ID Chapter 2: Streptococcal Diseases
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
13 Terms
Distinguish between the Staphylococci and Streptococci using key morphological and biochemical features.
Staphylococci:
- forms Grape Like Clusters
- Catalase +ve
- Develop Antibiotic resistance
Streptococci:
- Form Chains
- Catalase -ve
- Do not develop antibiotic Resistance
Name the pathogenic streptococci in terms of
1. How they are grouped
2. Tests Used for identification
3. Important Lancefield Groupings
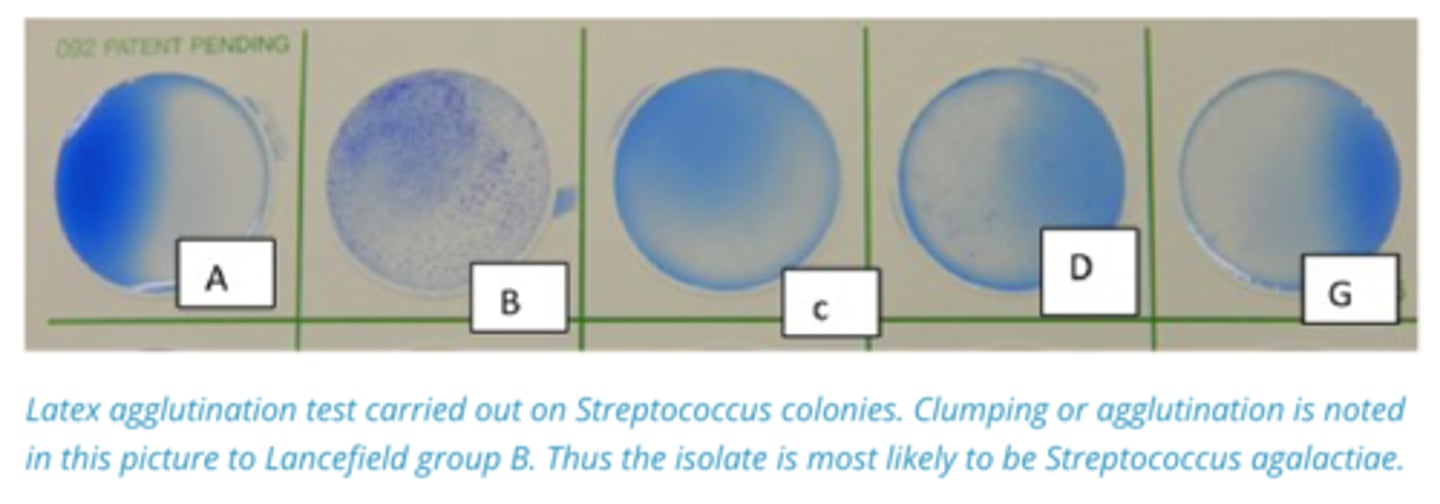
1. Beta-Haemolytic Streptococci are grouped into Lancefield types based on antibodies to Carbohydrates in the Streptococcal cell outer membrane.
2. Latex agglutination test is used as a method of antigen detection. Clumping of blue particles indicates agglutinating antibodies
3. Lancefield Group B: Streptococcus agalactiae (Mastitis). CAMP +ve
List the Potential sources of pathogenic streptococci and enterococci.
