PMLS LECTURE (Finals)
0.0(0)
Card Sorting
1/102
There's no tags or description
Looks like no tags are added yet.
Last updated 3:16 PM on 5/10/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
103 Terms
1
New cards
What top tube should be collected for blood bank test?
▪ RED, LAVENDER, PINK
2
New cards
What are the things blood bank test are strict for?
Blood bank specimens require strict patient identification and specimen labeling procedures.
3
New cards
Possible errors from mislabeling or misidentification procedure for blood bank tests
An undetected error can result in administration of an incompatible blood product and the possibility of a fatal transfusion reaction.
4
New cards
One of the special ID bracelet
PDC Securline Blood Bank (Precision Dynamics Corporation, San Fernando, CA)
5
New cards
BLOOD TYPE, SCREEN, AND CROSS-MATCH
One of the most common tests performed by the blood bank. This test determines a patient’s blood type (ABO) and Rh factor (positive or negative).
6
New cards
BLOOD DONOR COLLECTION
involves collecting blood to be used for transfusion purposes rather than for diagnostic testing.
7
New cards
Age and weight requirement to donate blood
ages of 17 and 66 years and weigh at least 110 pounds.
8
New cards
Special requirement when blood donating for minors
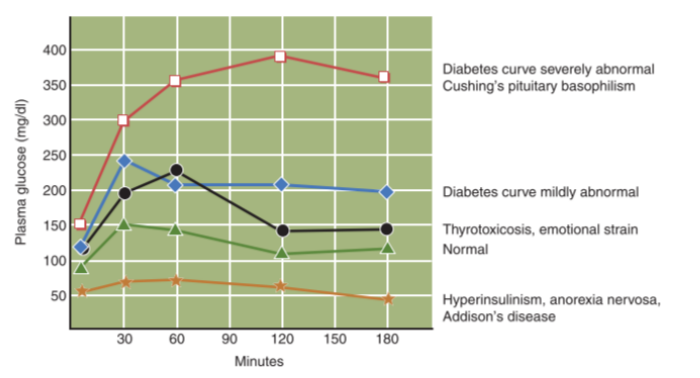
must have written permission from their parents.
9
New cards
Special requirement when blood donating for adults over 66 of age
may be allowed to donate at the discretion of the blood bank physician
10
New cards
The anticoagulant and preservative CPD (citrate–phosphate–dextrose) or CPDA1(CPD plus adenine)
is typically used in collecting units of blood for transfusion purposes
11
New cards
LOOKBACK PROGRAM
requires notification to all blood recipients when a donor for a blood product they have received has turned positive for a transmissible disease. At that point, it is absolutely necessary that verification for all blood components previously collected and currently in inventory has been retrieved.
12
New cards
AUTOLOGOUS DONATION
is the process by which a person donates blood for his or her own use. This is done for elective surgeries when it is anticipated that a transfusion will be needed.
13
New cards
Benefits of Autologous donation
Using one’s own blood eliminates many risks associated with transfusion, such as disease transmission and blood or plasma incompatibilities
14
New cards
Autologous donation minimum time
Although blood is normally collected several weeks prior to the scheduled surgery, the minimum time between donation and surgery can be as little as 72 hours.
15
New cards
CELL SALVAGING
Aqueous solutions, plasma, and serum samples or banked erythrocytes often contain lysed RBCs that have released hemoglobin into the solution. For example, during some surgical procedures, the patient’s blood is salvaged, washed, and reinfused.
16
New cards
ly·sis
Rupture
17
New cards
agglutination
clumping
18
New cards
Results of a high free hemoglobin levels
indicates that too many red cells were destroyed during the salvage process and renal dysfunction could result if the blood were reinfused.
19
New cards
instrument to detect free hemoglobin
using point-ofcare instruments such as the HemoCue Plasma/Low Hemoglobin analyzer
20
New cards
the size of the needle and the location to puncture a donor unit
Donor units are normally collected from a large antecubital vein using a sterile 16- to 18-gauge needle.
21
New cards
The size of the bag for blood donor and what happens when a bag is partially filled?
The unit is normally filled by weight but typically contains around 450 mL of blood when full. Only one needle puncture can be used to fill a unit. If the unit only partially fills and the procedure must be repeated, an entire new unit must be used.
