Infections of the central nervous system (CNS)
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
Why do we care about CNS infections?
Extremely dangerous
Significant morbidity and mortality
Very little time to act upon recognition of symptoms
Need to know the symptoms of CNS infections
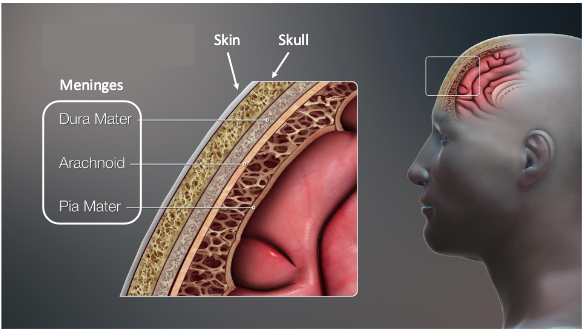
what are physical barriers to infection that protect the CNS?
Skin, skull, meninges
what is the blood-brain barrier?
Tight junctions between endothelial cells
what is the Blood-cerebrospinal fluid barrier (choroid plexus)?
Tight junctions between epithelial cells
what are the barriers against infection that protect the CNS?
Physical barriers to infection
Blood-brain barrier (BBB)
Blood-cerebrospinal fluid barrier (choroid plexus)
Immunosurveillance
what cells are involved in immunosurveillance of CNS?
Glial cells
infiltrating dendritic cells
macrophages
T cells in subarachnoid space
what are potential routes of CNS infection?
direct trauma
neural route
hematogenous route
how does direct trauma to CNS cause infection?
Direct inoculation of pathogenic microbes into the CNS
how does the neural route cause CNS infection?
Migration through the peripheral nerves or olfactory nerves
how does the hematogenous route cause CNS infection?
From the bloodstream into the cerebrospinal fluid (CSF) by crossing the choroid plexus
From the bloodstream into the brain by crossing the blood-brain barrier
what are the types of CNS diseases due to infection?
encephalitis (inflammation of brain)
meningitis (inflammation of meninges)
myelitis (inflammation of spinal cord)
what are symptoms of meningitis?
Altered mental status
Stiff neck
High fever
Headache
what are symptoms of encephalitis?
• Fever
• Altered mental status
• Headache
• Weakness in certain areas of body
• Confusion
what are symptoms of prion disease?
• Cognitive changes
• Lack of coordination
• Progressive dementia
what types of infectious agents can cause CNS infection?
The following statements about CNS infections are correct EXCEPT one. Which is the EXCEPTION?
A. Bacteremia can precede some CNS infections
B. Encephalitis means infection of the membranes surrounding the brain
C. The CNS is protected by multiple barriers, including physical, cellular, and immunological
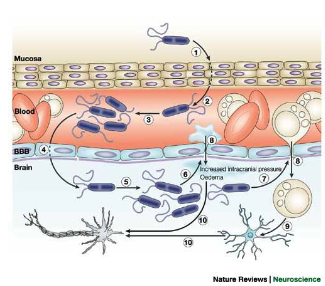
D. The concentration of glucose in the cerebrospinal fluid (CSF) is normal during viral meningitis but lower than normal during bacterial meningitis
B. Encephalitis means infection of the membranes surrounding the brain
Cerebrospinal fluid (CSF) parameters important in
diagnosing CNS infections.
Condition: no infection
Immune cell levels?
Glucose levels?
Protein levels?
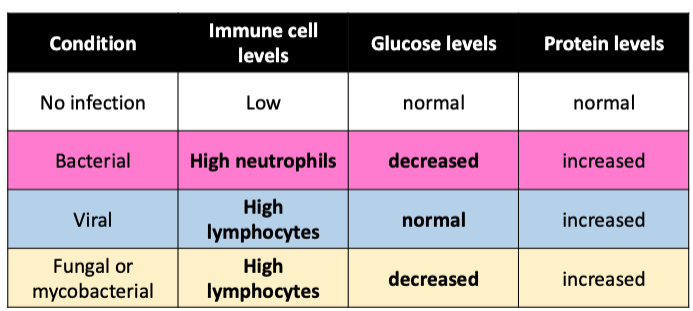
Cerebrospinal fluid (CSF) parameters important in
diagnosing CNS infections.
Condition: bacterial
Immune cell levels?
Glucose levels?
Protein levels?
