The form sense I : visual acuity
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
define the term visual acuity and what are the usual units of VA
the smallest visible detail that can be seen / the finest spatial detail that can be detected, discriminated,resolved or recognised
Usually specified in angular terms (e.g. minutes of arc)
name the 4 types of visual acuity - all can be used clinically
Detection
Resolution
Relative spatial localisation
Recognition
describe detection
Ability to detect an object
Detection acuity: angular size of the smallest visible target
Perception of presence or absence of an aspect of the stimulus/target
explain how detection would typically be measured experimentally
•The detection of a feature or object in the visual field.
•This could be a small dot or thin line presented to a patient.
•A typical target used in experimentation is the ability to detect a thin line against a white background (see figure).
•An observer is asked to identify in which of the 2 cards the line is present
explain the approximate thresholds attained by humans for detection - minimal visible acuity (detection) (4)
When a thin line appears on a plain background its image creates a line spread function on the retina (creates a blurry version of it)
As the line gets larger (e.g., closer to the eye), its image gets brighter or darker, the height of the line spread function increase, thus increasing the contrast
detection threshold: The line is detected when the change in brightness (ΔI)/luminance becomes just enough to cross the contrast threshold - the change in luminance is detected by the eye
a brightness/darkness discrimination or contrast sensitivity task
if you are far away and and cannot tell which card has the line, what % correct are you likely to achieve
50%
if the detection task has a guess rate of 50% at what performance level would the experimenter take as detection threshold
75%
remember the guess rate is 50% so can either be 50% or 100% as they can either detect it or not
so in between 50% and 100% cannot be lower than 50%
in between 50 and 100 = 75%
how can we generate a psychometric function by testing for detection acuity
At close distances, the observer would correctly identify the line on 100% of the presentations
As the distance from the observer increases, percentage of correct responses decrease as it becomes harder for the observer to see the line
At some distance, the line becomes so hard to see that the observer’s responses fall to a chance level at 50% correct (2AFC)
We can plot the results on a graph = psychometric function
explain the psychometric function - graph - how the detection threshold VA can be measured using this
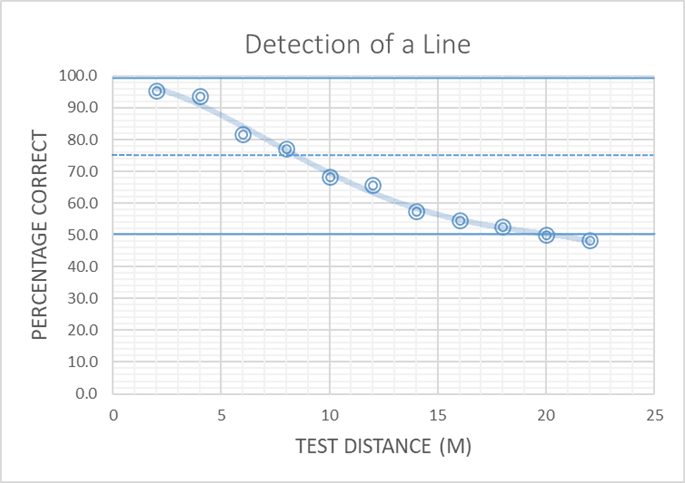
We can connect the data by an S-shaped curve called a ‘psychometric function’, describes human behaviour on this task.
Threshold distance is taken at a specified point on the function
Threshold size is calculated from the known target size and the threshold distance. Calculate the angle
what clinical tests may we use to test detection acuity - not common - why might we use them
dot visual acuity test
Cartford drum test
In this test, the patient has to detect the small black dot visible in the aperture.