22
New cards
BLOOD CULTURES
help determine the presence and extent of infection as well as indicating the type of organism responsible and the antibiotic to which it is most susceptible. They are also useful in assessing the effectiveness of antibiotic therapy once treatment is initiated. This should be ordered on the basis of whether the patient has a condition in which bloodstream invasion is possible and not only when a patient experiences a fever of unknown origin (FUO).
23
New cards
bacteremia
bacteria in the blood
24
New cards
septicemia
microorganisms or their toxins in the blood
25
New cards
TIMING FOR BLOOD CULTURE DRAWING
are typically ordered immediately before or after anticipated fever spikes when bacteria are most likely to be present. The best chance for detecting bacteremia exists from ½ hour to 2 ½ hours prior to the next fever peak
26
New cards
How many specimens for blood culture?
The most recent literature of the American Society for Microbiology (ASM) states that two to four blood cultures are necessary to optimize the detection of bacteremia and fungemia. For optimum results, such specimens should be drawn 30 to 60 minutes apart.
27
New cards
BLOOD CULTURE MINIMUM VOLUME
10 ml is usually the minimum volume.
28
New cards
BLOOD CULTURE VOLUME FOR INFANTS AND YOUNGER CHILDREN
1% to 4% of the patient’s total blood volume,
29
New cards
bloood culture volume for For adults or people weighing more than 80 pounds.
20 to 30 mL per culture with a minimum of 10 mL per draw.
30
New cards
THREE OTHER TYPES OF ANTISEPTIC FOR BLOOD CULTURE
* 10% providone or 1-2% tincture of iodine
* Benzalkonium chloride
* Chlorhexidine gluconate/isopropyl alcohol
* Benzalkonium chloride
* Chlorhexidine gluconate/isopropyl alcohol
31
New cards
MEDIA INOCULATION METHODS
Inoculation is the purposeful introduction of bacteria into a sterile growth medium. A material is sterile when it has no living organisms present; contamination is the presence of unwanted microorganisms. Inoculation of media can occur several different ways: directly into the bottle during specimen collection or after collection as when blood has been collected in a syringe. • A third way is to use an intermediate collection tube to collect the sample for inoculation in the laboratory and not at the bedside.
32
New cards
antimicrobial (antibiotic) therapy
Presence of the antimicrobial agent in the patient’s blood can inhibit the growth of the microorganisms in the blood culture bottle.
33
New cards
fastidious antimicrobial neutralization (FAN) (bioMerieux) or antimicrobial removal device (ARD)
In such cases, the physician may order blood cultures to be collected in these forms in order to blood culture without it being contaminated.
34
New cards
antimicrobial removal device (ARD)
contains a resin that removes antimicrobials from the blood
35
New cards
fastidious antimicrobial neutralization (FAN)
contain activated charcoal, which neutralizes the antibiotic.
36
New cards
Postprandial (PP)
means after a meal.
37
New cards
2 HOUR POSTPRANDIAL GLUCOSE
a glucose test on a specimen collected 2 hours after a meal (2-hour PP) is an excellent screening test for diabetes and other metabolic problems.a glucose test on a specimen collected 2 hours after a meal (2-hour PP) is an excellent screening test for diabetes and other metabolic problems.
38
New cards
GLUCOSE TOLERANCE TEST
is used to diagnose problems of carbohydrate metabolism. The major carbohydrate in the blood is glucose, the body’s source of energy. This evaluates the body’s ability to metabolize glucose by monitoring the patient’s tolerance to high levels of glucose without adverse effects.
39
New cards
The two major types of disorders involving glucose metabolism
Hyperglycemia & Hypoglycemia
40
New cards
hyperglycemia
glucose level is increased
41
New cards
hypoglycemia
blood glucose levels are decreased
42
New cards
GTT preparation
* The patient must eat balanced meals containing approximately 150 grams (g) of carbohydrate for 3 days before the test and must fast for at least 12 hours but not more than 16 hours prior to the test.
* The patient is allowed to drink water during the fast and during the test to avoid dehydration and because urine specimens may be collected as part of the procedure.
* The patient is also not allowed to smoke or chew gum, as these activities stimulate the digestive process and may cause erroneous test results. The patient should receive both verbal and written instructions to ensure compliance.
* The patient is allowed to drink water during the fast and during the test to avoid dehydration and because urine specimens may be collected as part of the procedure.
