FOPC Exam Two
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
127 Terms
Fryette’s Principles
Principle I: When the spine is in neutral, sidebending to one side will be accompanied by horizontal rotation to the opposite side. This law is observed in type I somatic dysfunction, where more than one vertebra is out of alignment and cannot be returned to neutral by flexion or extension of the vertebrae. The involved group of vertebrae demonstrates a coupled relationship between sidebending and rotation. When the spine is neutral, side bending forces are applied to a group of typical vertebrae and the entire group will rotate toward the opposite side: the side of produced convexity. Extreme type I dysfunction is similar to scoliosis.
Principle II: When the spine is in a flexed or extended position (non-neutral), sidebending to one side will be accompanied by rotation to the same side. This law is observed in type II somatic dysfunction, where only one vertebral segment is restricted in motion and becomes much worse on flexion or extension. There will be rotation and sidebending in the same direction when this dysfunction is present.
Principle III: When motion is introduced in one plane it will modify (reduce) motion in the other two planes. The third principle sums up the other two laws by stating dysfunction in one plane will negatively affect all other planes of motion.
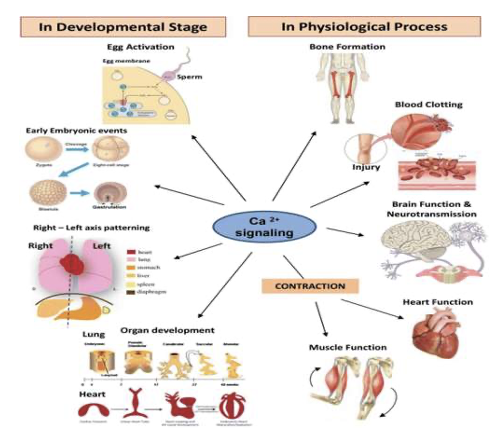
What are some ways calcium is used in the body and how do we increase/decrease this level?
PTH - increase levels
Calcitonin - decrease levels
Calcium is used for many different functions
Muscle contraction
Nerve transmission
Vascular Function
Coagulation
Intracellular signaling
Hormonal Secretion
Bone Structure
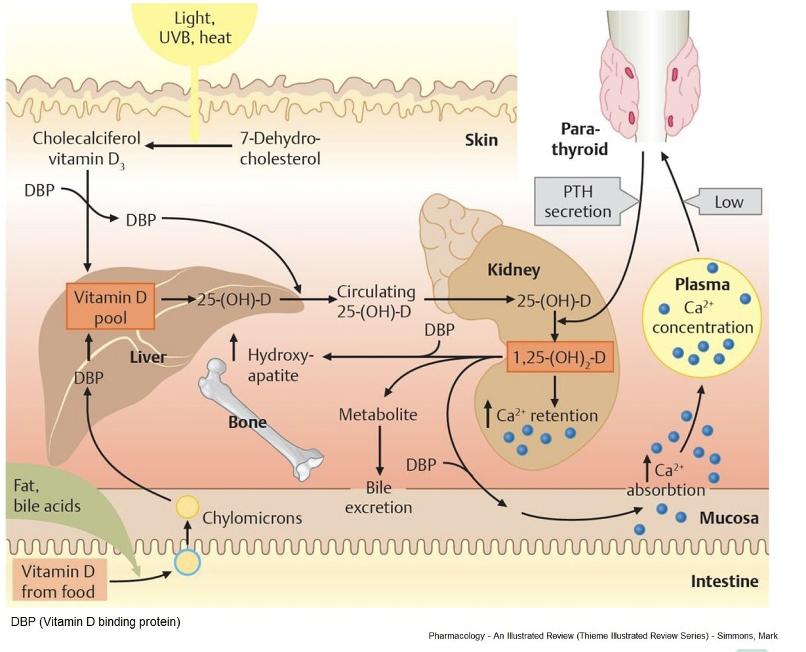
Vitamin D is required of the _______________________ of the dietary calcium.
the absorption of 75%
Vitamin D Metabolism Mechanism
What is a DEXA scan used for?
To determine Osteoporosis
If your T-score is: 1 or higher, your bone is healthy. –1 to –2.5, you have osteopenia, a less severe form of low bone mineral density than osteoporosis. –2.5 or lower, you might have osteoporosis.
Most common place to take a DEXA is in the spine, hip, or femur
What are some risk factors for osteoporosis?