Streptococci are normal flora on the Skin and MM of the mouth, nose, throat, and external genitalia
List and describe the Function of Importance streptococcal virulence factors
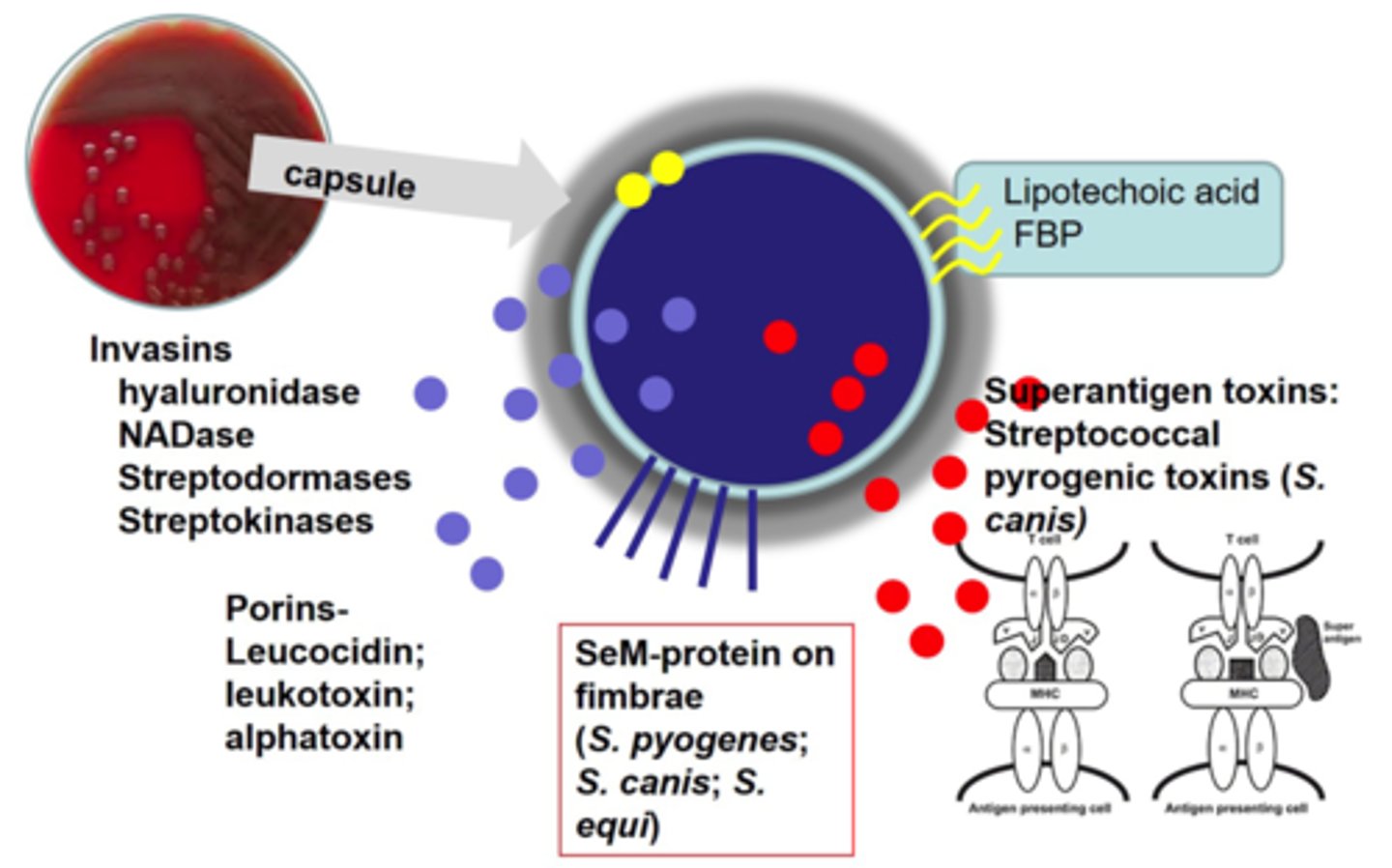
- Pus Causing (Pyogenic) infections of skin, udder, ear, Resp. Tract, Urogenital Tract.
- Some have Bacterial Capsules
- Produce Haemolysin (Porin) Toxins
- SeM Protein on fimbria,
- Fibrinogen Binding Protein + Lipotechoic acid on outer membrane
List the Antibiotics that are effective against Streptococcus
Penicillin, Amoxicillin (Oral):
Antibiotic Resistance uncommon
Describe Strangles (Streptococcus Equi Equi) in horses in terms of:
1. Horse→Horse Transmission
2. Morbidity/Mortality
3. Clinical Signs
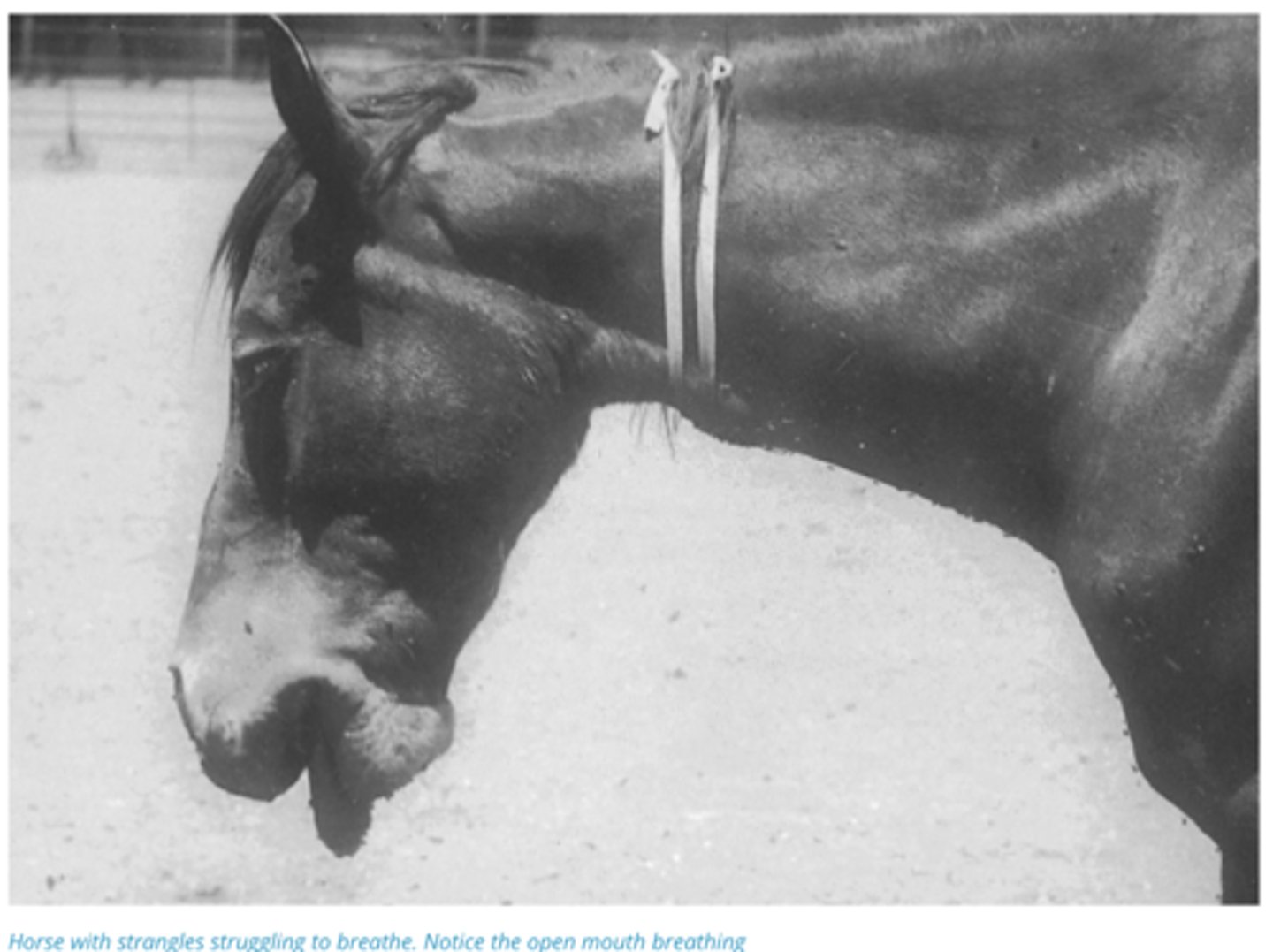
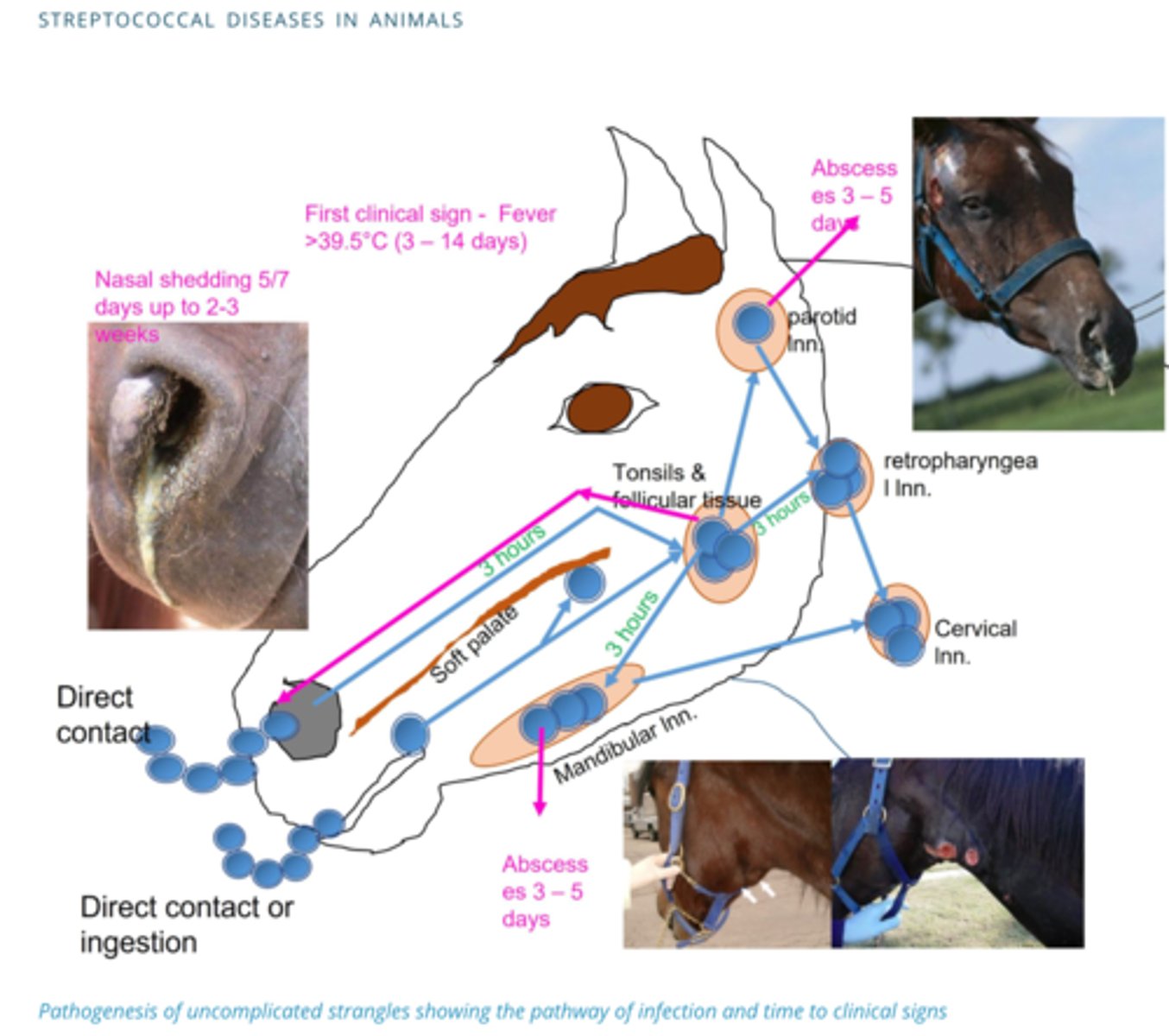
1. Spreads from Horse to Horse via inhalation of sneezed Bacteria or nasal/abscess contact directly or indirectly via contaminated surfaces and food
2. 100% Morbidity in unexposed stables, 1-2% Mortality
3. Head Lymph node abscesses/swelling, Pyrexia (High Fever), Nasal Discharge,
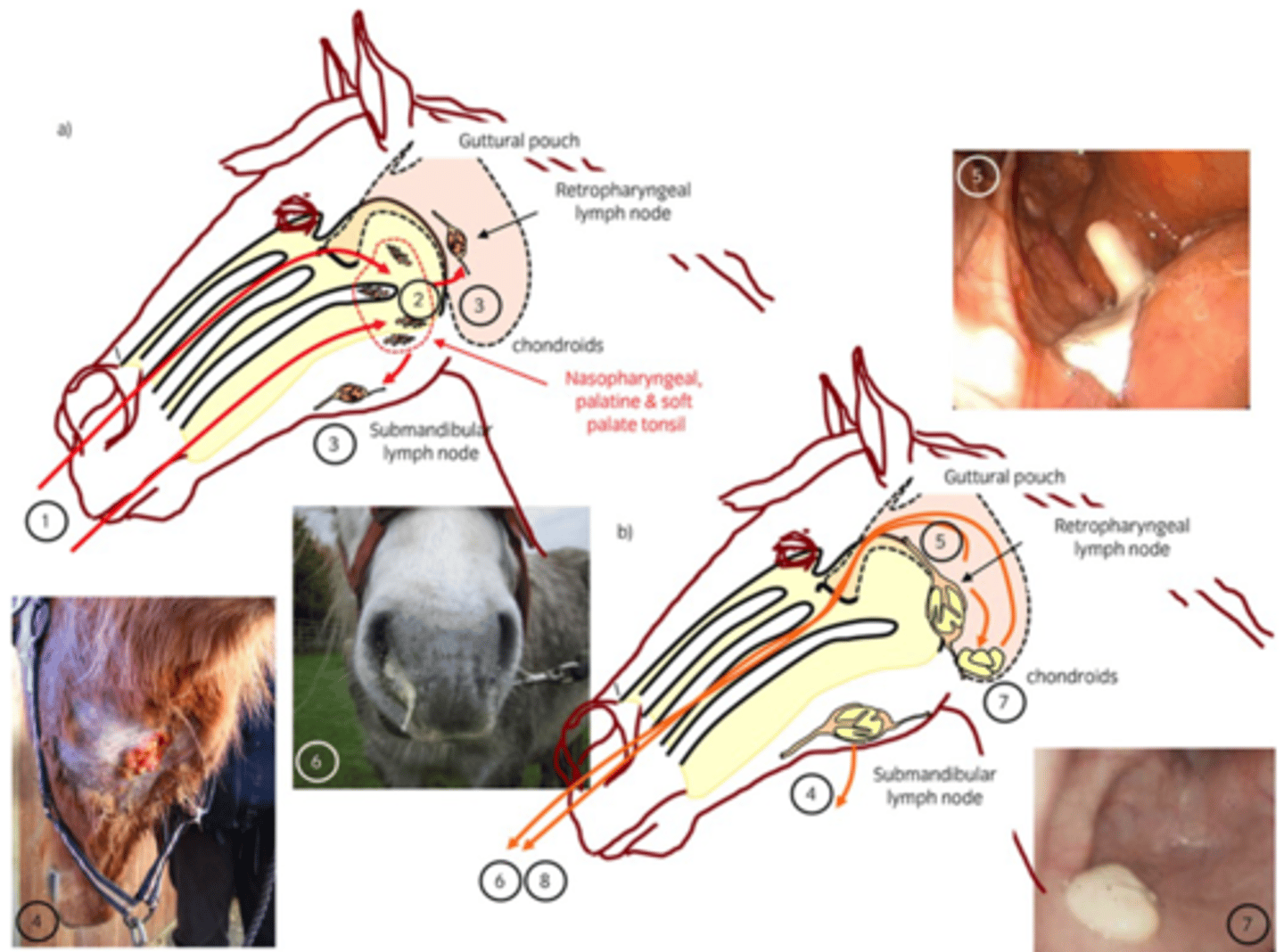
Describe the Pathogenesis of Strangles (Streptococcus Equi Equi)