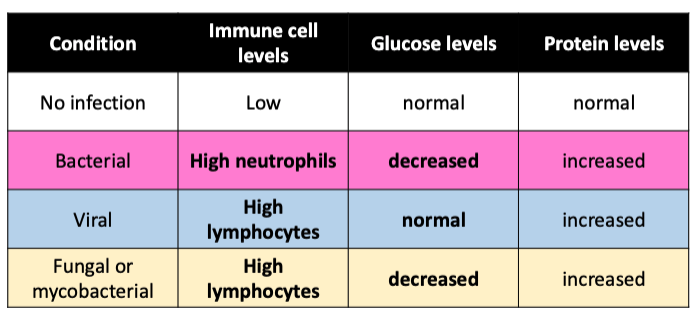
Cerebrospinal fluid (CSF) parameters important in
diagnosing CNS infections.
Condition: viral
Immune cell levels?
Glucose levels?
Protein levels?
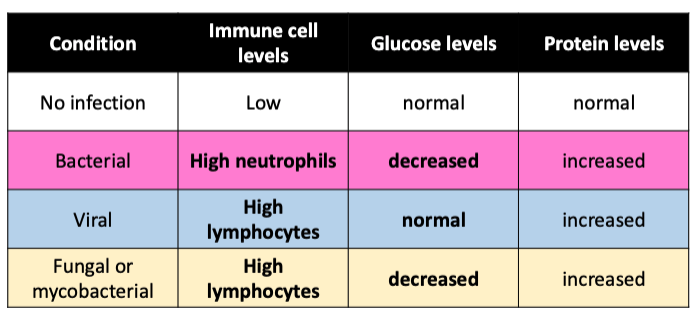
Cerebrospinal fluid (CSF) parameters important in
diagnosing CNS infections.
Condition: fungal or mycobacterial
Immune cell levels?
Glucose levels?
Protein levels?
Neisseria meningitidis: encounter
person-to-person, close contact
Respiratory droplets, kissing
Commensal, colonizes nasopharynx (10% people)
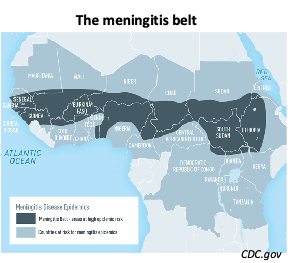
Neisseria meningitidis: entry
respiratory route, oral route
Group settings (e.g., colleges)
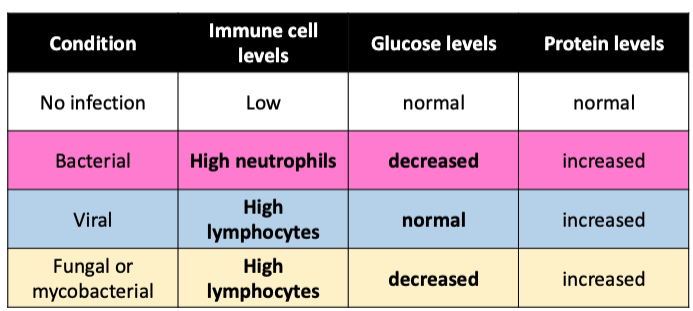
Neisseria meningitidis is endemic to….?
sub-Saharan Africa (the meningitis belt) and Saudi Arabia
Travelers are at risk
e.g., Hajj or Umrah pilgrimages
what type of bacteria is neisseria meningitidis?
Gram- diplococcus
Six serogroups

Neisseria meningitidis: spread
to bloodstream, crosses blood-brain barrier
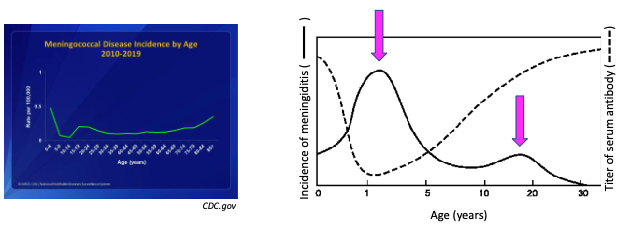
describe the age-dependen incidences of meningitis due to N. meningitidis
Peak incidence at 6-24 months of age (because that’s when maternal antibodies wean out)
Neisseria meningitidis: initial symptoms
Fever, headache, neck stiffness, aversion to bright light
what is critical for patient’s survival when infected with N. meninigitidis?
Rapid diagnosis and treatment with antibiotics
Neisseria meningitidis: outcomes
Very rapid progression, can be fatal within hours
Without antibiotic, brain damage with a 50% fatality
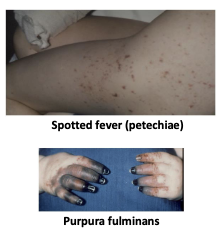
Neisseria meningitidis: damage (what damage does it cause?)
