Sodium Disorders II
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
19 Terms
Hypernatremia (>145 mEq/L)
Cause
Excess Na intake or excess water loss
↑ Osmolality → water shifts ICF → ECF
Clinical Effects
↓ Brain volume
Risk of cerebral vein rupture → focal intracerebral hemorrhage
Possible irreversible neurologic damage
Correction Goal
Target Na <145 mEq/L
Max correction rate: 10–12 mEq/L/day
Hypernatremia – Symptoms
Mild: lethargy, weakness, confusion, restlessness, irritability
Moderate: twitching
Severe: seizures, coma, death (usually acute Na >160 mEq/L)
Other: orthostatic hypotension, tachycardia, dry mucous membranes, ↓ skin turgor, ↑ or ↓ urine output
Hypernatremia – Labs
Serum Na >145 mEq/L
Urine Na and/or urine osmolality may help determine cause
Hypernatremia – Risk Factors
Hospitalized (iatrogenic), ICU
Elderly or infants
Tube feeding
Diabetic non-ketotic hyperglycemia
GI disorders
Renal dysfunction
Diabetes insipidus
Treatment & Limits of Correction of Severe Hypernatremia
Severe hypernatremia = plasma Na⁺ >150 mmol/L
Duration | Related Condition / Cause | Clinical Features | Initial Therapeutic Goal | Limit of Correction / Overcorrection Risk |
|---|---|---|---|---|
Minutes–Hours (Acute) | • Acute salt poisoning (accidental ingestion, suicide attempt) • Hypertonic saline administration • Dialysis errors | • Seizures • Coma • Hypertonia • High fever • Intracranial hemorrhage • Dural sinus thrombosis | Rapid infusion of 5% dextrose in water (D5W) ± Emergency hemodialysis→ Immediate restoration of normonatremia | Excessive correction NOT known to be harmful |
1–2 days | • Unreplaced urinary water losses • Glycosuria • Neurogenic or nephrogenic diabetes insipidus | • Persistent coma • Brain demyelination | Lower plasma Na⁺ by ~2 mmol/L/hour → Until Na⁺ reaches 145 mmol/L, then stop or replace ongoing losses | Excessive correction NOT known to be harmful |
Unknown or ≥2 days | Children: diarrhea, inability to breast-feed Adults: hypodipsia, impaired mental status | • Obtundation or coma • Rehydration-associated seizures • Cerebral edema(esp. children) | Children: ↓ Na⁺ by 0.3 mmol/L/hour Adults: ↓ Na⁺ by ≤10 mmol/L/day → Replace water losses | Children: avoid ↓ Na⁺ >0.5 mmol/L/hour ⚠ Use 3% saline if seizures occur with rehydration ⚠ Adults: risk of overcorrection unclear |
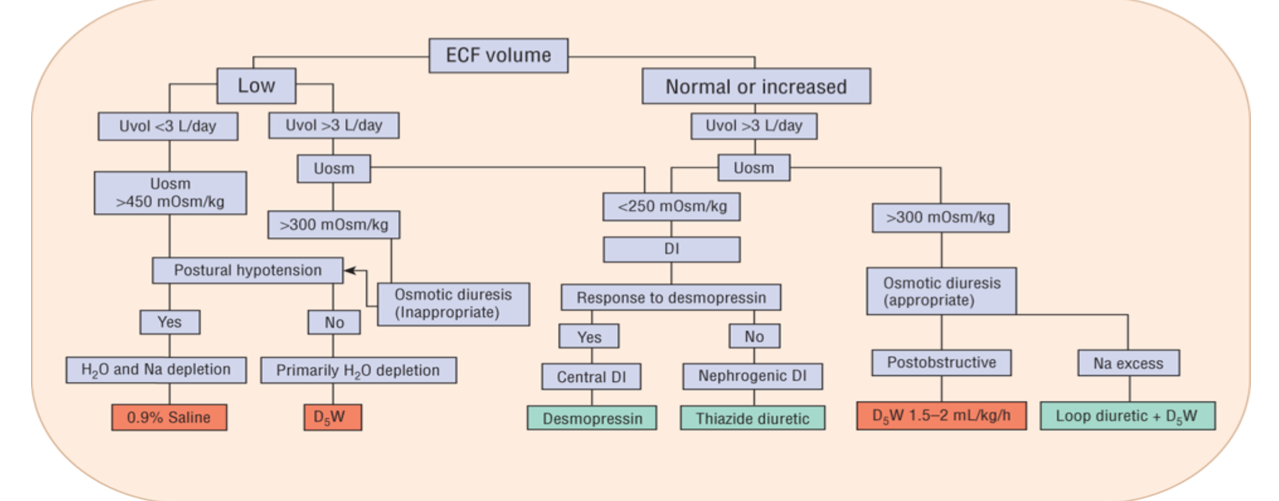
Treatment Algorithm
Hypovolemic Hypernatremia
Most common cause of hypernatremia
Primary problem: water loss >>> sodium loss
Causes
Renal losses
Loop diuretics
Osmotic diuresis (mannitol, glucose)
Postoperative diuresis
High-output acute tubular necrosis
Intrinsic renal disease
Extrarenal losses
GI losses
Cutaneous losses (burns, excessive sweating)
Physiologic Effects
TBW ↓↓
TBNa ↓
Laboratory Findings
Renal losses → UOsm high, UNa high
Non-renal losses → UOsm high, UNa low
Clinical Presentation
Orthostasis
Hypotension
Tachycardia
Treatment
0.9% NaCl until vital signs stable, then free water replacement