* The patient is also not allowed to smoke or chew gum, as these activities stimulate the digestive process and may cause erroneous test results. The patient should receive both verbal and written instructions to ensure compliance.
43
New cards
GTT Graph reading
In normal patients, blood glucose levels peak within 30 minutes to 1 hour following glucose ingestion. The peak in glucose levels triggers the release of insulin, which brings glucose levels back down to fasting levels within about 2 hours and no glucose spills over into the urine. • Diabetics have an inadequate or absent insulin response; consequently, glucose levels peak at higher levels and are slower to return to fasting levels. If blood is not drawn on time, it is important for the phlebotomist to note the discrepancy so that the physician can take this into consideration.
44
New cards
A lactose tolerance test
is used to determine if a patient lacks the enzyme (mucosal lactase) that is necessary to convert lactose, or milk sugar, into glucose and galactose.
45
New cards
mucosal lactase
enzyme use to convert lactose into glucose and galactose
46
New cards
If the patient is lactose intolerant
the glucose curve will be flat, rising no more than a few mg/dL from the fasting level. Some individuals normally have a flat GTT curve (resulting in a false-positive result); it is then suggested that they have a 2-hour GTT performed the day before the lactose tolerance test so that results can be evaluated adequately.
47
New cards
Paternity testing
is performed to determine the probability that a specific individual fathered a particular child.
48
New cards
paternity testing preparation
Testing may be requested by physicians, lawyers, child support enforcement bureaus, or individuals. It is requires a chain-of-custody protocol and specific identifi cation procedures that may include fingerprinting. A photo identification document such as a passport is usually required. The mother, child, and alleged father are all tested. Blood samples are preferred for testing; however, buccal (cheek) swabs are increasingly being used.
49
New cards
THERAPEUTIC DRUG MONITORING
the testing of drug levels at specific intervals, is used in the management of patients being treated with certain drugs in order to help establish a drug dosage, maintain the dosage at a therapeutic (beneficial) level, and avoid drug toxicity.
50
New cards
THERAPEUTIC PHLEBOTOMY
involves the withdrawal of large volumes of blood usually measured by the unit (as in blood donation), or approximately 500 mL. It is performed by phlebotomists who have been specially trained in the procedure or in donor phlebotomy, as the procedure is similar to collecting blood from donors. It is used as a treatment for certain medical conditions such as polycythemia and hemochromatosis.
51
New cards
Polycythemia
is a disease involving the body’s overproduction of RBCs, which is detrimental to the patient’s health and the most common reason for performing therapeutic phlebotomy. The patient’s RBC levels are monitored regularly, usually by the hematocrit test. Periodic removal of blood when the hematocrit exceeds a certain level is used to help keep the patient’s RBC levels within the normal range.
52
New cards
Hemochromatosis
is a disease characterized by excess iron deposits in the tissues. It can be caused by a defect in iron metabolism or result from multiple blood transfusions or excess iron intake. Periodic removal of single units of blood from the patient gradually depletes iron stores because the body then uses the iron to make new RBCs to replace those removed.
53
New cards
TOXICOLOGY
is the scientific study of toxins (poisons).
54
New cards
Clinical toxicology
is concerned with the detection of toxins and treatment for the effects they produce.
55
New cards
Forensic toxicology
is concerned with the legal consequences of toxin exposure, both intentional and accidental.
56
New cards
what Toxicology tests examines?
blood, hair, urine, and other body substances for the presence of toxins, which often exist in very small amounts.
57
New cards
FORENSIC SPECIMENS
is to collect evidence that may help prove or disprove a link between individuals and/or between individuals and objects or places
58
New cards
Chain of custody
requires detailed documentation that tracks the specimen from the time it is collected until the results are reported. The specimen must be accounted for at all times. If documentation is incomplete, legal action may be compromised. Information on the form also includes the time, date, and place where the specimen was obtained, along with the signature of the person from whom the specimen was taken. Patient identification and specimen collection take place in the presence of a witness, frequently a law enforcement officer, in which case protocol and packaging are completed by the officer before the specimen is sent to a crime laboratory for analysis. Any person who is involved in drawing a blood alcohol specimen for legal reasons can be summoned to appear in court.