Horse Gets coughed on → Breathed in → Nasal Cavity → Attaches to Tonsils → Moves to Lymph Nodes of the head (Mainly Retropharyngeal)→ Capsule Prevents Destruction → Inflammation → Neutrophils → Degranulation → Abscess → Abscess’s Rupture → Pus from nasal cavity
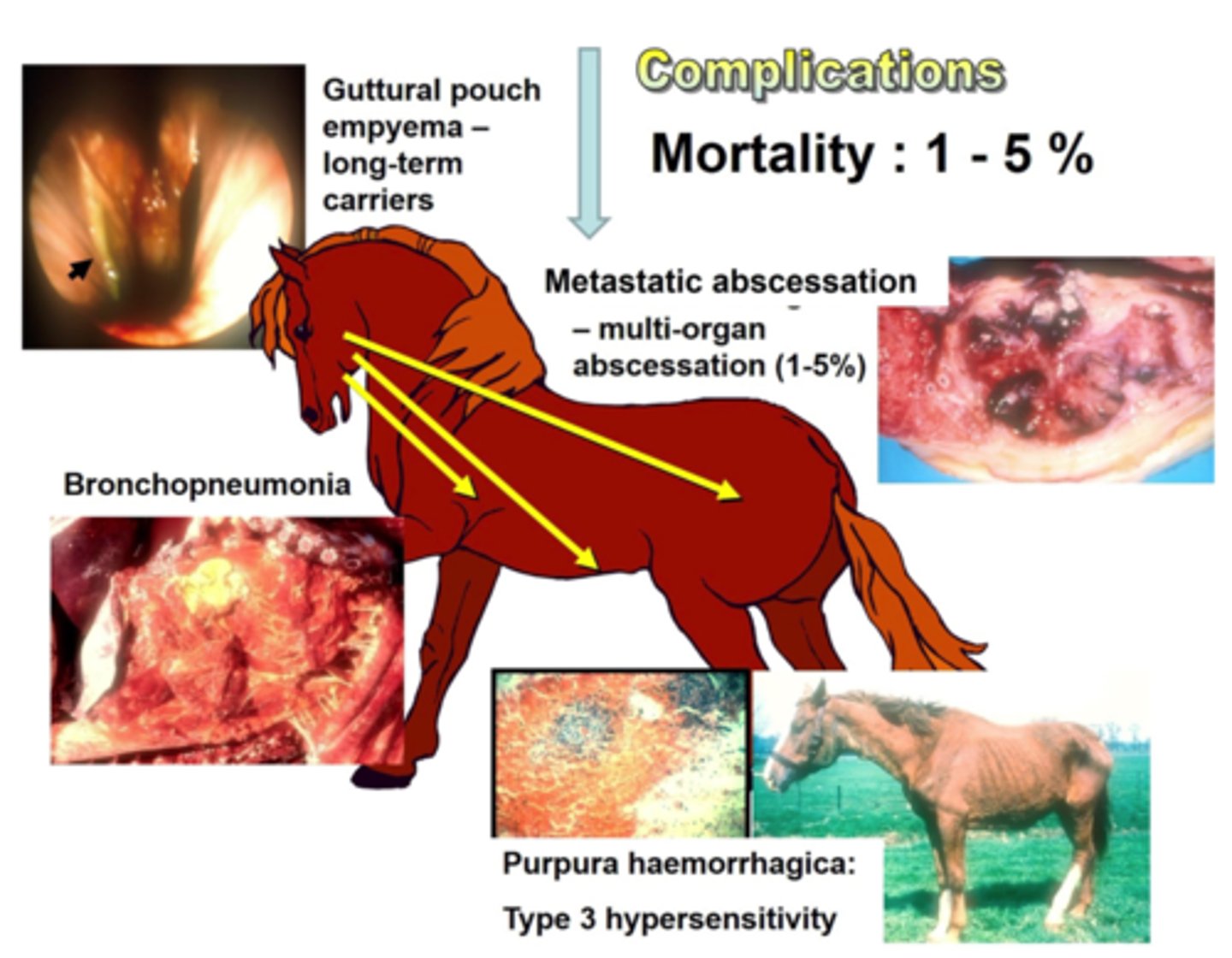
Describe the Complications that can occur with Strangles (Streptococcus Equi Equi) Infections
1. Abscess Rupture can lead to Bronchopneumonia/guttural pouch empyema (Long term Carriers)
2. Can spread throughout the Body (metastatic Strangles)
3. Purpura haemorrhagica (Type 3 Hypersensitivity)
Describe the Diagnosis and Control of Strangles (Streptococcus Equi Equi)
Diagnosis: - Diagnosed Via Guttural pouch flush and qPCR for Sem Gene
