First Aid USMLE Step 1: GI
1/167
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
168 Terms
What is gastroschisis?
Results from a defect in what stage of embryonic gut development?
What is gastroschisis?
- extrusion of abdominal contents through abdominal folds (usually right of umbilicus); NOT covered by peritoneum
Results from a defect in what stage of embryonic gut development?
- defect in lateral fold closure

What is an omphalocele?
Results from a defect in what stage of embryonic gut development?
What is an omphalocele?
- persistent herniation of abdominal contents into umbilical cord, sealed by peritoneum
Results from a defect in what stage of embryonic gut development?
lateral fold closure

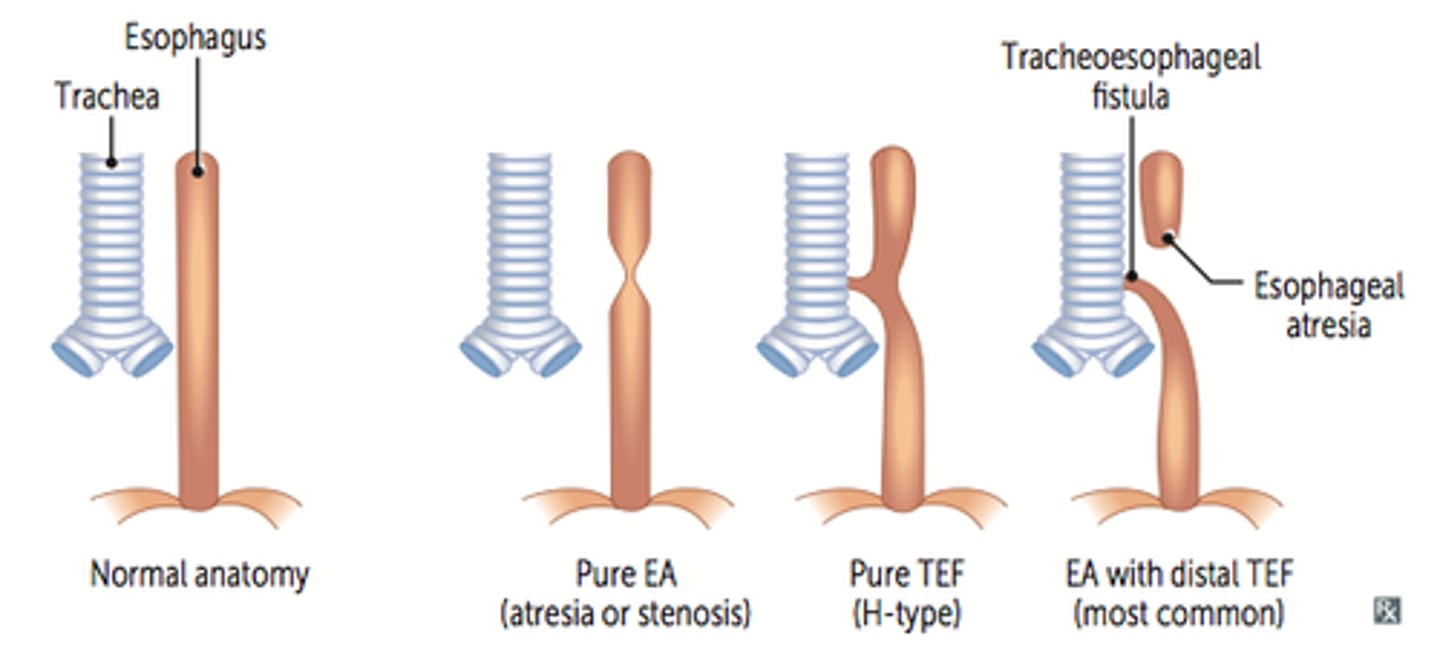
What are the 3 different kinds of tracheoesophageal anomalies that arise during development?
What causes them?
What are the symptoms?
Which is the most common?
1. pure esophageal atresia (EA) (atresia or stenosis) --> no gas in stomach
2. pure transesophageal fistula (TEF; aka H type) --> gas in stomach
3. EA with distal TEF --> gas in stomach
.
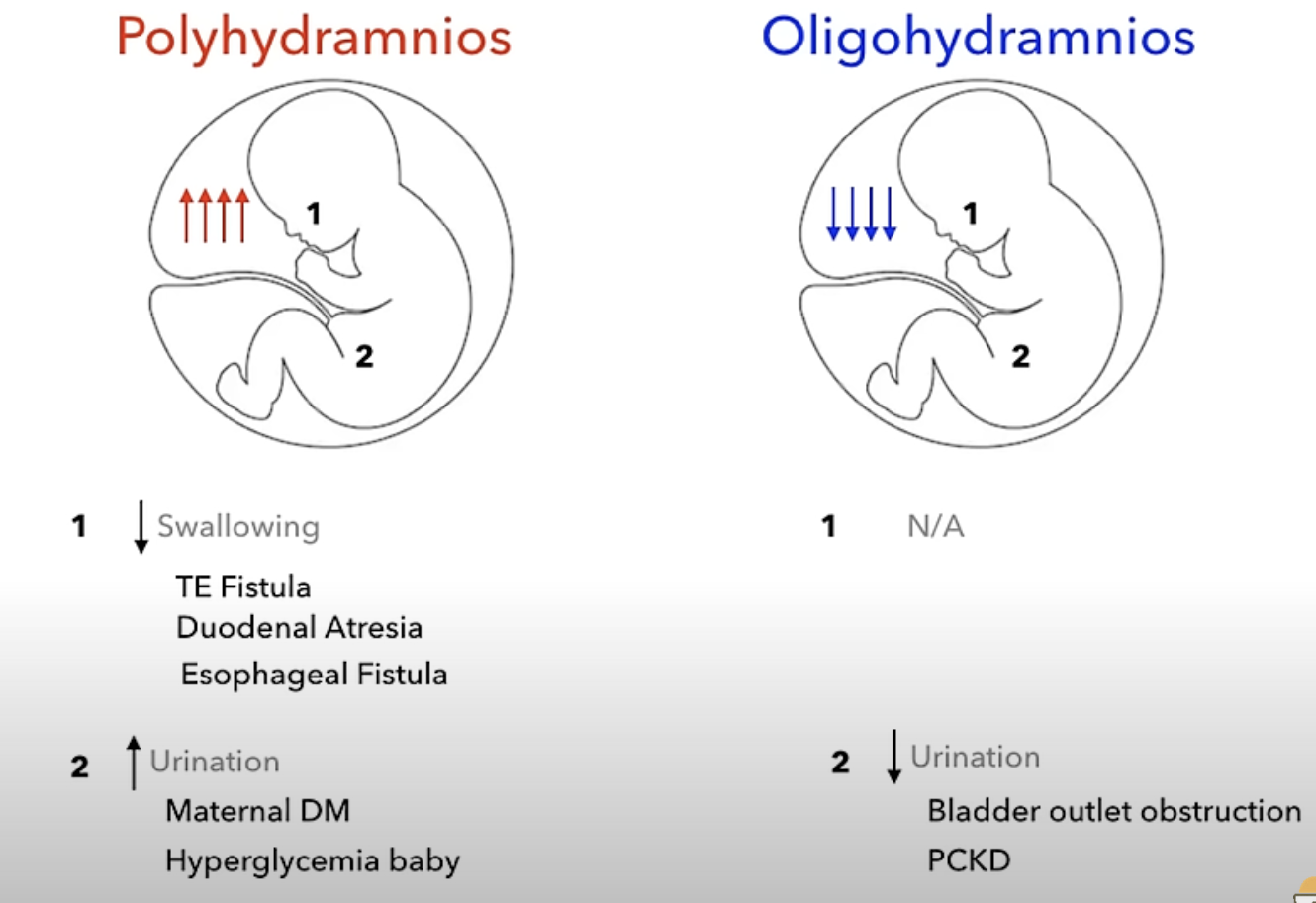
What causes them?
polyhydramnios in utero
.
What are the symptoms?
- drooling, choking, vomit with first feeding (non-bilious)
- TEF allows air to enter stomach which is visible on CXR
- cyanosis is 2/2 laryngospasm
- clinical test = failure to pass NG tube into stomach
.
Which is the most common?
- EA with TEF
What is polyhydramnios?
excess of amniotic fluid in the amniotic sac.
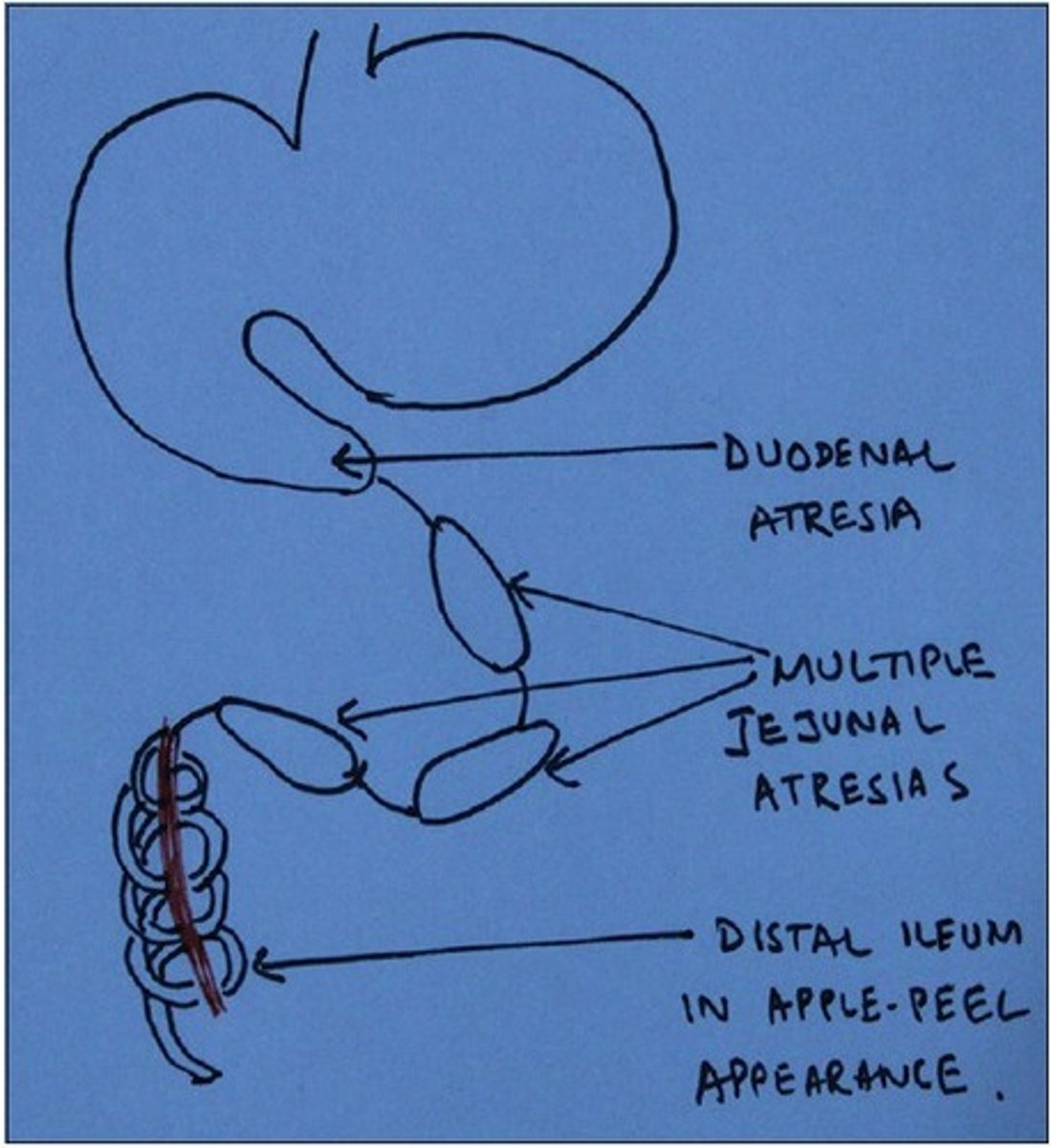
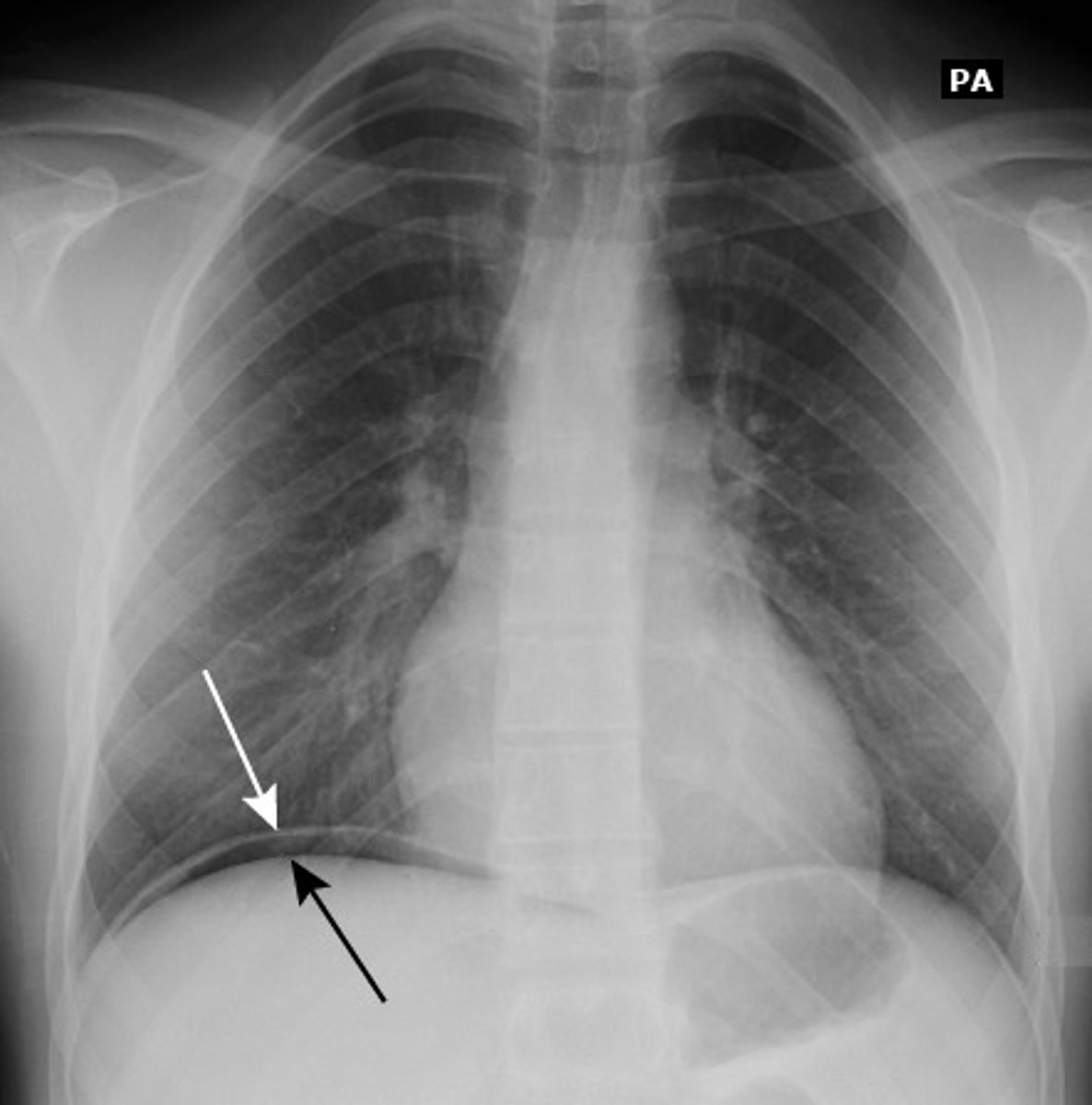
What are symptoms of intestinal atresia?
What causes duodenal atresia? What is the sign seen on x ray?
What causes jejunal and ileal atresia?
What are symptoms of intestinal atresia?
- presents with bilious vomiting and abdominal distention in first 1-2 days of life
.
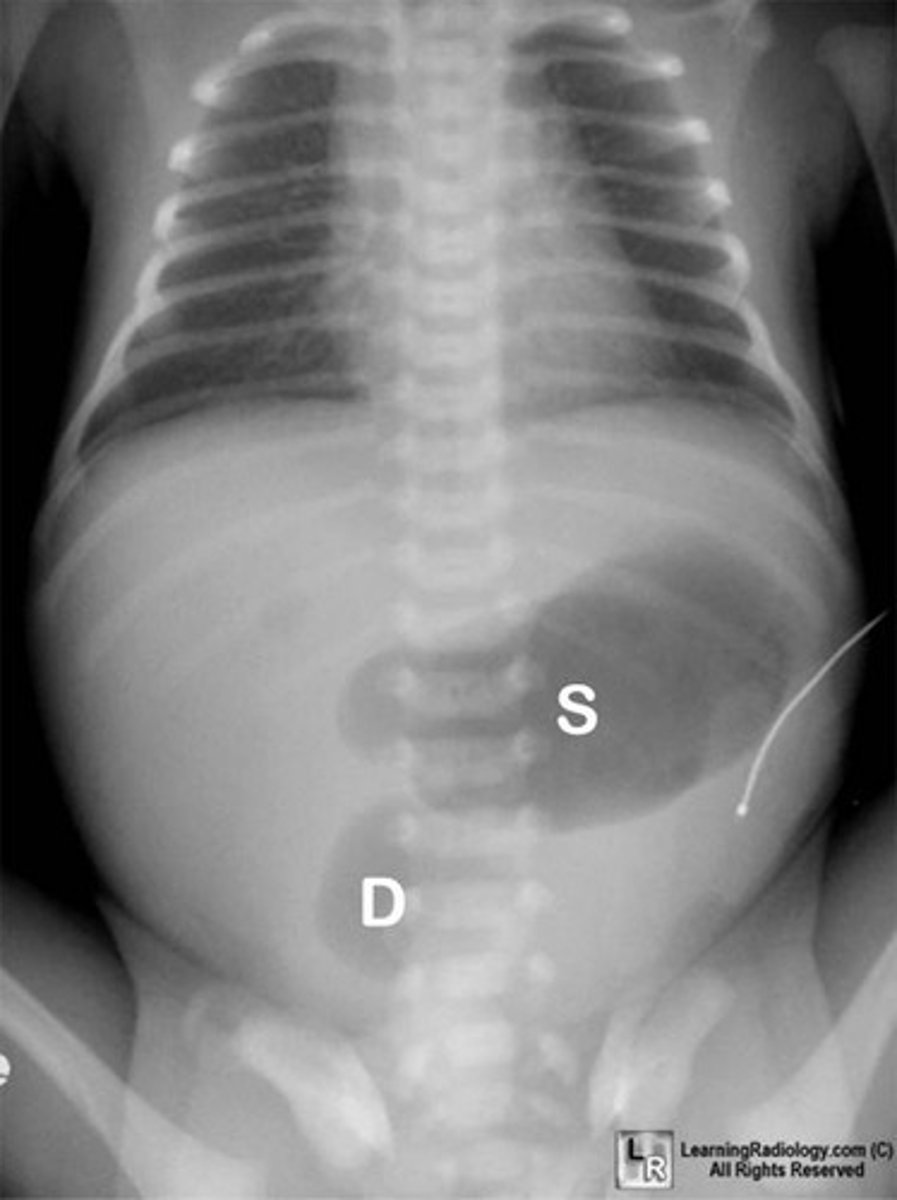
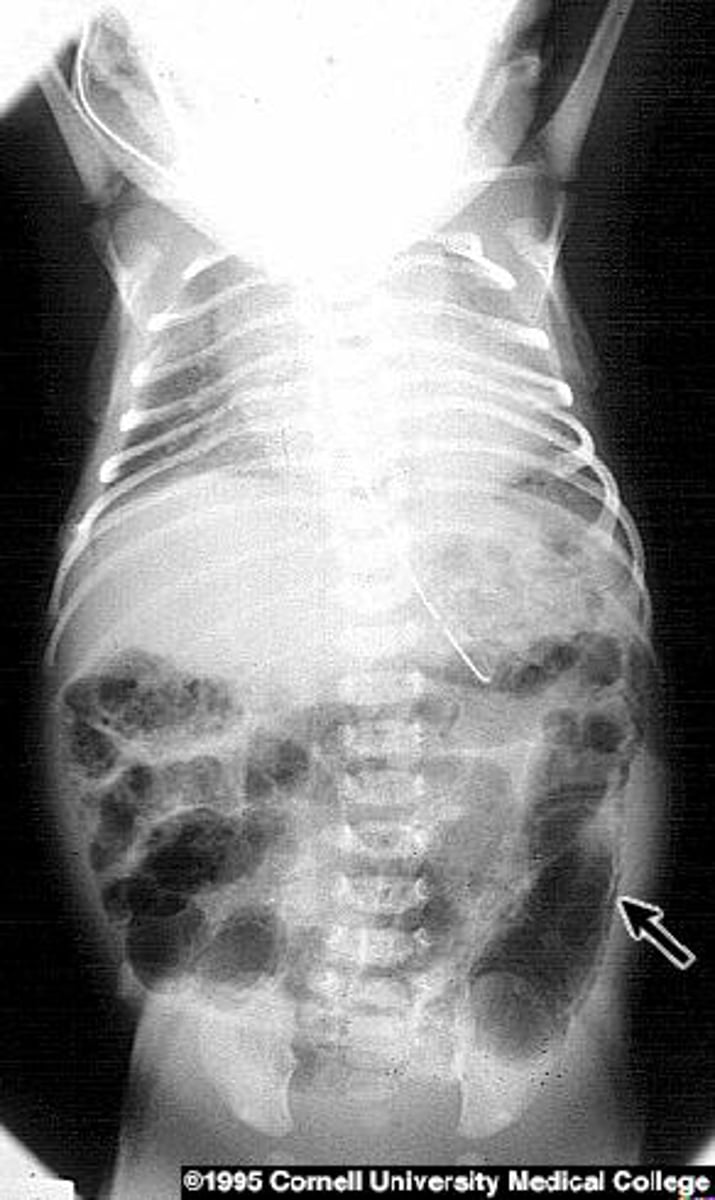
What causes duodenal atresia? What is the sign seen on x ray?
