6. small animal med- disease of the small intestine
1/120
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
121 Terms
what are the 3 functions of the small intestine?
1. digestion (w/ help of bile salts and pancreatic digestive enzymes)
2. absorption (simple sugars, AA, oligopeptides, fat-soluble vitamins ADEK)
3. motility (peristaltic contractions move digested food down)
what are the 7 clinical features of small intestinal disease?
1. small bowel diarrhea
2. malabsorption
3. melena
4. PLE
5. ionized hypocalcemia and hypovitaminosis D
6. flatulence and borborygmi
7. weight loss and failure to thrive
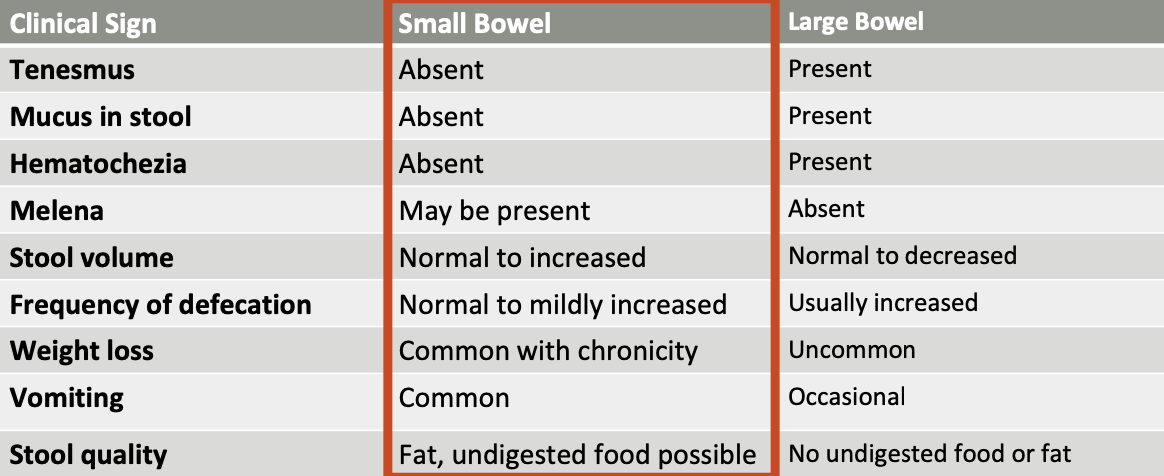
how is small bowel diarrhea differentiated from large bowel diarrhea?
small bowel:
-tenesmus, mucus, and hematochezia are absent in small bowel diarrhea
-melena may be present
-normal to increased stool volume
-frequency of defecation is normal to mildly increased
-weight loss is common with chronicity
-vomiting is common
-stool quality: fat, undigested food possible
what is malabsorption as seen in SI disease?
defective absorption of nutrients, resulting in nutrient depletion (vitamin D3, vitamin B12, folate)
what are clinical signs of malabsorption?
diarrhea
weight loss
altered appetite (polyphagia, coprophagia, pica)
what is melena?
dark, tarry oxidized blood in feces
dark black stool can also be seen with bismuth (pepto) and iron supplementation

in the absence of melena, what may be indicative of chronic blood loss due to SI disease?
iron deficiency anemia
what does protein losing enteropathy (PLE) result in?
protein leakage in gut exceeds protein synthesis--> hypoproteinemia (albumin +/- globulin)