Control: Quarantine for 21 days after last case, use of antibiotics can interfere with immune mediated response (horses don’t become immune). Flush out guttural Pouch
Describe Streptococcus suis serotype 1 in terms of:
1. Transmission
2. What the Bacteria Causes
3. Clinical Signs
4. Zoonosis
1. Transmission via Resp/oral droplets
2. Causes neonatal (Pre weaning) septicemia, polyarthritis, and meningitis in 10-14 day old piglets
3. Nervous signs, fevers, haemorrhages
4. NIL
Describe Streptococcus suis serotype 2 (More Common) in terms of:
1. Transmission
2. What the Bacteria Causes
3. Zoonosis
1. Transmission via Resp/oral droplets
2. Cause pneumonia and sepsis in weaned/grower pigs (4-12 Weeks)
3. Zoonotic
Describe Streptococcus canis in cats/dogs/cows terms of:
1. Where Bacteria is Found
2. Pathogenesis
1. Normal Commensal of the Mucosa in Dogs, Opportunistic Pathogens
2. Disseminates from infection site to the rest of the body, can cause septicaemia. Can Rarely Cause Mastitis in Cows
Describe Streptococcus iniae in fish in terms of:
1. What the Bacteria Causes
2. Zoonosis
3. Transmission
1. Causes Sepsis, neuro signs, ulcers, erratic swimming
2. Can infect People causing localised infection at site of injury
3. Spread through cannibalism