PC1 - Asthma
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
FEV1
forced expiratory volume in 1 second
FVC
forced vital capacity - amount of gas that can be forcibly and rapidly exhaled after a full inspiration
"Emptying the tank"
Asthma
Complex disorder that affects airways of the lung, characterized by variable and recurring respiratory symptoms, airflow obstruction, bronchial hyperresponsiveness, and underlying inflammation.
4 different types of asthma
• Allergic
• Aspirin-sensitive
• Neutrophilic
• Exercise-induced
T/F Asthma is one of the most common, chronic, noncommunicable diseases in the world.
True
What medications can trigger asthma
aspirin, NSAIDs, beta blockers
What viral respiratory infections can cause asthma and worsen it?
RSV, Influenza, COVID-19
Clinical presentation of asthma
Coughing, wheezing, chest tightness, shortness of breath
Asthma action plan personal best PEF (L/min)
Green: 80-100%
Yellow: 50-80%
Red: <50%
What plans are made for the asthma action plan?
• maintenance
• exercise
• exacerbation
• emergency
Risk factors for asthma exacerbation
Medications
• SABA overuse (≥3 x 200-dose canisters/year)
• inadequate ICS (not prescribed, poor adherence, wrong techn.)
Comorbidities
• obesity, chronic sinusitis, GERD, pregnancy
Exposures
• smoking, e-cig, vaping, air pollution
Setting
• Psychological/socioeconomic problems
PMH
• ≥ 1 severe exacerbation in past year
• intubation/intensive care for asthma treatment.
Lung f(x)
• Low FEV1, <60% predicted, high bronchodilator responsiveness
Spirometry
Pulmonary function test that measure lung volumes and airflow
Asthma or COPD diagnosis
• FEV1/Predicted FEV1 <70%
• Pre-bronchodilator FEV1/FVC <70%
Spirometry procedure