Post menopausal women that are older than 65
Post menopausal women that are younger than 65 with high risk factors
After a fracture
Most common fx in osteoporosis hip, femur, wrist
Estrogen
ie; hormone replacement therapy
Low body mass index = not enough stress, not putting as much bone down, we need lipids to help absorb vitamin d
Alcohol = drinking calories
Tobacco = appetite suppressant
Clinical conditions/medications = long term steriod use, proton pump inhibitors (prilosec)
Rickett’s
Vitamin D Deficiency in children
Osteomalacia
Vitamin D Deficiency in adults
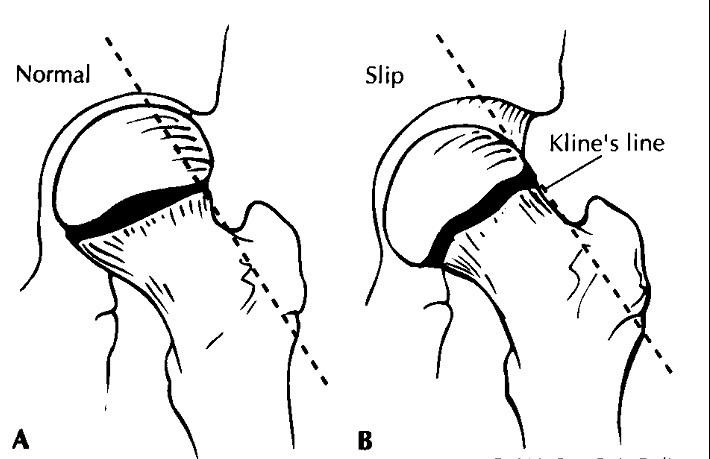
Trethowan's sign
Trethowan's sign is positive in slipped femoral epiphysis. If an anteroposterior view of the hip joint is taken then a line drawn along the superior surface of the neck should pass through the femoral head. If the line remains superior to the femoral head then this is termed Trethowan's sign.
Legg-Calve-Perthes Disease
Legg-Calve-Perthes disease (also known as Perthes disease) is a rare condition in which the ball-shaped head of the thighbone (femoral head) temporarily loses its blood supply. As a result, the head of the thighbone collapses, the femoral head becomes flat, and the area becomes inflamed and irritated.
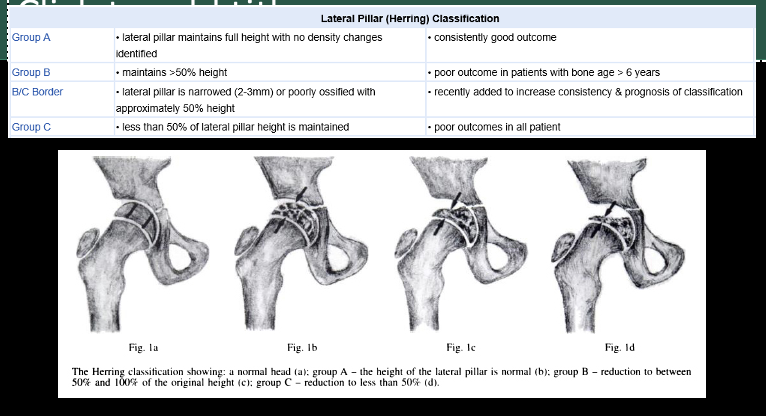
Lateral Pillar (Herring) Classification
Used for diagnosing LCPD
Ottowa Knee Rules
Age >55 years
Isolated patellar tenderness
Tenderness at the head of fibula
Inability to flex knee 90 degrees
Inability to bear weight (4 steps) immediately after injury
Ottawa Ankle Rules
Point tenderness over the posterior edge or tip of the malleolus
Inability to bear weight (4 steps) after the injury
Age >55 years
Point tenderness at the base of the fifth metatarsal
Point tenderness at the navicular
Inability to bear weight (4 steps) immediately after the injury
What is the most common complaint for the PCC and ER?
Back pain
What should you worry about with Bladder or Bowel Dysfunction, Saddle anesthesia?
Cauda Equina Syndrome
What are some red flags when a patient comes in for back pain?
Age <20 or >50
History of cancer
Unexplained weight loss, fever, or decline in general health
Pain lasting more than 1 month or not responding to treatment
Pain at night or present at rest
History of IV drug use, addiction, or immunosuppression
Presence of active infection or HIV infection
Long-term steroid therapy
Saddle anesthesia or bowel or bladder incontinence
Neuro symptoms
Torticollis
It is contracture of the Sternocleidomastoid muscle, SCM, unilaterally that results in abnormal positioning of the head.