- failure to recanalize (become a hollow tube again)
- this results in dilation of proximal stomach and duodenum (called the double bubble sign)
- associated with down syndrome
.
What causes jejunal and ileal atresia?
- disruption of the mesenteric vessels resulting in ischemic necrosis leading to segmental resorption (bowl discontinuity or "apple peel")
What are symptoms of intestinal atresia?
What causes duodenal atresia? What is the sign seen on x ray?
What are symptoms of intestinal atresia?
- presents with bilious vomiting and abdominal distention in first 1-2 days of life
What causes duodenal atresia? What is the sign seen on x ray?
- failure to recanalize (become a hollow tube again)
- this results in dilation of proximal stomach and duodenum (called the double bubble sign)
- associated with down syndrome
Hypertrophic pyloric stenosis
What is it and how does it present?
Associated with exposure to what?
Epi?
Treatment?
What is it and how does it present?
- most common cause of gastric outlet obstruction in infants (1:600)
- results in a palpable "olive" mass in the epigastric region with *non-bilious projectile vomit at 2-6 weeks old)
- results in hypokalemic hypochloremic metabolic alkalosis (due to vomiting of gastric acid and subsequent volume contraction)
Associated with exposure to what?
- macrolide exposure
Epi?
- more common in firstborn males
Treatment?
- surgical incision (pyloromyotomy)
What are the layers of the digestive tract?
Where does an erosion extend to?
What about ulcers?
Where does an erosion extend to? What about ulcers?
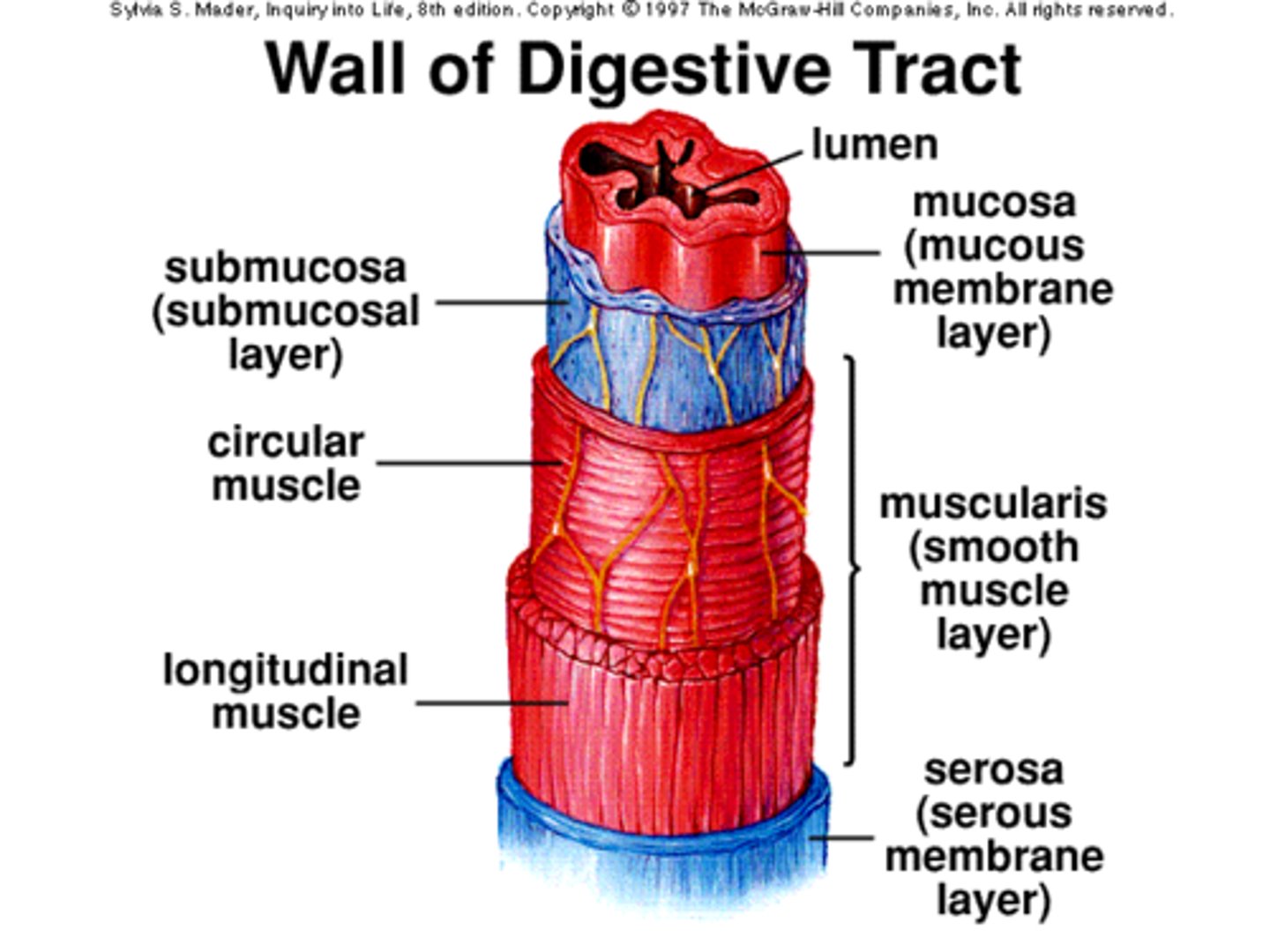
-erosions are in the mucosa ONLY
- uclers can extend into submucosa, inner or outer muscular layer
,
What are the layers of the digestive tract?
remember --> MSMS from inner to outer
Mucosa: epithelium, lamina propria, muscularis mucosa
Submucosa: submucosal nerve plexus (Meissner) and secretes fluid
Muscularis externa: includes the Myenteric nerve plexus (Auerbach), responsible for motility
Serosa when intraperitoneal, or adventita (when retroperitoneal)
What is the function of Peyer patches? Where are they primarily located?
What is the function of Peyer patches? Where are they primarily located?:
- aka gut-associated lymphoid tissues (GALT) are aggregates of lymphoid tissue located throughout the lamina propria and submucosa of the digestive tract
- act in immune function --> first line of defense against pathogens in the gut
- Peyer patches produce IgA in germinal centers of B cells located in the lamina propria
What is superior mesenteric artery syndrome?
What causes it? What conditions predispose to it?
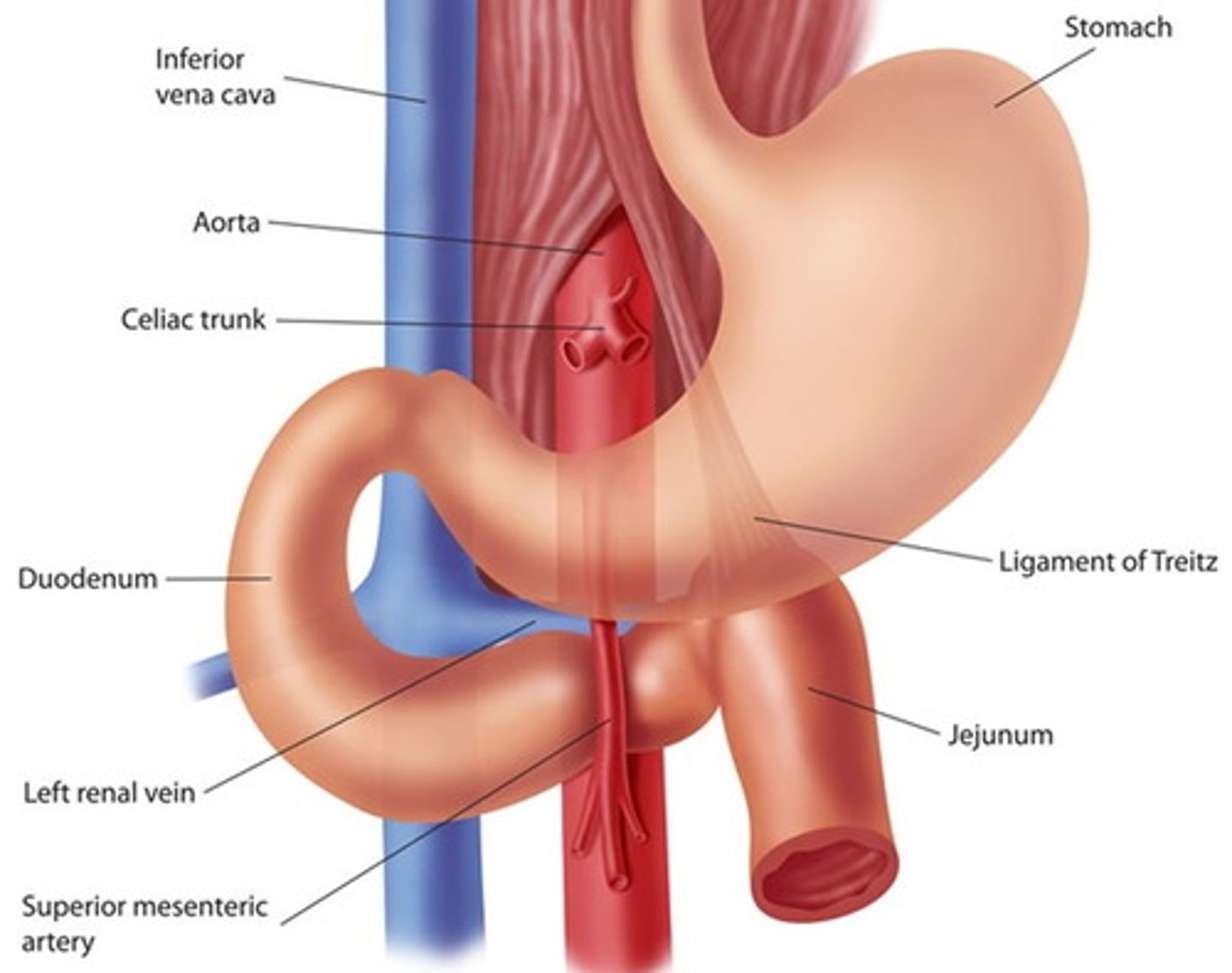
*What is superior mesenteric artery syndrome?
- intermittent intestinal obstruction symptoms-->post prandial pain
- compression of the transverse duodenum between the SMA and the aorta.
What causes it? What conditions predispose to it?
- conditions associated with diminished mesenteric fat (ie: low body weight/malnutrition).
What do anterior duodenal ulcers perforate?
Perforate into the anterior abdominal cavity-->pneumoperitoneum
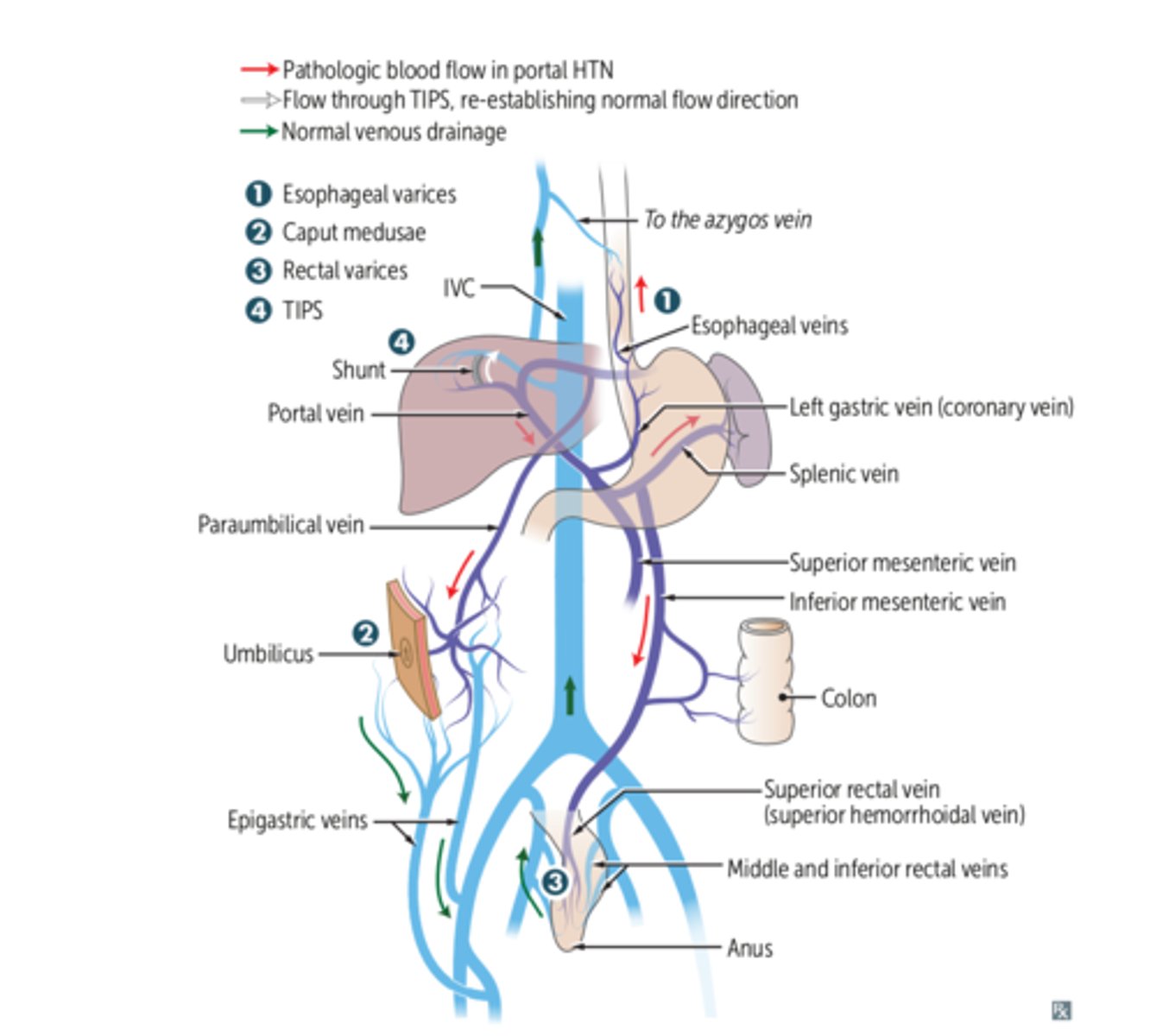
Compare and contrast internal vs external hemorrhoids:
Internal = above pectinate line = painless
External = below pectinate line = painful
What is the pectinate (dentate) line?
What is the pectinate (dentate) line?
- a line formed where endoderm (hindgut) meets ectoderm
What lies above the pectinate line?
- arterial supply?
- venous drainage?
- lymphatic drainage?
What lies above it?
- internal hemorrhoids
arterial supply: superior rectal artery (branch of IMA)
venous drainage: superior rectal vein --> inferior mesenteric vein --> portal system
- lymphatic drainage: to internal iliac lymph nodes
What lies below the pectinate line ?
- arterial supply?
- venous drainage?
- lymphatic drainage?
What lies below it?
- external hemorrhoids
- anal fissures
- squamous cell carcinoma
- arterial supply: inferior rectal artery (branch of internal pudendal)
-venous drainage: inferior rectal vein --> internal pudendal vein --> internal iliac vein --> common iliac vein --> IVC
- lymphatic drained to superficial inguinal nodes
What are anal fissures?
How do they present?
Risk factors/associations?
What are anal fissures?
- tear in the anal mucosa below the pectinate line
- tend to be located posteriorly because the area is poorly perfused
How do they present?
- pain while pooping
- blood on toilet paper
Risk factors/associations?
- associated with low fiber diets and constipation
What is Courvoisier sign?
Tumors that arise in the head of the pancreas (usually ductal adenoma) can cause obstruction of the common bile duct: enlarged GB with painless jaundice
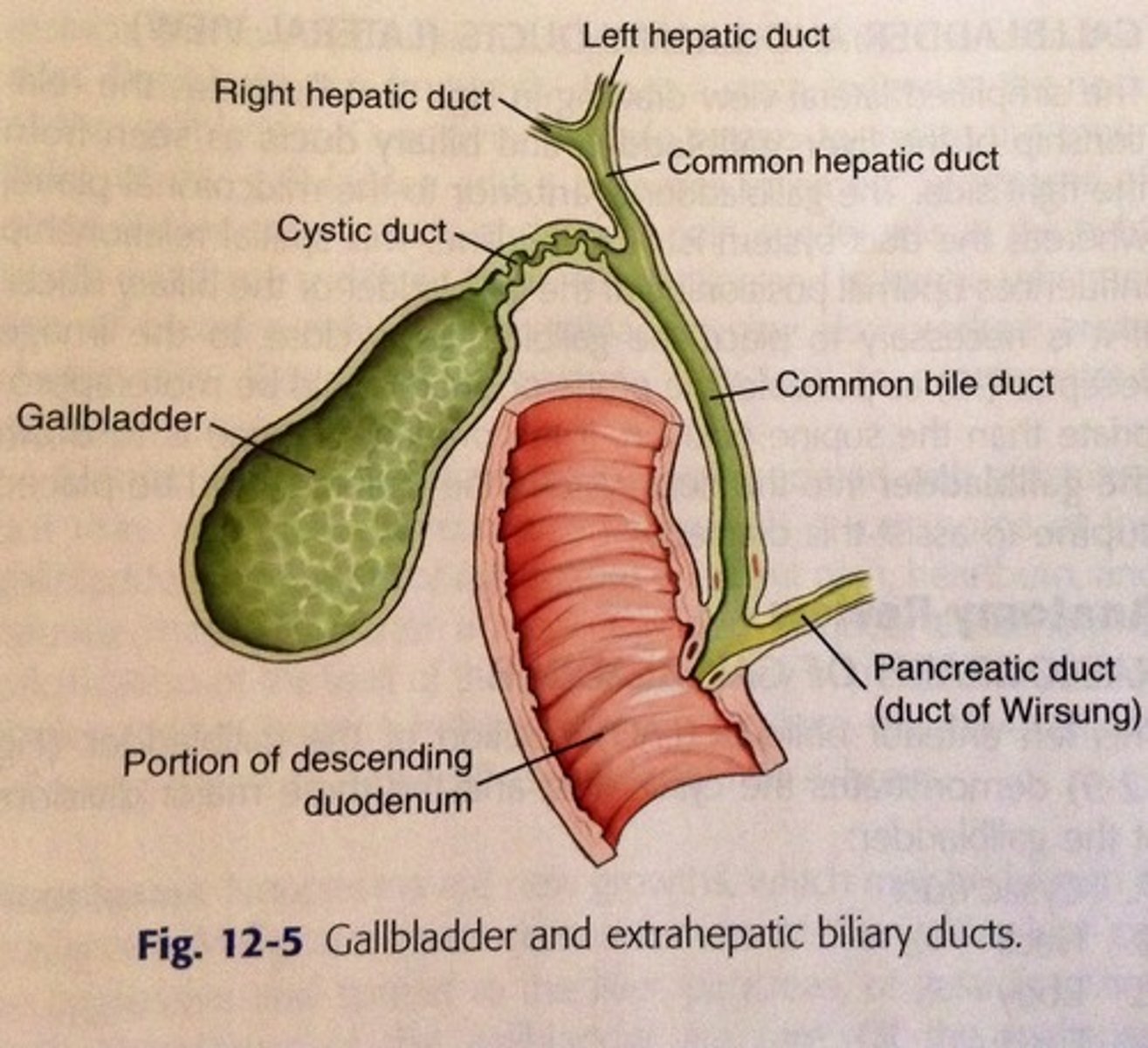
What regulates bile stored in the gallbladder?
1. Vagal stimulation via ACh
2. CCK: contraction and sphincter Oddi relaxation
What is a hernia?