59
New cards
BLOOD ALCOHOL (ETHANOL) SPECIMEN
test is commonly used to see if a person has been drinking alcohol recently. This test can find alcohol in your blood for up to 12 hours after drinking. It can also show the amount of alcohol that you drank.
60
New cards
ANTISEPTIC USE FOR TESTING BLOOD ALCOHOL
70% isopropyl alcohol used for routine venipuncture site preparation or other alcohols such as methanol and ethyl alcohol cannot be used for a BAC collection. • Tincture of iodine contains alcohol and likewise should not be used to clean the site. The most frequently used antiseptics for ETOH specimen collection are aqueous povidone–iodine and aqueous benzalkonium chloride (BZK). If an alternative antiseptic is not available, regular soap and water can be used.
61
New cards
DRUG SCREENING
Testing is typically performed on urine rather than blood because it is easy to obtain and a wide variety of drugs or their metabolites (products of metabolism) can be detected in urine for a longer period of time
62
New cards
TRACE ELEMENTS
metals include aluminum, arsenic, copper, lead, iron, and zinc. These elements are measured in such small amounts that traces of them in the glass, plastic, or stopper material of evacuated tubes may leach into the specimen, causing falsely elevated test values.
63
New cards
LABELING AND HANDLING (NONBLOOD SPECIMEN)
* should include the type and or source of the specimen
* should be labeled with the same identifying information as blood specimens
* should be applied to the container, not the lid.
* should be labeled with the same identifying information as blood specimens
* should be applied to the container, not the lid.
64
New cards
URINE
• Most frequently analyzed nonblood body fluid
65
New cards
TYPES OF SPECIMENS
Random, First morning , and the Midstream clean-catch
66
New cards
Random
most commonly received specimen because of its ease of collection and convenience for the patient. May be collected at any time. Useful for routine screening tests to detect obvious abnormalities.
67
New cards
First Morning
ideal screening specimens. Essential for preventing-false negative pregnancy tests and for evaluating orthostatic proteinuria. Concentrated
68
New cards
Midstream Clean-Catch
safe, less traumatic method for obtaining urine for bacterial culture and routine urinalysis. Less contaminated by epithelial cells and bacteria and therefore is more representative of the actual urine than the routinely voided urine
69
New cards
AMNIOTIC FLUID
Clear, almost colorless to pale-yellow fluid that fills the membrane that surrounds and cushions a fetus in the uterus
70
New cards
WHEN CAN WE COLLECT AMNIOTIC FLUID?
• Collected after 15 weeks gestation
71
New cards
TYPES OF TESTS FOR AMNIOTIC FLUID AND ITS TEMPERATURE
* Chromosome analysis: room temp
* Some chemistry tests: kept on ice
* Some chemistry tests: kept on ice
72
New cards
AMNIOTIC FLUID USES
• Used to detect problems in fetal development (neural tube defects; spina bifida) and assess fetal lung maturity
73
New cards
CEREBROSPINAL FLUID (CSF)
Clear, colorless liquid that surrounds the brain and spinal cord
74
New cards
THE THREE TUBES FOR CSF AND ITS TEMPERATURE
1st tube collected is used for chemistry an immunology (frozen), 2nd for microbiology studies (RT), 3rd for cell counts (refrigerated)
75
New cards
CEREBROSPINAL FLUID (CSF) uses
Primary reason for collecting CSF is to diagnose meningitis (brain abscess, CNS cancer and multiple sclerosis)
76
New cards
GASTRIC FLUID/ GASTRIC ANALYSIS
• Stomach fluid
77
New cards
GASTRIC FLUID/ GASTRIC ANALYSIS uses
Examines stomach contents for abnormal substances and measures gastric acid concentration to evaluate stomach acid production
78
New cards
THE TEST FOR GASTRIC FLUID
Basal gastric Analysis - Aspirating a sample of gastric fluid by means of a tube passed through the mouth and throat or nose and throat - Used to determine acidity prior to stimulation - after basal sample has been collected, a gastric stimulant (mc: histamine or pentagastrin) is administered IV and more gastric samples are collected.
79
New cards
NASOPHARYNGEAL SECRETION
• Comprised of the nasal cavity and pharynx
80
New cards
HOW IS NASOPHARYNGEAL COLLECTED?
NP spx: collected using sterile Dacron or cotton-tipped flexible wire swab. - Swab is inserted gently into the nose and passed into the nasopharynx - Gently rotated, then carefully removed, placed in a sterile tube containing transport medium, labeled, and delivered to the lab.