Sepsis, meningitis
Spotted fever, a.k.a. petechiae (hemorrhagic rash)
Purpura fulminans (necrosis, damage to blood vessels)
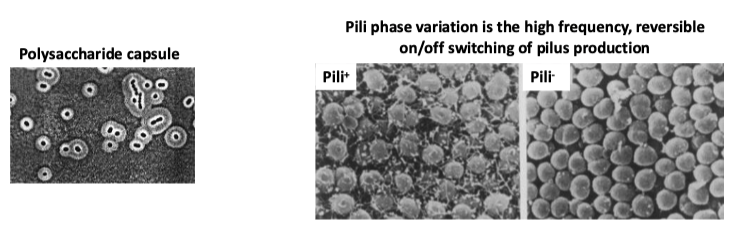
Neisseria meningitidis virulence factors
• Capsule (anti-phagocytic)
• Pili (attachment to cells)
• Phase and antigenic variation (avoid immune system)
• Lipooligosaccharide (LOS): inflammatory endotoxin
Neisseria meningitidis prevention
Vaccines
• MenACWY: 11-12 yo, travel to endemic areas
• MenB: 16-18 yo
Which one of the following statements concerning Neisseria meningitidis infection of the CNS is FALSE?
A. Bacterial meningitis is a potentially deadly disease that requires prompt antibiotic treatment
B. Capsule is an important virulence factor of this pathogen
C. N. meningitidis causes infection of the meninges
D. N. meningitidis is never found in healthy nasopharynx microbiota
D. N. meningitidis is never found in healthy nasopharynx microbiota
All of the following are virulence factors of the Neisseria meningitidis EXCEPT one. Which is the EXCEPTION?
A. AB toxin
B. Capsule
C. Phase variation
D. Pili
A. AB toxin
what are the categorizations of viral infections of the CNS?
neurotropic
respiratory
arboviruses
what type of viral infections of the CNS is eastern equine encephalitis virus?
arbovirus
Eastern Equine Encephalitis Virus (EEEV) is transmitted via…?
mosquitos, ticks, or other arthropods
A 15-year-old female complained to her dentist that she was ill, having vomited earlier.
She had a headache, stiff neck, and the bright dental examination light bothered her.
The dentist told the parent that she needed to go to the emergency room immediately.
The emergency room physical exam showed a fever of 103°F, scattered petechiae (small hemorrhages in skin and mucous membranes), and a stiff neck (she was unable to touch her chin to her chest).
A lumbar puncture was performed. The cerebrospinal fluid (CSF) had an elevated white blood cell count, elevated protein levels, and decreased glucose concentration. Gram stain of the CSF showed Gram– diplococci. She was treated with immediate IV penicillin.
Her blood and CSF cultures both grew …?
She was treated with antibiotics for 7 days and made a complete recovery.
N. meningitidis.
in EEEV, infections, serological testing of CSF will show…?
IgM antibodies positive for EEEV
what is a common characteristic found in CSF analysis of EEEV infections?
high leukocytes (mostly neutrophils)
EEEV: Multiplication
• Replicates in mesenchymal lineage tissues (fibroblasts, osteoblasts, myocytes, etc.)
EEEV: spread
Invades CNS by hematogenous route
EEEV: symptoms
• Often asymptomatic
• Some develop systemic febrile illness or neurologic disease
incubation period of EEEV?
4-10 days
EEEV mortality rate?
• ~ 30% mortality rate
• mild to severe physical and mental sequelae in survivors
EEEV: diagnosis?
• Patient history (clinical features, travel, etc.)
• Testing CSF for anti-EEEV IgM and viral RNA genomes
Herpes simplex virus (HSV) oral infections: entry
• Transmitted in saliva and other bodily fluids
• Infects mucosal epithelial cells of the oral region
• Primary mucosal infection
• Mostly, asymptomatic
• Gingivostomatitis

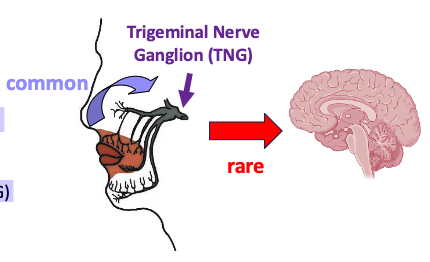
Herpes simplex virus (HSV) oral infections: spread
Spreads to local sensory neurons (PNS) and travels along the fiber to the craniospinal ganglia
• Typically, to trigeminal nerve ganglion (TNG)
• Rarely, from TNG to CNS
Herpes Simplex encephalitis (HSE): symptoms
seizures, fever, headaches, language impairment, mental status change
Herpes Simplex encephalitis (HSE): diagnosis
testing cerebrospinal fluid (CSF)
– PCR for HSV DNA
– Lymphocytes >> neutrophils
– MRI
what is the Most common and the only treatable viral encephalitis?
