Renal Physio Combined 1-2
1/183
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
184 Terms
What end products of metabolism is excreted (3)
Uric acid
Urea
Creatinine
What are the hormones and vitamins produced from the renal system
Renin
Erythropoietin
Calcitriol
Vitamin D
What is the functional unit of kidney?
Nephron
Renal Pyramids can be found in the renal?
Medulla
The base of renal pyramids originate from the?
Corticomedullary border
The apex of renal pyramids terminante at?
Papilla
All minor Calyces converge into?
Major Calyces
Renal artery → __artery → _ artery → ___ artery
Renal → Interlobar → Arcuate → Interlobular → Afferent arteriole →Glomerular capillaries (filtration)→ Efferent arteriole → Peritubular capilaries→ Venules → Interlobular→ Arcuate vein → Interlobar vein → renal vein → IVC
The kidney’s are composed of how many nephrons?
1.2 Million nephrons
Parts of the nephron?
Renal Corpuscle
Proximal Tubule / Proximal convoluted tubule
Loop of Henle
Distal tubule / Distal convoluted
Collecting duct
WHich part of the loop of henle is part of the MAcula Densa?
Macula Densa → where nephron passes between the afferent and efferent arterioles of the same nephron
Ascending Thick Limb
Which part of the Nephron is involved in Ultrafiltration?
Glomerulus
The glomerular filtration barrier is composed of?
Capillary Endothelium
Basement membrane
Foot processes of Podocytes
What is the function of the Mesangium of the Glomerulus?
Mesangium →
Provide structural support for glomerular capillaries
Secrete Matrix
Exhibit Phagocytic activity
Secrete Prostaglandins & Pro-inflammatory cytokines
What do you call mesangial cells found outside the glomerulus?
Extraglomerular Mesangial Cells
The (?) is a specialized set of cells from the Thick ascending limb of loop of Henle that signals extraglomerular mesangial cells and granular cells.
Macula Densa
Which cells produce Renin and Angiotensin 2?
Granular cells
Which segment of the renal tubule is characterized by a prominent brush border and a high density of mitochondria to support active reabsorption?
A.
Proximal tubule
B.
Thin Limbs of LOH
C.
Distal tubule
D.
Medullary Collecting Duct
Proximal tubule
Which specific cell type in the collecting duct is known for having a high density of mitochondria and relying on Na-K ATPase?
A.
Inner medullary collecting duct cells
B.
Intercalated cells
C.
Descending thin limb cells
D.
Principal cells
Intercalated cells
Almost all cells in the nephron are lined by a single non-motile cilium. Which of the following is the only exception mentioned in the text?
A.
Principal cells
B.
Intercalated cells
C.
Thin limb cells
D.
Proximal tubule cells
Intercalated cells
All cells except the intercalated cells are lined by this single non-motile cilium.
acts as mechanosensor & chemosensor = autoregulation in kidney
In the medullary collecting duct, reabsorption is mainly focused on which two substances?
A.
Potassium and Bicarbonate
B.
Protein and Amino acids
C.
Glucose and Sodium
D.
Water and Urea
Water and Urea
How do the cells of the Thin Limbs of the Loop of Henle (LOH) differ from the Thick Ascending Limbs?
A.
Thin limbs have a more developed brush border.
B.
Thin limbs have more mitochondria.
C.
Thick limbs are only involved in water reabsorption.
D.
Thin limbs do not rely on ATP for their primary functions.
Thin limbs do not rely on ATP for their primary functions.
Thin limbs have poorly developed surfaces and few mitochondria, indicating they do not rely on active, ATP-driven transport.
Which segment relies on a 'constant supply of ATP' to fuel the Na-K ATPase pump for its primary function?
A.
Principal cells
B.
Proximal tubule
C.
Descending thin limb
D.
Medullary collecting duct
Proximal tubule
Based on the provided table, which of the following segments is involved in 'solute reabsorption' and uses 'many invaginations'?
A.
Inner Medulla Collecting Duct
B.
Thick Ascending Limbs and Distal Tubule
C.
Cortical Collecting Duct (Principal cells)
D.
Thin Limbs of LOH
Thick Ascending Limbs and Distal Tubule
Which of the following is true regarding the surface development of the Cortical Collecting Duct cells?