Hernia:
- protrusion of peritoneum though an opening, usually at a site of weakness
- contents may be at risk for incarceration (meaning not reducible back into abdomen/pelvis) and strangulation
- complicated hernias can present with tenderness, erythema, fever
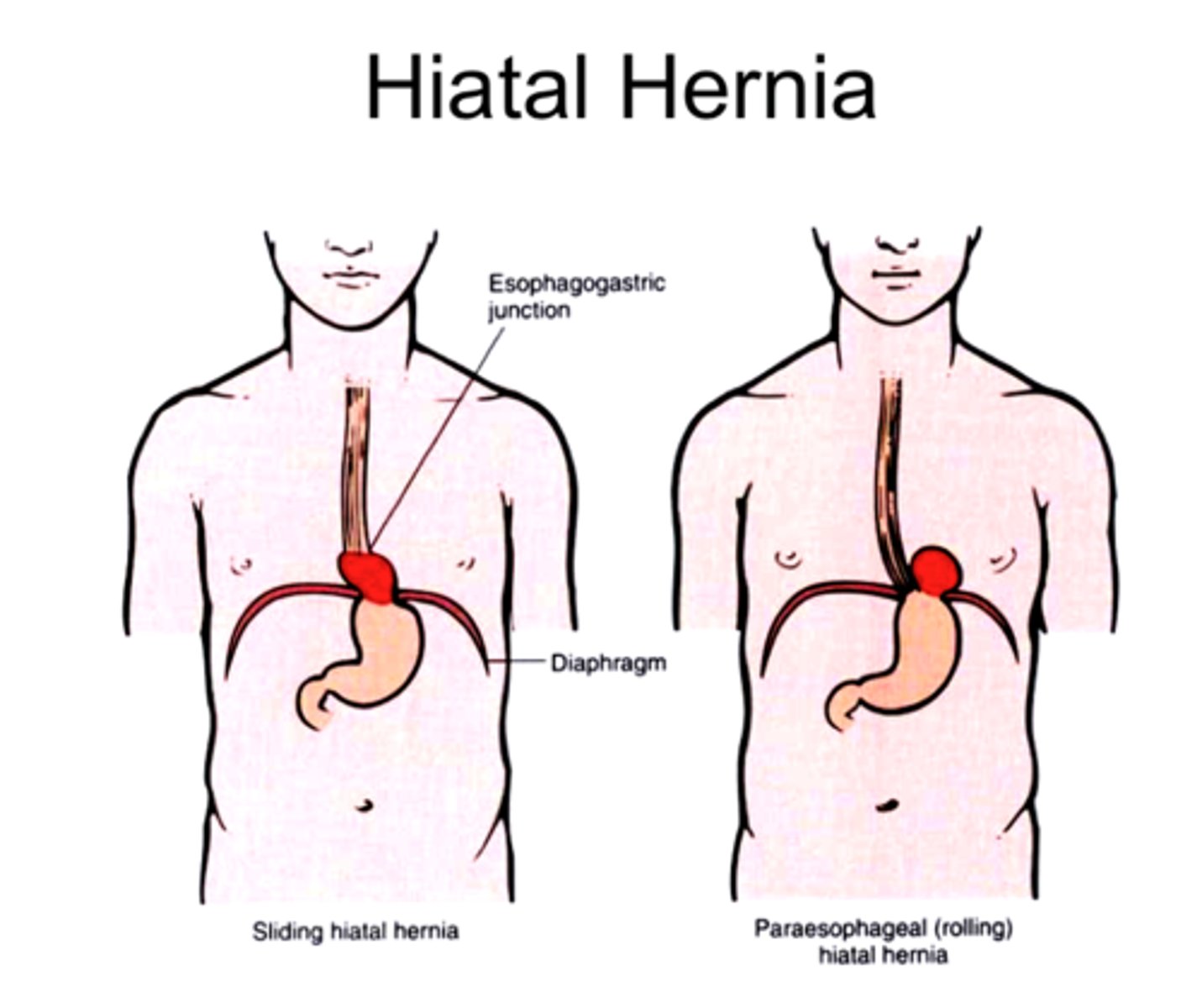
What is a diaphragmatic hernia?
Where does it happen most often?
What is a sliding hiatal hernia?
What is a paraesophageal hernia?
What is a diaphragmatic hernia?
- when an abdominal structure herniates into the thorax
- can occur from congenital defect or pleuroperitoneal membrane or as a result of trauma
- commonly occurs on the left side due to relative protection of right hemi-diaphragm by liver
- most commonly a hiatal hernia in which the stomach herniates upward through the esophageal hiatus of the diaphragm
What is a sliding hiatal hernia?
- most common
- when the gastroesophageal junction is displaced upward, resulting in a "hourglass stomach"
What is a paraesophageal hernia?
- gastroesopheal junction is usually normal
- when the fundus of the stomach protrudes into the thorax
-if congenital, can lead to pHTN and R-HF
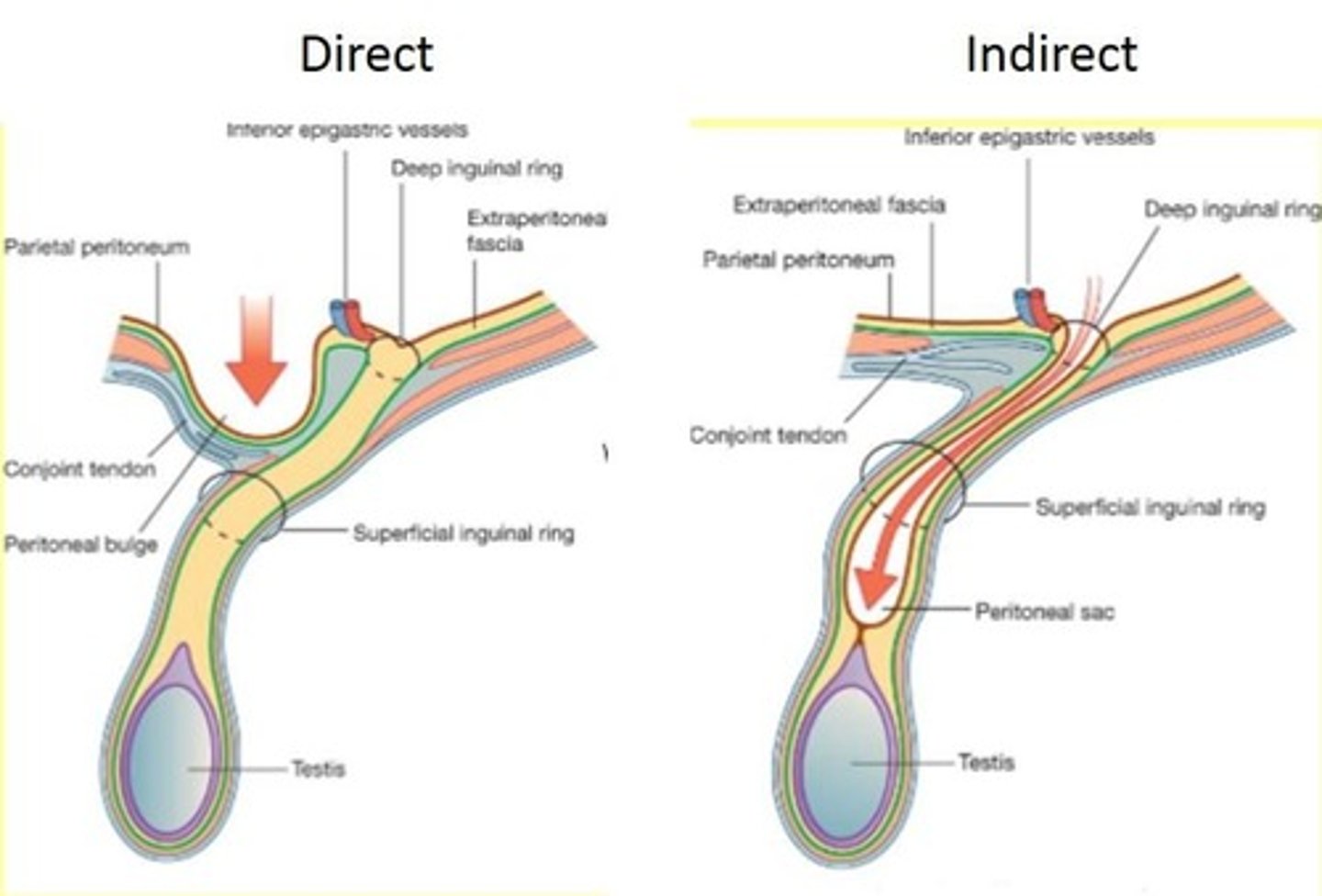
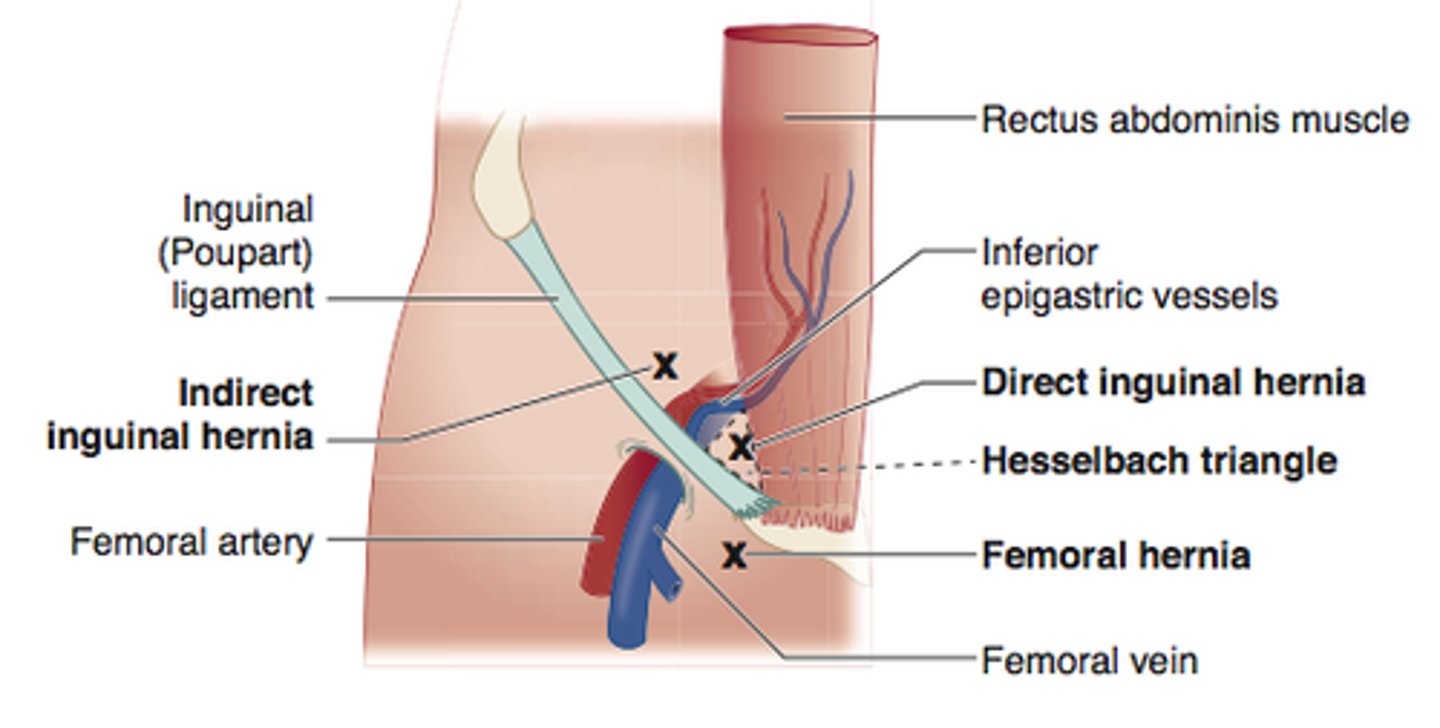
Where do indirect inguinal hernias occur?
Who does it occur in and why?
Where do do indirect inguinal hernia occur?
-through the INternal (deep) inguinal ring
- enters the internal inguinal ring lateral to the inferior epigastric vessels
Who does it occur in and why?
- occurs in INFANTS--> failure of the processus vaginalis to close
- much more common in males
- follows the path of descent of the testes
-covered by all 3 layers of the spermatic fascia
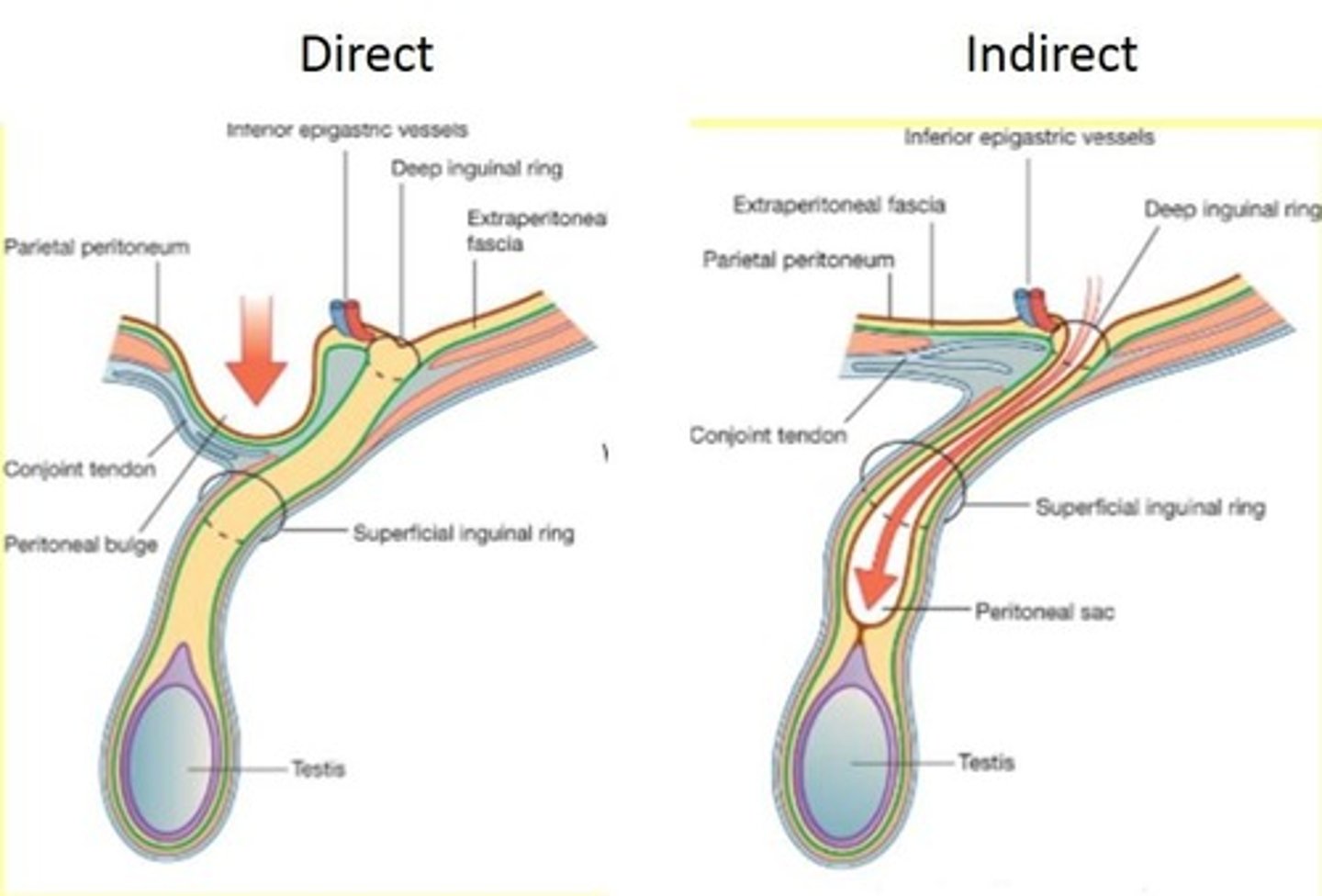
Where do direct inguinal hernias occur?
Where do direct hernias occur?
- through the INguinal (aka Hesselbach) triangle and through the external inguinal ring only
- covered by external spermatic fascia
- usually seen in only men-->acquired weakness in the transversals fascia
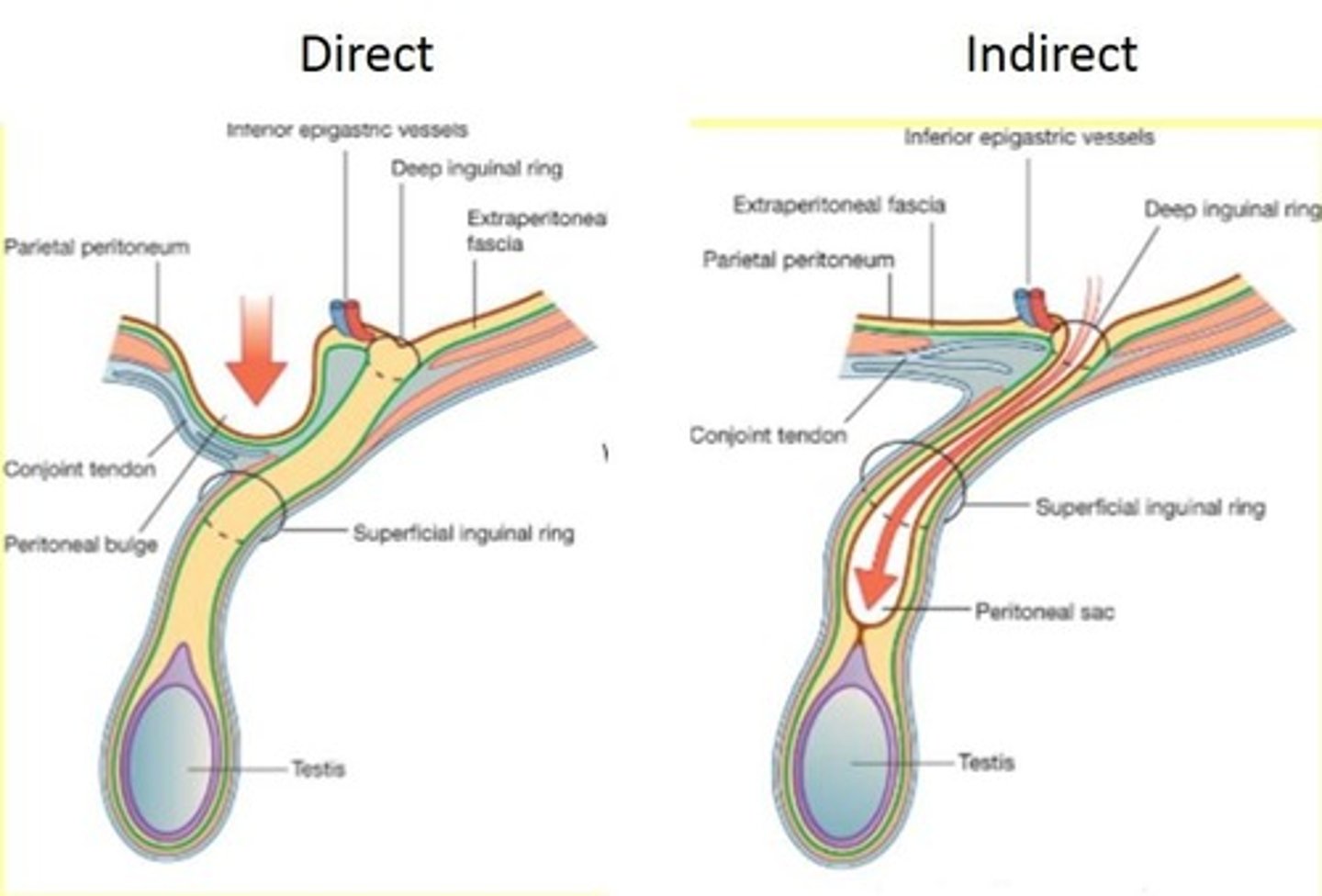
Define the borders of the INguinal triangle
Define the borders of the INguinal canal
The Inguinal aka Hesselbach Triangle:
1. inferior epigastric artery
2. rectus abdominis muscle
3. inguinal ligament
Define the borders of the INguinal canal:
boundaries include:
- deep inguinal ring: oval opening in the fascia transversalis lateral to the inferior epigastric vessels
- superficial inguinal ring: triangular defect in the aponeurosis of the external oblique muscle, lateral to the pubic tubercle
- anterior wall: aponeurosis of the external oblique muscle with some of the internal oblique aponeurosis laterally
- posterior wall: mainly transversalis fascia, with the conjoint tendon (falx inguinalis) medially
- roof: internal oblique and transverse abdominal muscles
- floor: inguinal and lacunar ligaments
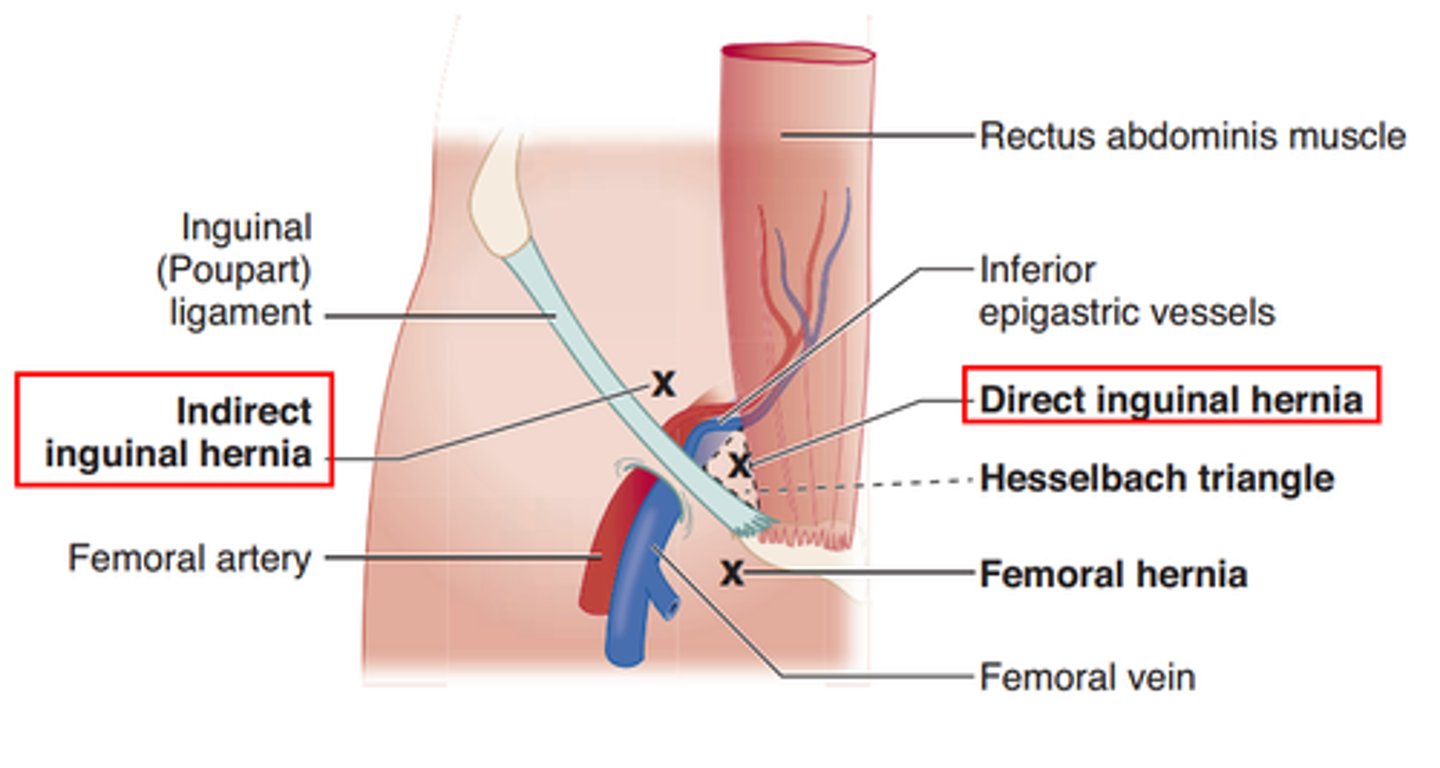
Mnemonic for distinguishing direct from indirect hernia
Remember: MDs dont LIe
Medial to the inferior epigastric vessels = Direct hernia
Lateral to the inferior epigastric vessels = Indirect hernia
Where do femoral hernias occur?
