Pharmacology Exam 1 - How to do Drugs
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
87 Terms
The study of the relationship between drug concentration and physiological response is ...
Pharmacodynamics
ex. anti-inflammatory
The study of the time course of drug absorption, distribution, metabolism, and excretion is called:
Pharmacokinetics
The use of drugs in the treatment of disease is:
Pharmacotherapy
Pharmacology founded on observation of patient treatment is ...
Clinical pharmacology
What are the drug nomenclature names?
Chemical name (7-chloro-1,3-dihyrdo-1-...)
Nonproprietary (generic) name (Diazepam)
Proprietary (brand) name (Valium)
Drugs achieve a pharmacological response, the magnitude of which is determined by ...
The number of receptors
Drug ___ and ___ determine plasma/tissue concentrations, while biotransformation ____ and ____ terminate drug actrion
Absorption
Distribution
Metabolism
Excretion
Drugs pass across membranes via ___ and ___ transport processes
Passive and active
The most important mechanism of drug transfer is ...
Passive diffusion
Any molecule with sufficient ____ can cross via passive diffusion
lipid solubility
What factors are directly proportional to the rate of drug transport?
What factors are inversely related?
Direct: Concentration gradient, lipophilicity
Inverse: Molecular weight, membrane thickness, polarity
Does carrier mediated transport require energy?
Depends
Facilitated diffusion - no energy
Active transport - energy
Carrier mediated transport is saturable, meaning ...
At a certain point, adding more into the blood will not affect it if there are no more carriers for the higher concentration, meaning it is competitive
Physiochemical factors are site dependent, and for drugs crossing the skin, ___ is of great importance
Lipid solubility (as opposed to drugs outside of capillary beds, since they are very good for passive diffusion)
Most drugs are weak acids or bases and are present as nonionized or ionized, meaning ...
Nonionized: lipid soluble, diffuse across cell membrane
Ionized: Low lipid solubility, can't cross lipid membrane
What is the formulas for percent ionization?
100/(1 + antilog(x))
x = pKa - pH if weak acid
x = pH - pKa if weak base
How do you calculate an antilog?
An antilog counts the number of places that a decimal is moved from the number one.
antilog(0) = 1 (moved 0 decimal places)
antilog(3) = 1000 (moved 3 decimal places right)
antilog(5) = 100000 (moved 5 decimal places right)
antilog(-3) = 0.001 (moved 3 decimal places left)
Calculate the percent ionization of a weak acid with pKa = 4 in a pH = 3
What about a weak base with pKa = 8 in a pH = 3?
antilog(4 - 3) = antilog(1) = 10
100/(1 + 10) = 9.1% ionized
antilog(3 - 8) = antilog(-5) = 0.00001
100/(1 + 0.00001) = 99.999% ionized
Weak bases are more ionized in ___ environments, and vice versa
acidic
An acidic drug will accumulate on the more (acidic/basic) side of the membrane
Basic, because that will ionize it and it won't pass the membrane easily
If pKa and pH differ by 1, the ratio of U:I varies by ___ fold
10
What is the rate limiting step of release of an orally administered drug?
Dissolution (salts dissolute faster)
What is micronization for?
To enhance absorption by decreasing particle size
What is Griseofluvin for?
Fungal infection of skin, hair, and claws in dogs/cats/horses
Microsize absorption: 25 - 70%
Ultramicrosize: 100%
Generally, food (prevents/enhances) absorption
However, if a drug is ____, this affect is swapped
Prevents, due to dilution and blocking surface area. Lipophilic drugs
What are the major factors affecting the small intestine's drug absorption?
