Critical Care Exam 4
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
What are the early signs and symptoms of acute liver failure?
anorexia, nausea, vomiting, abdominal distention, fatigue.
What are the late signs and symptoms of acute liver failure?
low grade fever, enlarged/tender liver, jaundice
What are the types of viral hepatitis?
fecal, blood borne, fecal-oral, sexual transmission.
What are the types of non-viral hepatitis?
induced by chemicals and medications that are hepatotoxic.
EX: carbon tetrachloride, chloroform, acetaminophen, anticonvulsants, or antituberculosis agents.
What is the management for hepatitis?
there is no definitive treatment. These pts need rest, nutritional support, and preventing the spread of the virus.
What is liver cirrhosis?
destruction of healthy liver cells that over time get replaced by fibrotic tissue. This distorts the normal shape of the liver lobule. This is usually irreversible and causes chronic liver dysfunction.
What labs can be drawn to diagnose liver failure?
ALT, AST, protein, albumin, serum bilirubin, cholesterol, PT/INR, ammonia. We can also do a liver biopsy and an ultrasound
What is ascites and how does it present?
Accumulation of serous fluid in peritoneal or abd cavity
Water and sodium retention leads to decreased albumin and ascites
Can be caused by portal HTN, hypoalbuminemia, hyperaldosteronism
What is the management of ascites?
monitor abd girth, weight gain, and respiratory status. Restrict sodium, give diuretics. TIPS procedure, paracentesis.
What is a paracentesis?
removal of fluid through a small incision in the abd wall.
What is a TIPS procedure?
stent placed to serve as a shunt between the portal circulation and hepatic vein
What is hepatic encephalopathy?
Neurotoxic effects of ammonia. Liver is unable to convert increased ammonia and it crosses the blood brain barrier.
S/S: tremors, slurred speech, impaired decision making, drowsiness, loss of sphincter control, asterixis, confusion, somnolence, coma, unresponsive to pain, GI alterations.
What is the treatment for hepatic encephalopathy?
Lactulose: draws the ammonia from the bloodstream into the stool to be excreted.
Metronidazole: antibiotic that destroys normal bacteria found in the bowel to decrease protein breakdown and ammonia production.
What are the signs and symptoms of a GI bleed?
Pain or discomfort, blood emesis (hematemesis), stool bloody, tarry stools, increased bowel sounds, decreased CO, decreased BP, cold clammy skin, decreased pulses, tachycardia, decreased perfusion to kidneys/brain/lung, confusion, decreased U/O, hyperventilation
What is a stress ulcer?
type of peptic ulcer that occurs after illness trauma or neurological injury (curlings). Ischemia is primary mechanism
What are esophageal varices?
portal HTN causes the veins to become distended and varices form in the esophagus and upper portion of the stomach. These bleed very easily
What is peptic ulcer disease?
can be duodenal or gastric.
risk factors: smoking, H pylori bacteria, alcohol use, NSAIDS, steroids.
What is a Mallory-Weiss tear?
arterial hemorrhage from acute longitudinal tear in mucosa.
Can be caused by retching, alcohol use, or NSAID use
How is a GI bleed diagnosed?
Hematocrit: norm then low, Hemoglobin: norm then low, Platelets: high then low , WBC: high, PT/INR: high, BUN/CR: high, Ammonia levels, endoscopy, barium swallow study.
What is the treatment for a GI bleed?
hemodynamic stability, gastric lavage, medications, Billroth 1, Billroth 2, band ligation.
What medications are given for the treatment of GI bleeds?
PPIs (protonix, Pepcid), antacids, H2 receptor blocks, antibiotics, Somatostatin/Octreotide, Vasopressin
What is a Billroth 1?
duodenum resection
What is a Billroth 2?
jejunum resection
What are band ligation for varices?
band is placed around the varices to cut off blood flow to it and reduce the bleeding or risk for bleeding.
What is important to consider for GI bleed patients?
they are at a higher risk for hypovolemic shock due to blood loss.
What is acute pancreatitis?
inflammation of the pancreas caused by digestive enzymes being activated but not being released. this leads to an inflammatory response that causes Increased permeability causing hemorrhage, edema, and necrosis
What are the three functions of the pancreas?
endocrine, exocrine, and digestive
What are the signs and symptoms of acute pancreatitis?
Abdominal pain, nausea, vomiting, Anorexia, Ascites, Jaundice
What is Cullen's Sign?
bluish hue around the belly button which indicates severe pancreatitis.