Hypovolemic Hypernatremia – Treatment
Rapid development (<48 hours)
Can correct more rapidly
Correction rate: 1–2 mEq/L/hr
Chronic hypernatremia
Correct slowly to prevent cerebral edema
Vital signs unstable (low BP, tachycardia)
Give 0.9% NaCl first to restore volume and stabilize patient
Then switch to hypotonic fluids
Vital signs stable
Start hypotonic fluids:
D5W
0.2% NaCl
0.45% NaCl
More hypotonic fluid → slower infusion rate
Rate of Correction: Equations
Hypernatremia due to water loss
Do NOT memorize the equation
Know TBW fraction:
Men: 60% (0.6)
Women: 50% (0.5)
Elderly (>60 yrs): 45% (0.45)
Free Water Deficit
Formula:
Free water deficit (L) =
(% total body water) × (weight, kg) × [(Current Na / Ideal Na) − 1]
Expected Change in Serum Sodium
Per liter of infusate:
ΔNa (mEq/L) =
(Infusate Na − Serum Na) ÷ (TBW + 1)
Practice: Calculate Free Water Deficit
Patient
55-yo male, 86 kg
Light-headed, dehydrated after working outdoors in heat
No access to water
Meds: HCTZ 25 mg, lisinopril 10 mg
Vitals
BP 89/54, HR 121, Temp 97.4°F, O₂ 94% RA
Labs
Na 156, K 5.3, Cl 102, CO₂ 24
SCr 2.2, BUN 35, glucose 119
Calculation
TBW = 0.6
Free water deficit:
0.6 × 86 × [(156 / 140) − 1]
≈ 6 L
Treatment
Start 0.9% NaCl until vital signs stabilize
Then switch to 0.45% NaCl
Euvolemic Hypernatremia
Pure water loss exceeds sodium loss
Classically due to diabetes insipidus
Extrarenal free water loss
Increased insensible losses
Characteristics (Euvolemic / Isovolemic)
Water & Sodium: Water loss only
Causes:
Congenital or acquired diabetes insipidus (DI)
Nephrogenic DI
Effect on TBW: ↓
Effect on TB Na: ↔
Laboratory:
Renal: UOsm low, UNa variable
Non-renal: UOsm high, UNa variable
Clinical Presentation:
Depends on severity: lethargy, seizures
Treatment:
Free water replacement
Vasopressin
Treatment Principles
Treat underlying cause of free water loss
Replace:
Free water deficit
Ongoing losses
Daily maintenance needs
Diabetes insipidus
Discontinue offending agents
Initiate pharmacotherapy
Diabetes Insipidus
Inadequate ADH secretion (central) OR
Renal tubules unresponsive to ADH (nephrogenic)
Clinical Manifestations
Polyuria
Polydipsia
Nocturia
Urine output: 3–18 L/day
Urine specific gravity: < 1.005
Urine osmolality: < 200 mOsm/kg
Euvolemic Hypernatremia – Treatment
Free access to water or D5W
Correct serum Na slowly
Rate: 0.5 mEq/L/hr
Max correction: 10–12 mEq/L/day
Goal: prevent cerebral edema
Treatment of Diabetes Insipidus
Remove underlying cause if possible
Central DI
Replace ADH
Desmopressin 5–20 mcg intranasal q12–24h
Chronic cases
Pharmacologic therapy as needed
Lithium-induced DI → treat with amiloride
Drug-Induced Diabetes Insipidus
Lithium = most common offender
DI incidence with lithium: 15–87%
Long-term lithium patients: ~12%
Usually reversible
Rarely fatal (only 3 reported deaths)
Mechanism
Antagonizes adenylyl cyclase & cAMP
Inhibits aquaporin channel opening in renal tubules