pH
Epithelial surface/surface area
Motility
Efflux proteins (P-glycoprotein)
- Fights against drug absorption
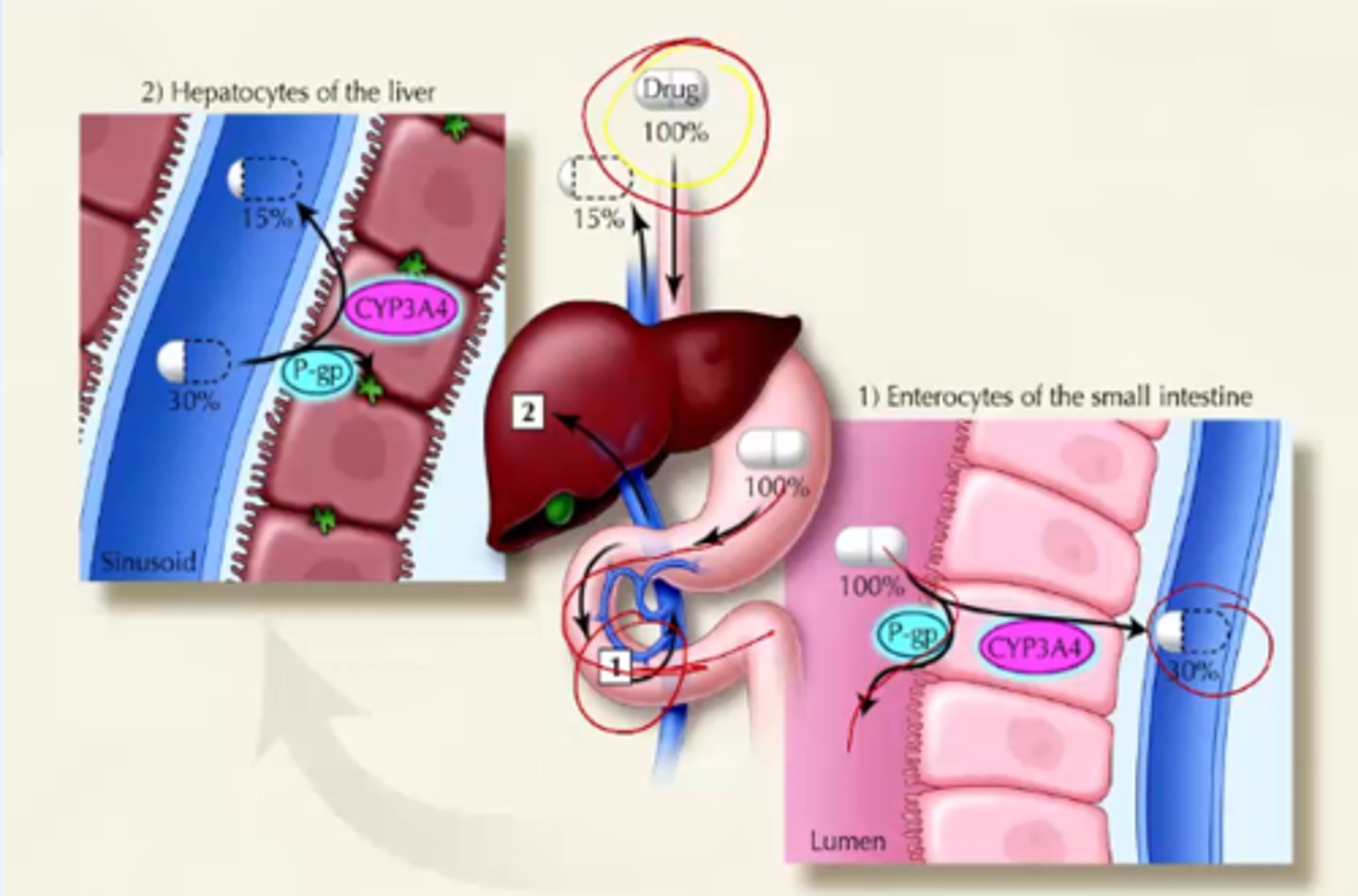
If a drug somehow escapes the GI tract, it then encounters the evil ...
Liver! May be removed entirely with the "first pass effect"
So dosages take into account that 90% of the drug may be metabolized by the liver
The rate/extent a drug will enter systemic circulation is ...
Bioavailability
Take 2 grams, 0.3 enters circulation, only 15% bioavailable
Bioavailability is described by three aspects of the function:
Peak plasma concentration (Cmax)
Time to reach Cmax
Area under the curve (AUC)
The major reason for species differences in doses is ...
Bioavailability
What is firocoxib for?