is PLE more common in dogs or cats?
more common in dogs
if seen in cats, most often related to GI lymphoma
what other causes of hypoalbuminemia (Ddx) should be ruled out before diagnosing PLE?
1. PLN (protein losing nephropathy)
2. hemorrhage or acute phase response (inflammation)
3. liver failure
what does severe hypoalbuminemia result in?
albumin <2.0g/dL --> results in ascites, pleural effusion
predisposes to thromboembolism, most commonly PTE or aortic thrombus
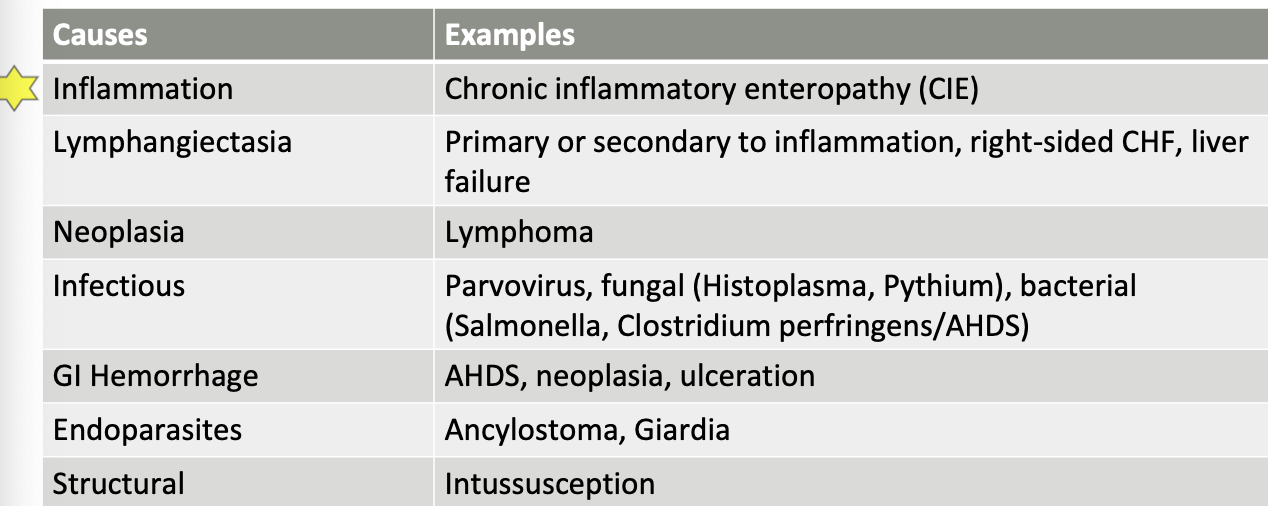
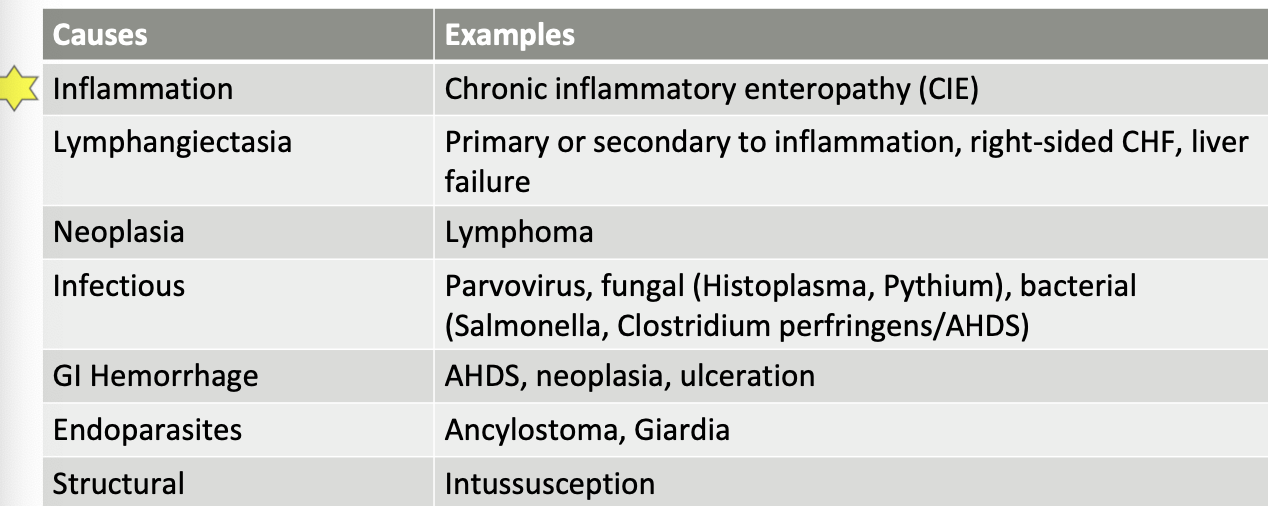
what are the general causes of PLE?
-inflammation (CIE)
-lymphangiectasia
-neoplasia (lymphoma)
-infectious etiologies (parvo, histoplasma, pythium, bacterial)
-GI hemorrhage (AHDS, neoplasia)
-endoparasites (ancylostoma, giardia)
-structural (intussusception)
I SINGLE
Ionized hypocalcemia and hypovitaminosis D, a clinical feature of SI disease, is common in ___ cases. Recommend test for ___ at ___
PLE
serum vitamin D3, Michigan State CVM
what is hypocalcemia and hypovitaminosis D associated with when seen in SI disease?
secondary hyperparathyroidism, accompanies an elevated parathyroid hormone
what is the treatment for hypocalcemia/hypovitaminosis D?
tx: calcitriol, elemental calcium (TUMs)
monitor ionized calcium and phosphorus
what is flatulence/borborygmi? what causes it?
abdominal rumbling noises caused by propulsion of gas in the GI tract
caused by swallowed air or bacterial fermentation of fiber
what causes weight loss/failure to thrive due to SI disease?
reduced nutrient intake
increased nutrient loss
increased catabolism
What is the first step when you see a patient with weight loss/failure to thrive?
check caloric intake!
What are the 6 major diseases of the small intestine?
acute hemorrhagic diarrhea syndrome (AHDS)
infectious etiologies
chronic inflammatory enteropathy (CIE)
alimentary small cell lymphoma
primary lymphangiectasia
feline gastrointestinal eosinophilic sclerosing fibroplasia (FGESF)
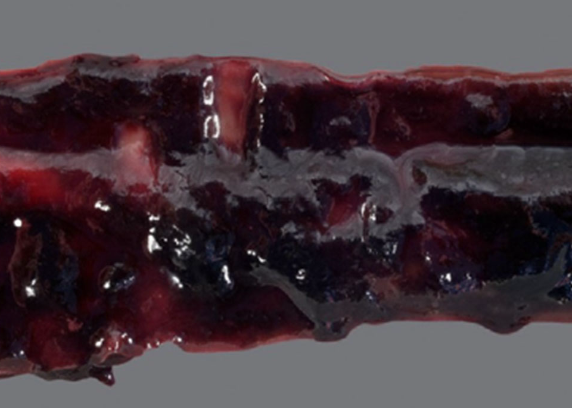
what is acute hemorrhagic diarrhea syndrome (AHDS)?
acute onset (<24 hours) of severe watery hemorrhagic diarrhea with significant fluid loss into the intestinal lumen
'raspberry jam' characteristic stool

what is the typical signalment of AHDS?
dogs only; young adult dogs

what are the clinical signs of AHDS?
vomiting is frequently the first clinical sign (hematemesis common) in 50% of cases
often norm/hypothermic at presentation