Herpes Simplex encephalitis (HSE)
Herpes Simplex encephalitis (HSE): treatment
Intravenous acyclovir (efficient and safe)
– Reduces mortality to 20-30% but <3% recover normal function
what is the most severe complication of HSV?
Herpes Simplex encephalitis (HSE)
70% mortality without treatment
CNS infections with which of the following viruses can be treated with antivirals?
A. Eastern Equine Encephalitis virus
B. Herpes simplex virus
C. West Nile virus
D. Zika virus
B. Herpes simplex virus
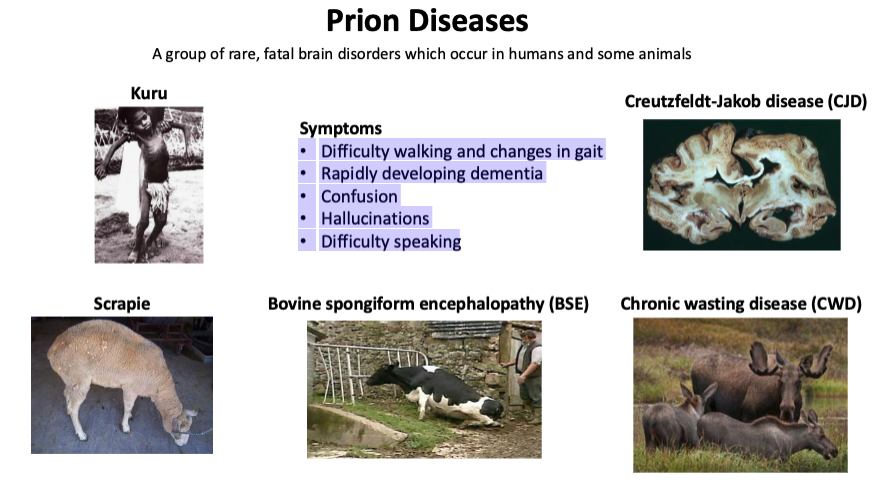
what are prion diseases?
A group of rare, fatal brain disorders which occur in humans and some animals
symptoms of prion diseases?
• Difficulty walking and changes in gait
• Rapidly developing dementia
• Confusion
• Hallucinations
• Difficulty speaking
what are examples of prion diseases?
kuru (humans)
scrapie (sheep)
bovine spongiform encephalopathy (cows)
chronic wasting disease (moose, elk)
creutzfeldt jakob disease (humans)
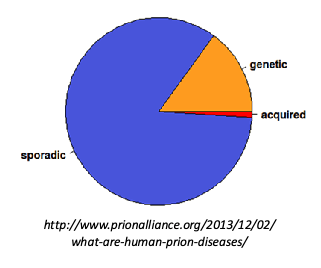
what are the different causes of prion diseases in humans?
sporadic (mutations)
genetic (hereditary)
acquired (infection or inoculation)
what type of prion disease is creutzfeldt jakob disease?
sporadic disease (mutation) and genetic
what are some genetic prion diseases?
• Creutzfeldt-Jakob disease (CJD)
• Fatal familial insomnia (FFI)
• Gerstmann–Sträussler–Scheinker (GSS)
what are some acquired prion diseases?