The dot size is varied until the observer cannot detect the dot - watch patients eyes
good for children
If the detection threshold distance of a KNOWN target size (m) is 7.5m how would you find threshold angular size
use arctan (tan -1 (inverse of tan)) function to find the angular size as tan angle = size / distance
so you would do tan-1 ( target size / 7.5) = …
to convert from degrees to arcmin multiply degrees by 60 as 1 degree = 60 arcmin = answer
•If size of dot seen at threshold performance is 1mm, seen at 50cm, what is the detection threshold?
first convert 50 cm to mm = 500mm
tan -1 ( 1 / 500) = 0.11459 (degrees)
0.11459 × 60 = 6.88’ armcin
Describe physiological limits underlying visual acuity - DETECTION (4)
When objects are very small, the size of the image they create on the retina is limited by the eye’s optics - line spread function of the eye
The spread function can be effected by a number of factors: including diffraction, aberrations, light scatter, absorption and focus factors
Also limited by contrast sensitivity response properties of underlying neurons
outer segment length of the photoreceptors - longer can catch more photons
describe spatial resolution
Ability to resolve the details of an object
Smallest angular size at which observers can discriminate the separation between two points or lines (MAR: minimum angle of resolution)
what does the ability of spatial resolution depend on (3)
1.The optics of the eye and the quality of the retinal image.
2.The structure and function of the retina.
3.The capacity of the neural pathways
what is the approximate thresholds attained by humans for spatial resolution
the smallest gap or separation that could be detected