1. Pt seated upright and understands procedure
2. Explain importance of tight seal around mouthpiece
3. Instruct pt to take deep, full breath in.
4. Exhale forcefully and as quick as possible into spirometer
5. Repeat at least 3 times for reproducibility and accuracy
Asthma diagnosis reversibility
Post-bronchdilator FEV1 increases ≥12% and ≥200 mL OR
Post-bronchodilator PEF increases ≥20%
Most frequent finding in asthma physical exam?
Wheezing on auscultation
Bronchodilator reversibility test
1. Forcefully exhale (preFEV1/FVC)
2. Bronchodilator
3. Wait ~15 min
4. Forcefully exhale (postFEV1/FVC)
• compare pre and post
- reversible if FEV1 or FVC ≥12% and ≥200 mL
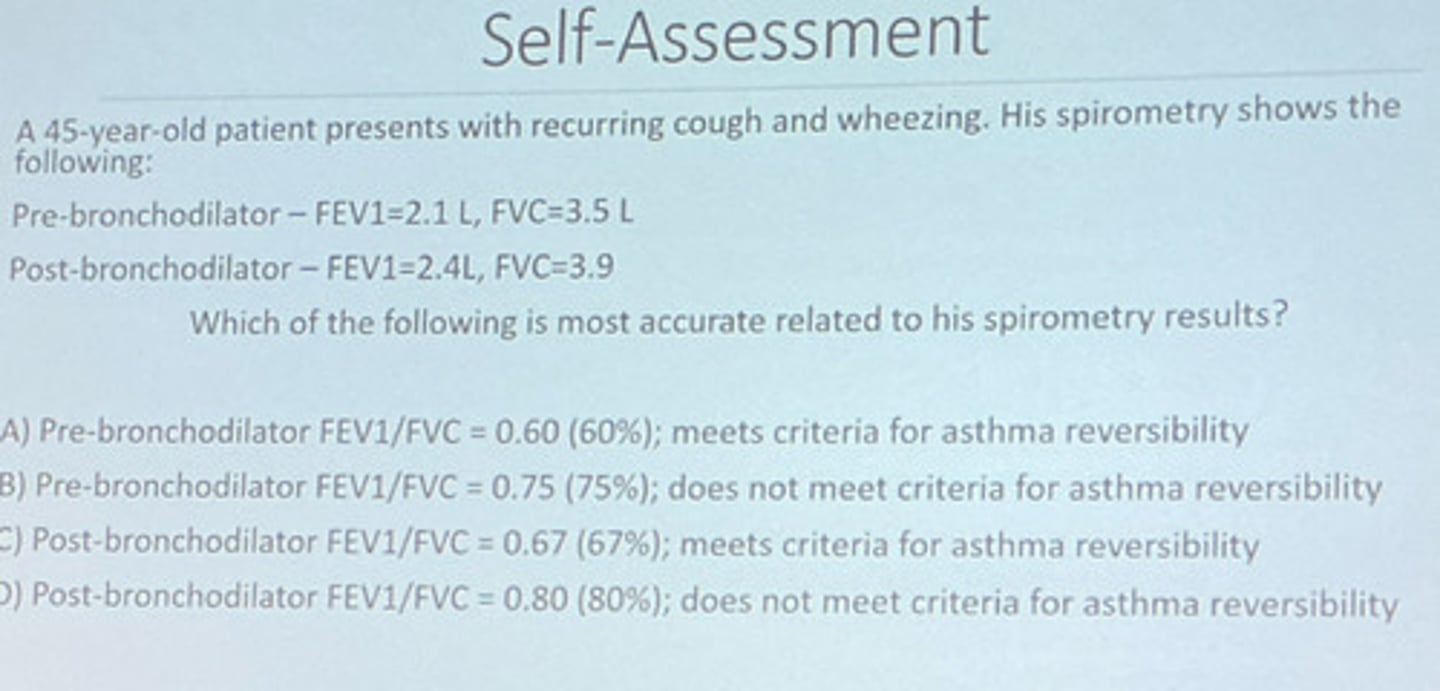
A 45-y.o patient presents with recurring cough and wheezing. His spirometry shows:
Pre-bronchodilator - FEV1=2.1 L; FVC = 3.5 L
Post-bronchodilator - FEV1 = 2.4 L; FVC = 3.9 L
Which of the following is most accurate related to his spirometry results?
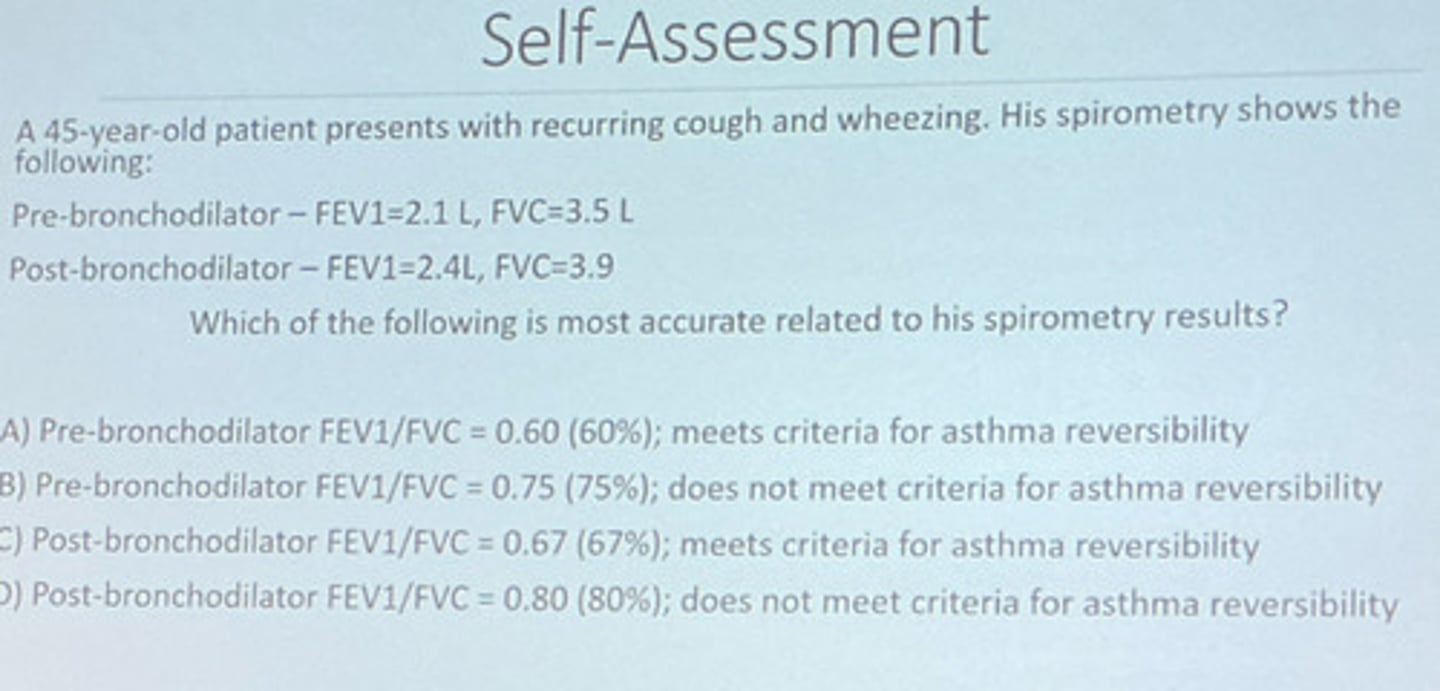
A. Pre-bronchodilator FEV1/FVC = 0.6(60%); meets criteria for asthma reversibility
B. Pre-bronchodilator FEV1/FVC = 0.75 (75%); does not meet criteria for asthma reversibility
C. Post-bronchodilator FEV1/FVC = 0.67 (67%); meets criteria for asthma r
A. Pre-bronchodilator FEV1/FVC = 0.6(60%); meets criteria for asthma reversibility
Asthma guidelines
NAEPP (last updated 2020) - National Asthma Education and Prevention Program
Key concepts
• SMART
• Asthma severity classification
- intermittent, mild, moderate, severe
GINA
Global Initiative for Asthma (annually updated)
• prioritizes symptom presentation
Key concepts
• terminology - AIR, MART
• two treatment tracks
• SMART
• various relief inhalers