Who do they occur in?
Symptoms?
What is are the boundaries of the space through which femoral hernias occur?
Where do femoral hernias occur?
- protude below the inguinal ligmanet through the femoral canal below and lateral to the pubic tubercle
- more common in FEmales and on the right side
- note they are MORE likely to present with incarceration or strangulation than inguinal hernias because of how small the femoral ring is
Symptoms:
- upper thigh, groin or pelvic discomfort
What are the boundaries of the space through which femoral hernias occur?
- protrude through the femoral ring--> can widen and lax with age
-lateral to the pubic tubercle and lacunar ligament and medial to the femoral vein and artery
What is a VIPoma? What are the symptoms of a VIPoma?
VIPoma is a non-alpha, non-beta, islet cell pancreatic tumor that secretes BIP
Causes: *WDHA --> watery diarrhea, hypokalemia, achlorhydria)
Which hormones decrease gastric acid?
1. CCK (I cells)
2. Secretin (S-cells)
3. GIP (K-cells)
4. Somatostatin (D-cells)
What 3 things stimulate parietal cells?
1. Vagus--ACh
2. Histamine (ECL cell)
3. Gastrin (G-cell)
What inhibits the parietal cell?
1. Somatostatin
2. Prostaglandin
3. GIP
4. Secretin
What effect do prostaglandins (PGE1) have on stomach acid?
PGE1 allows for HCO3- production--protects the stomach
This is why NSAIDs increase ulcer risk
How are different types of carbohydrates absorbed in the gut?
What is the D-xylose absorption test used for?
How are different types of carbohydrates absorbed in the gut?
- only monosaccharides are absorbed by enterocytes
- examples of monosaccharides = glucose, galactose and fructose
Glucose and galactose:
- taken up by SGLT1 in a Na+ dependent fashion
Fructose:
- taken up by facilitated diffusion by GLUT-5
Note that ALL are transported to the blood by GLUT-2
What is the D-xylose absorption test used for?
- used to distinguish GI mucosal damage from other causes of malabsorption
What are Peyer's patches?
Where are they located?
What are they important for?
What are Peyer's patches?
- unencapsulated lymphoid tissue found in the lamina propria and submucosa of the ileum
- contain specialized M cells that sample and present antigen to immune cells
Where are they located?
- lamina propria and submucosa of the ileum
What are they important for?
- B cells stimulated in the germinal centers of Peyer's patches differentiate into IgA secreting plasma cells which ultimately reside in the lamina propria
- IgA receives protective secretory component and is then transported across the epithelium to the gut to deal with the intraluminal antigen
- SECRETORY IGA
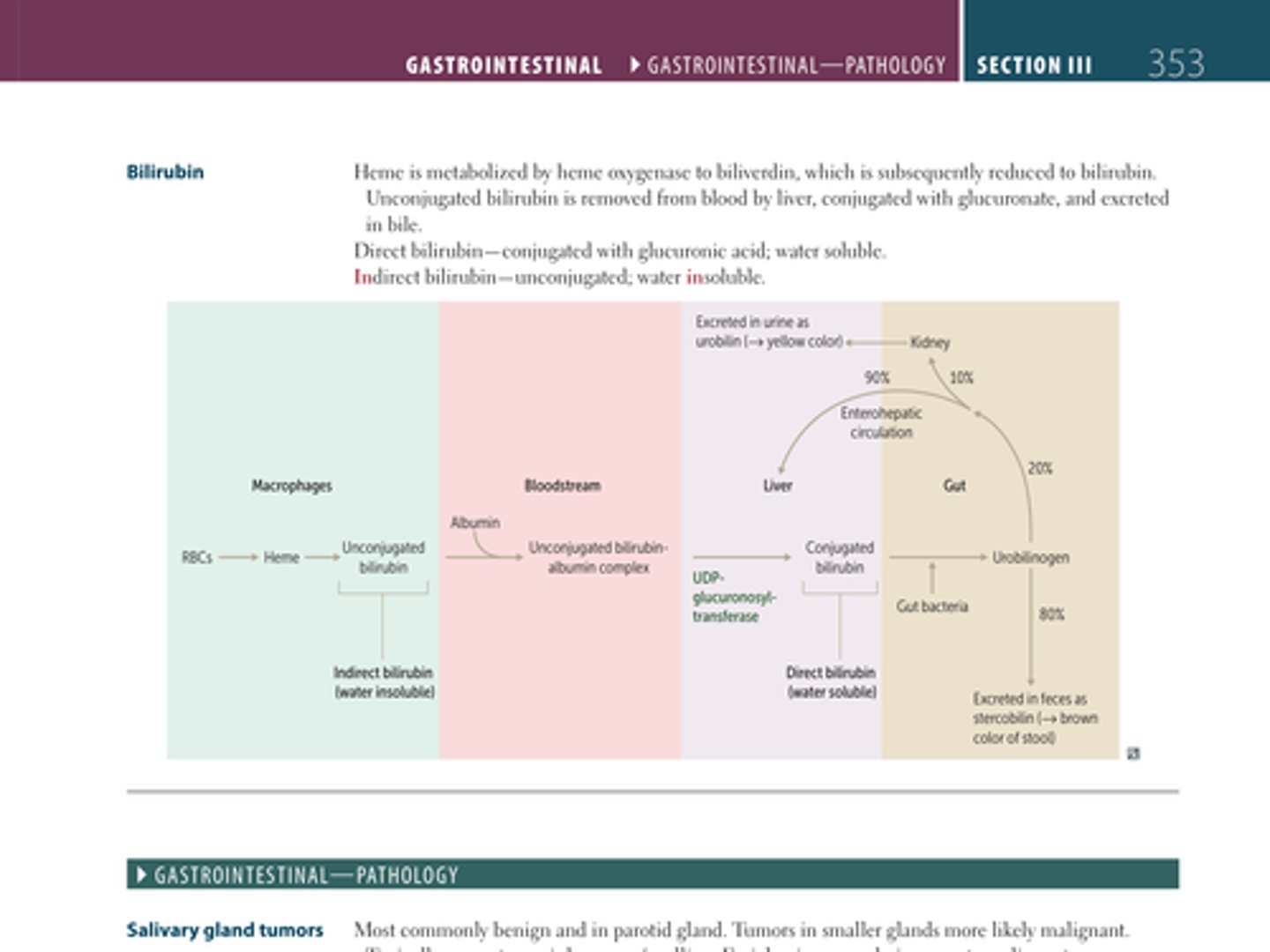
Walk through the breakdown/recycling of heme from RBCs to various products by location:
RBC
↓
Heme
↓ (heme oxygenase)
Biliverdin
↓
Unconjugated bilirubin
↓
Bound to albumin
↓ (UDPGT)
Conjugated Bilirubin
↓ (gut bacteria)
Urobilinogen
↓
excreted as feces (stercobilin
--OR--
Recycled back to liver
--OR--
Excreted in urin as urobilin
For the following salivary gland tumors, provide their commonality, and histological features:
Pleomorphic adenoma
Mucoepidermoid carcinoma
Warthin tumor
- salivary gland tumors are most commonly benign in the parotid gland
- tumors in smaller glands are more likely malignant
- typically present as a painless mass/swelling
- the presence of facial pain or paralysis suggests malignant involved of CN VII
Pleomorphic adenoma:
- benign mixed tumor
- most common salivary gland tumor
- made of chondromyxoid stroma and epithelium
- recurs if incompletely excised or ruptured inraoperatively
Mucoepidermoid carcinoma:
- most common malignant tumor
- has mucinous and squamous components
Warthin tumor:
- aka papillary cystadenoma lymphomatomsum
- benign cystic tumor with germinal centers
-SMOKERS
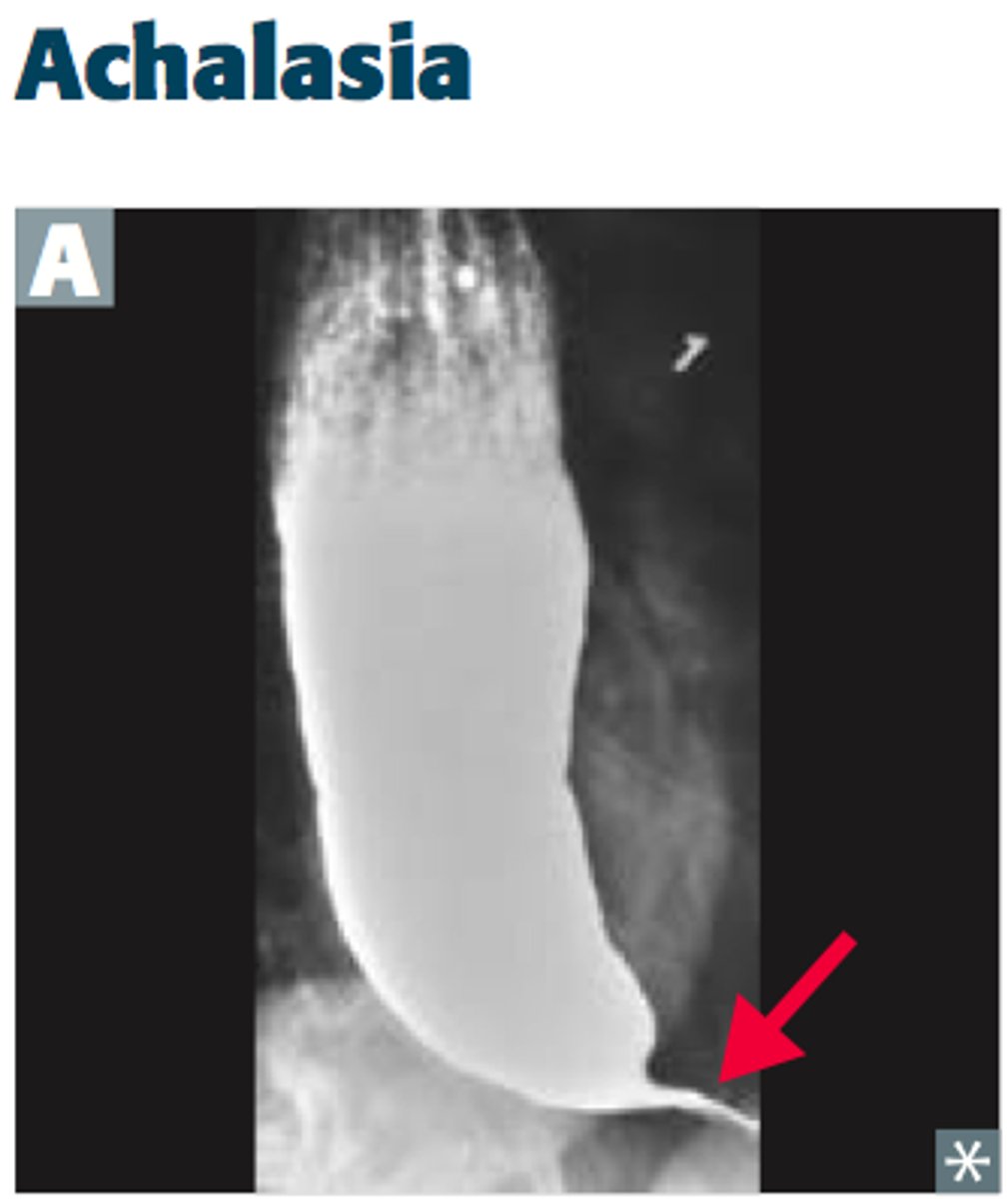
What is achalasia, provide the pathophysiology
What are the classic findings on barium swallow?
Achalasia increases risk for what cancer?
What are 1mary vs 2ndary causes of achalasia?
What is achalasia, provide the pathophysiology:
- achalasia MEANS "failure to relax"
- must have aperistalsis and failure of relaxation of the LES due to LOSS of Auerbach (myenteric) plexus
- there is a progressive dysphagia for liquids than liquids + solids
What are the classic findings on barium swallow?
- dilated esophagus with area of distal stenosis (bird beak sign)
Achalasia increases risk for what cancer?
- increases risk of esophageal cancer, esp squamous cell carcinoma
What are 1mary vs 2ndary causes of achalasia?
- primary: failed ganglion cell migration
- 2ndary: T. Cruzi infection or extra-esophageal malignancies (mass effect, paraneoplastic)
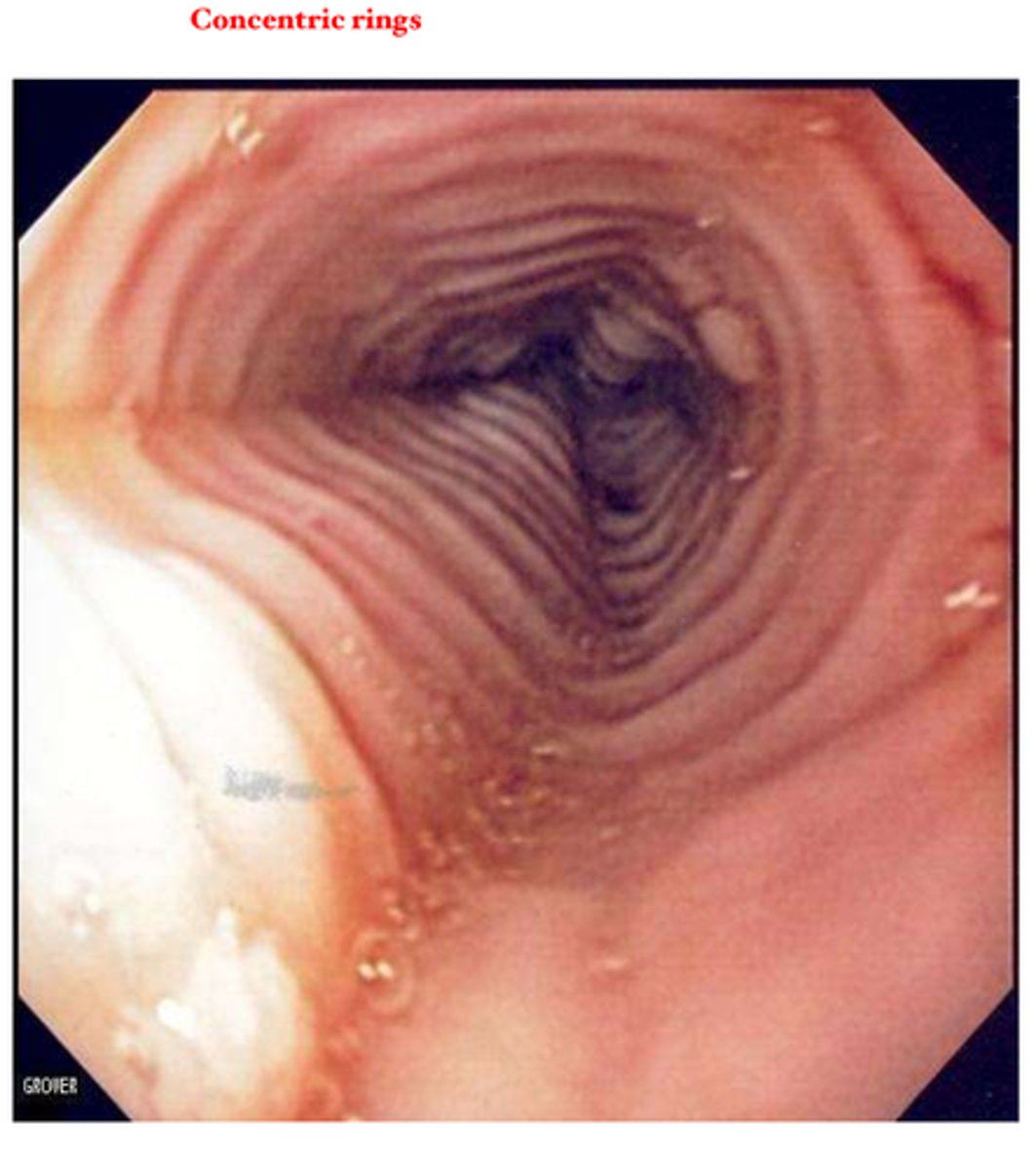
Eosinophilic esophagitis
- pathophys?
- endoscopy findings?
- rx?