Congenital vs Acquired Torticollis
Congenital Torticollis
Congenital muscular Torticollis is the most common kind of torticollis in children. The prevalence is 0.3%-2% of newborns in the US
Believed to be due to intrauterine positioning or trauma to the soft tissue resulting in ischemia of the SCM and eventual fibrosis
It occurs more often in breech presentation.
Difficult w/ vertex delivery
It is associated with hip dysplasia in 10-20% of affected children
Although it is congenital, it may not appear until 2-4 weeks of age
During the first 4-6 weeks, a firm, nontender mobile mass may appear at SCM body due to hematoma. It regresses gradually by 6 months of age
Torticollis resolves spontaneously in most infants by 1-2 years of age.
If it persists, surgical release of the contracted muscle may be required
Acquired Torticollis
Much more common in older children
Usually due to infection, like cervical lymphadenitis, retropharyngeal abscess, myositis, or even URI
It can also happen due to trauma
Benign paroxysmal torticollis can happen between 1-5 years of life. Familial tendency is noted
Treatment depends on etiology
Scoliosis
Any lateral curvature of the spine that measures more than 10˚ as determined on an upright posteroanterior, PA, radiograph of the spine
Unlike Kyphosis or Lordosis which are curvatures seen on the lateral plane of the spine
It can be congenital, neuromuscular or idiopathic
Some scoliosis can cause secondary complications/associations such as heart disease and asthma
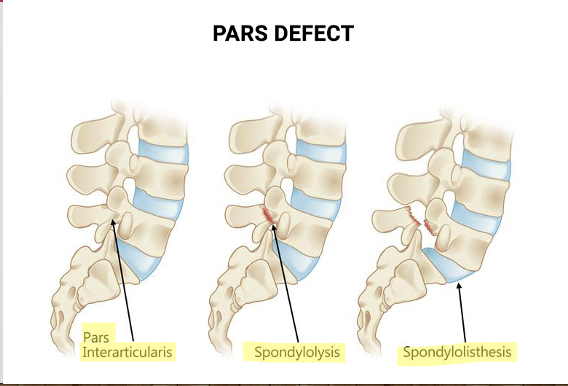
Types of Pars Defects
What is the most common scoliosis curve seen by physcians?
Right Thoracic Single Curve
Congenital vs Acquired Scoliosis Occurrence
Congenital scoliosis affects boys more than girls, and is associated with other abnormalities
Scoliosis that begins in childhood affects boys and girls equally
Scoliosis Prognosis
Most mild idiopathic scoliosis in children resolve spontaneously
Moderate scoliosis, 20-30 degrees needs exercise and close observation
Severe scoliosis, > 30 degrees needs referral to Orthopedics
Brachial Plexus Palsy or “Erb’s Palsy”
It usually occurs in cases of shoulder dystocia, Infant weight > 4 kg, diabetic mother and other causes of cephalopelvic disproportion
C-Section and twin or triplet deliveries are protective from BPP
The usual position of the arm is shoulder adduction, forearm pronation, wrist and fingers flexion ( Arthur)
80% of affected children recover completely, 20% will have some functional arm deficit
Nursemaid’s Elbow
Subluxation of the proximal radial epiphysis due to a tear in the annular ligament at its attachment to the radius. A portion of the ligament gets trapped in the joint
It usually happens when there is hyperextension of the forearm
It presents with sudden extension and hyperpronation of the forearm
It can be corrected by active hyperextension and supine positioning of the affected forearm
Polydactyly
Extra digits, Polydactyly, can be seen at the hands in one of two positions:
1. Attached to the fifth finger. It is benign and can be removed by tight suturing at the base of the digit. It falls off spontaneously in a few days.
2. Attached to the thumb. In this case, it usually is associated with other deformities, like renal abnormalities. Comprehensive evaluation should be carried out. The abnormal digit needs to be surgically removed.
Hip Dysplasia (Cause, Occurrence, Diagnosis, Treatment)
Shallow acetabulum causes subluxation or complete dislocation of the femoral head
Acetabulum is abnormally shallow
Occurrence is markedly different among locations, genetics and sex.
It occurs in females 7 times more than males due to intrauterine estrogen-induced ligamentous laxity
Diagnosis can be done via:
Ortolani test: Performed to return a dislocated femoral head into the acetabulum
Barlow test: To check to see if a normally placed femoral head is dislocatable
Galeazzi test: to check the asymmetry of the height of the knees when the child is lying supine, and the hips are placed in 90 degrees of flexion
Management
The goal of treatment is to keep the hip in abduction as early as possible so that the femoral head remains at the acetabulum.