– Kuru
– Variant Creutzfeldt-Jakob disease (vCJD)
creutzfeldt jakob disease: symptoms
• Cognitive changes: failing memory, behavioral changes
• Lack of coordination
• Progressive dementia
• Fatal
creutzfeldt jakob disease: diagnosis
• Electroencephalography (EEG): measures brain’s electrical patterns
• CSF tests: elevated 14-3-3 and tau proteins (released from damaged brain tissue)
• MRI: disrupted brain structure
• Definitive: brain biopsy or autopsy
creutzfeldt jakob disease: treatment
none
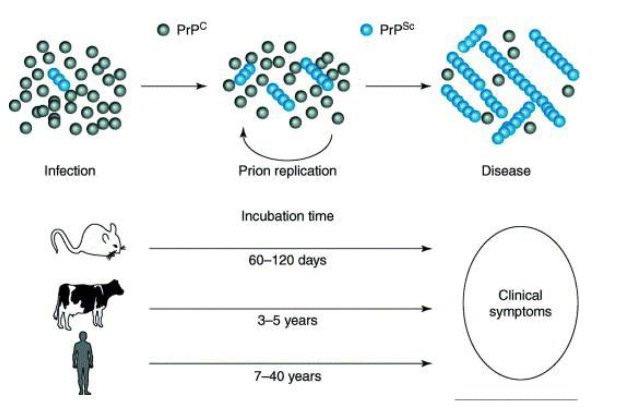
prion protein (PrP) can exist in 2 forms:
• PrPc, the non-pathogenic cellular form (C for cellular)
• PrPsc, the pathogenic form (SC for scrapie, the disease)
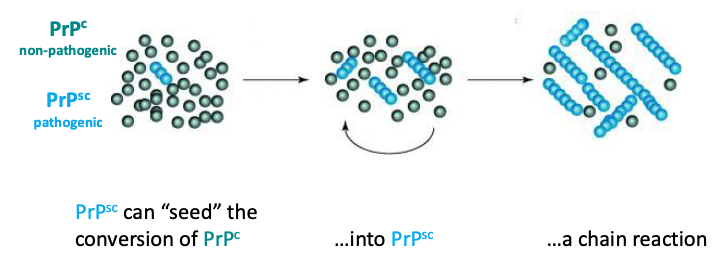
what is the infectious component of prion disease?
prion protein (PrP), a type of shape-shifting protein that is found in the brain (functions not well understood)
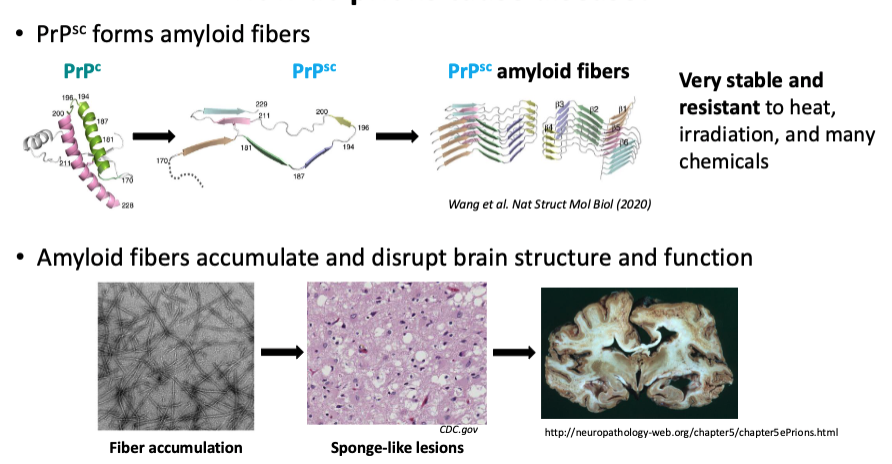
how do prions cause disease?
PrP-sc can “seed” the conversion of PrP-c into PrP-sc to start a chain reaction.
PrP-sc forms amyloid fibers that are very stable and resistant to heat, irradiation, and many chemicals.
Amyloid fibers accumulate to form sponge-like lesions that disrupt brain structure and function
t/f: Prions are transmissible (infectious)
true (acquired prion diseases)
Acquired prion diseases: encounter
Inoculation (direct route)
Contaminated surgical tools (iatrogenic)
Ingestion (indirect route)
consumption of brain tissue or meat contaminated with brain tissue
what are examples of acquired prion disease?
kuru (New Guinea, women/children due to cannibalistic practices)
variant Creutzfeldt-Jakob disease (vCJD) → mad cow disease in UK led to emergence in humans
t/f: Prion infections have very long incubation times
true
Which one of the following statements concerning Prions is TRUE?
A. Conversion of a normal cellular prion protein into a highly stable form that accumulates in the brain causes neurodegenerative disease
B. Prion diseases can only result from ingestion of food contaminated with pathogenic (disease-causing) prion proteins
C. Prion diseases can be treated
D. Transmission of prions occurs when bacteria that contain prion proteins are ingested
A. Conversion of a normal cellular prion protein into a highly stable form that accumulates in the brain causes neurodegenerative disease