- infiltration of eosinophils in the esophagus often in ATOPIC patients
- exposure to food allergens results in dysphagia and food impaction
- esophageal RINGS and linear furrows often seen on endoscopy ("feline esophagus")
- UNresponive to GERD therapy
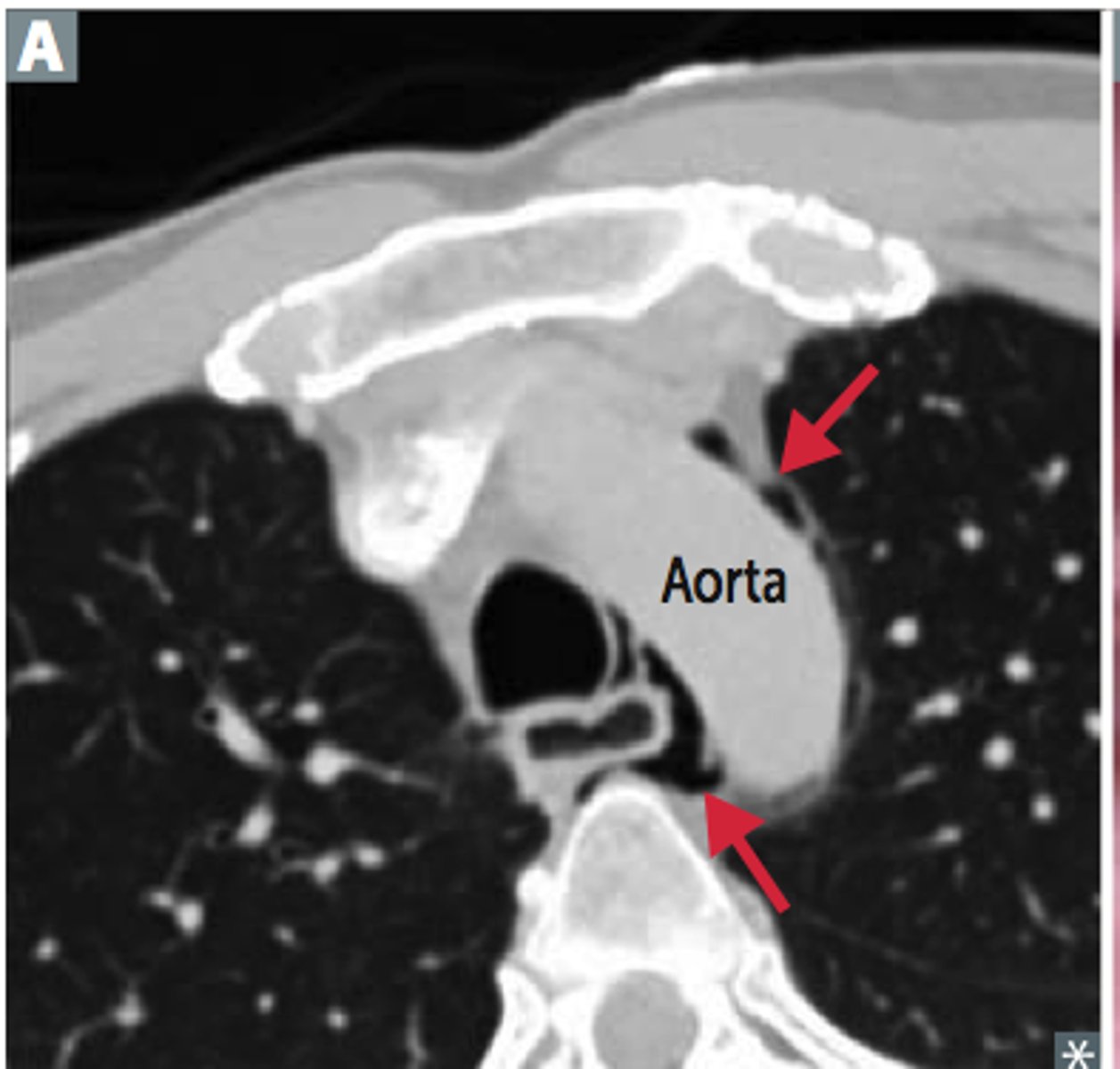
Boerhaave syndrome
- extent of injury?
- radiographic findings?
- rx?
- transmural
- usually distal esophageal rupture with pneumomediastinum due to violent retching (alcoholics)
-subcutaneous emphysema
- surgical emergency
Esophageal stritures
- narrowing of esophageal lumen, often due to caustic ingestion or acid reflux
Esophageal varices
what are they?
epidemiology?
rx? (ppx vs active bleed)
- dilates submucosal veins in the lower 1/3 of the esophagus, due to portal hypertension
- located at the anastomosis of the left gastric vein and the esophageal vein
CIRRHOTICS (alcoholics)
- may be source of life-threatening hemorrhage
Tx:
- beta-blockers
- vasopressin, somatotstatin, endoscopy (band ligation, slcerotherapy), TIPS
Esophagitis:
- causes (include the various infectious causes and unique presentations for each)
- inflammation of the esophagus
candida --> white pseudomembrane
HSV-1 --> punched out ulcers
CMV --> linear ulcers
caustic ingestion
medications
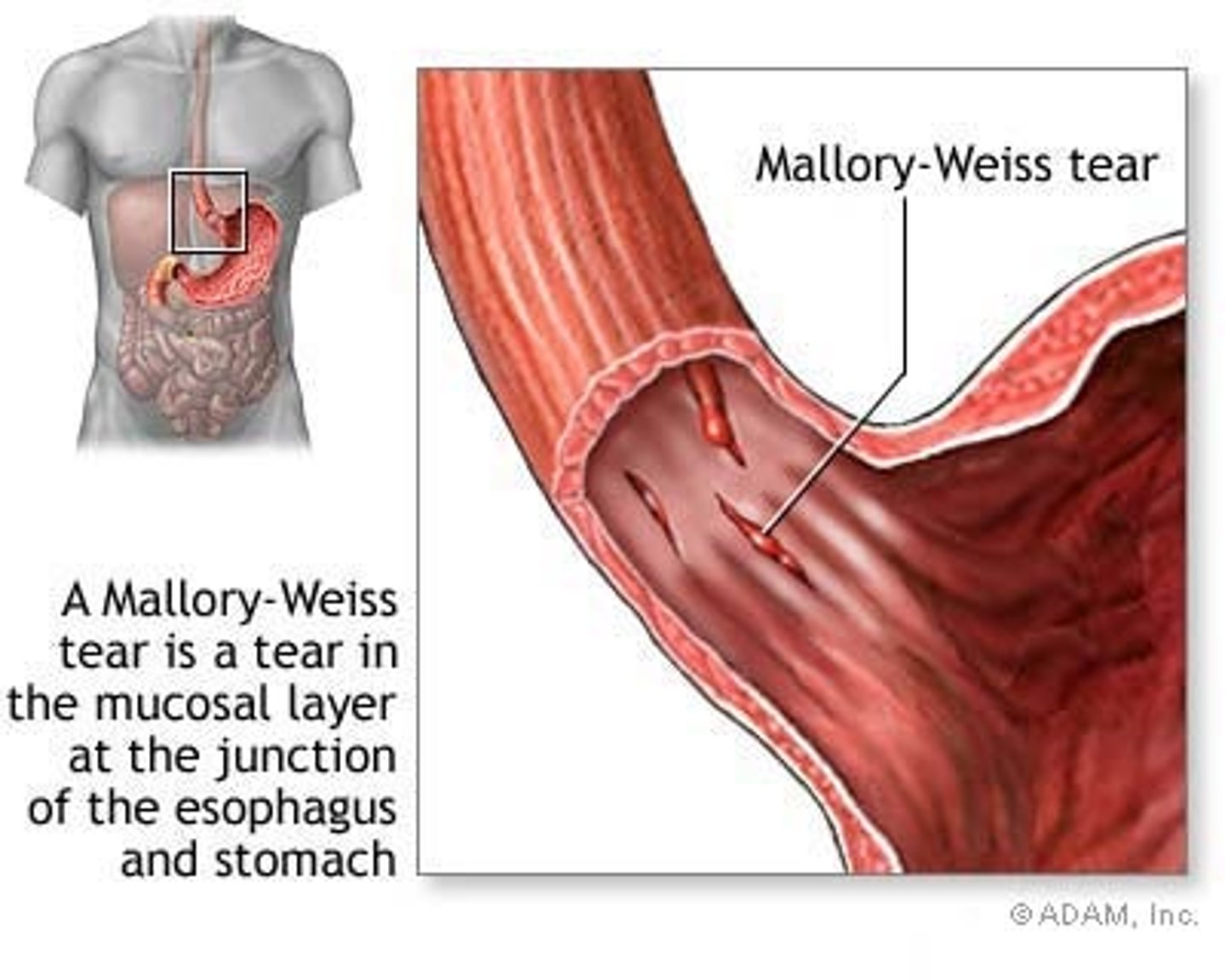
Mallory-Weiss Syndrome
extent of injury and cause?
epidemiology:
extent of injury and cause?
- mucosal lacerations at the G-E junction due to severe vomiting
-metabolic alkalosis from vomitting
- lead to hematemesis that can be painful
- accounts for 5-10% upper GI bleeds
epidemiology:
- usually seen in alcoholics and bulimics
GERD
presentation
association
pathophys
histology:
presentation:
- heartburn, regurgitation, dysphagia
- globus sensation (lump in throat)
- chronic cough, hoarseness (laryngopharyngeal reflux)
association:
- with asthma
pathophys:
- transient decrease in LES tone or increased stomach pressure (ie: hiatal hernia, pregnancy, fat)
histology: triad of mucosal findings is key to diagnosis
- eosinophils (or neutrophils)
- basal zone hyperplasia
- elongation of lamina propria papillae
RF: obesity, alcohol, tobacco, fatty diet, caffeine, hiatal hernia
Plummer-Vinson Syndrome
symptoms:
cause:
cancer risk:
symptoms:
remember PLUMBERS DIE, thus a triad of
- Dysphagia
- Iron deficiency anemia
- Esophageal webs
- may be associated with glossitis
cancer risk:
- increased risk of esophageal squamous cell carcinoma

Sclerodermal esophageal dysmotility:
pathophysiology:
relationship to scleroderma:
Sclerodermal esophageal dysmotility:
- esophageal smooth muscle atrophy --> decreased LES pressure and dysmotility --> acid reflux and dysphagia --> stricture, Barrett esophagus and aspiration
relationship to scleroderma:
- part of the CREST syndrome in limited scleroderma
C: calcinosis
R: raynaulds
E: esophageal dysmotility
S: sclerodactyly
T: telangiectasias
How would you distinguish Mallory-Weiss from Esophageal Varices?
M-W: painFUL hematemesis
Varices: painLESS hematemesis
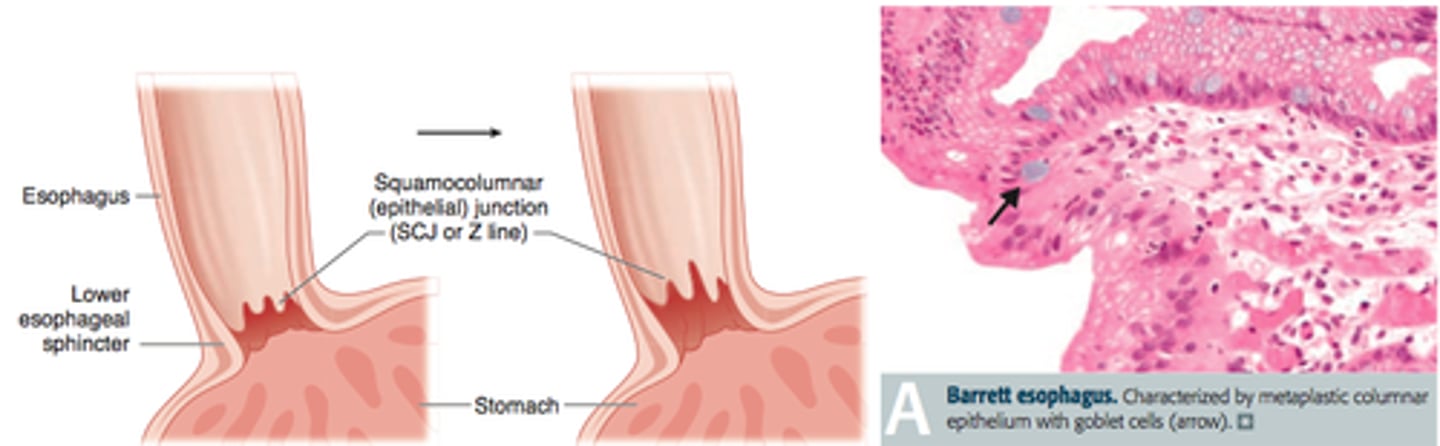
Barrett Esophagus
pathophysiology:
cause:
pathophysiology:
- precancerous lesion of the distal esophagus
- non-keratinized stratified squamous epithelium with non ciliated columnar with goblet cells (note: goblet cells stain blue due to their mucin)
cause:
- long standing GERD
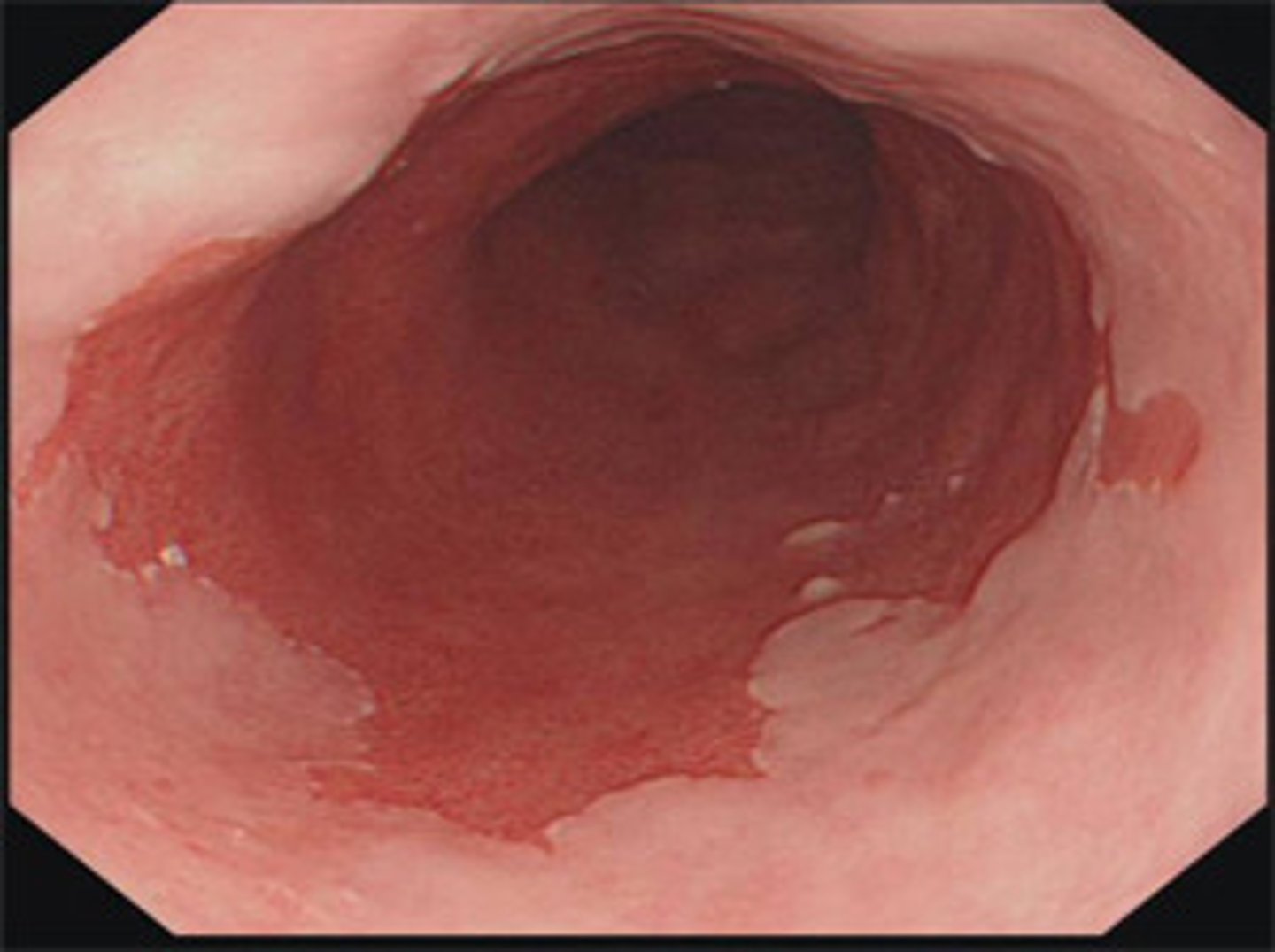
Barrett Esophagus
findings on endoscopy, biopsy:
- endoscopy: red, velvety GI mucosa extending upward from the GE junction in contrast to the normal pink mucosa of the esophagus
- biopsy: intestinal type goblet cells in the columnar mucosa of the esophagus
Esophageal cancers:
- presentation
- squamous cells vs adenocarcinoma
presentation:
-presents LATE
- progressive dysphagia, first solids then liquids
- weight loss
- overall, poor prognosis
Squamous cell carcinoma:
- affects upper 2/3 of esophagus
- risk factors: alcohol, hot liquids, caustic strictures, smoking, achalasia
- more common worldwide
-blacks
Adenocarcinoma:
- lower 1/3 of esophagus
- RF: chronic GERD, Barrett esophagus, obesity, smoking, achalasia
- more common in America
-whites
AdenoCA
bArrett's
America
If a patient has esophageal cancer, which lymph nodes will it metastasize to?
1. Upper 1/3-->Cervical nodes
2. Middle 1/3-->Mediastinal/trachobronchial nodes
3. Lower 1/3--> celiac/gastric nodes
What is gastritis? What are the two subdivisions of it?
What are the causes of chronic gastritis?
What is gastritis? What are the two subdivisions of it?
- inflammation of gastric mucosa: acute or chronic
What are the causes of acute gastritis?
What are the causes of acute gastritis?
- transient mucosa damage with mucosal edema and inflammation
- injury can erode the mucosa and affect the underlying epithelium
Acute gastritis: inflammation, erosion, ulceration
causes of erosions include:
1. NSAIDS --> decreased PGE2 --> loss of gastric mucosa protection
2. Curling ulcers --> severe burns reduce plasma volume leading to ischemia and necrosis of the gastric mucosa
Curling irons burn!
3. Cushing ulcers --> increased ICP from injury =stimulation of the vagus nerve--> increased gastrin secretion and H+ =gastric mucosal injury
CUSHion the brain!
What are the causes of chronic gastritis?
What are the causes of chronic gastritis?
- caused by continuous inflammation of the gastric mucosa leading to atrophy (hypochlorhydria --> hyperstrinemia) and intestinal metaplasia (increased risk of gastric cancers)
Type A = autoimmune-->body/fundus
autoantibodies against parietal cells and IF
- increased risk of pernicious anemia and gastric adenoCA
Type B = H. pylori-->antrum
- most common
- H. pylori infection
- increased risk of PUD and MALT lymphoma
What is Menetrier disease?
Relevant findings?
Hyperplasia of mucosa --> hypertrophied rugae =excess mucus production, protein loss, parietal cell atrophy with decreased acid production.
↑# mucus cells
Considered precancerous
Relevant findings:
hypoproteinemia
*atrophy of partietal cells --> achlorhydria
What is the treatment of H. Pylori?
Triple Therapy
1. PPI
2. Clarithromycin
3. Amoxicillin or Metronidazole
What is Leser-Trelat sign? What disease is it observed in?
Leser-Trelat sign is multiple outcroppings of seborrheic keratosis seen in patients with gastric cancer

Gastric Cancer:
What is the most common type?
Presentation and findings?
What is the most common type?
- most commonly gastric adenocarcinoma > lymphoma > GI stromal tumor > carcinoid (rare)
- often has early, aggressive local spread with node/liver mets
Presentation and findings?
- presents late often, with weight loss, early satiety
- *acanthosis nigricans
- Leser-Trelat sign --> multiple outcroppings of seborrheic keratosis
- Sister Mary Joseph sign --> metastatic mass protruding into the umbilicus producing a bulging palpable nodule
Intestinal vs. diffuse gastric cancer
INTESTINAL:
- due to intestinal metaplasia of gastric mucosal cells: looks like ulcer with raised margins
- ulcerative lesions in antrum with raised margins
- associated with H pylroia, dietary nitrosamines (smoked foods), tobacco, achlorjydria, chronic gastritis
DIFFUSE:
- NOT H pylori associated
- signet ring cells --> mucin filled with peripheral nuclei
- stomach is diffusely thickened and leathery --> LINITIS PLASTICA
Risks for Intestinal vs Diffuse Gastric Cancer
Intestinal:
1. Intestinal metaplasia (H.pylori, autoimmune gastritis)
2. Smoked foods
3. Blood Type A
Diffuse
1. NOT ASSOCIATED WITH ANY OF THE ABOVE
What are the associated metastatic findings that can be associated with Gastric Cancer?
1. Virchow Node: involvement of left supraclavicular node by mets from the stomach
2. Krukenburg tumor: bilateral mets to ovaries. Abundant mucin-secreting signet ring cells
3. Sister Mary Joseph Nodule: subQ periumbilical mets
What is the general pathophysiology behind peptic ulcer disease?
Compare and contrast GASTRIC ULCERS vs DUODENAL ULCERS in terms of:
- pain
- H pylori
- mechanism of injury
- other causes
- risk of carcinoma
- other
What is the general pathophysiology behind peptic ulcer disease?
- gastric mucosal cells secrete mucus with large quantities of BICARB in order to maintain a pH of 6-7 around the gastric epithelial cells (as opposed to 1-2 in the gastric lumen)
- mucus layer breachd=epithelial injury occurs and ULCERS can form
- presents as burning, gnawing, epigastric pain
Compare and contrast GASTRIC ULCERS vs DUODENAL ULCERS in terms of:
GASTRIC ULCERS:
pain: Greater with meals = weight loss
H pylori: 70%
mechanism of injury: in antral/prepyloric regions, loss of mucosal protection
other causes: NSAIDS
risk of carcinoma: INCREASED
other: biopsy to rule out malignancy
DUODENAL ULCERS:
pain: Decreases with meals = weight gain
H pylori: 90%
mechanism of injury: >90% in first part of duodenum. loss of mucosal protection or increased acid
other causes: Zollinger-Ellison syndrome
risk of carcinoma: generally benign
other: hypertrophy of Brunner glands
RX: triple therapy with 2 abx (amoxicillin and clarithromycin + omeprazole)
What are the general symptoms of malabsorption syndromes?