Pain/inflammation associated with osteoarthritis in dogs (Previcox) and horses (Equioxx)
0.1 mg/kg in horses and 5 mg/kg in dogs due to bioavailability
Administering drugs _____ will give 100% bioavailability
intravenously
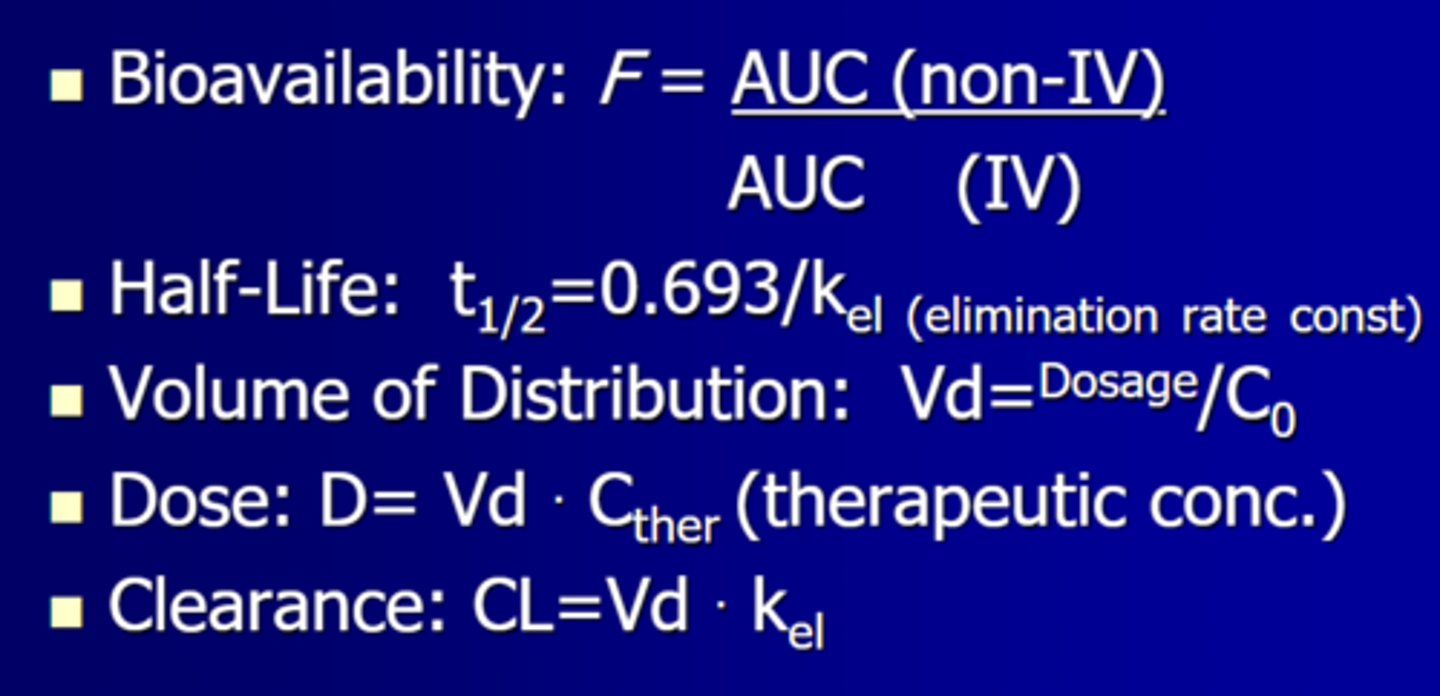
Bioavailability is calculated using the formula:
F = (Oral AUC)/(IV AUC)
So it is the fraction of the area of the curves of oral over IV
What factors may negatively affect bioavailability?
Poor dissolution
Instability, inactivation
Poor passage
First pass metabolism
What is buprenorphine for?
Low/high first pass?
Administration?
Pain management in in cats
Oral, with extensive first pass metabolism
Giving transmucosally (pKA = 8.24, saliva = 8-9)
What are the factors affecting drug distribution?
Physiochemical properties of the drug
- pKa
- Lipid solubility
- Molecular weight
Conc. Grad. between blood and tissue
Ratio of blood flow to tissue mass
Affinity of drug to tissue constituents
How do insoluble drugs travel in the blood?
On plasma proteins (albumin)
They are inactive when bound
What are some potential setbacks when dealing with drugs that are highly protein bound?
Administering 2 drugs will yield competition, leading to a higher free drug concentration
An injured dog with an unknown but lower protein count will need a different dosage than usual to avoid overdose
What proteins do acidic and basic drugs bind to?