what clinpath/PE changes are seen with AHDS?
clinpath: typically reflect hypovolemia
PE: tachycardia, prolonged CRT, weak pulses
what causes AHDS?
-acute necrotizing and neutrophilic enterocolitis
-no association with diet change/dietary indiscretion
-in some cases, enterotoxemia due to clostridium perfingens (netF toxin gene)
how is AHDS diagnosed?
there is no confirmatory diagnostic test (positive fecal PCT for NetF toxin is suggestive)
diagnosis is based on clinical presentation, clinical course, and exclusion of other causes of acute GI disease
what is the diagnostic approach for AHDS?
1. perform PCV and TS
2. CBC/chem/UA, fecal float, fecal giardia ELISA, basal cortisol
3. exclude other causes of acute GI disease based on clinical picture and suspicions
how can running a PCV help with diagnosis of AHDS?
if PCV is <30% at presentation, it is not AHDS (look for other causes of GI bleed)
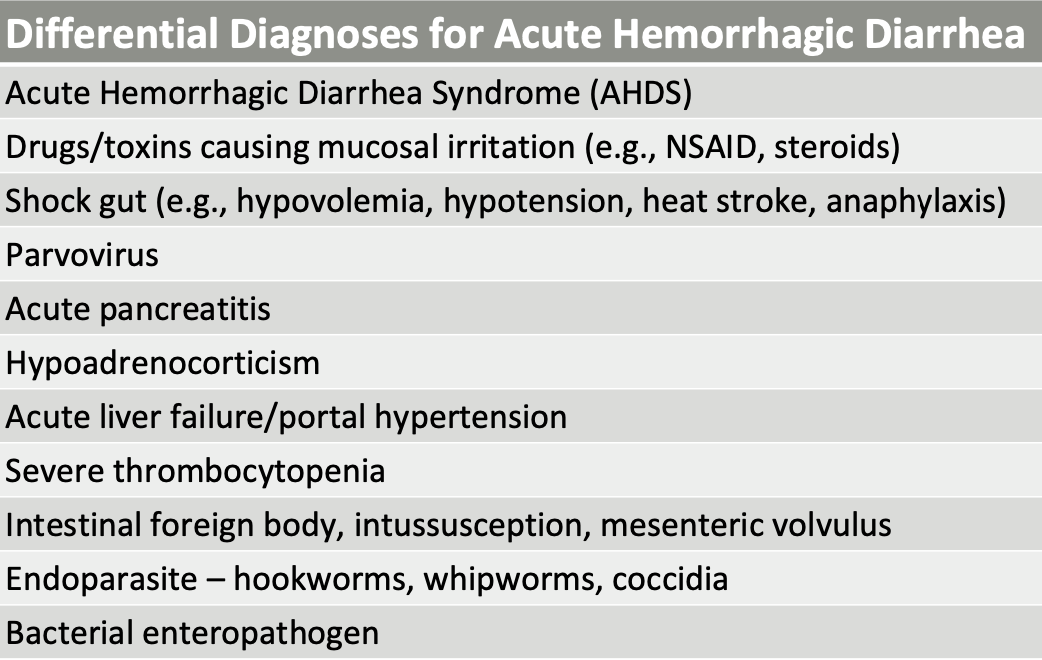
what are some differentials for acute hemorrhagic diarrhea?
-AHDS
-drugs/toxins
-shock gut
-parvovirus
-acute pancreatitis
-addison's
etc
what is included in the treatment for AHDS?
1. IV fluid replacement therapy
2. antiemetics (maropitant, ondansetron, metoclop)
3. pain meds PRN
4. nutrition (GI diet, may need to place NE/NG tube)
How should IV fluid replacement therapy be done for AHDS?
rapid volume replacement with balanced electrolyte solution
LRS/Norm R - 30 mL/kg over 10 minutes, repeated up to 3x
followed by continuous replacement of ongoing losses
how should IV fluid replacement therapy be monitored when treating AHDS?
monitor electrolytes every 12-24 hours, as well as monitor for hypoalbuminemia after rehydration
if severe <1.8 g/dL, synthetic colloids, albumin, plasma
what NSAIDs can be given to patients when treating AHDS?
opioids (fentanyl, methadone, buprenorphine)
not NSAIDs
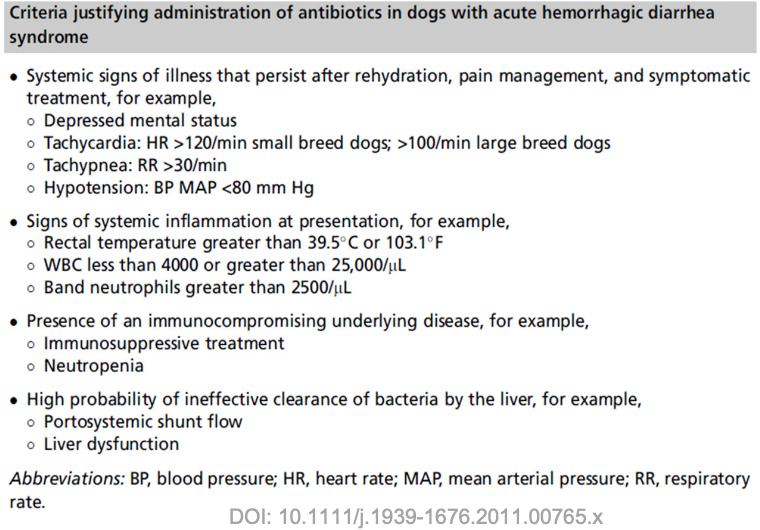
are antibiotics necessary for treating AHDS?
there is no documented clinical benefit in dogs that are not exhibiting clinical signs of sepsis
what is the prognosis for AHDS?
usually rapid improvement within 24-48 hours
what should you do if there is lack of improvement in a patient being treated for AHDS?
-reevaluate for other causes of hemorrhagic diarrhea
-look for complications (hypoalbuminemia, bacteria translocation/sepsis, DIC)
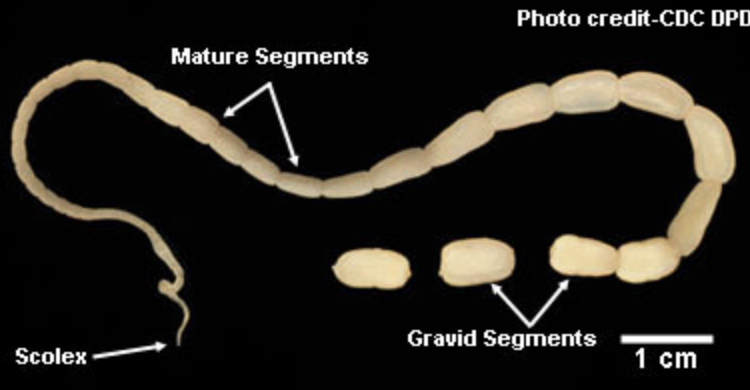
what are the most common helminths that cause SI disease in dogs and cats?
1. roundworms (toxocara canis, cati)
2. hookworms (ancylostoma)
3. tapeworms (dipylidium caninum)
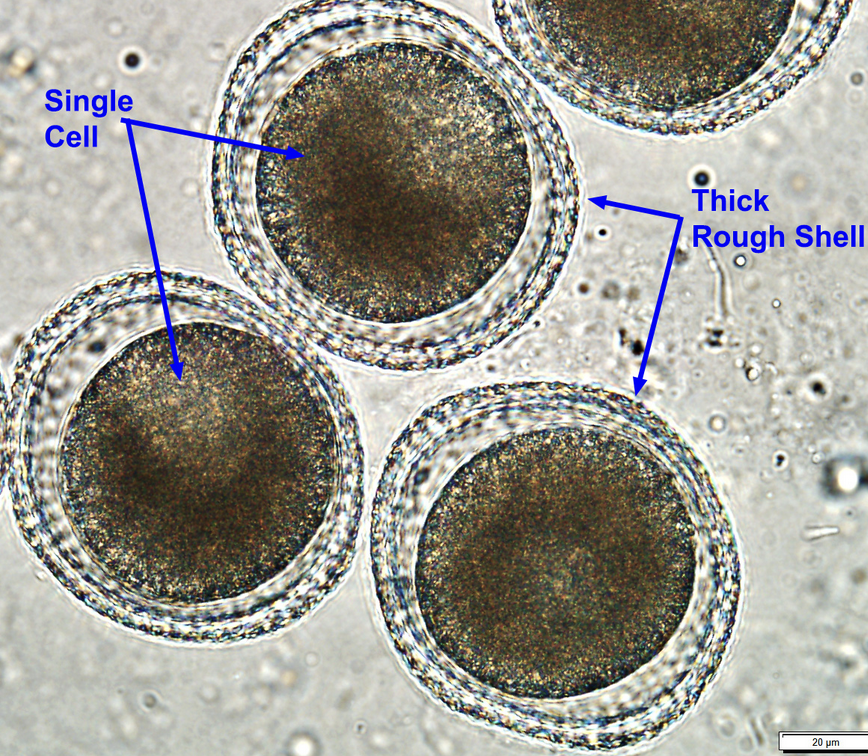
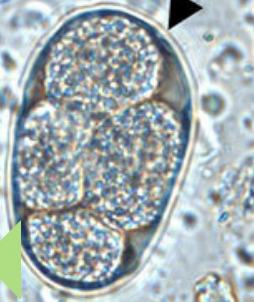
What parasite egg is this?
toxocara canis (dog) or toxocara cati (cat)