How can you screen for it?
What are the general symptoms of malabsorption syndromes?
- diarrhea
- steatorrhea (loose, floating)
- weight loss
- weakness
- vitamin and mineral deficiencies
How can you screen for it?
- fecal fat screen (Sudan stain)
What are the 3 complications of ulcers?
1. Hemorrhage:
- gastric > duodenal (posterior > anterior)
- most common complication
- rupture of gastric ulcer on lesser curvature of stomach--> bleeding from left gastric artery
- rupture of ulcer on posterior wall of duodenum --> bleeding from gastroduodenal artery
2. Obstruction:
- at the pyloric channel
3. Perforation:
- duodenal (anterior > posterior)
- free air under the diaphragm with referred pain to the shoulder via the phrenic nerve
What is dermatitis herpetiformis? What disease is it associated with?
Pruritic, excoriated grouped vesicles on the knees, buttocks, elbows and posterior scalp.
Associated with celiac sprue

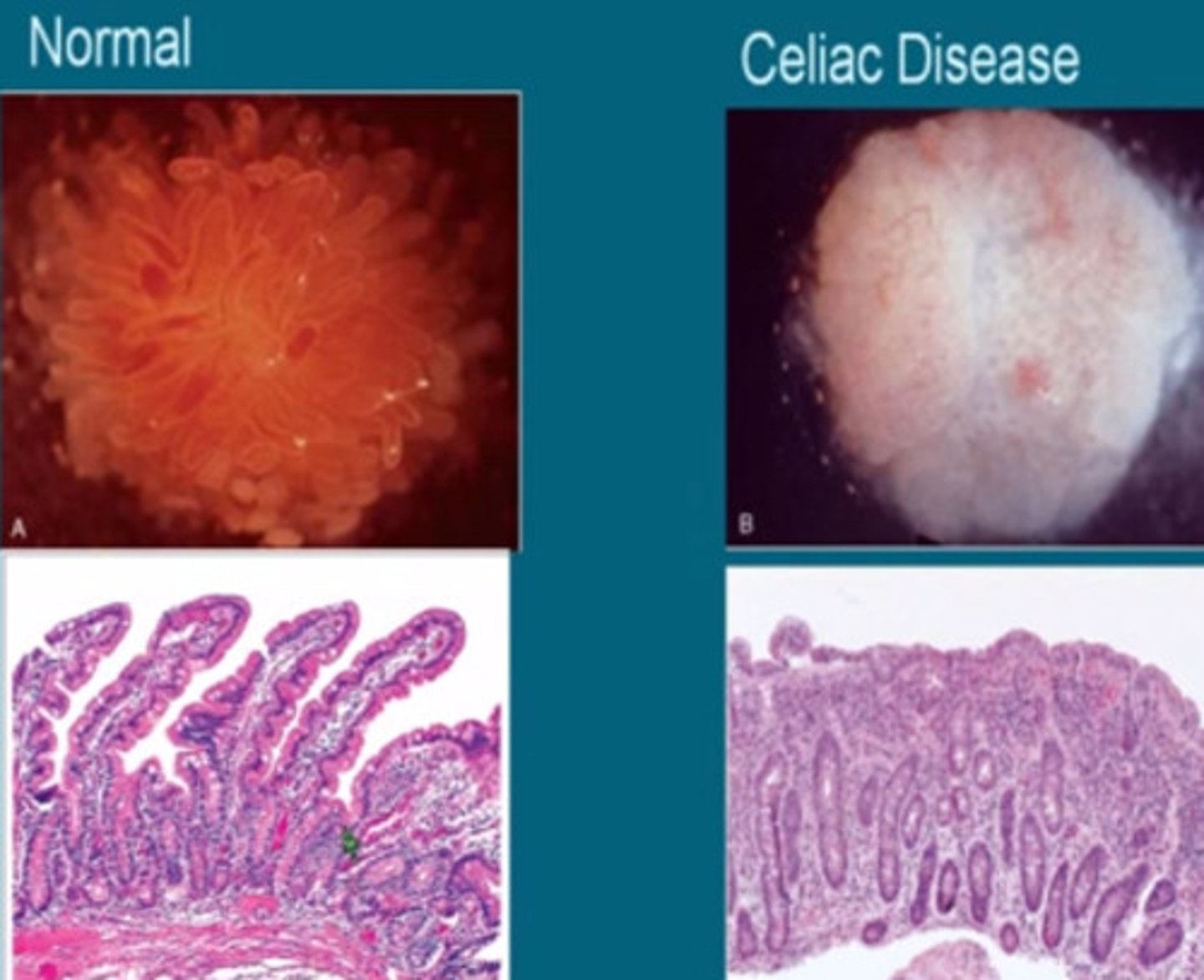
Celiac disease:
what is it
which HLA
LABS
histo
- malabsorption syndrome due to gluten-sensitive enteropathy (aka celiac sprue)
-autoimmune intolerance of gliadin =malabsorption and steathorrhea
- HLA-DQ2, HLA-DQ8
- northern european descent
- dermatitis herpetiformis
- decreased bone density
Labs: IgA Aby against
1. endomysium
2. tTG
3. Gliadin
4. can be IgG if IgA deficient
Histo:
1. villous flattening
2. crypt hyperplasia
3. intraepithelial lymphocytosis
Tx: gluten free diet
note that:
- decreased mucosal absorption primarily affects the distal duodenum and/or proximal jejunum
Celiac Disease increases the risk for what?
Small bowel cancer
T-Cell lymphoma (EATL)
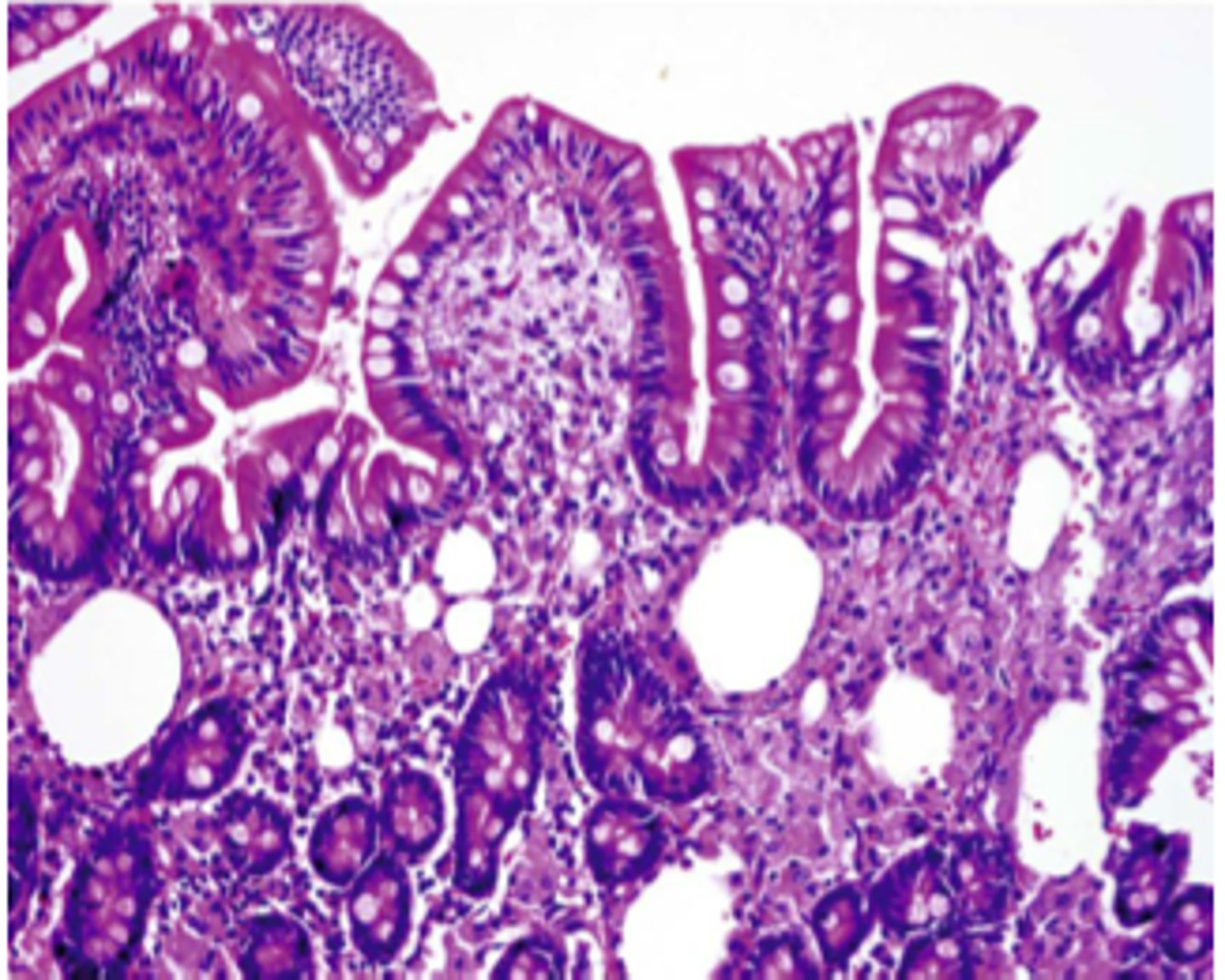
Lactose intolerance
- loss of lactase by genetics or other MOA
- lactase located at brush border tips of villi that breaks down lactose into galactose and glucose
histology/findings?
- normal appearing villi except when 2° inury at tips of villi (ie viral enteritis)
- OSMOTIC diarrhea with ↓ stool pH (due to the fermentation of lactose by colonic bacteria)
- lactose hydrogen breath test--> is POSITIVE for lactose malabsorption if post-lactose breath hydrogen value rises > 20 ppm compared with baseline
Pancreatic insufficiency
- malabsorption syndrome caused by chronic pancreatitis, cystic fibrosis, obstructing cancer
- causes malabsorption of fat and fat-soluble vitamins (ADEK) as well as vitamin B12
histology/findings?
- decreased duodenal pH (bicarbonate) and fecal elastase
Tropical sprue
- similar to celiac sprue (affects small bowel) but responds to antibiotics
pathophysiology?
- unknown but seen in tropics
- results in decreased mucosal absorption affecting the duodenum and jejunum but can involve the ileum with time
- associated with megaloblastic anemia due to FOLATE deficiency and later, B12 deficiency
Which sprue affects the Duodenum more? Which sprue affects the I/J more?
Duodenum: Celiac Sprue
I/J: Tropical Sprue
Whipple Disease
Foamy Whipped Cream in a CAN*
- foamy macrophages
- Whipple
- Cardiac, Arthralgias, Neurologic
.
- infection with Tropheryma whipplei (intracellular)
gram+
PAS+
symptoms?
- Cardiac symptoms
- Arthralgias
- Neurologic symptoms
histology/findings?
- + PAS
- foamy macrophages in the intestinal lamina propria
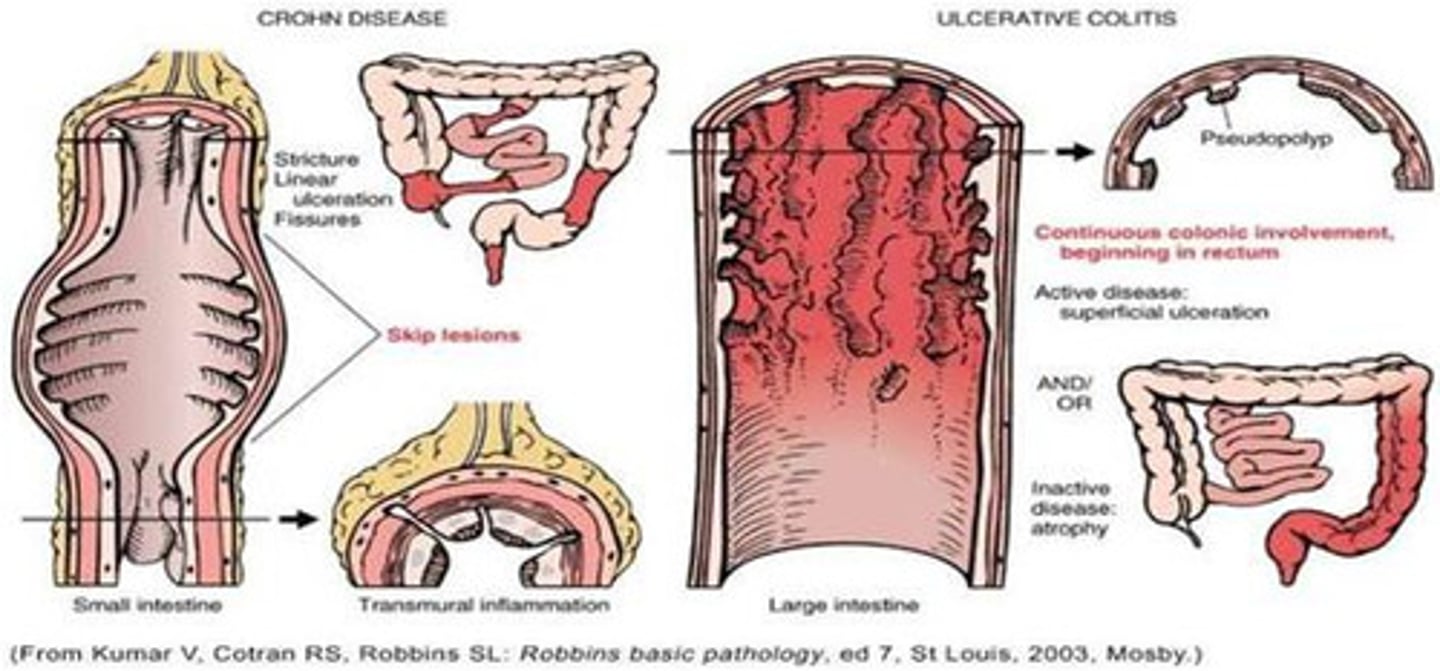
Tell me everything you know about Crohn's
location:
- usually terminal ileum and colon but can be anywhere
- skip lesions
- rectal sparing
gross morphology:
- transmural lesions --> fistulas
- cobblestone mucosa
- creeping fat
- bowel wall thickening ("string sign" on barium swallow)
- linear ulcers, fissures
microscopic morphology:
- non-caseating granulomas and lymphoid aggregates
complications:
- malabsorption, malnutrition
- colorectal cancer
- fistulas (enterovesical --> recurrent UTI and pneumaturia)
- strictures (leading to obstruction)
- perianal disease
intestinal manifestation:
- diarrhea +/- blood
extraintestinal manifestation:
- rash (pyoderma gangrenosum, erythema nodosum), eye inflammation (episcleritis, uveitis), oral ulcerations (apthous stomatitis), arthritis (peripheral, spondylitis)
- kidney stones (usually calcium oxalate)
- gallstones
treatment:
- corticosteroids, azathioprine, antibiotics (cipro, metro), infliximab, adalimumab
Old crohn skips a stone down a cobble stone road, but it never comes out
- cobble stoning
- skip lesions
- rectal sparing
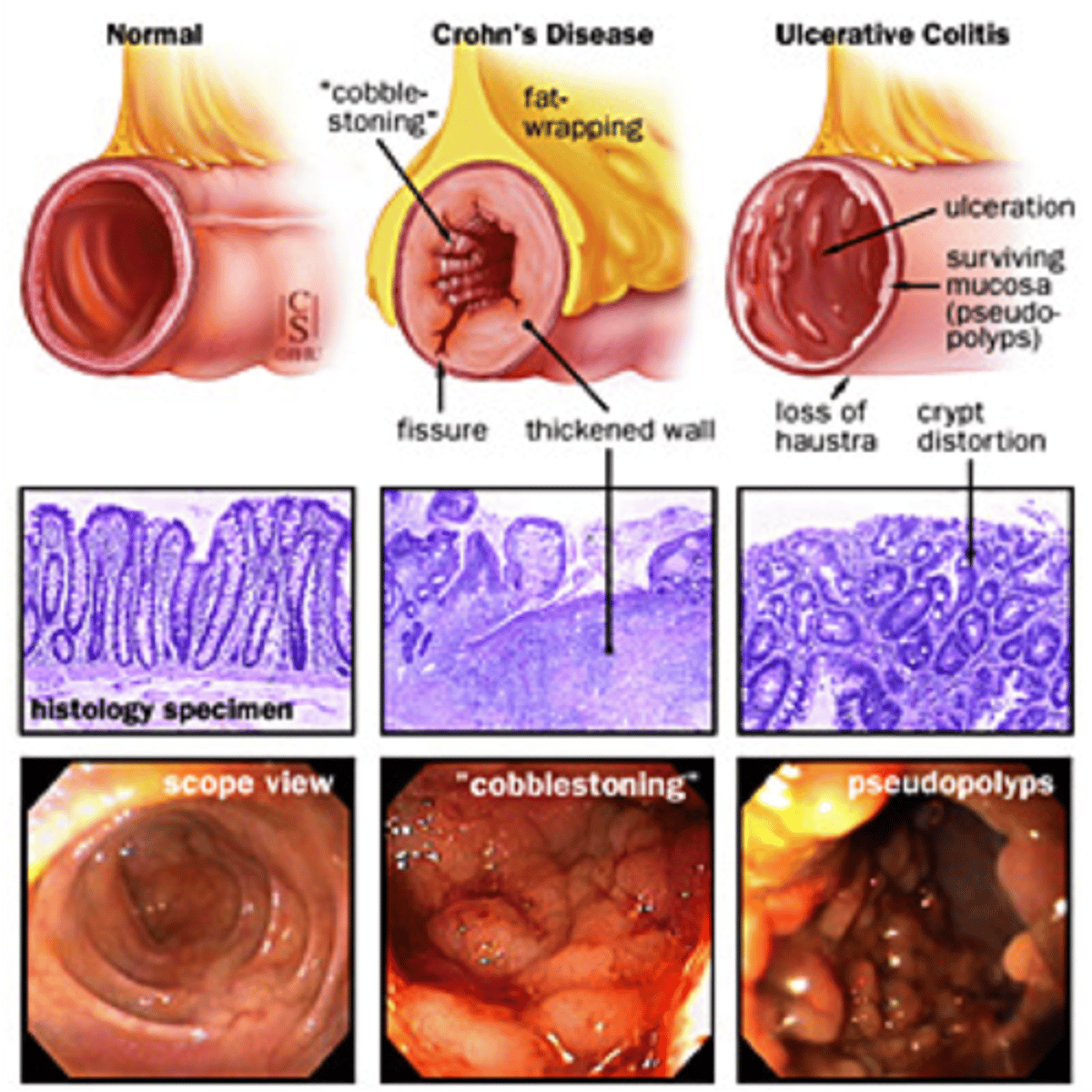
Compare and contrast Crohn's Disease vs Ulcerative Colitis
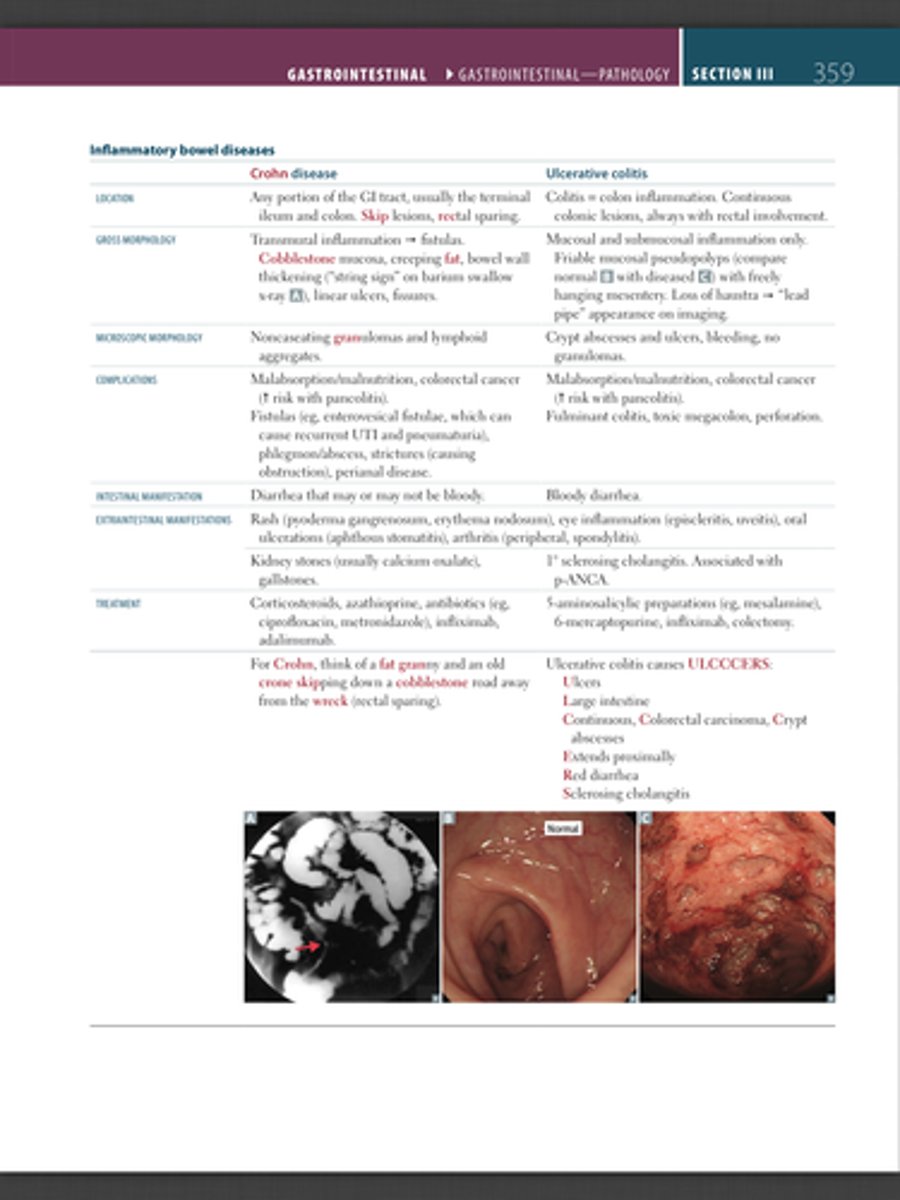
Tell me everything you know about Ulcerative Colitis
location:
- continuous colon involvement
- ALWAYS rectal involvement
gross morphology:
- mucosal and submucosal inflammation only
- friable mucosal polyps
- loss of haustra --> "lead pipe" appearance
microscopic morphology:
- crypt abscesses and ulcers
- bleeding
- no granulomas
complications:
- malabsorption, malnutrition
- colorectal cancer
- fulminant colitis, toxic megacolon, perforation
intestinal manifestation:
- BLOODY diarrhea
extraintestinal manifestation:
- rash (pyoderma gangrenosum, erythema nodosum), eye inflammation (episcleritis, uveitis), oral ulcerations (apthous stomatitis), arthritis (peripheral, spondylitis)
- PRIMARY SCLEROSING CHOLANGITIS, p-ANCA
treatment:
- 5-ASA, 6-MP, infliximab, colectomy
ULCCCERS
ULCERS
Large intestines
Continuous, Colorectal carcinoma, Crypt abscesses
Extends proximally
Red diarrhea
Sclerosing Cholangitis
Which IBD is associated with Primary Sclerosing Cholangitis?