Acid: Albumin (50% - 55%)
Base: alpha - 1- acid glycoproteins and lipoproteins
Ivermectin toxicity is due to a gene mutation that leads to decreased production of ...
P-glycoprotein, meaning the blood brain barrier was easier to cross
The theoretical volume required for a set drug dosage to create a specific plasma concentration is ...
Volume of distribution
25 mg/L plasma conc. desired
Have 500 mg of a drug
Vd = 20 liters (since 500/20 = 25)
What areas of the body are the following drugs limited/allowed to?
Protein-bound
Water soluble
Lipid spluble
Protein: Limited to plasma since proteins don't pass
Water: Can pass to the extracellular fluid, as well as plasma
Lipid: Distributed to plasma, ECF, and ICF, equivalent to total body water
To determine the dose of a drug, the equation is ...
Dose = Volume of Distribution (Vd) * Target conc.
500 mg = (20 L) * (25 mg/L)
A drug with a very large volume of distribution implies ...
The drug is trapped
(500 mg)/(2000 L) = 0.25 mg/L
=> small plasma conc.
=> large tissue conc.
=> trapped in tissues
Drug metabolism typically involves the enzymatic alteration to make it (more/less) lipid soluble and (more/less) polar
Less lipid soluble and more polar so it doesn't travel through cells and stays in the blood to reach organs of excretion
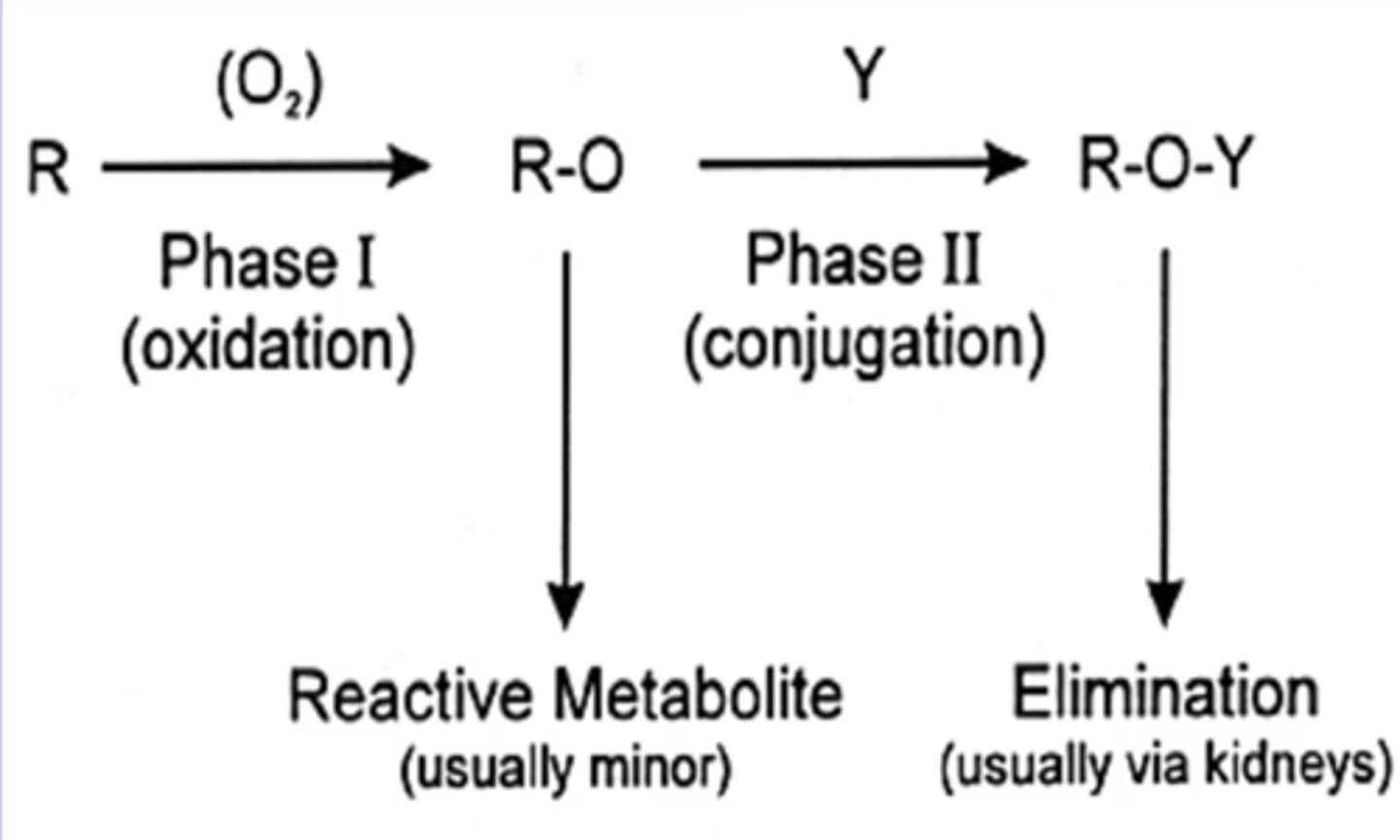
General metabolism is biphasic. Those two phases involve:
Phase 1: Add a polar group (-OH or -COOH)
Phase 2: Conjugation to endogenous compounds, typically water soluble
Note: Not necessarily sequential (Either or both phases can be absent)
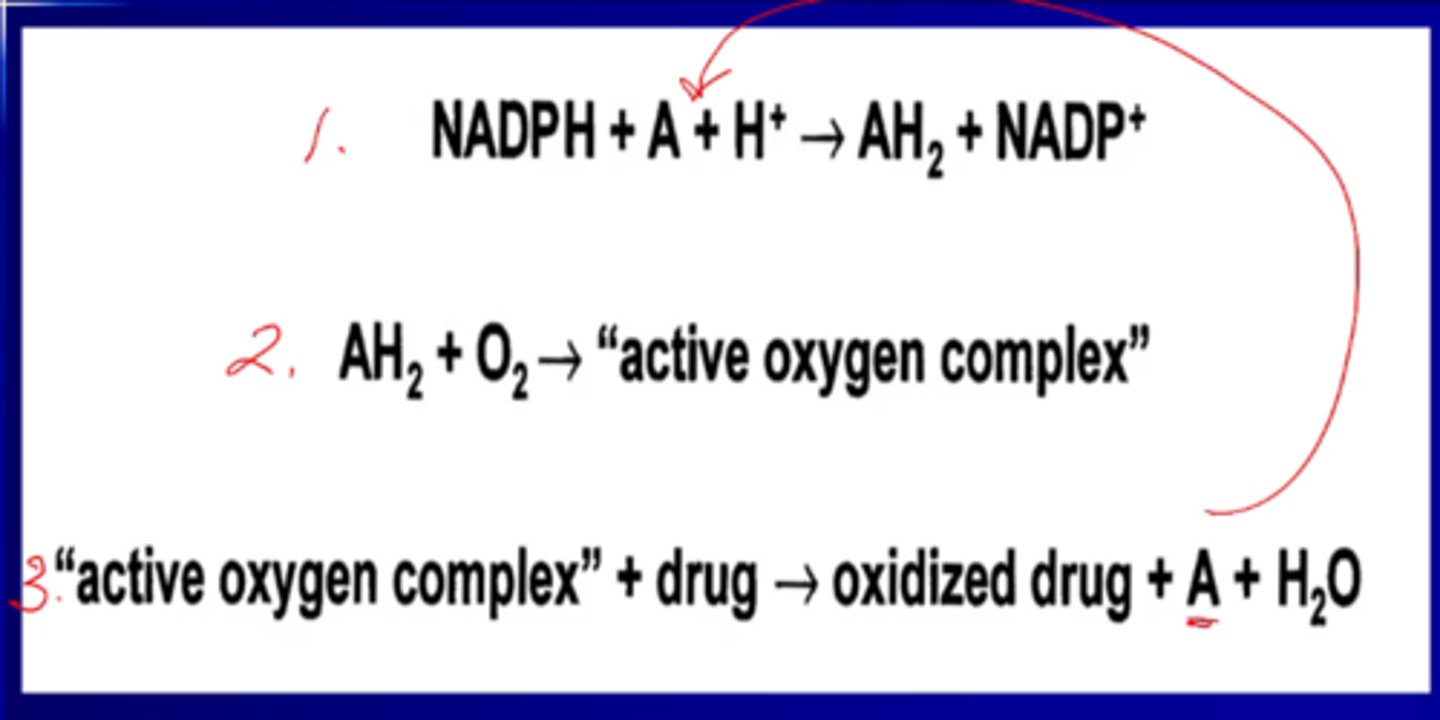
Cytochrome P450 is a major phase (1/2) metabolic enzyme
Phase 1
It is key in producing an "active oxygen complex" which will oxidize drugs
What are the 3 effects of phase 1 metabolic reactions?