Treatment goals for asthma
1. Control short and long-term symptoms
2. Prevent exacerbation
3. Prevent airway damage
4. Prevent medication s/e
Bronchodilators
SABA
• Short-acting Beta-2 agonist
ICS
• inhaled corticosteroid
ICS + LABA
LAMA
Leukotriene Receptor antagonist
Montelukast
Zileuton
Antibiotics (asthma management)
Azithromycin
Biologics
Omalizumab
Mepolizumab
Reslizumab
Benralizumab
Dupilumab
Tezepelumab
Systemic corticosteroids
Prednisone
Prednisolone
Methylprednisolone
SABA
MOA - Relaxes bronchial smooth muscle (duration ~4-6h)
Quick relief of symptoms and acute bronchospasms + pre-treatment for exercise
Albuterol
Levalbuterol
Proair Digihaler, Proair Respiclick, Proventil HFA, Ventolin HFA
Albuterol
SABA
MDI, DPI - 90, 117, 120 mcg
1-2 puffs q4-6h PRN
A/e: tremor, tachycardia (tachyphylaxis), increased airway responsiveness, decreased effectiveness with beta blockers
Xopenex HFA (MDI)
Levalbuterol
SABA
- MDI - 45 mcg; 1-2 puffs q4-6h PRN
- Nebulizer - 0.63 mg/3mL (0.021%) 1 unit q6-8h PRN
- 1.25 mg/3mL (0.042%)
A/e: tremor, tachycardia (tachyphylaxis), increased airway responsiveness, decreased effectiveness with beta blockers
ICS
• MOA - suppresses multiple inflammatory processes characteristic of asthma w/i airways
• Place in therapy - ALWAYS included in asthma regimens
- decreases airway responsiveness and symptoms
- increases lung function
• inhaled a/e - oral candidiasis - thrush; dysphonia (hoarse voice)
• systemic a/e - osteoporosis (chronic use), cataracts, glaucoma
LABA
• MOA - relaxes bronchial smooth muscle (duration: ~12-24 hours)
• place in therapy: Combined w/ ICS -> ICS+LABA
• NEVER use LABA w/o ICS
BBW: increased risk of asthma-related deaths in LABA monotherapy.