Ulcerative Colitis (p-ANCA)
Chron's disease is Th___ mediated while UC is Th___ mediated
Chron's: Th1
UC: Th2
Smoking is protective in __________ (chrons/UC)?
UC
What is the diagnostic criterion for IBS?
What is the diagnostic criterion for IBS?
recurrent abdominal pain associated with >2 of the following:
- pain improves with defecation
- change in stool frequency
- change in appearance of stool
Additionally:
- must have no structural abnormalities
- most common in middle aged women
- chronic symptoms may be diarrhea-predominant/constipation-predominent or mixed
Appendicitis
What is it?
- acute inflamamtion of the appendix
- obstruction by a fecalith (in adults)
- lymphoid hyperplasia (in children)
Signs/Symptoms?
- initially diffuse periumbilical pain then migrates to McBurney point
- nausea, fever --> suggests peritonitis
- can elicit psoas, obsturator, Rovsing signs
- guarding and rebound tenderness on exam
Treatment:
- appendectomy
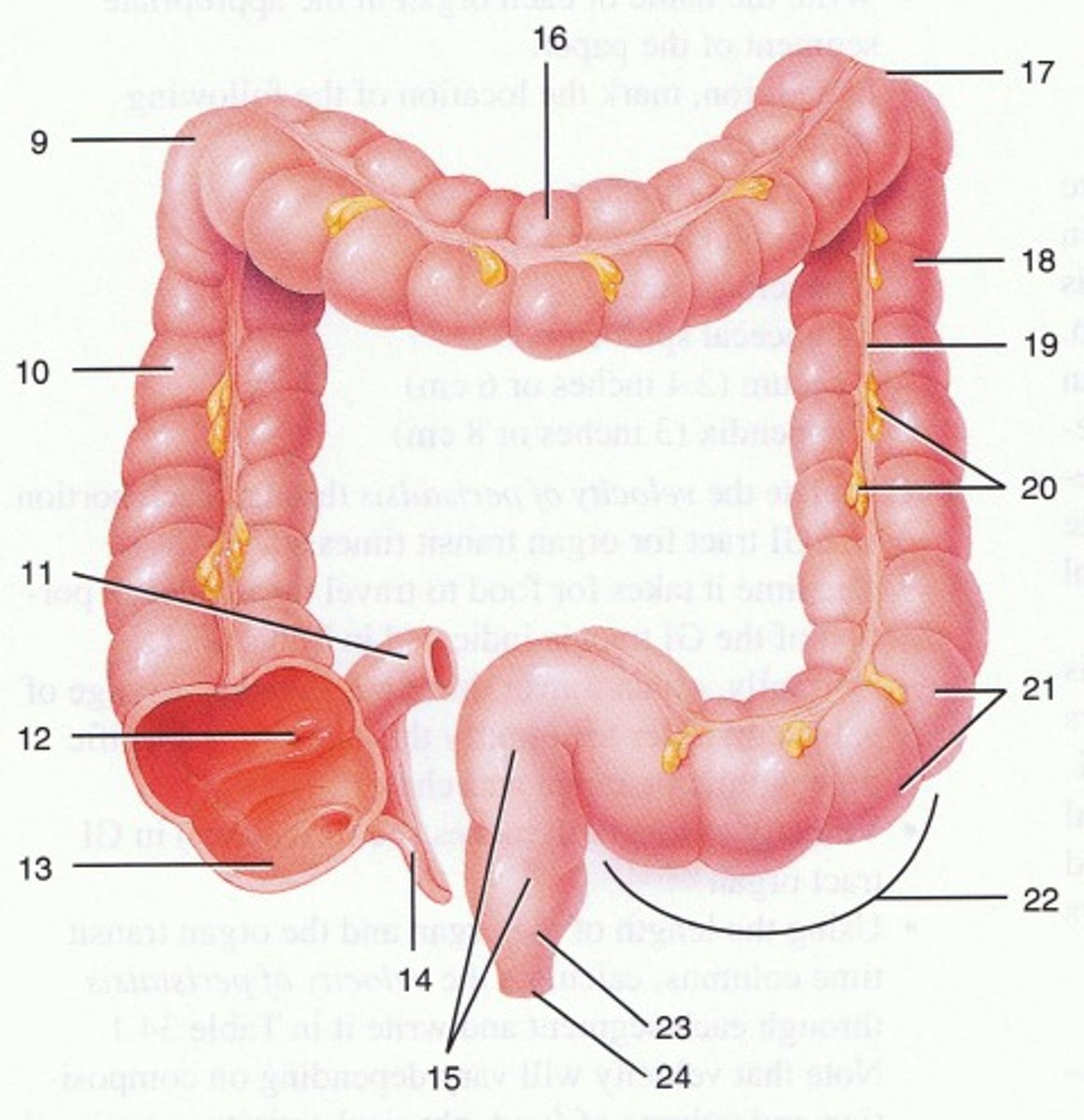
What is Diverticulum?
DIVERTICULUM:
- blind pouch protruding from gut tract
- most are acquired and termed "false" because they lack or have an attenuated muscularis externa
- most often in the sigmoid colon
"True" diverticulum = all 3 gut wall layers are involved (Meckels)
"False" diverticulum = aka pseudodiverticulum = only mucosa and the submucosa outpouch. Occur especially where the vasa recta perforate the muscularis externa
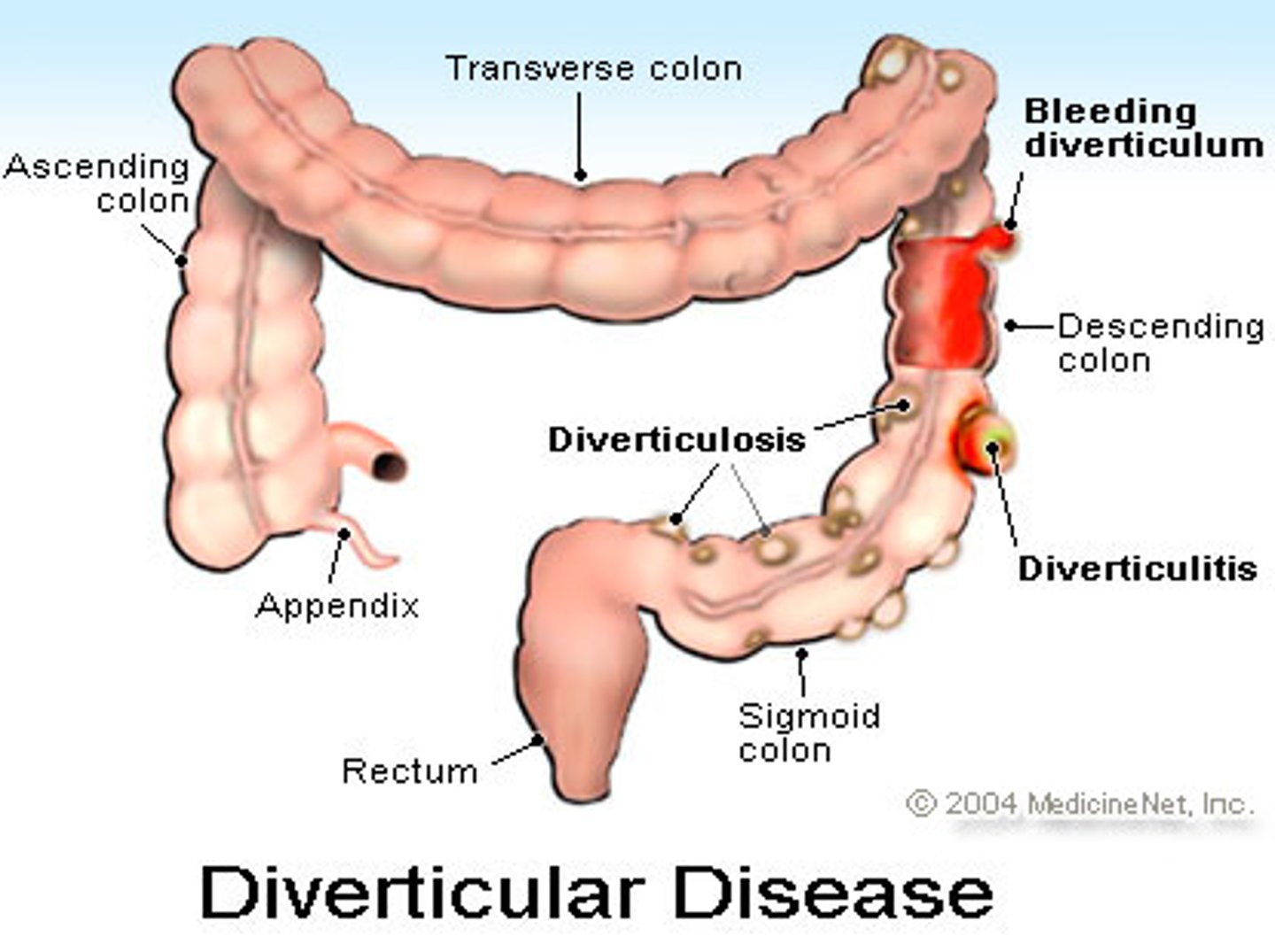
What is Diverticulosis?
DIVERTICULOSIS:
- many false diverticula of the colon, commonly sigmoid
- common (in 50% of people > 60)
- due to increased intraluminal pressure and focal weakness in the colonic wall
.
Associated with obesity and diets low in fiber,
high in total fat/red meat.
- asymptomatic with vague discomfort
- complications include diverticular bleeding (painless hematochezia), diverticulitis
What is Diverticulitis?
DIVERTICULITIS:
-Inflammation of Diverticula-->LLQ pain, fever, leukocytosis
- complications: absecess, fistula, obstruction, perforation (peritonitis)
RX: antibiotics (metronidazole, fluoroquinolone, TMP-SMX)
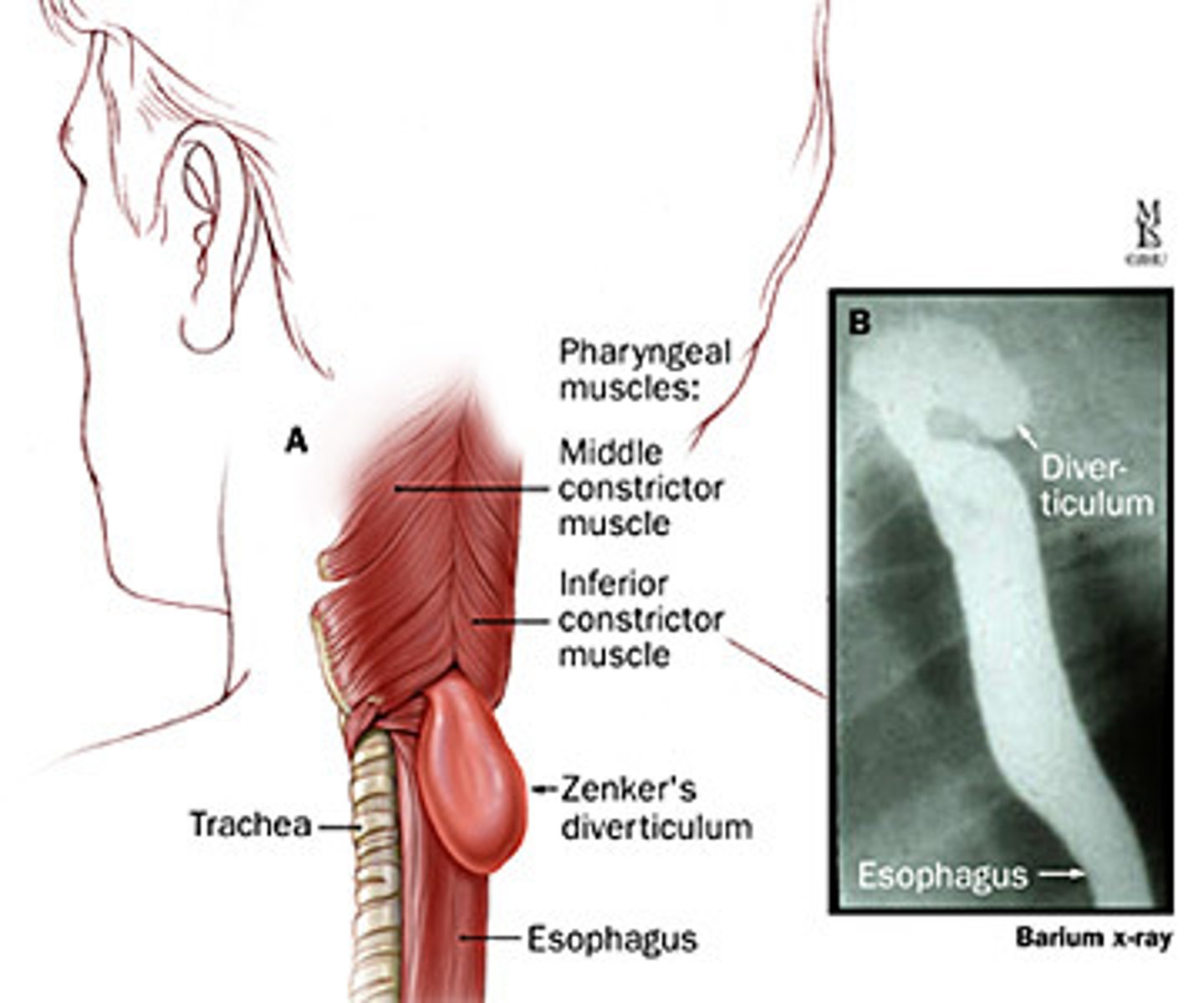
Zenker diverticulum
what is it? where does it happen?
- pharyngoeosphageal FALSE diverticulum
- esophageal dysmotility causes herniation of mucosal tissue at Killian triangle between the thyropharyngeal and cricopharyngeal parts of the inferior pharyngeal constrictor
symptoms?
- dysphagia
- obstruction
- gurgling
- aspiration
- foul breath (halitosis)
- neck mass
- elderly males
"Elder MIKE has HALITOSIS"
- Elderly
- Males
- Inferior pharyngeal constrictor
- Killian triangle
- Esophageal dysmotility
- Halitosis
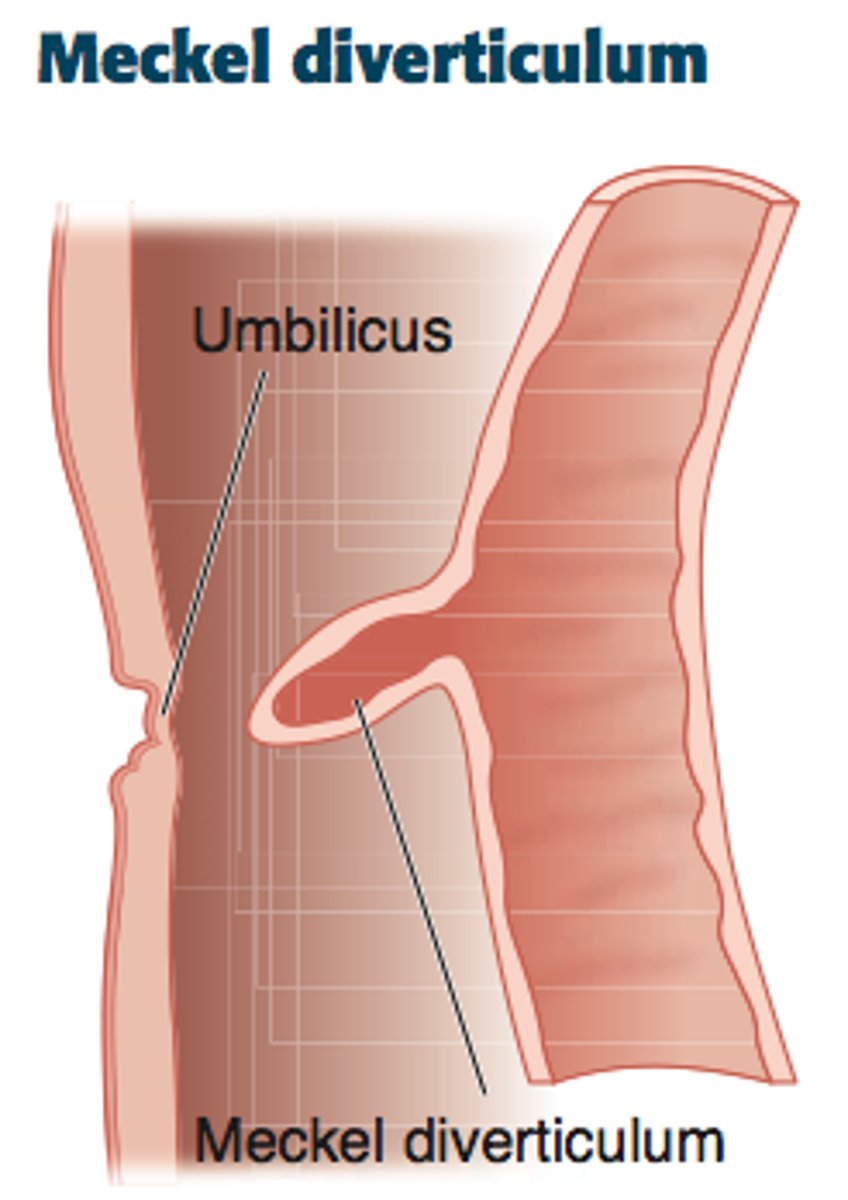
Meckel Diverticulum
what is it?
- TRUE diverticulum-- persistence of the vitelline duct (failure to involute)
- may contain ectopic acid secreting gastric mucosa and/or pancreatic tissue
- MOST common congenital anomaly of the GI tract
Sx:
- melena
- RLQ pain
- intussusception
- volvulus
- obstruction near terminal ileum
- current jelly stool --> if intussesception
diagnosis?