1) Active drug --> inactive metabolite
2) Active drug --> active metabolite
3) Inactive drug (pro-drug) --> active drug
4)
Note: active drug --> toxic metabolite
Phase II reactions are synthetic reactions that combine a ____ with a natural compound to form a readily excreted polar metabolite
Drug or phase I metabolite
The most common conjugating agent is ....
Glucuronic acid
Why would you give a cat a drug less often than a dog?
They are poor glucuronic acidifiers, so they can't convert drugs to excretable metabolites very quickly
T/F: Cats get acetaminophen toxicity because normally, 42% of acetaminophen is turned into glucuronide, but since cats are bad at that, it is overwhelmed and instead turns to NAPQI, which is toxic
True, leads to cyanosis
GI microorganisms can mediate metabolic transformations, including:
Hydrolysis and reduction reactions
Renal excretion is the principle route for drugs that ...
have limited lipid solubility and are ionized at physiological pH
What are the three mechanisms of renal excretion?
1) Glomerular filtration
2) Carrier mediated excretion (polar)
3) Passive reabsorption
T/F: Biliary excretion involves the reversible transfer from plasma to bile
False, it is irreversible
What sort of compounds are conjugated by hepatocytes?
What is the conjugate?
High MW, polar compounds
Glucuronic acid
T/F: Once a drug glucuronide enters the intestines by the bile duct, it is always excreted
False, glucoronidase in the intestines will reactivate it, and it can be absorbed again (enterohepatic circulation)
Enterohepatic circulation, inhibited renal/biliary secretion, and drug competition will all the drug's ...
Dosage
Parentral administration means ...
The GI tract is bypassed (IV, IM, SQ)
Doctors give local anesthetics with epinephrine because ...
It is a vasoconstrictor and keeps the anesthetic in the site of action longer
Drugs delivered across the skin (transdermal) are ...
Percutaneous absorbed
Must be lipophilic
Buccal, sublingual, intranasal, and rectal are all examples of ...
transmucosal administration
What is buprenorphine?
How is it administered
Opioid agonist used to treat mild/moderate pain in dogs/cats
Transdermal or buccal
The study of the time course of ADME principles is ...
Pharmacokinetics
The rate and extent a drug enters circulation is ...
Bioavailability (F)
Bioavailability is described by three factors:
Peak plasm concentration (Cmax)
Time to reach peak
Area under the curve (AUC)
The curve that graphically defines the time course, described in its entirety by the area under the curve, is the ...
Disposition curve
The bioavailability of an IV drug is ...
100%
Comparing an IV drug versus non-IV, it is called ...
Comparing two non-IV drugs is called ...
Absolute bioavailability
Relative bioavailability
What are the two phases associated with IV administration?
Alpha/Distribution phase: rapidly distribute to tissues
Beta/Elimination phase: removal of drug via biotransformation
The fraction of drug eliminated per unit of time is denoted as ___ and is determined by ...
Elimination rate (K_el)
Slope of beta phase
K_el = 0.1 implies __% of that drug is eliminated per minute
K_el = 0.3 implites __%
10%
30%
The time required for the body to eliminate 1/2 of the drug from the blood is called ...
Half-life
What is equation for half-life?
T(1/2) = 0.693/(K_el)
What are the two major determinants of half life?