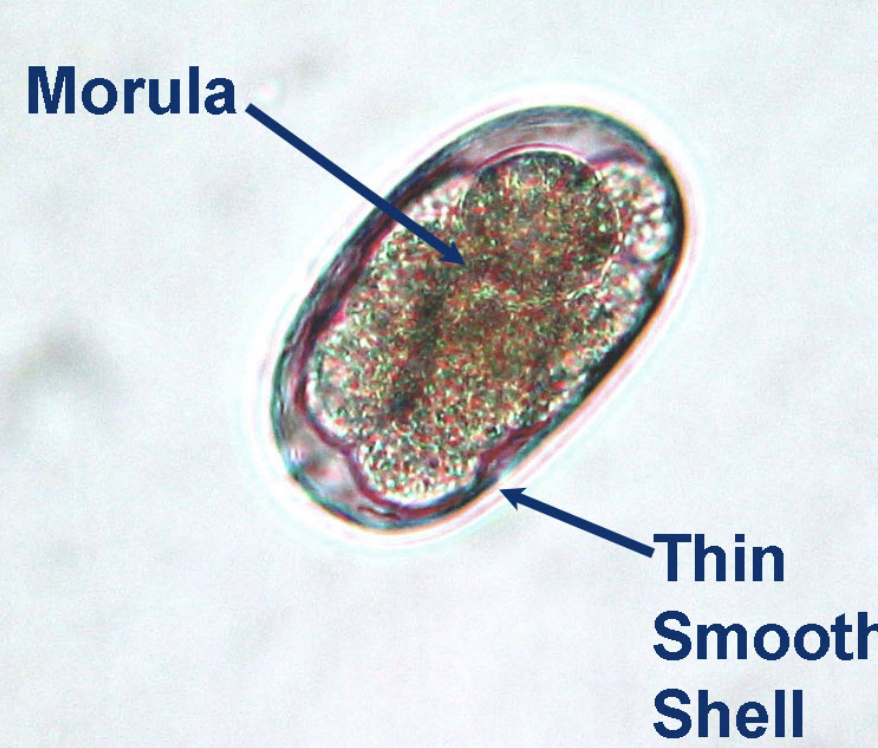
What parasite egg is this?
ancylostoma (hookworm)
What parasite egg is this?
ancylostoma (hookworm)
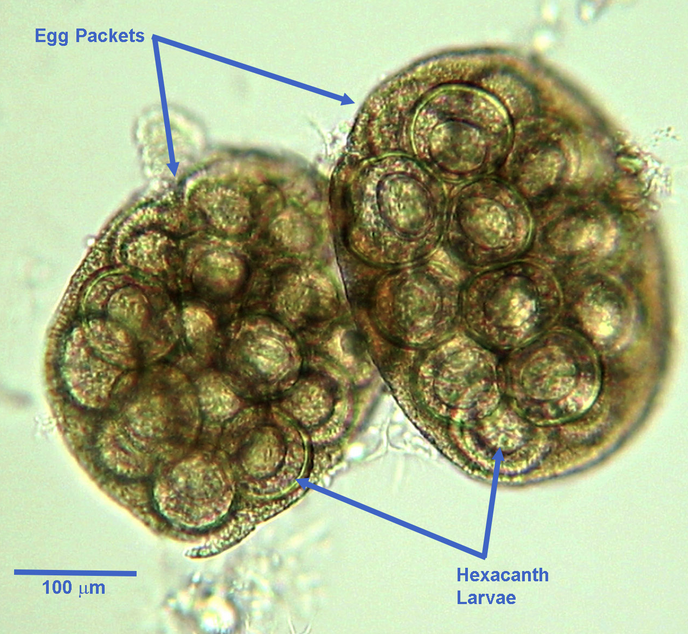
What parasite egg is this?
Diplydium caninum (tapeworm)
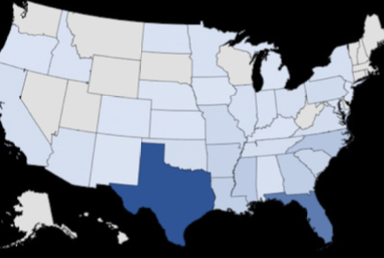
what is heterobilharzia americana?
canine schistosomiasis
trematode infecting dogs
endemic in gulf/southern atlantic coasts
larvae in standing freshwater penetrates hosts intact skin (migrates thru blood vessels to lungs and liver, mature into adults in mesenteric veins)