A.
They have poorly developed surfaces and few mitochondria (specifically in Principal cells).
B.
They have highly developed surfaces with many invaginations.
C.
They have a brush border similar to the proximal tubule.
D.
All cells in this segment have a high density of mitochondria.
They have poorly developed surfaces and few mitochondria (specifically in Principal cells).
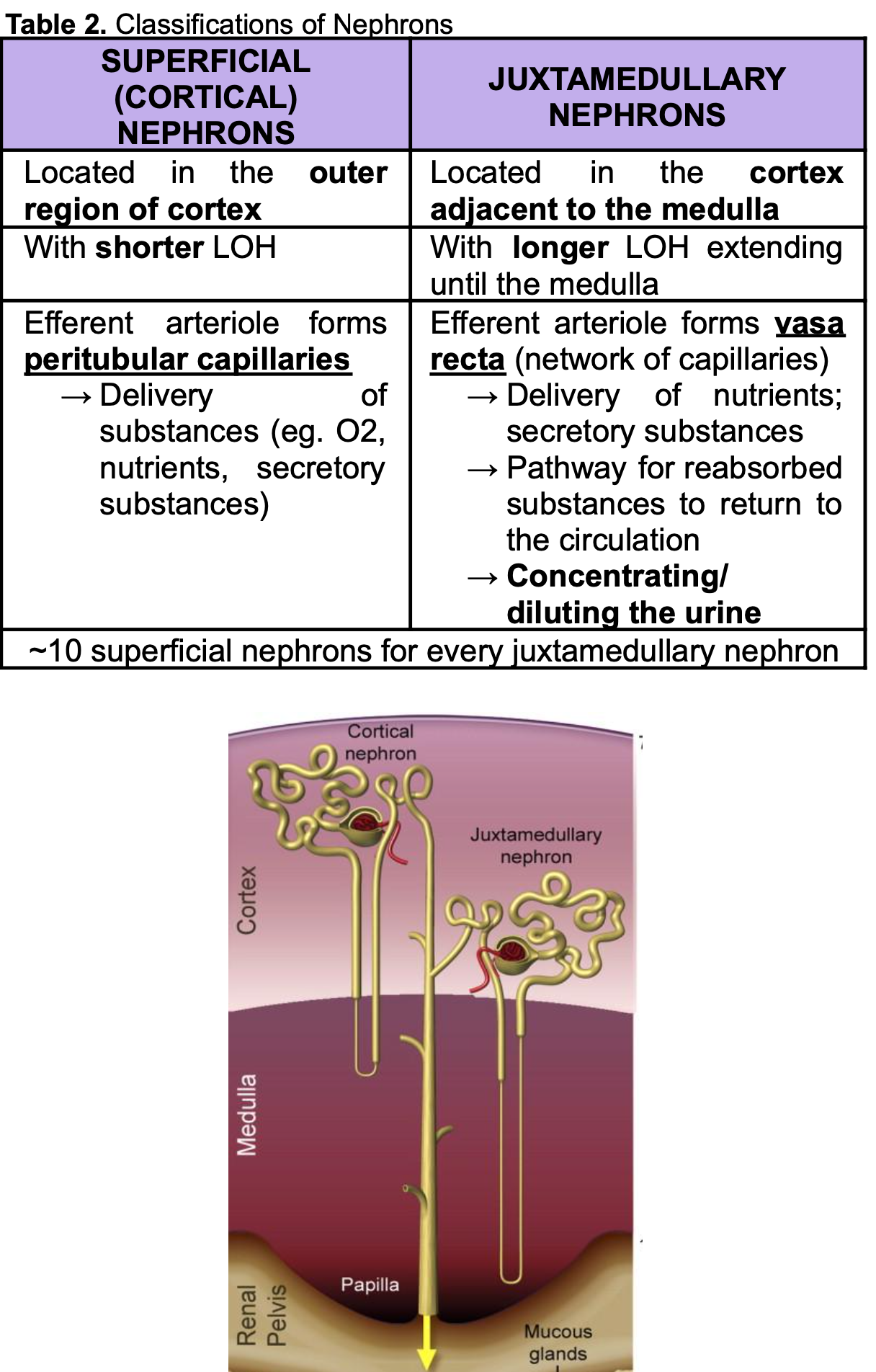
Which one is responsible for Concentrating or Diluting urine?