Advair Diskus, Wixela Inhub (generic)
ICS + LABA
Fluticasone Propionate + Salmeterol (DPI)
A/e = tachycardia, h/a, decreased effectiveness w/ B-blockers
Airduo respiclick
ICS + LABA
Fluticasone propionate + Salmeterol (MDI)
A/e = tachycardia, h/a, decreased effectiveness w/ B-blockers
Advair HFA
ICS + LABA
Fluticasone Propionate + Salmeterol xinfoate (MDI)
A/e = tachycardia, h/a, decreased effectiveness w/ B-blockers
Breo Ellipta
ICS + LABA
Fluticasone Furoate + Vilanterol (SMI)
A/e = tachycardia, h/a, decreased effectiveness w/ B-blockers
Symbicort, Breyna
ICS + LABA
Budesonide + Formoterol Fumarate (MDI)
A/e = tachycardia, h/a, decreased effectiveness w/ B-blockers
Dulera
ICS + LABA
Mometasone Furoate + Formoterol Fumarate (MDI)
A/e = tachycardia, h/a, decreased effectiveness w/ B-blockers
Qvar Redihaler
ICS
Beclomethasone dipropionate - MDI
Low dose 100-200
Medium dose >200-400
High dose >400
Pulmicort Flexhaler (DPI)
Pulmicort Respules (Neb)
ICS
Budesonide
LD: 200-400
MD: >400-800
HD: >800
Alvesco HFA (MDI)
ICS
Ciclesonide
LD: 80-160
MD: >160-320
HD: >320
Arnuity Ellipta (SMI)
ICS
Fluticasone Furoate
LD + MD: 100
HD: 200
ArmonAir Respiclick
fluticasone propionate (ICS)
LD: 100-250
MD: >250-500
HD: >500
Asmanex HFA (MDI)
Asmanex Twisthaler (DPI)
Mometasone Furoate (ICS)
HFA
• LD-MD: 200-400
• HD: 400
Twisthaler
• LD: 110-220
• MD: >220-440
• HD: >440
Atrovent HFA
Ipatropium - SAMA
AirSupra
Albuterol and budesonide (SABA/ICS)
Combivent Respimat
albuterol/ipratropium bromide (SABA+SAMA)
DuoNeb
albuterol sulfate/ipratropium bromide (SABA+SAMA)
Wixela Inhub
Fluticasone propionate/Salmeterol xinfoate (ICS/LABA)
Triple Therapy
ICS - LABA - LAMA
Trelegy Ellipta (Fluticasone, vilanterol, umeclidinium)
Breztri Aerosphere (budesonide, glycopyrrolate, formoterol fumarate)
- Breztri not indicated for asthma
Incruse Ellipta
Umeclidinium (LAMA)
Lonhala Magnair
Glycopyrrolate (LAMA)
Spiriva handihaler
tiotropium (LAMA)
SMI
1.25 mcg; 2 puffs daily
A/e: dry mouth, urinary retention
Tudorza Pressair
Aclidinium bromide (LAMA)
Yupelri Neb
Revefenacin (LAMA)
Brovana Neb
Arformoterol (LABA)
Perforomist Neb
Formoterol fumarate dihydrate (LABA)
Serevent diskus
Salmeterol xinafoate(LABA)
Striverdi respimat
Olodaterol HCl(LABA)
Cinqair
Reslizumab
Dupixent
Dupilumab
Fasenra
Benralizumab
Nucala
Mepolizumab
Tezspire
Tezepelumab-ekko
Xolair
Omalizumab
Singulair
Montelukast sodium (Leukotriene inhibitor)
Asthma
10 mg PO once every evening
FDA warning - serious neuropsychiatric events such as suicidal thoughts or action have been reported.