what lesions are seen in dogs infected with heterobilharzia americana?
granulomatous inflammation and fibrosis in affected tissues (liver and intestine)

what is the typical signalment of dogs infected with heterobilharzia americana?
younger, large breed dogs

what are the clinical signs of dogs infected with heterobilharzia americana?
asymptomatic to non-specific acute or chronic GI signs +/- liver disease
-late onset of illness possible as number of parasitic eggs deposited in tissue increases
-intestine, liver, pancreas, LNs, lungs

what clinpath changes are seen in dogs infected with heterobilharzia americana?
-anemia, regenerative or nonregenerative
-elevated liver enzymes
-hypercalcemia
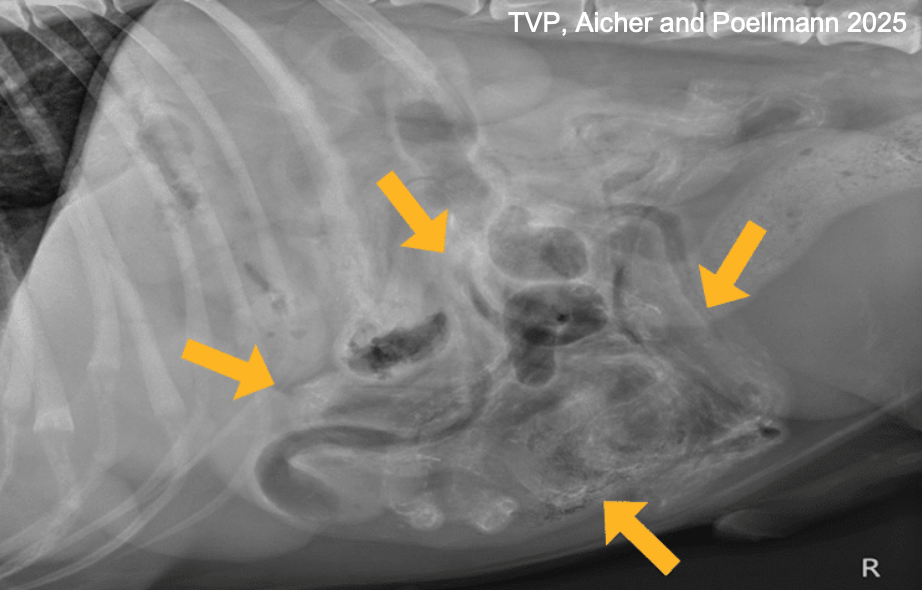
what will be seen on imaging in dogs infected with heterobilharzia americana?
rads: multifocal areas of mineralization within organs (calcified eggs)
ultrasound: pinpoint hyperechoic foci in visceral organs
how are heterobilharzia americana infections diagnosed?
1. saline fecal sedimentation
2. fecal PCR at texas A&M GI lab
3. histology of intestinal and liver biopsies (most reliable method- may reveal eggs and parasites with granulomatous inflammation)

what is the treatment for dogs infected with heterobilharzia americana?
praziquantel and fendendazole
-high doses of praziquantel for 2 days
-give with maropitant and ondansetron to reduce side effects
-may need to repeat to eradicate infection
-prednisone (to mitigate inflammatory rxn following die-off of adult parasite)
how is giardia transmitted in dogs?
ingestion of cysts
how does giardia infections in dogs cause SI disease?
trophozoites attach to surface of SI enterocytes and cause blunting of intestinal villi
--> maldigestion, malabsorption, diarrhea

what are the clinical signs of giardia infections in dogs?
most infections are asymptomatic but clinical picture can vary:
-mild, self-limiting acute diarrhea
-severe or chronic small bowel diarrhea and weight loss
-PLE (rare)
how is giardia diagnosed in dogs?
test dogs with a combo of:
-fecal wet mount (falling lead motility)
-fecal flotation with centrifugation
-fecal ELISA/IFA
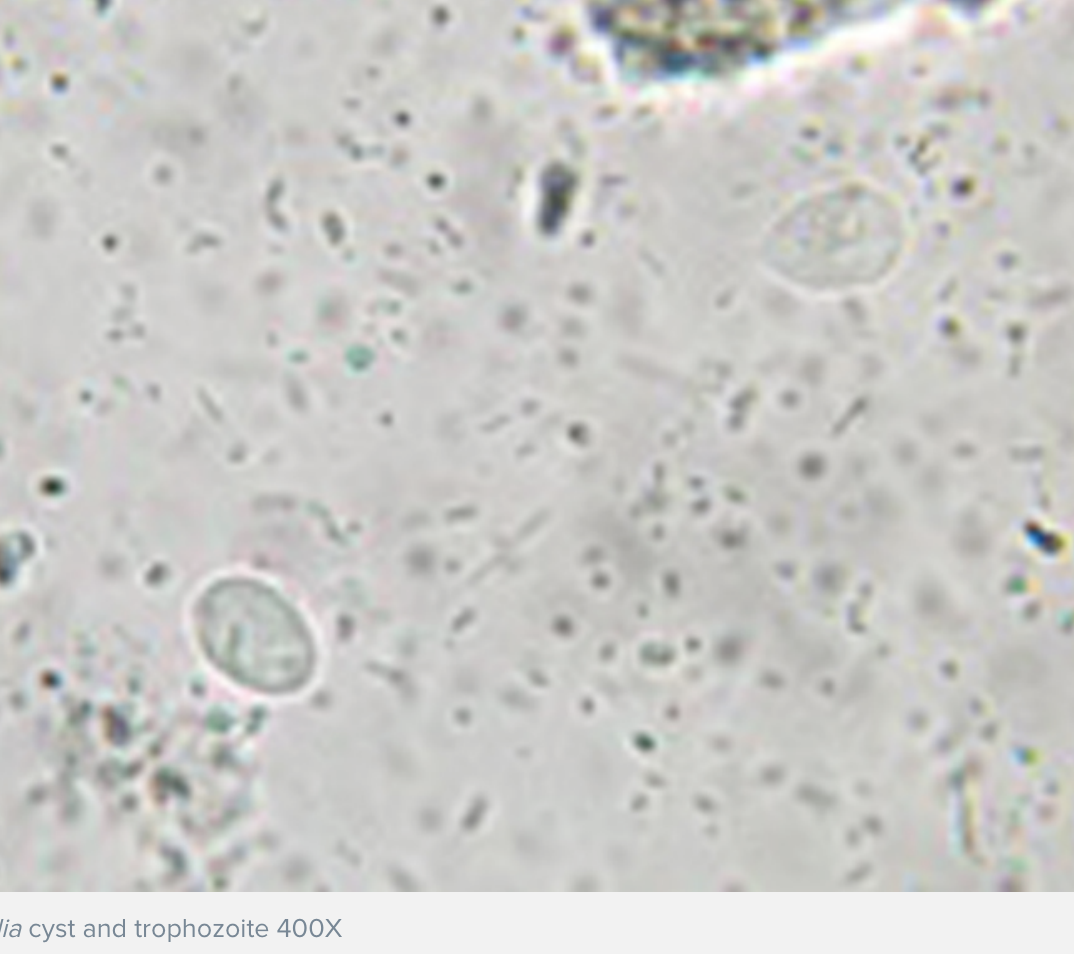
what is the treatment for symptomatic dogs infected with giardia?
metronidazole for 5-8 days or fenbendazole for 3-5 days
use combo of both in resistant cases
should you treat asymptomatic dogs infected with giardia?
no (may develop resistance if treating asymptomatic dogs)
where do most infections of histoplasma capsulatum occur?
ohio, missouri, mississippi river valleys
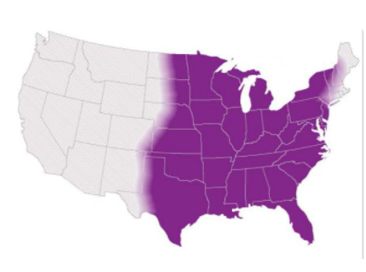
what are the 2 forms of histoplasma capsulatum infections?
1. pulmonary
2. disseminated
how does the disseminated form of histoplasma capsulatum present in dogs and cats?
dogs: most commonly manifests as small and/or large bowel signs with weight loss, fever, inappetence
cats: GI signs are rare and manifest as respiratory or ocular disease