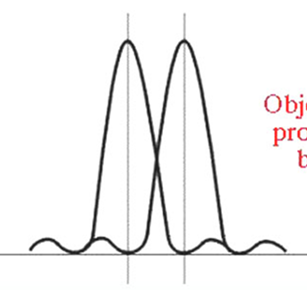
explain the threshold for resolution in detail (4)
Consider two adjacent lines closely spaced
Their images form two line spread functions on the retina. If the lines are very close together the line spread functions will overlap almost completely
As the lines are separated, the overlap in their respective line spread functions is less. This creates a pattern of light, two peaks with a ‘trough’
Resolution is possible when the visual system can distinguish presence of the trough
explain what the Raleigh’s criterion is - when this type of resolution is achieved (2)
2 lines will be resolved if the separation between their line spread functions is sufficiently wide (at least the width of the PSF i.e. the radius of the respective Airy disc)
Equates to about 1 cone separation at the fovea
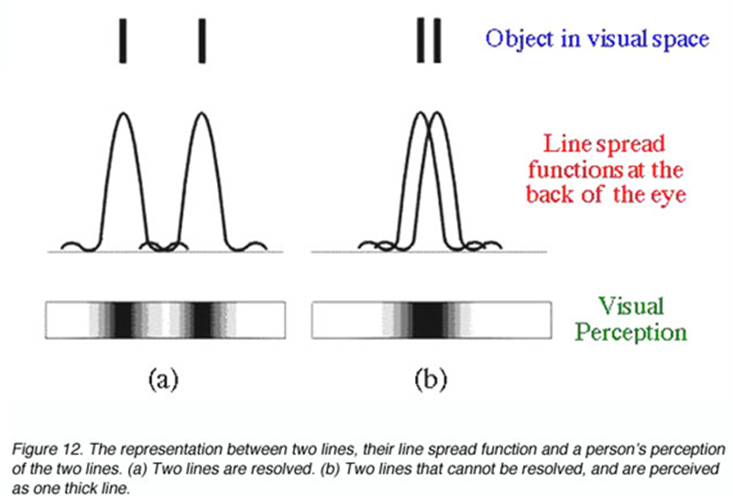
what is the physiological limit for resolution
spacing (sampling rate) of relevant receiving CONES
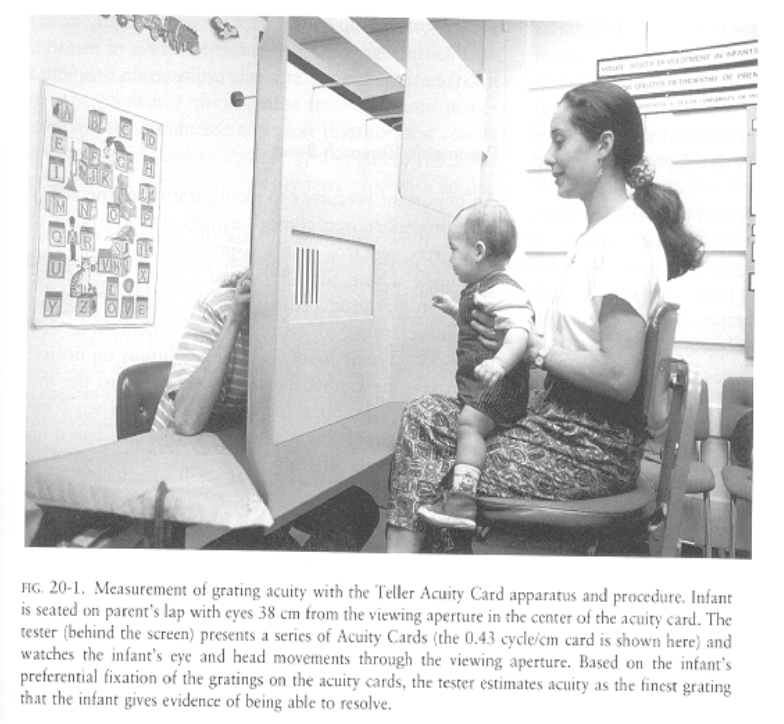
explain when and how gratings are used to clinically measure resolution acuity
used for infants/non-literate/lens opacities
which detector array [A-F] will be able to resolve 2 lines from 1
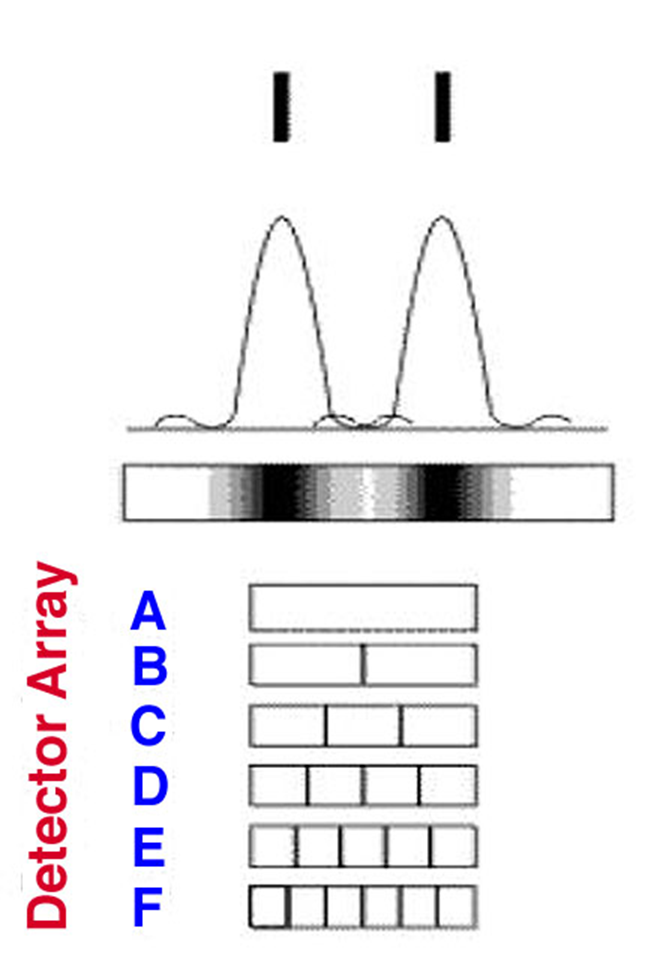
Only detector arrays C-F will be able to resolve 2 lines.
an observer can resolve that there are two lines rather than one when a centrally located photoreceptor is illuminated sufficiently less than it neighbours
the resolution limit at the fovea is defined by the separation of the cone photoreceptors
Resolution of two lines (or the stroke in the tumbling E) will occur if the images of the lines fall on 2 independent cones separated by a single cone.