What is Turner's sign?
severe bruising on the flank which can indicate hemorrhagic pancreatitis
What labs can be drawn to help diagnose acute pancreatitis?
lipase: rises within 12 hours of onset normal is 0-160
amylase: rises within 4-8 hours of onset normal is 30-110
LOOK FOR ELEVATION 3 TIMES THE NORMAL LIMIT
Calcium: low
ALT/AST: high (gallstones)
Alk Phos: elevated
WBC: elevated
Glucose: high
K: low with severe emesis, high with acute renal failure
What scans can be done to diagnose acute pancreatitis?
CT scan: can assess for severe cases
Xray: can visualize calcifications
Ultrasound: can detect gallstones
What is Ranson Criteria for pancreatitis?
used to predict the severity and mortality of pancreatitis.
0-2 minimal, 3-5 10-20%, 6+ 50%.
What is an ERCP?
Endoscopy like, looks at bile and pancreatic duct to see if it is emptying. If it is not, catheter goes into duct to determine blockage and place stent if needed
What are some causes of pancreatitis?
Biliary tract obstructed and alcohol abuse, Use of corticosteroids, thiazide diuretics, and sulfonamides, Trauma, hyperlipidemia, ERCP
What is the treatment for pancreatitis?
ERCP, IV hydration (crystalloids or colloids), Nutrition, (Usually NPO, TPN if severe), Pain management, Antibiotics if severe, Surgery
What are some complications of pancreatitis?
Increased abdominal pressure (causes ARDS), Respiratory distress or failure, Sepsis, Coagulopathy, Renal Failure, Acute Necrotizing Pancreatitis
What is Diabetic Ketoacidosis (DKA)?
type one diabetes. No insulin leads to hyperglycemia and cellular starvation, that burns fat and causes ketoacid production, into metabolic acidosis causing kussmaul breathing and potassium exchange
What are the signs and symptoms of DKA?
fruity smelling breath, kussmal respirations, ketones in urine
What is the treatment for DKA?
insulin drip, fluid replacement, potassium, bicarb
What is hyperglycemic hyperosmolar state (HHS)?
type 2 diabetes. No insulin leads to hyperglycemia, osmotic shift, increased U/O (potassium loss, dehydration)
What is the treatment for HHS?
insulin drip, fluid replacement, pressers
What are the nursing considerations for DKA and HHS?
Educate on managing blood glucose, diet, exercise, medication, and assess access to care, Take vitals hourly, Monitor I/O, Monitor neuro
What is SIADH?
created in the hypothalamus. Too much ADH. caused by CNS disorders that cause failure of normal regulatory feedback loops.
What are the signs and symptoms of SIADH?
confusion, lethargy, weakness, headaches, seizures
How is SIADH diagnosed?
hyponatremia, elevated urine sodium, BUN, Cr, Albumin
What is the treatment for SIADH?
Mild to moderate: fluid restriction, monitor serum sodium
severe: hypertonic saline in small amounts (correct slowly, slow infusion rates, risk of neuro damage and heart failure)
What are the causes of burns?
flame related (most common), scalding, contact, electrical, contact.
What is a superficial burn depth?
Involves epidermis and possibly a portion of the dermis
Appearance: reddened, blanches with pressure, minimal edema, possible blisters
Normally heals on its own within 3-7 days
What is partial thickness burn depth?
Involves epidermis, upper dermis, and portion of deeper dermis, Appearance: blistered, mottled, red base, weeping surface, edema, Can be grafted, Has the potential to heal on its own in 2-4 weeks
What is full thickness burn depth?