Cortical Nephrons
Juxtamedullary Nephrons
What
activates Granular Cells to produce renin
Enhances Na+ reabsorption in the PT, LOH, DT, CD?
Sympathetic Nervous system - Celiac Plexus
A patient’s kidney is failing to concentrate urine effectively. Which type of nephron is primarily responsible for establishing the medullary concentration gradient?
A) Superficial Nephrons
B) Juxtamedullary Nephrons
C) Cortical Collecting Duct cells
D) Proximal Tubule cells
Answer: B
Juxtamedullary nephrons have a major role in creating a concentration gradient in the medulla to enable water reabsorption.
Unlike Superficial nephrons, which stay mainly in the cortex, Juxtamedullary nephrons have long loops that extend deep into the medulla.
Which vessel type is specifically associated with the efferent arterioles of Juxtamedullary nephrons?
A) Peritubular capillaries
B) Glomerular capillaries
C) Vasa recta
D) Renal vein
Answer: C
The efferent arterioles of Juxtamedullary nephrons form the vasa recta.
Superficial nephrons form peritubular capillaries instead.
Which segment of the renal tubule features a "brush border" to maximize surface area for reabsorption?
A) Thick Ascending Limb
B) Distal Tubule
C) Proximal Tubule
D) Medullary Collecting Duct
Answer: C
The Proximal tubule has a brush border to increase surface area for reabsorption.
It also contains many mitochondria to provide ATP for the Na-K ATPase pump
You are examining a Cortical Collecting Duct. Which specific cell type contains a high density of mitochondria and relies on Na-K ATPase?
A) Principal cells
B) Intercalated cells
C) Macula densa cells
D) Podocytes
B) Intercalated cells
As the Medullary Collecting Duct descends towards the inner medulla, what two substances are primarily reabsorbed?
A) Sodium and Glucose
B) Water and Urea
C) Potassium and Proteins
D) Bicarbonate and Hydrogen
B) Water and Urea
The efferent arteriole of Cortical nephrons form?
Peritubular capillaries
The efferent arteriole of Juxtamedullary nephrons form?
Vasa recta
The glomerulus is
supplied by _ artery
drained by _ artery
supplied by afferent artery
drained by efferent artery
T or F? The Capillary Endothelium is freely permeable to
RBCs, WBCs, Platelets
Albumin
Plasma porteins
False!
Only Water, Small solutes (Ions, Urea or Glucose) and small proteins are freely permeable.
What are 2 regulators of Vessel resistance?
Nitric Oxide
Endothelin 1
Which one is a vasodilator and which one is a vasoconstritor?
Nitric Oxide
Endothelin-1
Which one is a vasodilator and which one is a vasoconstritor?
Nitric Oxide - vasodilator ***
Endothelin-1 - vasoconstrictor
(?) are finger-like processes that unterdigitate, covering the basement membrane?
Podocytes
What is renal clearance?
The Removal rate of a substance in Plasma
What is the normal Filration Fraction (FF)?
15-20%
What can you check to tell the progression of Kidney disease?
GFR
Creatinine
T or F? GFR decreases with age due to the deterioration of nephrons.
True
T or F? Ultrafiltrate is completely devoid of cells (WBC and RBC) and proteins
True
T or F? Ultrafiltrate gas lesser Salts and Organic molecules than Plasma.
False. It should be ISOSMOTIC. Similar composition as that in Plasma.
The more positively charged an ion is the (higher/lower) the filterability.
More positive charge = Higher Filterability
In the Starling equation for GFR, which force is considered the 'principal force favoring filtration'?
A.
Hydrostatic pressure of the Bowman's space (PBS)
B.
Hydrostatic pressure of the glomerular capillaries (PGC)
C.
Oncotic pressure of the Bowman's space (πBS)
D.
Oncotic pressure of the glomerular capillaries (πGC)
Hydrostatic pressure of the glomerular capillaries (PGC)
This positive pressure pushes fluid out of the capillary into the Bowman's space, driving filtration.