•This corresponds to a separation of approximately 0.5 arc mins
spatial pooling of information from photoreceptors onto ganglion cells is good and bad for what and its location (3)
frequently occurs at peripheral vision - remember not central vision as at the fovea each cone has a ganglion cell
bad for resolving fine detail in objects
good as it improves the ability of the eye to catch photons and detect a stimulus
what is the rod peak in density
•Rods peak in density ~18° or 5 mm out from the center of the fovea, in a ring around the fovea at 160,000 rods/mm2
a 6/6 letter is approximately equivalent to what deg grating
30 c / deg grating
a 6/60 letter is approximately equivalent to what deg rating
3 c / deg grating
describe Relative spatial localisation
Ability to localise relative features of an object
Judgements of the position of one part of an object relative to another
explain how this may be tested experimentally
•An example would be a task where the observer identifies which one of 2 cards (shown) has the line with a small displacement or offset.
•Under optimal conditions, thresholds of a few seconds of arc of visual angle have been measured.
•We could use the method previously described to determine a threshold visual acuity for this task.
describe practical applications of localisation acuity
•the use in the calipers and in navigational tools.
•Very fine measurements are possible due to the ability of the visual system localise to such fine levels.

explain what is meant by - Relative Spatial Localisation is a Hyperacuity (4)
•Hyperacuity refers to the ability to judge relative spatial position with a precision that is far finer than the minimal effective receptor size
•e.g. diameter of human foveal cone about 30 arcsec; optimal vernier threshold about 3-5 arcsec
so the position of the 2 lines could be within a single cone
so it is believed that the retina cannot discriminate the difference itself. This discrimination is achieved at the cortical level
explain the effect of increasing eccentricity / peripheral vision has on acuity - resolution acuity AND relative position acuity
•Resolution acuity is degraded with increases in retinal eccentricity (in peripheral vision)
•Relative position acuity is particularly sensitive to increases in peripheral viewing and in amblyopia
•As eccentricity increases, resolution acuity deteriorates more rapidly than relative position acuity, which may still function but with reduced precision due to contrast and light sensitivity changes.
what is the Effect of Eccentricity on Thresholds E2 - Define E2 and explain the 2 groups it falls into for spatial vision
E2 is defined as the eccentricity at which the foveal threshold has doubled.
E2 generally falls into two groups for spatial vision:
–1.5-4.0 deg (about 2.5 deg): cone/P ganglion cell spacing/sampling at retina
–0.3-0.9 deg (about 0.8 deg): cortical magnification – one degree on the retina is magnified at the cortex - if you move the target away less cortex looking at this 1 degree – CM is why we are able to extract the 3-5 arc seconds
the ability of the eye to judge relative position in central vision is known as a hyperacuity because….
thresholds are much better than the size of a single cones
thresholds are much better than expected based on cone spacing at the fovea
explain a clinical test that may be used to test localisation acuity - binocularly
•Clinical tests using localisation ability include tests of binocular vision and eye alignment.
•One example as shown in the image, is a test of fixation disparity.
•The patient has to say whether the line above and below the ‘X’ appear to be aligned.
•For this test, the patient would wear special glasses so each eye would only see one of the lines (either the top or bottom)

describe recognition (4)
Ability to recognise an object
•Requires the observer to recognize or name a target, i.e., most visual acuity tasks
•Thought to require abilities of detection, resolution, relative spatial localization as well as naming the target
Also known as “identification” acuity
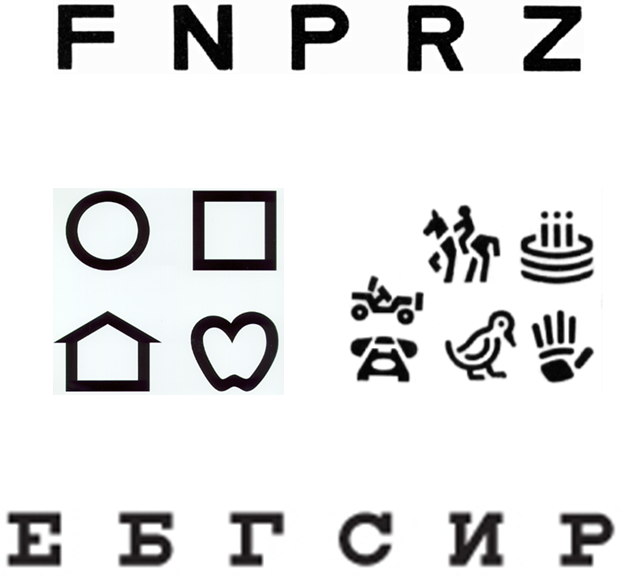
how is recognition tested clinically and what are the units
•Most clinical tests are based on recognition acuity.