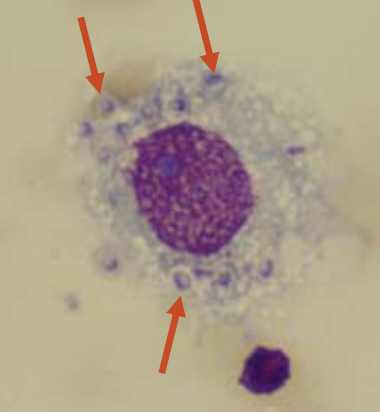
how are histoplasma capsulatum infections diagnosed?
1. cytology and histology of affected organ or draining LN (rectal scrape to look for organisms within macrophages)
2. urine and serum galactomannan antigen (highest sensitivity achieved with testing both urine and serum)
what is the treatment for animals infected with histoplasma capsulatum?
antifungal for >6 months
-itraconazole
-fluconazole
-amphptericin B for very severe/sick animals
what is pythiosis?
infection of a fungus-like, water mold pythium insidiosum
mostly seen in gulf coast states and OK area
not contagious
what are the 2 forms of pythiosis?
1. cutaneous form: from direct contact with skin wound (causes ulcerative, nodular skin lesions)
2. GI form: from ingestion of infected water

what factors may indicate infection of pythiosis?
suspect when:
-in endemic area
-focal or multifocal transmural thickening of intestinal tract (pylorus and ileocolic junction most commonly affected)
-pyogranulomatous inflammation
how is pythiosis diagnosed?
diagnosis is difficult: ☹
-recommend surgical biopsy to evaluate submucosa
-may miss on routine H&E stain
-requires special stains (PAS, GMS)
-tissue PCR and ELISA titer
how is pythiosis treated?
treatment is difficult and usually a fatal disease:
-wide surgical excision
-itraconazole and terbinafine for 6-9 months
-use ELISA to monitor tx and for relapse
what is the prognosis of pythiosis?
poor ☹