81
New cards
NASOPHARYNGEAL SECRETION uses
Detect presence of microorganisms causing diphtheria, meningitis, pertussis (whooping cough), and pneumonia
82
New cards
SALIVA
• Fluid secreted by glands in the mouth
83
New cards
SALIVA uses
Used to monitor: - hormone levels (salivary amylase) - detect alcohol - Detect drug abuse because it can be collected quickly and easily in a noninvasive manner
84
New cards
SEMEN (SEMINAL FLUID)
Sperm-containing thick yellowish-white fluid discharged during male ejaculation
85
New cards
HOW IS SEMEN COLLECTED AND MAINTAIN
Collected in a sterile or chemically clean containers and must be kept warm, protected from light, and delivered to the lab immediately. Semen should not be collected in a regular condom because it often contain spermicides (substances that kill sperm) that invalidate test results.
86
New cards
SEMEN (SEMINAL FLUID) uses
Assess fertility or determine the effectiveness of sterilization following vasectomy. Forensic or legal issues (criminal sexual investigations)
87
New cards
SEROUS FLUIDS
Pale yellow, watery, serum-like fluid found between the double-layered membranes enclosing the pleural, pericardial, and peritoneal cavities.
88
New cards
SEROUS FLUID TESTS
* EDTA : cell count or smears
* Heparin / Sodium fluoride : chemistry tests
* Nonanticoagulated : biochemical tests
* Sterile heparinized tube : cultures
* Heparin / Sodium fluoride : chemistry tests
* Nonanticoagulated : biochemical tests
* Sterile heparinized tube : cultures
89
New cards
(Mycobacterium tuberculosis)
* bacteria that causes TB: acid-fast bacillus
* sputum test: AFB culture
* First morning specimens : preferred
* Collected from a sputum and usually 1 hour after a meal to minimize the risk that the px will gag or vomit
* - Transported at RT and require immediate processing upon arrival in the lab to maintain spx quality.SP
\
* sputum test: AFB culture
* First morning specimens : preferred
* Collected from a sputum and usually 1 hour after a meal to minimize the risk that the px will gag or vomit
* - Transported at RT and require immediate processing upon arrival in the lab to maintain spx quality.SP
\
90
New cards
SWEAT
Chloride content in the diagnosis of cystic fibrosis, predominantly in children and adolescents under the age of 20
91
New cards
SWEAT uses
Can be used to detect illicit drug use. Sweat is collected on patches places on the skin for extended periods of time and then tested for drugs.
92
New cards
SWEAT TEST
CF px have abnormally high levels of chloride in their sweat (2-5x higher) - Transporting pilocarpine (a sweatstimulating drug) into the skin by electrical stimulation from electrodes placed on the skin, a process called iontophoresis
93
New cards
SYNOVIAL FLUID
Clear, pale-yellow, viscous fluid that lubricates and decreases friction in movable joints.
94
New cards
SYNOVIAL FLUID USES
Identify or differentiate arthritis, gout, and other inflame conditions.
95
New cards
SYNOVIAL FLUID tubes and tests
Collected in three tubes: -
* EDTA/Heparin : cell counts, crystal ID, and smear prep -
* Sterile tube : culture and sensitivity -
* Nonadditive tube : macroscopic appearance, chemistry, immunology tests, and to observe clot formation.
* EDTA/Heparin : cell counts, crystal ID, and smear prep -
* Sterile tube : culture and sensitivity -
* Nonadditive tube : macroscopic appearance, chemistry, immunology tests, and to observe clot formation.
96
New cards
BUCCAL SWABS
\: less invasive, painless alternative to blood collection for obtaining cells for DNA analysis
97
New cards
HOW TO OBTAIN A BUCCAL SWABS
Gently massage mouth on the inside of the cheek with a special swab, • DNA is later extracted from the cells on the swab.
98
New cards
BONE MARROW
Site of blood cell production obtained by a physician only Hematology and Histopathology Department
99
New cards
BREATH SAMPLES
* C-Urea Breath Test – Helicobacter pylori
* Hydrogen Breath Test – Lactose intolerance
* Hydrogen Breath Test – Lactose intolerance
100
New cards
HAIR
• Trace heavy metal analysis • Detection of drugs of abuse