•They require the correct recognition of letters, symbols, or numbers (known as optotypes).
•Similar to resolution acuity, the stroke width (or thickness of the line) of the smallest optotype that can be seen is used to specify the minimum angle of resolution (MAR) in min or arc.
summary of comparison of spatial acuity thresholds
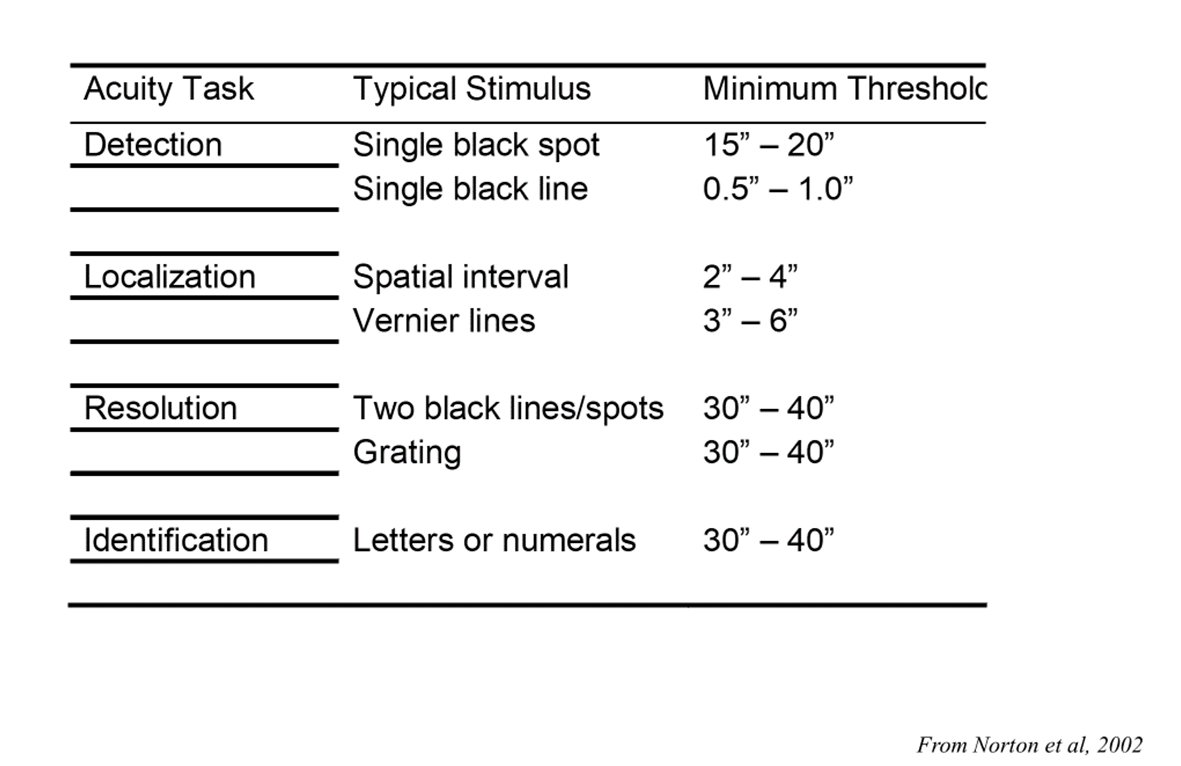
memorise the minimum threshold numbers !!!