Which of the following describes the biphasic effect of severe efferent arteriolar constriction on GFR?
A.
GFR decreases because the rise in colloid osmotic pressure outweighs the rise in hydrostatic pressure.
B.
GFR decreases because renal blood flow increases too much.
C.
GFR increases infinitely as the 'outlet' is narrowed.
D.
GFR remains constant due to the Donnan effect.
GFR decreases because the rise in colloid osmotic pressure outweighs the rise in hydrostatic pressure.
While moderate constriction raises hydrostatic pressure, severe constriction causes a nonlinear increase in oncotic pressure that eventually lowers GFR.
If the ultrafiltration coefficient (Kf) increases, what is the expected effect on GFR?
A.
GFR will decrease.
B.
GFR will become negative.
C.
GFR will remain unchanged.
D.
GFR will increase.
GFR will increase.
GFR is directly proportional to $K_f$, which represents the surface area and permeability of the glomerular membrane.
What happens to Glomerular Hydrostatic Pressure (PGC) and GFR when there is an increase in afferent arteriolar resistance (RA)?
A.
Both PGC and GFR decrease.
B.
Inner medullary pressure increases while GFR decreases.
C.
GFR increases due to the Donnan effect.
D.
Both PGC and GFR increase.
Both PGC and GFR decrease.
Constricting the 'inlet' reduces blood flow into the glomerulus, lowering the pressure and the filtration rate.
Why is the oncotic pressure of the Bowman's space (πBS) designated as zero in the Starling force calculation?
A.
The glomerular ultrafiltrate is essentially protein-free.
B.
The hydrostatic pressure is too high.
C.
The Bowman's space is actually empty.
D.
Water is reabsorbed too quickly.
The glomerular ultrafiltrate is essentially protein-free.
Oncotic pressure is generated by proteins; since proteins aren't filtered under normal conditions, there is no osmotic pull in the space.
A patient is administered a drug that causes significant constriction of the afferent arteriole. What is the most likely combined effect on the hydrostatic pressure of the glomerular capillaries (PGC) and the Renal Blood Flow (RBF)?
A.
PGC will increase while RBF decreases.
B.
PGC will decrease while RBF increases.
C.
Both PGC and RBF will decrease.
D.
Both PGC and RBF will increase.
Both PGC and RBF will decrease.
Which of the following scenarios would lead to an increase in the net filtration pressure, assuming all other variables remain constant?
A.
A decrease in the plasma protein concentration within the glomerular capillaries.
B.
A decrease in the glomerular capillary hydrostatic pressure (PGC).
C.
An increase in the systemic oncotic pressure.
D.
An obstruction in the ureter causing fluid to back up into the Bowman's space.
A decrease in the plasma protein concentration within the glomerular capillaries.
Lowering plasma proteins reduces the oncotic pressure (πGC) that opposes filtration, thus increasing the net pressure pushing fluid out.
The Donnan effect is cited in your notes as a reason for the biphasic effect of efferent constriction. How does this effect specifically contribute to a decrease in GFR during severe constriction?
A.
It causes a rapid, nonlinear increase in colloid osmotic pressure due to the interaction of ions bound to plasma proteins.
B.
It decreases the permeability of the glomerular basement membrane.
C.
It reduces the hydrostatic pressure by shunting blood to superficial nephrons.
Level of Constriction | Effect on PGC | Effect on πGC | Final Effect on GFR |
Moderate | Significant Increase | Slight Increase | Increase |
Severe | Slight Increase | Massive Increase | Decrease |
It causes a rapid, nonlinear increase in colloid osmotic pressure due to the interaction of ions bound to plasma proteins.
f a disease state increases the thickness of the glomerular basement membrane, which component of the GFR equation is primarily affected, and what is the resulting change in GFR?
A.
PGC increases, leading to an increase in GFR.
B.
Kf increases, leading to an increase in GFR.
C.
Kf decreases, leading to a decrease in GFR.
D.
πGC decreases, leading to an increase in GFR.
Kf decreases, leading to a decrease in GFR.
A patient has a condition that significantly lowers their blood pressure. How would the kidney's GFR respond transiently, according to the 'Regulation of GFR' notes?
A.
The PGC and GFR will both transiently decrease.
B.