Involves epidermis, entire dermis, subcutaneous, and may involve muscle and bone. Appearance: dry, white, leathery, or charred, edema
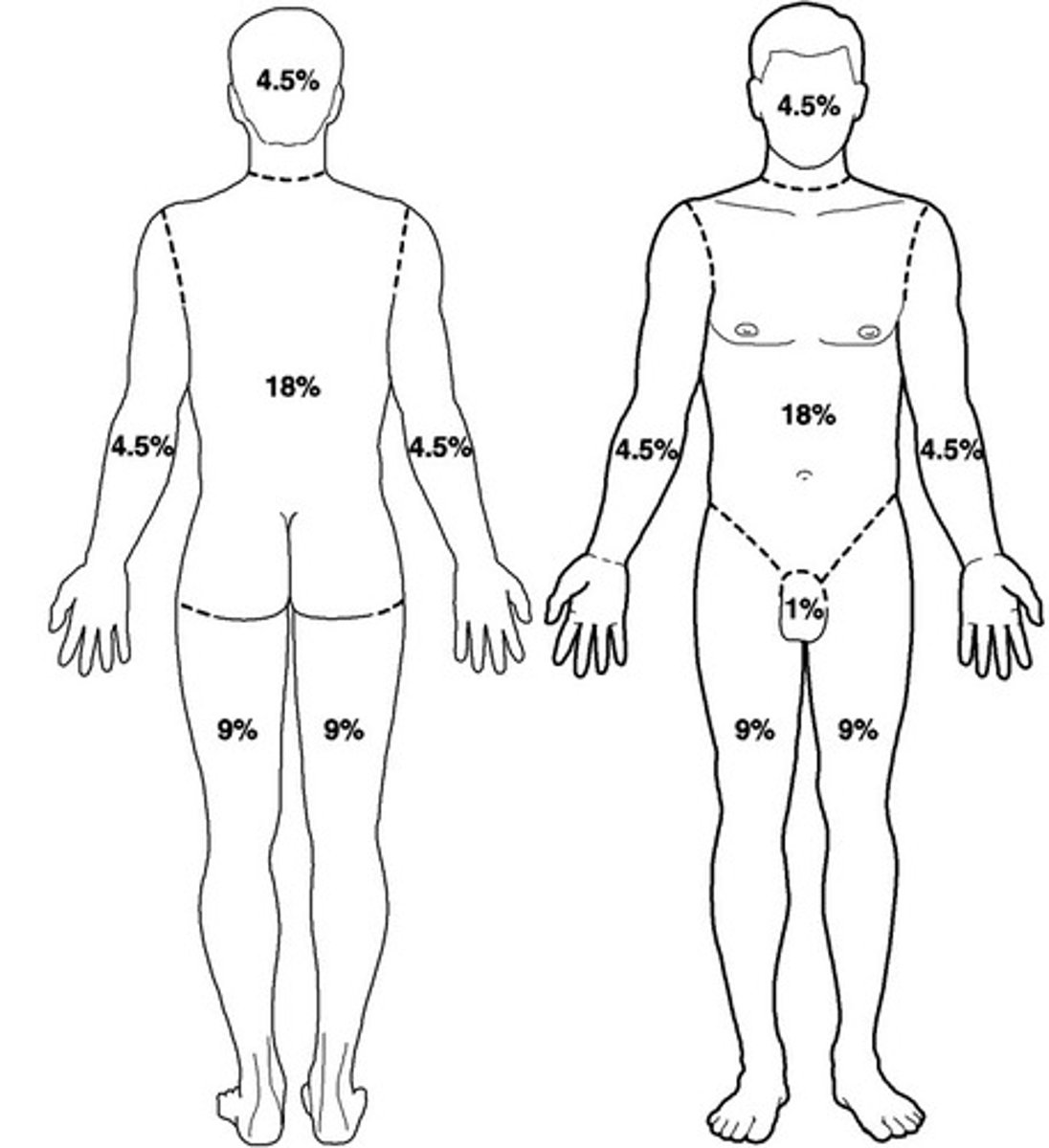
What is the rule of nines?
way to determine the extent of burns. 25-30% is considered a major burn.
What is the pathophysiology of a burn?
Transfer of energy from a heat source, burns less than 25% total body surface area produces a local response. There is swelling, constriction, and hypovolemic.
What is the Resuscitative phase of a burn?
From onset to completion of fluid resuscitation.
nursing care: Manage respiratory issues and prevent shock, Reduced blood volume and hemoconcentration, Low U/O, low BP, tachycardia, hyperkalemia, hyponatremia, metabolic acidosis, Replace fluids and electrolytes, Stop injury, cool burn, irrigate, ABC’s, start O2 and large bore IV, do assessment, foley, fluids, NG if over 25%, Maintain systolic over 100 and U/O 30-50 hourly
What is the Parkland Baxter formula?
2-4 ml x kg x %burn
What is the acute/intermediate phase of burns?
From beginning of diuresis to near completion of wound closure, 48-72 hours
Attention goes from assessment to infection prevention, nutritional support, fluid support, and pain management, Fluid re enters the vascular, hemodilution, increased U/O, sodium lowers with diuresis, hypokalemia, metabolic acidosis
What is the rehabilitation phase of burns?
From major wound closure to return of individuals optimal Early as possible, focus on wound healing, psychosocial support, self-image, lifestyle, restoring function
Home care: Mental health, skin and wound care, exercise, nutrition, pain, thermoregulation, sexual issues, no tanning
What is the wound care for burns?
Hydrotherapy, wound debridement, wound dressing, skin grafts, PERMANENT (ONLY ONE): Autograft: own skin, heals 7-14 days), Homograft/Allografts: from living or deceased human, Heterografts/Xenografts: skin from animal, Biobrane: synthetic