Zyflo
Zileuton (Leukotriene Inhibitor)
600 mg CR PO BID w/i 1 hour of meals
Elevated LFTs
LAMA
MOA: Blocks acetylcholine bronchoconstrictor effect on airway smooth muscle.
Place in therapy: Step 5 (severe) or triple combination inhaler
Comments: Modest improvement in lung function, but not asthma symptoms.
Zithromax
Azithromycin
MOA: antibacterial, antiviral and anti-inflammatory effects limiting mucus airway secretions
Dosing: 500 mg PO TIW ≥ 6 months
Place in therapy: Severe asthma only after specialist referral in persistent symptoms
A/e: elevated LFTS, tinnitus (long-term use), abdominal pain
Concern for increased Ab resistance.
Prior to therapy with Zithromax, screen for:
Baseline hearing
QTc prolongation
Major drug-drug interaction
Fasenra
Benralizumab
IL-5 antagonist for asthma w/ eosinophilia
30 mg Subcutaneous monthly
A/e Injection site reaction
Cinqair
Reslizumab
Anti-IL-5; depletes eosinophils
3 mg/kg IV monthly
Indicated for severe eosinophilic asthma
BBW for anaphylaxis
Nucala
Mepolizumab
Binds IL-5 and depletes eosinophils
100 mg subcutaneous monthly
Indicated for severe eosinophilic asthma
Injection site reaction
Dupixent
Dupilumab
Inhibits IL-4, 13 signaling in B, CD4, T cells, smooth muscle
300 mg subcutaneous every 2 weeks
Indicated for severe eosinophilic asthma, OC-dependent asthma.
Injection site reaction
Xolair
Omalizumab
Binds IgE, inhibiting mast cell, basophil binding
75-375 mg subcutaneous every 2-4 weeks
Indicated for severe allergic asthma
BBW for anaphylaxis
Tezspire
Tezepelumab-ekko
Blocks thymic stromal lymphopoietin-reducing inflammatory cytokines
210 mg subcut monthly
Indicated for severe asthma
Injection site reactions
Prelone
Prednisone (systemic corticosteroid)
Omnipred, Orapred
Prednisolone (systemic corticosteroid)
A/e of systemic corticosteroid
Short term: insomnia, hyperglycemia, mood changes
Maintenance: cataracts, glaucoma, HTN, T2DM, adrenal suppression, osteoporosis.
Major drug-drug interaction w/ Systemic corticosteroids
Ritonavir - metabolism boosting agent
Ketoconazole
Itraconazole
T/F: Aminophylline and theophylline are recommended in asthma
False
- previously recommended oral bronchodilator
- life-threatening s/e at high doses.
- lack of efficacy
General principles of treating asthma
• Avoid SABA and LABA monotherapy
• always include ICS
• relief inhaler options
Why is SABA and LABA monotherapy avoided in treating asthma?
- exacerbation
- asthma related death
- reduced bronchodilator response
- allergic response
Relief inhaler options in treating asthma
• SMART rescue inhaler
- ICS - formoterol
• combination rescue inhaler
- ICS - SABA
• maintenance inhaler + rescue inhaler
- ICS + SABA
____ is utilized as a SMART alternative in the USA but it has not been studied or approved by NAEPP or GINA
Dulera