The PGC will decrease but GFR will increase due to autoregulation.
C.
The oncotic pressure will increase to compensate for the lost hydrostatic pressure.
D.
The Kf will increase to allow more fluid through the membrane.
The PGC and GFR will both transiently decrease.
The kidney maintains a relatively constant Renal Blood Flow (RBF) and GFR despite fluctuations in systemic blood pressure. What is the specific range of mean arterial pressure (mmHg) where this autoregulation is effective?
A.
60 to 120 mmHg
B.
90 to 180 mmHg
C.
100 to 200 mmHg
D.
120 to 150 mmHg
90 to 180 mmHg
If a patient's mean arterial blood pressure drops to 75 mmHg, what is the expected status of the renal autoregulatory mechanisms?
A.
Autoregulation will increase vascular resistance to compensate.
B.
Vascular resistance will stay constant to maintain RBF.
C.
Autoregulation becomes more efficient to protect the GFR.
D.
Autoregulation stops.
Autoregulation stops.
autoregulation ceases when the blood pressure drops below 90 mmHg.
Hydrostatic Pressures:
→PGC = hydrostatic pressure of the glomerular capillaries
▪ Designated as a positive pressure
▪ Principal force favoring filtration
→ PBS = hydrostatic pressure of the Bowman’s space
▪ Designated as a negative pressure because it decreases filtration
● Oncotic Pressures:
→ πGC = oncotic pressure of the glomerular capillaries
▪ Designated as a negative pressure because it decreases filtration
▪ ↑ protein concentration in the plasma = ↑ oncotic pressure = ↓ GFR = reabsorption [ 2025 Trans]
→ πBS = oncotic pressure of the Bowman’s space
▪ Designated as zero because glomerular ultrafiltrate is essentially protein free under normal conditions
patient experiences a significant decrease in efferent arteriolar resistance (RE). How does this change influence the GFR?
A.
GFR remains constant as long as the afferent resistance is unchanged.
B.
GFR increases due to a drop in oncotic pressure.
C.
GFR decreases because fluid leaves the glomerulus too quickly, lowering PGC.
D.
GFR increases because blood flow through the kidney is faster.
GFR decreases because fluid leaves the glomerulus too quickly, lowering PGC.
Decreasing the 'exit' resistance allows blood to flow out of the glomerulus with less back-pressure, reducing the pressure that drives filtration.
Which of the following resistance changes would be most effective at increasing the GFR in a healthy kidney?
A.
Increased afferent resistance and decreased efferent resistance.
B.
Decreased afferent resistance and increased efferent resistance.
C.
Decreased resistance in both the afferent and efferent arterioles.
D.
Increased resistance in both the afferent and efferent arterioles.
Decreased afferent resistance and increased efferent resistance.
an increase in efferent resistance (RE) leads to an increase in PGC. Why does this occur?
A.
It reduces the amount of protein in the blood, lowering opposition.
B.
It stimulates the heart to pump blood into the kidney with more force.
C.
It creates a 'back-pressure' effect within the glomerular capillaries.
D.
It increases the permeability of the filtration membrane (Kf).
It creates a 'back-pressure' effect within the glomerular capillaries.
what detects changes in your sodium levels in the tubular fluid?
Macula densa
An increase in filtered NaCl will trigger the Macula Densa in the Thick ascending limb of LOH , what will happen?
Increases synthesis of ATP and Adenosine
Vasoconstriction of Afferent Arteriole
Decrease in GFR = normalization of GFR
Adenosine, ATP and Angiotensin are known as Vasodilators or Vasoconstrictors?
Vasoconstrictors
What are vasodilators?
Nitric Oxide
**What are substances that can cause vasoconstriction of afferent arteriole?
Norepi and Epinephrine
High angiotensin 2
Endothelin
Adenosine
ATP
What are substances that can cause constriction of efferent arterioles?
Low Angiotensin 2
Endothelin
Natriuretic peptide
**What is the effect of Natriuretic Peptide on
Efferent arteriole
Afferent arteriole
(Dilate/constrict)
What is the effect of Natriuretic Peptide on
Efferent arteriole → Constrict
Afferent arteriole → Dilate
What are vasodilators of the afferent arteriole?