are feline and canine parvovirus caused by the same virus?
DNA viruses are antigenically similar but species specific
how are canine/feline parvoviruses transmitted?
fecal-oral route or fomites
how do animals obtain immunity for parvoviruses?
-vaccination (very effective at preventing disease)
-maternal antibodies (susceptibility wanes around 12-14 weeks of age)
what are clinical signs/presentations of parvovirus infections?
acute small bowel hemorrhagic diarrhea with neutropenia
-vomiting, inappetence, weakness
-septicemia, endotoxemia, shock
how are feline/canine parvovirus infections diagnosed?
POC fecal antigen ELISA (use canine fecal antigen test in cats)
-high specificity, low sensitivity
-false positives: 4-8 days after vaccination with modified live vaccine
-false negatives: transient fecal shedding, antibodies bind virus, specific viral antigen not tested
what is an important differential for parvovirus that should be included in diagnostic testing?
ancylostoma (hookworms)
what is the general treatment for parvo infections?
supportive treatment, requires on average 3-5 days of treatment
what does treatment for hospitalized patients with parvo include?
-IV fluid therapy with potassium supplementation
-antibiotics (due to high likelihood of becoming septic)
-maropitant +/- ondansetron
-nutrition
-pain control (opioid)
(canine parvovirus monoclonal ab - $$$, study show no difference in hospitalization time if treating symptomatically in both treated and control)
what does out-patient treatment for parvovirus infections include?
-IV fluid resuscitation followed by SQ fluids
-convenia (Cefovicin) SQ injection once
-maropitant SQ q 24hrs
-oral karo syrup q2-6 hours until eating
-tumil-k (potassium gluconate) q4-6 hours until eating
-daily DVM exam
what is the prognosis of parvovirus infections?
great with treatment
survival:
-inpatient= 90%
-outpatient= 80%
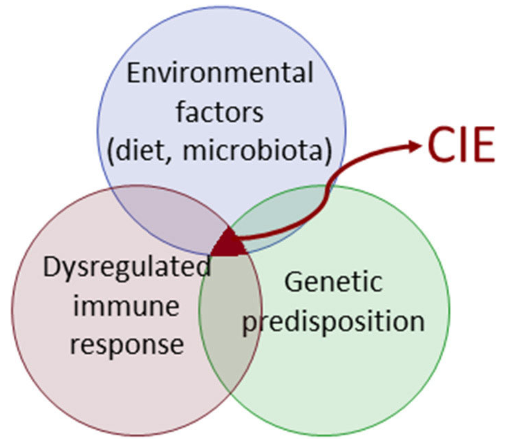
what is the etiology of chronic inflammatory enteropathy (CIE)?
unknown, likely due to a combination of factors such as:
-environmental factors
-dysregulated immune response
-genetic predispositions
what 3 factors is diagnosis of CIE based on?
1. presence of chronic GI signs >= 3 weeks
2. exclusion of other underlying causes (primary and secondary GI dz)
3. histopathologic evidence of intestinal mucosal inflammation
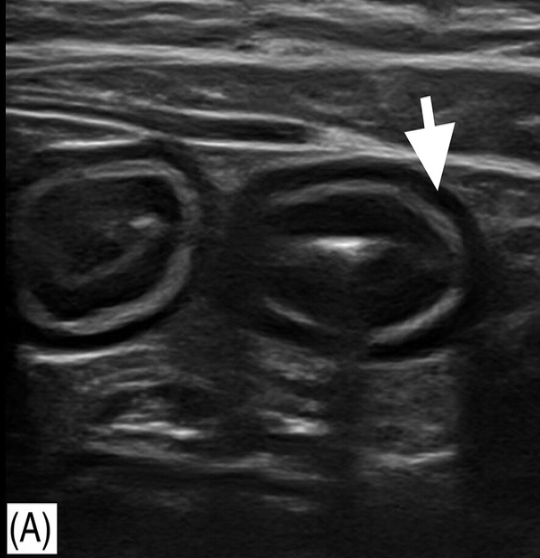
is ultrasound beneficial for diagnosing CIE?
U/S findings are highly variable and no distinguishing features (can use U/S to exclude other causes of chronic GI symptoms)
U/S of GI tract can be normal
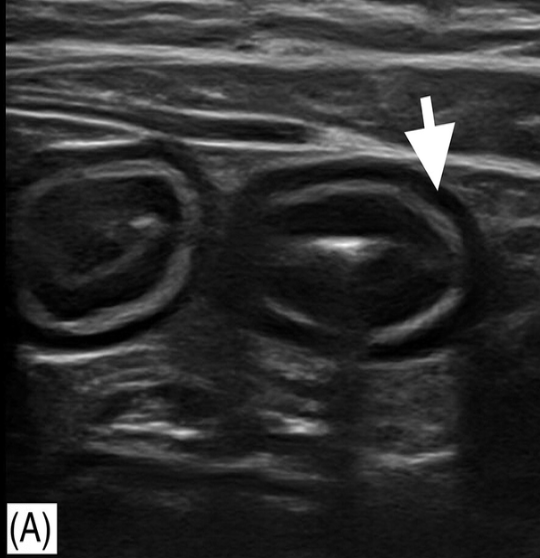
what are non-specific findings seen on ultrasound in animals with CIE?
thickening of muscularis propria (most common), submucosa, or mucosal layer
abdominal (reactive) lymphadenopathy
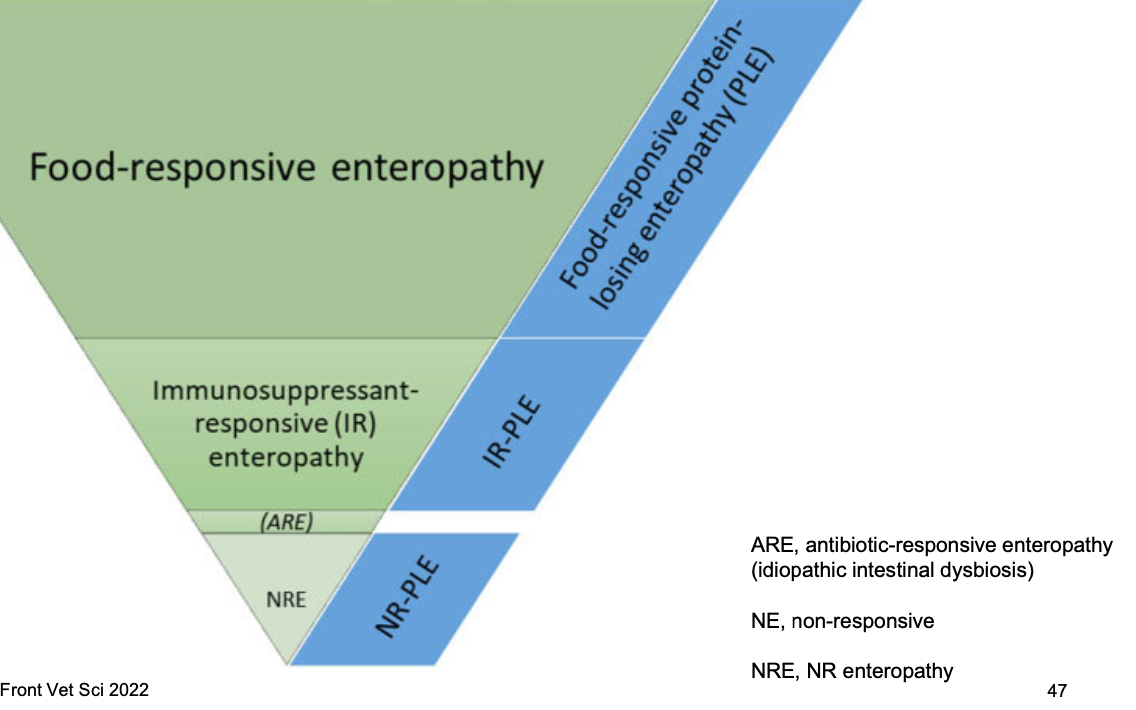
what is CIE classification based on? what are the 3 classifications?
based on response to therapy:
1. food-responsive CIE (signs resolve/improve within 2-4 wks of hypoallergenic diet)
2. steroid-responsive CIE
3. non-responsive CIE