Drug distribution and clearance
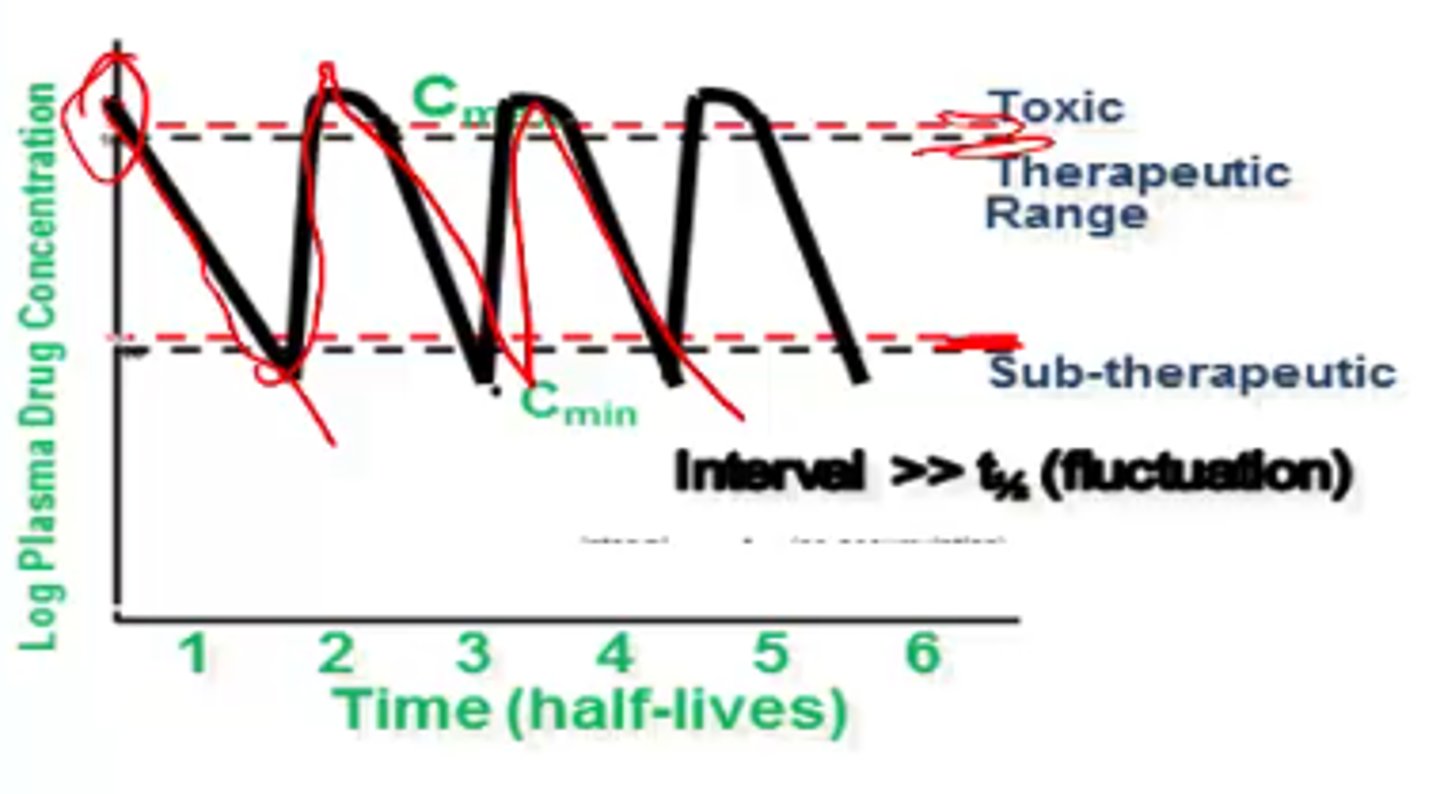
If a drug is administered to concentration A, falls to concentration B, and is re-administered to concentration A, this is called ...
Fluctuation (dosed after half-life)
If a drug is administered to concentration A, falls to concentration B, and is re-administered to a higher concentration C, this is called ...
