thyroid hormones asynch-pharm
1/37
Earn XP
Description and Tags
pharm 2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
thyroid is located
in from of the esophagus
the thyroid gland is the. . .
largest endocrine glands
the thyroid controls
how quickly the body uses energy, makes proteins, controls how sensitive the body is to other hormones
the primary function of the thyroid is the
production of hormones T3, T4, and calcitonin
hypothalamus
regulates the anterior pituitary gland by releasing TRH
TRH
thyroid releasing hormone
TSH
thyroid stimulating hormone
anterior pituitary
regulates the thyroid gland by releasing TSH
they thyroid gland releases
T3 and T4
T3 and T4 normally
do negative feedback by acting on the hypothalamus
if someone has hypothyroidism, their TSH will be
high in the blood tests
if someone has hyperthyroidism, their TSH will be
low in the blood tests
steps of how T3 and T4 get released
the hypothalamus releases TRH
the TRH travels thru the portal venous system to get to the anterior pituitary
the anterior pituitary then releases TSH and it gets into the blood
TSH act on the thyroid gland
the thyroid then releases T3 and T4
T3 and T4 will travel back to the hypothalamus and will do negative feedback (in a normally functioning body)
iodine
is important for they thyroid gland→ needs iodine in order to produce a proper amount of thyroid hormone
if iodine is too low. . .
then the proper amount if thyroid hormone cannot be made
where are thyroid hormones produced?
within thyroid follicles that make up the thyroid gland
T4 is . . .
the precursor to T3
T3
triiodothyronine
T4
tetraiodothyronine
T3 is. . .
4 times more potent (so our bodies do not produce much of it)
T4 is produced
90% of the time
it is less potent and acts as a safeguard mechanism to decreased production of T3
they thyroid follicles are the. . .
main powerhouse of the thyroid gland
thyroid follicle structure
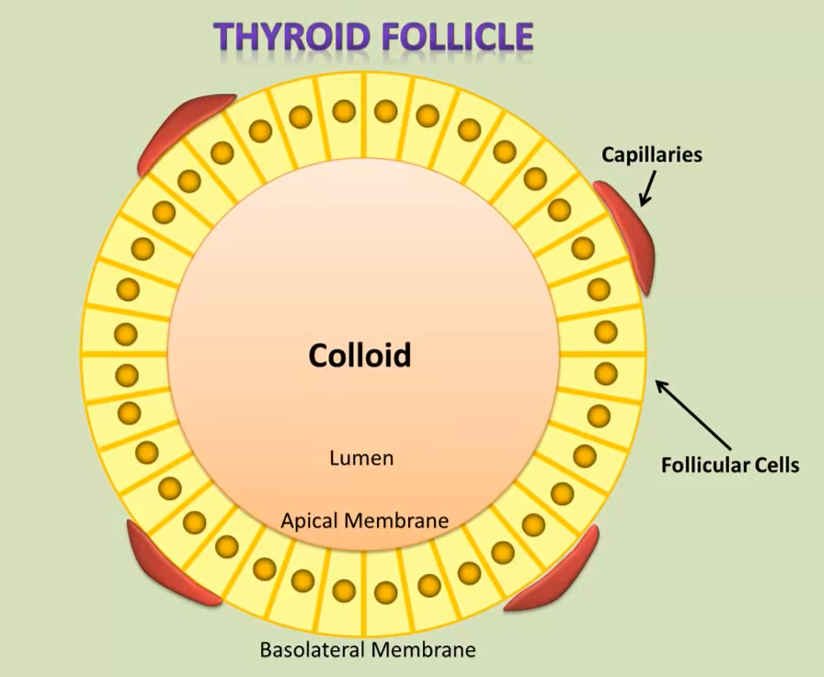
colloid of the the follicle
the center
where thyroid hormone (both precursors) are being produced
capillaries
where blood/amount of iodine comes in
capillaries face the
basolateral membrane of each cell
basolateral membrane
the outside of the follicle
apical membrane
faces the lumen
where do we get most of our iodine?
from iodized table salt (NaCl)
foods with the most iodine
dried seaweed
cod fish
cranberries
yogurt
baked potatoes
turkey breast
navy beans
tuna
strawberries
eggs
thyroid peroxidase
oxidized iodine
pendrin
a transporter that take iodine all the way across the cell/follicle and into the lumen
iodination
the process of how the thyroid hormone precursor and the iodine get together→ how they integrate→ how they combine
conjugation
losing H→ rings together
how the precursor hormone either gets 3 or 4 iodines to it
proteolysis
when the precursor splits and creates T3, T4
thyroglobulin
thyroid hormone precursor
Na/I symporter
ions are transferred in the same direction
iodine move in with sodium
how T3 and T4 are made
iodine is brought into the cell by the capillaries dumping iodine to the Na/I symporter
the Na/I symporter brings in both iodine and sodium into the cell
the iodine gets shuttles across the cell to Pendrin
Pendrin then pumps iodine into the lumen of the follicle cell
once iodine is in the lumen, it is oxidized by thyroid peroxidase
at the same time, the follicular cell’s ER is budding off and it contains thyroglobin and gets exocytosed into the lumen at the same time as iodine
the thyrogloubin and oxidized iodine combine in the lumen
they undergo conjugation
they get endocytosed into the cell again
they then undergo proteolysis where the precursor gets split into T3 and T4
T3 and T4 are then dumped into the blood stream