what is the first line therapy and diagnostic for CIE?
diet trial
how is food-responsive CIE diagnosed?
diagnosed based on favorable response to diet:
-elimination diet (commercial hydrolyzed protein diet, or novel protein/limited ingredient diet)
-commercial or home cooked low-fat diet
-fiber enhanced diet
do most dogs/cats with CIE respond to diet changes?
yes, most dogs and cats with CIE respond to diet (>60% of cases)
-typically younger and less severe clinical signs than dogs wit other CIE subclasses
when are intestinal biopsies indicated for animals with CIE?
endoscopy or surgical biopsies recommended only after 2-3 diet trials
what are the exceptions to the rule of performing intestinal biopsies only after 2-3 diet trials?
-rapidly progressive decline in clinical status
-severe clinical signs unresponsive to supportive care measures (ie dysrexia)
-unstable PLE (ascites, thromboembolism)
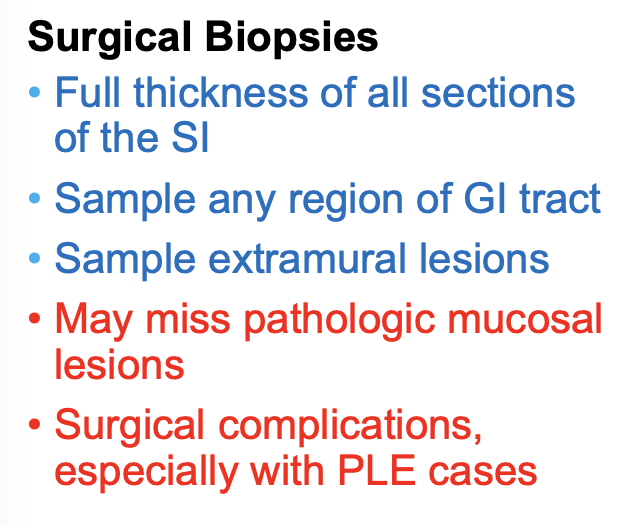
what are advantages of intestinal surgical biopsies?
-full thickness of all sections of small intestine
-sample any region of GI tract
-sample extramural lesions
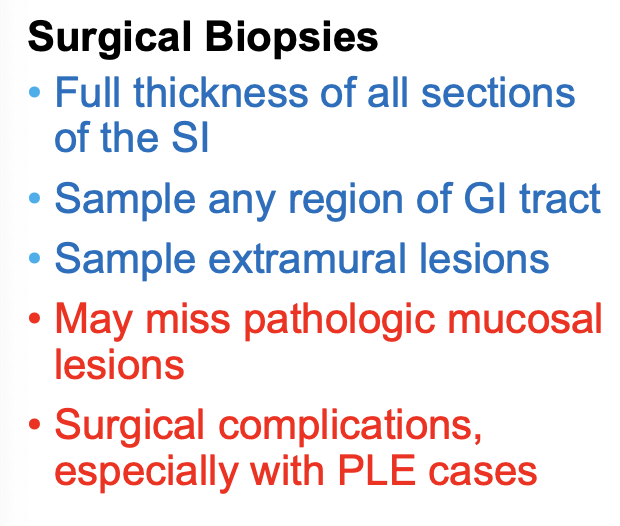
what are disadvantages of intestinal surgical biopsies?
-may miss pathologic or mucosal lesions
-surgical complications, especially with PLE cases
what are advantages of intestinal endoscopic biopsies?
-target specific mucosal regions
-obtain 5-10 samples of duodenum and ileum
-outpatient procedure with minimal complications
what are disadvantages of intestinal endoscopic biopsies?
-limited mucosa +/- submucosa sampled
-unable to reach jejunum in large breed dogs
what is steroid responsive CIE?
idiopathic intestinal inflammation responsive (at least in part) to immunosuppression (often prednisolone/one or budesonide)
how is steroid-responsive CIE diagnosed?
diagnosis of exclusion
referred to as idiopathic inflammatory bowel disease (IBD)
how is steroid-responsive CIE characterized?
characterized based on type of inflammatory cell:
-lymphoplasmacytic (most common)
-eosinophilic
-granulomatous (rare- look for evidence of parasitic or fungal dz)
what drugs are used for treatment of steroid-responsive CIE in dogs?
1. prednisone (start at higher dose 1-2mg/kg PO x 2wk, then taper down to lowest effective dose 25% q2wks)
2. budesonide (1-3mg/day)
3; cyclosporine (5mg/kg PO q12-24h)
when is budesonide used in place of prednisone for treatment of steroid-responsive CIE in dogs?
for diabetic dogs or dogs with adverse reactions to prednisone
considered first-choice glucocorticoid in dogs >25kgs
slower than pred, has a 10-14 day lag before seeing clinical response
when is cyclosprine used for treatment of steroid-responsive CIE in dogs?
for dogs that dont tolerate glucocorticoids
can freeze capsules to reduce stomach upset
what drugs are used for treatment of steroid-responsive CIE in cats?
1. prednisOLONE (start high 1-2mg/kg PO SIDx2 wks, then taper down to lowest effective dose- watch for diabetes and aggravation of cardiac dz)
2. budesonide (no studies in cats, may have anecdotal improvement)
what does concurrent treatment for CIE include?
-multi-strain, high dose probiotics (Visbiome)
-fecal microbial transplant (FMT)
-fiber (prebiotic efect--> psyllium husk)
-folate and cobalamin supp.
-clopidogrel for PLE patients (prevention of thromboembolism)
how are patients with CIE monitored?
-assess response to tx with CCECAI/FCECAI scores
-body weight
-CBC/chem/UA q3-6 months (monitor for hypoalbuminemia, monitor for side effects of immunosuppressive therapy)
what are the treatment goals for CIE?
>75% improvement in CCECAI/FCECAI score
albumin >2.0g/dL
is alimentary small cell lymphoma more common in dogs or cats?
cats »»» dogs