Nitric oxide
Bradykinin
Histamine
Natriuretic peptides**
Glucocorticoids
Dopamine
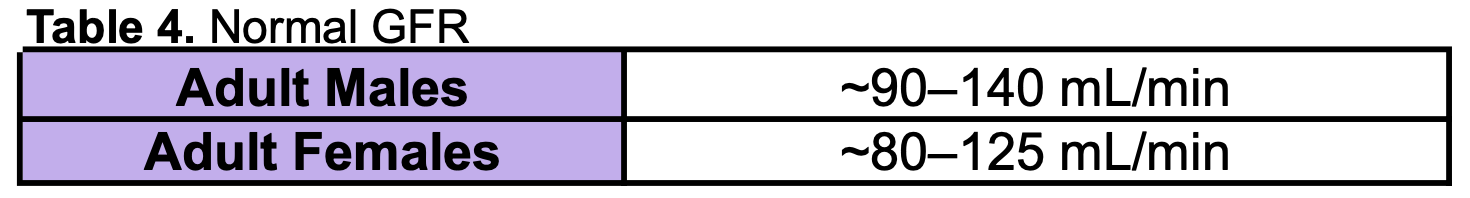
What is the average glomerular filtration rate for adults?
180-200L per day
T or F? Less than 1% of filtered NaCL and water will be excreted in the urine due to the process of reabsorption
True
Beyond the Transport Maximum, can glucose be re-absorbed?
No
What is the Threshold to which glucose will start to be excreted in urine despite not reaching Transport maximum?
What is this phenomenon called?
Threshold: 200mg/dL
Maximum: 400 mg/dL
SPLAY phenomenon
Water can be reabsorbed by which 2 ways?
Transcellular pathway via Aquaporin 1
Paracellular pathway
What is the condition caused by increased proteins in filtrate (appearance of protein in urine)?
PROTEINURIA
Which area is exclusively permeable to water?
Thin DL
Thin AL
Thick AL
Thin DL → exclusively permeable to water
Which area is IMpermeable to water and is where NaCl is reabsorbed in the bloodstream?
Thin DL
Thin AL
Thick AL
Thin AL
Thick AL
Which area is causes the osmolality of tubular fluid to become HYPERosmotic?
Thin DL
Thin AL
Thick AL
Thin Descending Limb
water is reabsorbed here and only solute remains
Which area is NaCl absorbed Passively?
Thin DL
Thin AL
Thick AL
Thin Ascending Limb
On the basolateral side of the Thick Ascending Limb cell, which mechanism is primarily responsible for maintaining the low intracellular sodium concentration that powers other transporters?
A.
NKCC2 symporter
B.
Na+/K+-ATPase Pump
C.
ROMK channel
D.
Na+/H+ exchanger (NHE3)
Na+/K+-ATPase Pump
The NKCC2 symporter on the apical membrane facilitates the transport of which ions into the cell together?
A.
1 K+ and 1 Cl-
B.
1 Na+, 1 K+, and 2 Cl-
C.
2 Na+, 1 K+, and 1 Cl-
D.
1 Na+ and 1 H+
1 Na+, 1 K+, and 2 Cl-
What is the primary role of the ROMK (Renal Outer Medullary Potassium) channel in the apical membrane of the TAL?
A.
Recycling potassium back into the tubule lumen to keep NKCC2 functioning.
B.
Exchanging potassium for hydrogen ions to regulate pH.
C.
Generating ATP for the basolateral pumps.
D.
Final reabsorption of potassium into the blood.
Recycling potassium back into the tubule lumen to keep NKCC2 functioning.
The movement of chloride in the Thick Ascending Limb helps create a 'positive transepithelial voltage.' What is the functional consequence of this positive charge in the tubule lumen?
A.
It inhibits the function of the NKCC2 symporter.
B.
It causes water to move into the tubule lumen.
C.
It drives the paracellular diffusion of cations like Ca++ and Mg++.
D.
It prevents the reabsorption of sodium.
It drives the paracellular diffusion of cations like Ca++ and Mg++.
A patient has a mutation in the tight junction protein claudin-16. Based on the provided notes, which of the following is the most likely result?
A.
Failure of the Na+/K+-ATPase pump.
B.