- pertechnetate study for uptake by ectopic gastric mucosa
Rule of 2's
- 2x M>F
- 2 inches long
- 2 feet from the ileocecal valve
- 2% of population
-first 2 years of life
-2 types of epithelia (gastric/pancreatic)
Hirschsprung disease
- congenital megacolon-- lack of ganglion cells/enteric nervous plexuses (Auerbach and Meissner plexuses) in distal segment of the colon
- due to failure of neural crest migration
- RET mutations
- increased risk in Down Syndrome
Sx:
- bilious emesis
- abdominal distention
- failure to pass meconium in 48 hours after birth
- normal portion of the colon proximal to the aganglionic segment is dilated, resulting in a "tranistion zone"
Dx:rectal suction biopsy
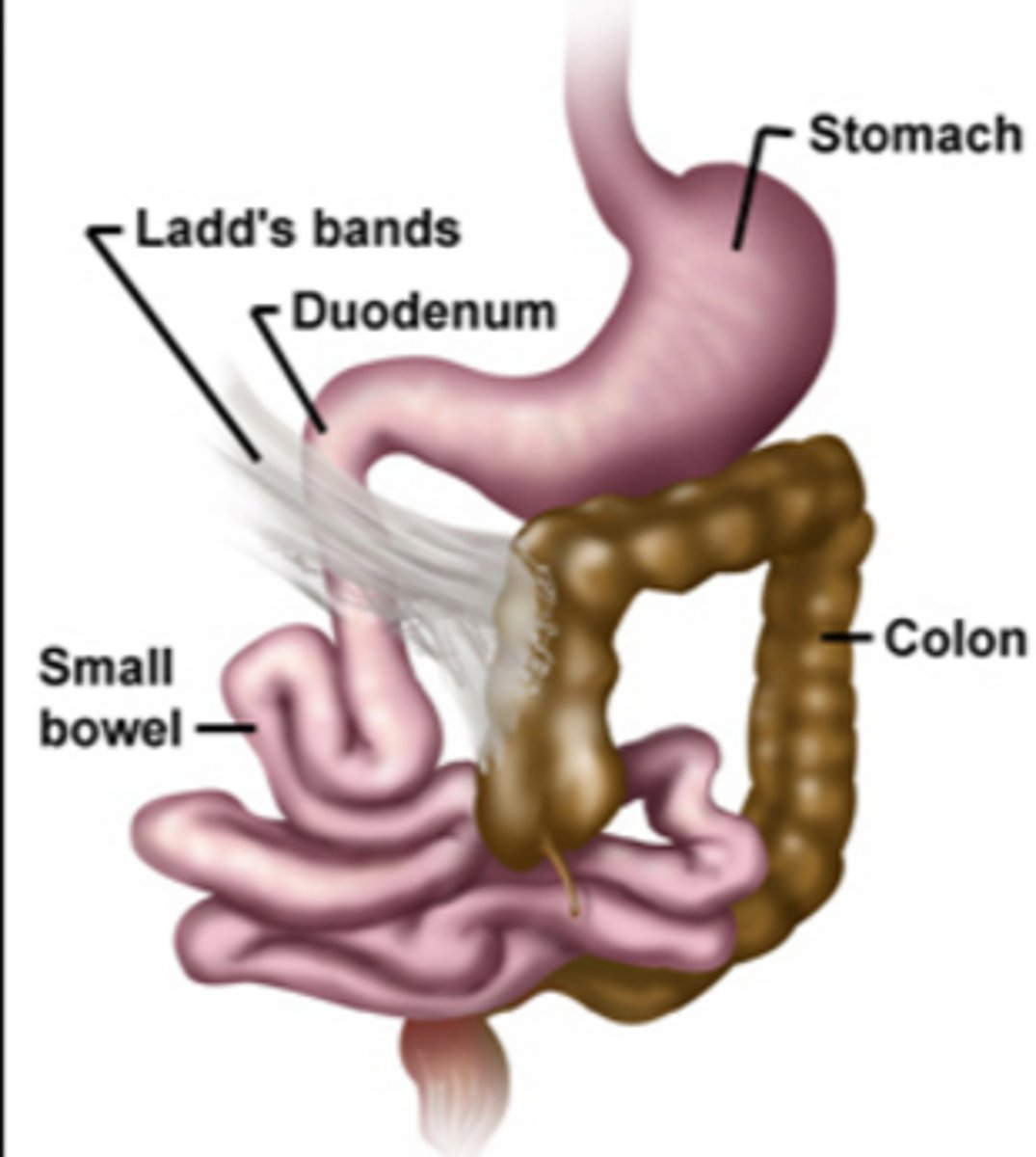
Malrotation
- anomaly of midgut rotation during fetal development
-improper positioning of the bowel, formation of fibrous bands (Ladd bands)
- can lead to volvulus, duodenal obstructionz
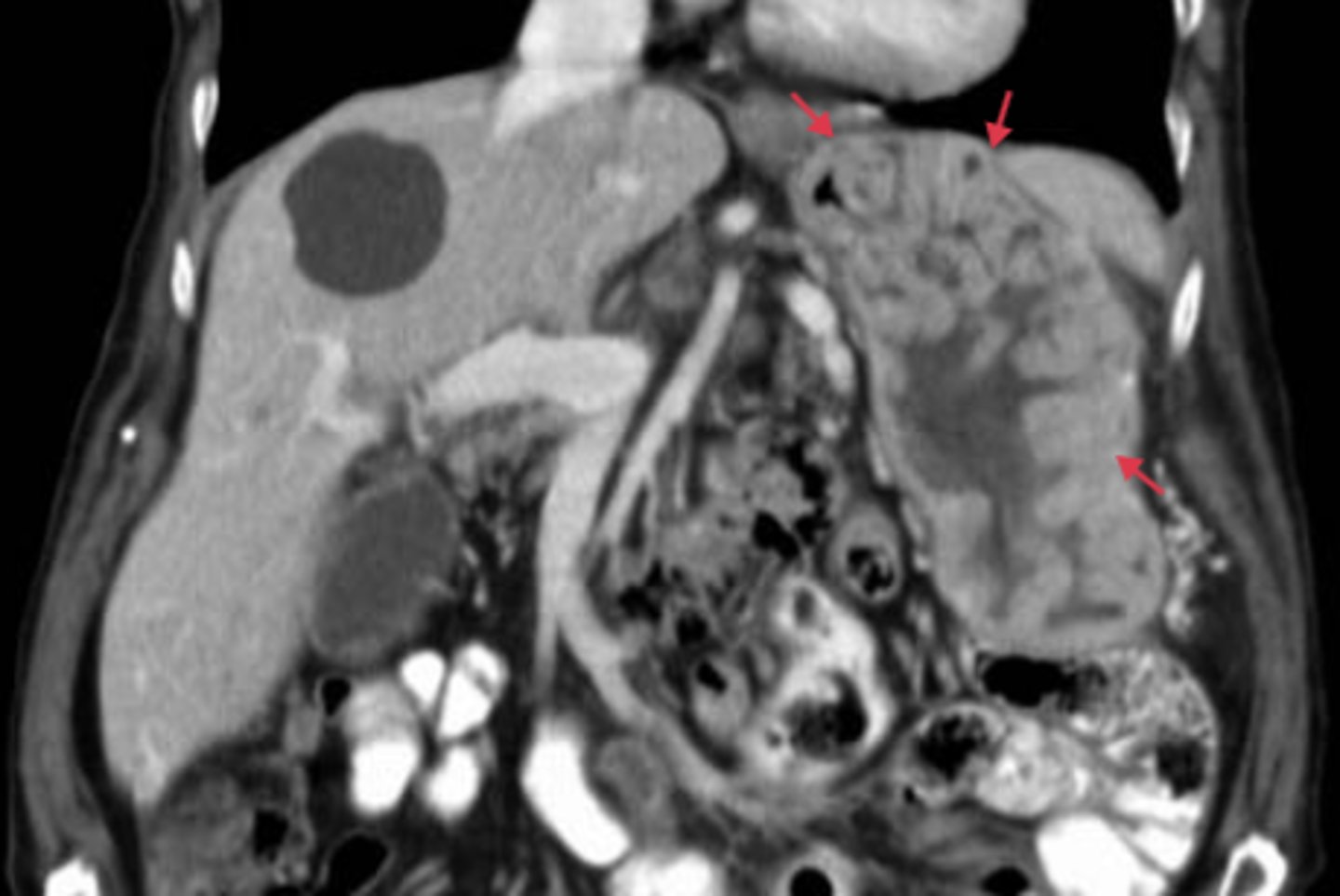
Which GI diseases are associated with Down's?
1. Hirschsprung
2. Annular pancreas- abnormal rotation of ventral pancreatic bud forms a ring of pancreatic tissue
encircles 2nd part of duodenum; may cause duodenal narrowing (arrows in A ) and vomiting.
3. Duodenal atresia
4. Celiac disease
Red current jelly stool
Seen in a lot of stuff --> intussusception, acute mesenteric ischemia

Volvulus
- twisting of a portion of bowel around its mesentery
- can lead to obstruction/infarction
where does it happen?
- can occur anywhere in GI tract
Kids: midgut volvulus
Young adults: Cecum
Elderly: sigmoid volvulus

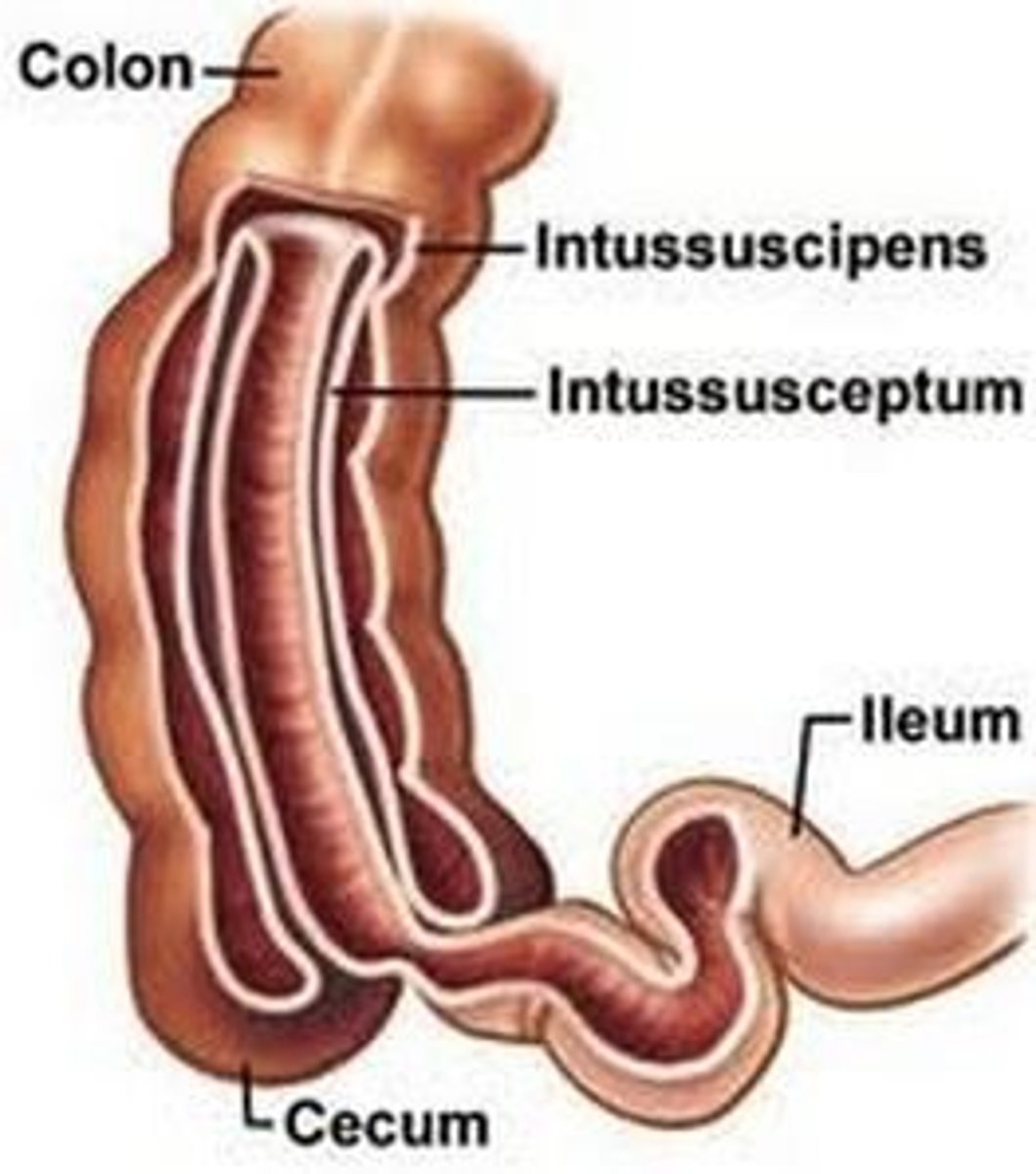
Intussusception
- telescoping of proximal bowel segment into distal segment--> ileocecal junction
Sx:
- intermittent abdominal pain with "currant jelly" stools
- bulls eye appearance on ultrasound
- UNUSUAL in adults (associated with intraluminal mass or tumor)
- majority of cases are in children (associated with recent viral infection like adenovirus --> Peyer patch hypertrophy --> creating a lead point)
Abdominal emergency
Acute mesenteric ischemia
critical blockage of blood (often embolic occlusion of SMA) --> small bowel necrosis --> abdominal pain out of proportion to physical findings
May see currant jelly stools
Chronic mesenteric ischemia
- "intestinal angina"
- atherosclerosis of celiac artery, SMA, IMA resulting in intestinal hypo-perfusion --> postprandial epigastric pain
food aversion and weight loss
Colonic ischemia
- reduction in intestinal blow flow leading to ischemia
- causes crampy abdominal pain followed by hematochezia
- commonly occurs at watershed areas (splenic flexure, distal colon)
- typically affects the elderly
Thumbprint sign on imaging due to mucosal edema/hemorrhage
Adhesion
- due to fibrous bands of scar tissue
- commonly forms after surgery
- most common cause of small bowel obstruction
- can have well demarcated necrotic zones
Angiodysplasia
- tortuous dilation of vessels resulting in hematochezia
- most often found in the cecum, terminal ileum and ascending colon
- more common in elderly
- Associated with end-stage renal disease,
von Willebrand disease, aortic stenosis.
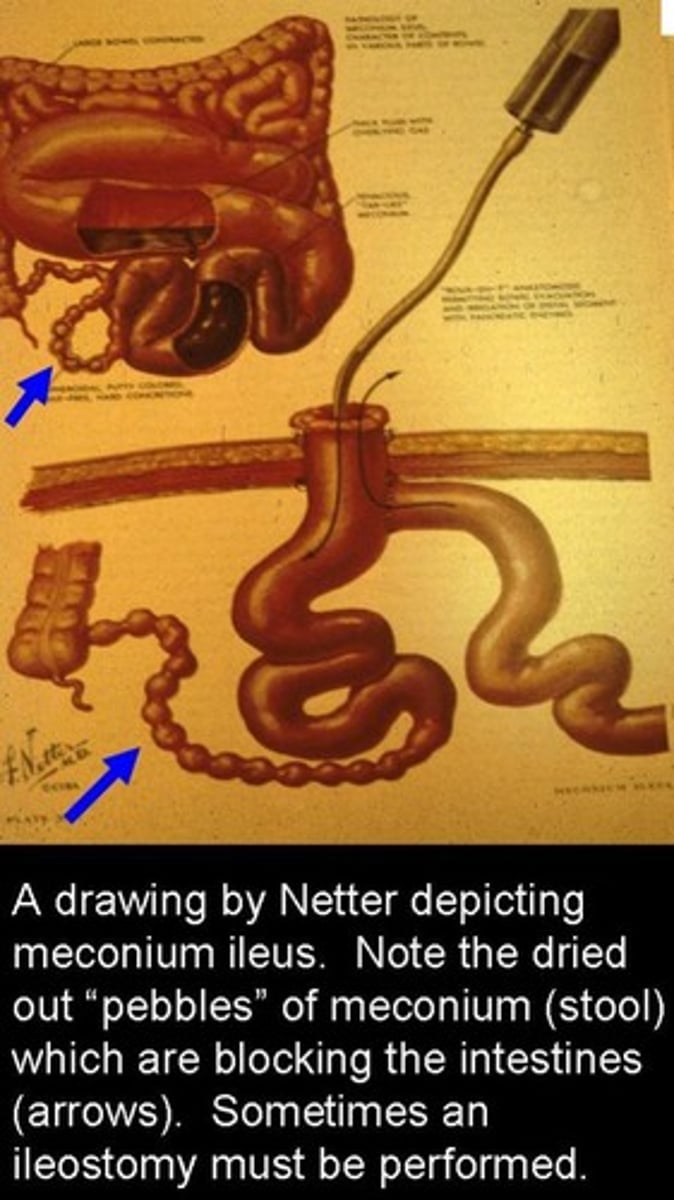
Meconium ileus
- seen in cystic fibrosis
- when a meconium plug obstructs the intestine, preventing the passage of stool at birth
Ileus
- intestinal hypomotility WITHOUT obstruction resulting in:
- constipation and ↓ flatus
- distended/tympanic abdomen with decreased bowel sounds
- associated with abdominal surgeries, opiates, hypokalemia, sepsis
rx:
- bowel rest
- electrolyte correction
- cholinergic drugs (to stimulate intestinal motility)
Necrotizing enterocolitis
- seen in premature, formula-fed infants with immature immune systems
- necrosis of the intestinal mucosa --possible perforation, which can lead to pneumatosis intestinalis, free air in abdomen, portal venous gas
Small Bowel Ischemia can come in 2 flavors. What are they?
1. Transmural infarct: due to thrombosis/embolus of SMA/mesenteric vein
--abdominal pain, bloody diarrhea, ↓bowel sounds
2. Mucosal infarct: due to marked hyPO tension
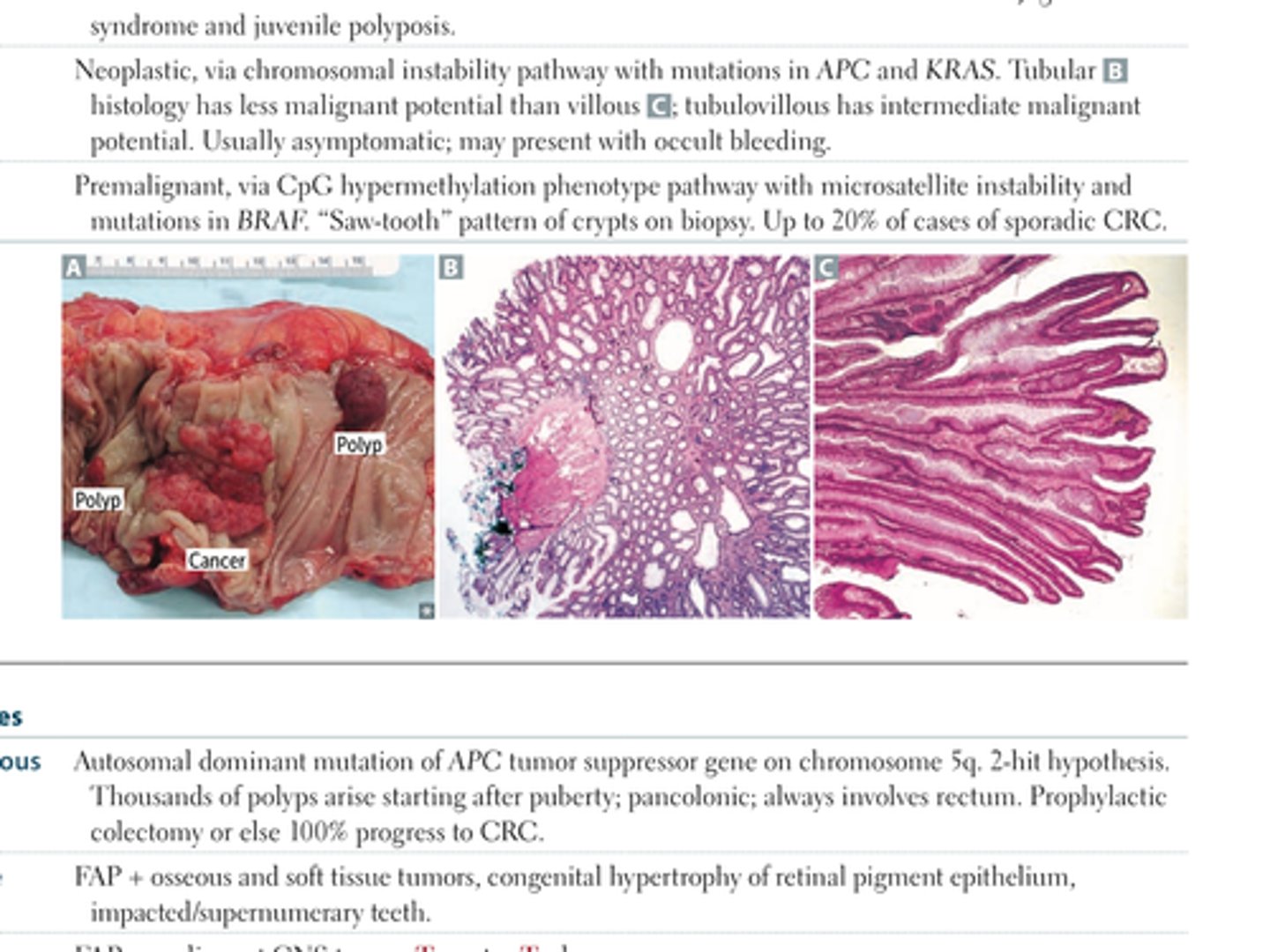
Colonic polyps:
- growths of tissue in the colon that can be neoplastic or non-neoplastic
- generally classified by histologic type
1. Flat
2. Sessile
3. Pedunculated
Histological Types:
1. Non-neoplastic: Hamartomatous, inflammatory, Submucosal, Hyperplastic
2. Malignant potential: Adenomatous, Serrated