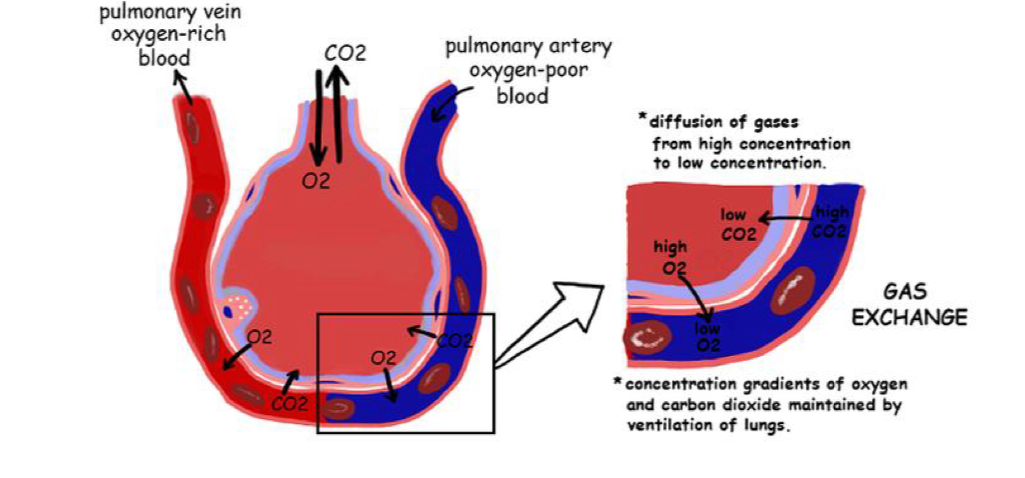
Explain the role of ventilation and diffusion in oxygen/carbon dioxide gas exchange
Ventilation: movement of air in and out of the lungs, bringing oxygen into the alveoli and removing carbon dioxide
Diffusion: O₂ moves from the alveoli into the blood and CO₂ moves from the blood into the alveoli, driven by concentration (partial pressure) differences across the alveolar-capillary membrane.
Compare carbon dioxide and oxygen in maintaining homeostasis
Oxygen: cellular metabolism and energy production,
carbon dioxide: waste product that helps regulate blood pH through the bicarbonate buffer system.
Both gases must be balanced—too little O₂ (hypoxia) or too much CO₂ (hypercapnia) disrupts homeostasis and affects organ function.
Describe the processes that can impair ventilation and diffusion
Ventilation and diffusion can be impaired by airway obstruction, lung diseases (e.g., COPD, asthma, pneumonia), chest trauma, pulmonary edema, or thickening of the alveolar membrane, all of which limit airflow or gas exchange between the lungs and blood.
Explain why ventilation and perfusion must be matched
Ventilation (air reaching alveoli) and perfusion (blood reaching alveoli) must be matched (V/Q balance) so that adequate oxygen enters the blood and carbon dioxide is effectively removed. A mismatch such as in pulmonary embolism or airway obstruction reduces gas exchange efficiency and leads to hypoxemia.
List 3 types of conditions in which hypoxia can occur
Hypoxic hypoxia – due to low oxygen in the air or poor ventilation (e.g., high altitude).
Anemic hypoxia – from low hemoglobin or impaired oxygen-carrying capacity.
Circulatory (stagnant) hypoxia – due to poor blood flow (e.g., heart failure, shock).
Discuss common causes and clinical manifestations of impaired ventilation and diffusion
Causes: COPD, asthma, pneumonia, pulmonary edema, pulmonary embolism, or chest injuries.
Clinical manifestations: Shortness of breath (dyspnea), rapid breathing (tachypnea), cyanosis, confusion, fatigue, and abnormal blood gas values (low PaO₂, high PaCO₂).
A&P of the Respiratory System
upper and lower airways
Upper: nose, mouth, nasopharynx, and oropharynx
Laryngeal pharynx connected the upper and lower airways
Lower: trachea, bronchi, bronchioles and alveoli
Alveoli
Alveolar capillary junction: oxygen and carbon dioxide are exchanged
Type I alveolar cells: provide structure and air exchange
Type II alveolar cells: secrete surfactant
Breathing
Ventilation: process of moving air into and out of the trachea, bronchi and lungs
Diffusion: process of moving and exchanging oxygen and carbon dioxide across the alveolar-capillary membrane
Perfusion: process of supplying oxygenated blood to the lungs and organ system via blood vessels
Respiration: cells throughout the body use oxygen aerobically to make energy
Ventilation
acquire oxygen
Removes carbon dioxide
Cellular metabolism
Intercostal muscles, diaphragm, sternocleidomastoid which aids in chest expansion and recoil
What makes us breathe
drive to ventilate is stimulated by the respiratory control center in the brainstem in response to chemical messages in the body
Respiratory control center comprises of neurons in the pons and medulla
Central Chemoreceptors
detects CO2 changes
Medulla and pons
Central chemoreceptors
Most sensitive
Alter rate of breathing to adapt to higher or lower levels of CO2 in the body
Carbon dioxide is acidic therefore if blood is more acidic, the respiratory center increases the rate and depth of breathing to release excess carbon dioxide
Peripheral Chemoreceptors
most sensitive oxygen levels in the arterial blood (PaO2)
Located in the aorta and carotid arteries
Trigger an increase of ventilation in response to low oxygen levels in the blood
Partial Pressure of Gases
oxygen and carbon dioxide gases are countless particles in constant collison
Force of these collisions forms a pressure
Small amount of oxygen is dissolved and circulating in the plasma
Dissolved portion creates a pressure in the plasma called partial pressure
Partial pressure of oxygen in arterial blood is labeled PaO2
Oxygen Diffusion and Transport
As PaO2 (oxygen in plasma) rises, oxygen moves from the plasma into red blood cells
oxygen is attracted to iron
Oxygen binds to hemoglobin Forming oxyhemoglobin
1 hemoglobin carries 4 oxygen molecules
Binding attraction continues until saturated
oxygen saturation (SaO2) refers to amount of oxyhemoglobin
87-99% of O2 is combined with hemoglobin
When fully saturated, O2 continues to diffuse and dissolve until partial pressure in arteries are equal to partial pressure of the O2 in the alveoli
Diffusion stops until a change in PaO2 in sensed again
dissolved O2 in the plasma is diffused into cells and used for cellular metabolism
Blood moves and senses PaO2 and PaO2 passes the carotid and sends a message to the brain saying they need more oxygen. I actually have no idea what i am writing.