Prevents water reabsorption in collecting duct
Euvolemic Hypernatremia – Diabetes Insipidus Treatment
Drug | Indication | Dose |
|---|---|---|
Desmopressin acetate | Central and nephrogenic DI | 5–20 mcg intranasal q12–24 h |
Chlorpropamide | Central DI | 125–250 mg PO daily |
Carbamazepine | Central DI | 100–300 mg PO BID |
Clofibrate | Central DI | 500 mg PO QID |
Hydrochlorothiazide | Central and nephrogenic DI | 25 mg PO q12–24 h |
Amiloride | Lithium-induced nephrogenic DI | 5–10 mg PO daily |
Indomethacin | Central and nephrogenic DI | 50 mg PO q8–12 h |
Hypervolemic Hypernatremia
Uncommon
Caused by addition of sodium to the ECF
Sodium gain > water gain
Causes
Iatrogenic (most common)
NaHCO₃ infusion
Hypertonic saline infusion
Salt tablets
Hypertonic tube feedings
Hypertonic dialysate
Sodium-containing medications
Hyperalimentation (TPN)
Cushing’s syndrome
Ingestion of sea water
Hypertonic dialysis
Physiology
↑ Total body water (TBW)
↑↑ Total body sodium (TBNa)
Laboratory Findings
Urine osmolality: high
Urine sodium: high
Clinical Presentation
Peripheral edema
Pulmonary edema
Variable blood pressure
Treatment
Free water AND loop diuretics
Loop diuretics alone are not sufficient
May require hemodialysis to remove excess volume
Classifications of Hypernatremia
Feature | Hypovolemic | Euvolemic (Isovolemic) | Hypervolemic |
|---|---|---|---|
Water & Sodium | Water loss >>> sodium loss | Water loss only | Sodium gain > water gain |
Causes | DiureticsOsmotic diuresisPost-op diuresis | Diabetes insipidus (central or nephrogenic)Primary polydipsia | Na overload (3% NaCl, NaHCO₃, salt tablets, tube feedings) |
Effect on TBW | ↓↓ | ↓ | ↑ |
Effect on TBNa | ↓ | ↔ | ↑↑ |
Laboratory | UOsm highUNa high (renal)UNa low (non-renal) | DI: UOsm lowUNa variable | UOsm highUNa high |
Clinical Presentation | OrthostasisHypotensionDry mucous membranes | Neurologic symptoms (seizures, lethargy) | Peripheral/pulmonary edemaVariable BP |
Treatment | 0.9% NaCl first until stableThen free water replacement | Free water replacementVasopressin for DI | Free water + loop diureticMay require dialysis |
Patient
31-year-old male
Bipolar disorder
Lithium increased from 200 mg BID → 400 mg BID
Now has polyuria and polydipsia
Labs
Na 154
K 4.1
Cl 115
CO₂ 22
BUN 16
SCr 1.1
Glucose 110
Question
What is the best treatment option?
Answer Choices
A. Stop lithium, give one-time amiloride
B. Decrease lithium back to 200 mg BID, start amiloride daily
C. Stop lithium, give D5W
D. Continue lithium, give furosemide
Decrease lithium back to 200 mg BID, start amiloride daily
Patient
83-year-old female
Recently discharged for SIADH
On NaCl 1 g TID for 1 week
Now thirsty, retaining water, gained 5 lb
Labs
Na 149
Question
What is the best treatment option?
Answer Choices
A. Decrease NaCl to 1 g once daily
B. Stop NaCl, give amiloride
C. Stop NaCl, encourage free water, give furosemide
D. Stop NaCl, give desmopressin
Stop NaCl, encourage free water, give furosemide