Accumulation (dosed before half-life)
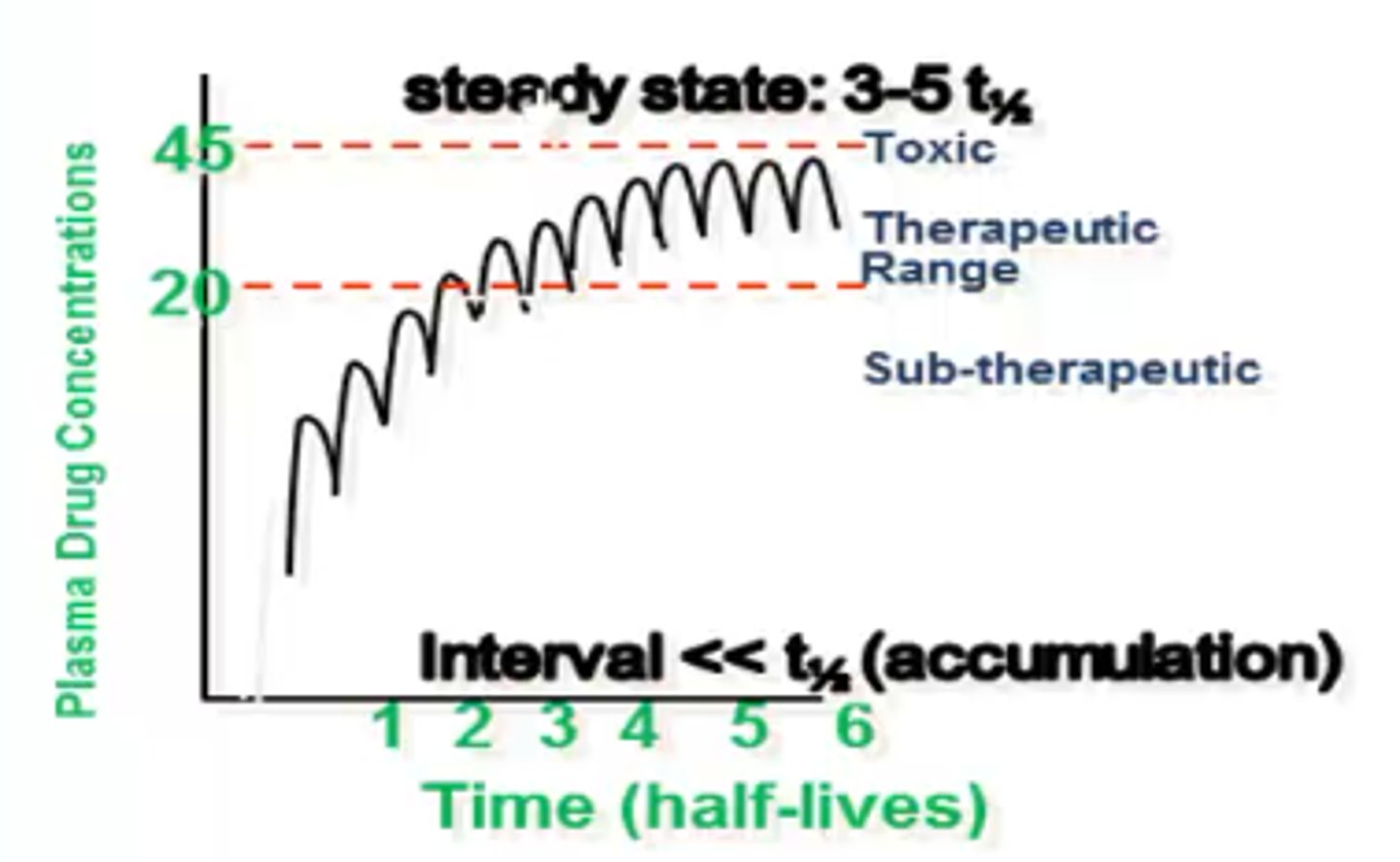
When the amount of drug eliminated is equivalent to the amount taken in, this is called ...
Steady-state
The volume of tissue that dilutes the drug or the volume to which a drug appears to distribute is the ...
Volume of distribution
The volume required to contain all drug in the body if it were at an equal concentration to plasma
Volume of distribution is calculated as:
Vd = Dose/(Target Conc.)
Increasing the volume of distribution will have what affect on plasma concentration and half-life?
lower plasma concentration
Increase half-life
The volume of plasma irreversibly emptied of the drug
Body clearance
The calculation for body clearance is:
CL = Vd * K_el
Units = mL/(minutes * kg)
In drugs with similar _________, the smaller the volume of distribution the shorter the half-life
body clearance values
Two drugs, A and B, have the same clearance rate of 4
Drug A has a half-life of 100 minutes
Drug B has a half-life of 1000 minutes
Calculate their volume of distribution
Vd = Cl/K_el
K_el = 0.693/T(1/2)
Drug A
Vd = 4/(0.693/100) = 577.2
Drug B
Vd = 4/(0.693/1000) = 5772.0
Forumulas
Yay