Increased reabsorption of water in the loop.
C.
Reduced reabsorption of Mg++ and Ca++.
D.
Inhibition of the ROMK channel.
inactivated Claudin-16 = Reduced reabsorption of Mg++ and Ca++.
T or F? The Reabsorption of NaCl deacreases as you move futher down the Nephron.
True. Most reabsorption occurs in the PCT and least at the Collecting duct
Where does Antiduretic hormone (ADH) exert its effect in the nephron?
Collecting ducts
Difference in reabsoprtion in the Early distal tubule vs Late distal tubule & Collecting duct?
early distal tubule → Nacl and Ca2+ reabsorption
later distal tubule + collecting duct → NaCl and H20 reabsorption
T or F? The early distal tubule is IMPERMEABLE to water.
True
The "diluting segment" of the kidney includes the Thick Ascending Limb (TAL) and the Early Distal Tubule. What physical property do these two segments share that allows them to dilute the tubular fluid?
A) They are highly permeable to water under the influence of ADH.
B) They are completely impermeable to water.
C) They use active transport to pump water into the blood.
D) They have a brush border for massive water reabsorption.
B) They are completely impermeable to water.
Both the TAL and the Early Distal Tubule are impermeable to water.
Because they reabsorb solutes (NaCl) but leave the water behind, the remaining tubular fluid becomes diluted.
Which apical transporter is specific to the Early Distal Tubule and facilitates the passive movement of Sodium and Chloride into the cell?
A) NKCC2
B) NHE3
C) NCC
D) ROMK
Answer: C
The NCC (Na+/Cl− symporter) is the primary apical transporter in the Early Distal Tubule.
It facilitates the movement of Na+ along with Cl−, and occasionally K+.
In the Late Distal Tubule and Collecting Duct, the cells are specialized for "fine-tuning." Which cell type is specifically responsible for H+ and HCO3− secretion based on acid-base status?
A) Principal cells
B) α and β-intercalated cells
C) Podocytes
D) Macula densa cells
Answer: B
Intercalated cells (α and β) are responsible for H+ and HCO3− secretion.
Principal cells are instead focused on Na+ reabsorption and K+ secretion.
Why is the ROMK channel considered "vital" for the proper functioning of the NKCC2 symporter in the TAL?
A) It provides the ATP needed for the symporter.
B) It recycles K+ back into the lumen because the available K+ in tubular fluid is low.
C) It creates the hydrostatic pressure needed for filtration.
D) It allows water to follow K+ into the cell.
B) It recycles K+ back into the lumen because the available K+ in tubular fluid is low.
What causes the "positive transepithelial voltage" in the TAL, and what is the functional result of this voltage?
A) Na+ movement; drives water reabsorption.
B) K+ movement; drives glucose reabsorption.
C) Cl− movement; drives paracellular diffusion of cations (Na+,K+,Ca++,Mg++).
D) ATP consumption; drives urea reabsorption.
C) Cl− movement; drives paracellular diffusion of cations (Na+,K+,Ca++,Mg++).
This cell is primarily responsible for sodium reabsorption and potassium secretion
Principal Cell
Which hormone is the primary regulator for increasing the number of Epithelial Sodium Channels (ENaC) on the apical surface of Principal cells?
A.
Atrial Natriuretic Peptide (ANP)
B.
Antidiuretic Hormone (ADH)
C.
Aldosterone
D.
Parathyroid Hormone (PTH)
Aldosterone
Which cell type is most active during a state of systemic acidosis to help lower blood acidity?
A.
Beta (β)-Intercalated cell
B.
Glomerular Mesangial cell
C.
Principal cell
D.
Alpha (α)-Intercalated cell
Alpha (α)-Intercalated cell
These cells are specialized to secrete hydrogen ions into the urine and reabsorb bicarbonate back into the blood.
Which cell type is most active during a state of systemic alkalosis to help lower blood acidity?
A.
Beta (β)-Intercalated cell
B.
Glomerular Mesangial cell
C.
Principal cell
D.
Alpha (α)-Intercalated cell
Beta (β)-Intercalated cell
Secrete HCO3- in bicarbonate
Remember B = Bicarbonate
What is used as an indirect measure of GFR?
Creatinine