The Pavlik harness is the most commonly used device worldwide
Closed reduction by well molded spica cast
Surgical correction
Hip Dysplasia Prognosis
Depends on the time of diagnosis and severity of the deformity
Generally, unilateral hip dysplasia has worse prognosis than if it is bilateral
Bowlegs and Knock-Knees Evaluation
Evaluation for pathologic bowlegs is required if the intercondylar distance (i.e., distance between the knees) is more than 10 cm when the child is lying supine, and the malleoli are touching
Evaluation for pathologic knock-knees is required if the intermalleolar distance (i.e., the distance between the ankles) is more than 10 cm with the child lying supine and the knees are touching
In-Toeing & Out-Toeing
These deformities are the results of internal or lateral tibial torsions
In-toeing after the second year of life is usually due to femoral internal torsion
Out-toeing is almost always due to lateral tibial torsion
The shape of the feet remains normal
Metatarsus Adductus & Abductus
The forefront of the foot is curves inward along the tarso-metatarsal joint
Occurs in 1/500 birth
It causes in-toeing in neonates and young infants
It is part of the clubfoot deformity
In abductus, the forefront of the foot is curved laterally along the tarso-metatarsal joint. It is rarely an isolated condition.
Clubfoot Diagnosis
Congenital abnormality of the foot that is usually an isolated deformity or part of other neuromuscular abnormalities, amniotic band syndrome, arthrogryposis etc.
The diagnosis is based on three conditions: forefoot varus, heel varus, and ankle equinus
It can be a rigid or nonrigid deformity in which the forefront can be gently brought to the midline
Clubfoot Management
Clubfoot is a pathologic condition that requires treatment since the first week after birth
Serial manipulation and foot casting for several months is the first step
Surgery is required in 50-75% of cases and is performed at 6-12 months of age
Different surgical procedures “a la carte” are performed depending on the type and severity of the deformity
What conditions cause dystocia? (Dystocia = difficult birth)
Clavicle fracture, BPP, cephalhematoma = dystocia
Adam’s Forward Bend
Purpose: Used to screen for scoliosis, a condition involving abnormal curvature of the spine.
Procedure: The patient bends forward at the waist with arms hanging down, and the examiner observes the curvature of the spine.
Straight Leg Raise Test
Purpose: To assess for nerve impingement or disc herniation in the lower back.
Procedure: The patient lies on their back, and one leg is raised with the knee extended. Pain or radiation into the leg during this maneuver suggests nerve compression.
Braggard’s Test
Purpose: A variation of the SLR test to further evaluate sciatic nerve compression.
Procedure: Similar to the SLR test, but the examiner dorsiflexes the patient's foot (pulls the toes up) while keeping the knee extended. This may provoke pain or symptoms.
Valgus Stress Test (Knee & Ankle)
Purpose: Assesses the stability of the knee and ankle joint by applying a valgus (inward) force.
Procedure: The examiner applies a lateral force to the joint while stabilizing the opposite side.
Varus Stress Test (Knee & Ankle)
Purpose: Assesses the stability of the knee and ankle joint by applying a varus (outward) force.
Procedure: The examiner applies a medial force to the joint while stabilizing the opposite side.
Squeeze Test
Purpose: Used to evaluate pain and instability in the ankle joint
Procedure: The patient lies on their back, and the examiner compresses the thigh by squeezing. Pain or instability indicates potential issues.
Apley Distraction/Compression Test
Purpose: Helps assess joint instability, especially in the knee.
Procedure: Two versions - distraction (joint is pulled apart) and compression (joint is compressed). These tests are used to assess shoulder pain and instability.
Anterior Drawer Test
Purpose: Assesses anterior cruciate ligament (ACL) injuries in the knee and ligament injuries in the ankle.
Procedure: The examiner applies anterior force to the joint to assess for abnormal movement.
Posterior Drawer Test
Purpose: Assesses posterior cruciate ligament (PCL) injuries in the knee.
Procedure: The examiner pushes the tibia backward to assess posterior movement.
Lachman’s Test
Purpose: A specific test for ACL injury.
Procedure: The examiner stabilizes the femur while pulling on the tibia to assess anterior movement.
Ballotment Test
Purpose: Detects knee effusion (excess fluid in the knee joint).
Procedure: The examiner pushes the patella downward to assess for fluid movement.
McMurray’s Test
Purpose: Detects meniscal tears in the knee.
Procedure: The examiner rotates the tibia while extending and flexing the knee to elicit pain or clicking.
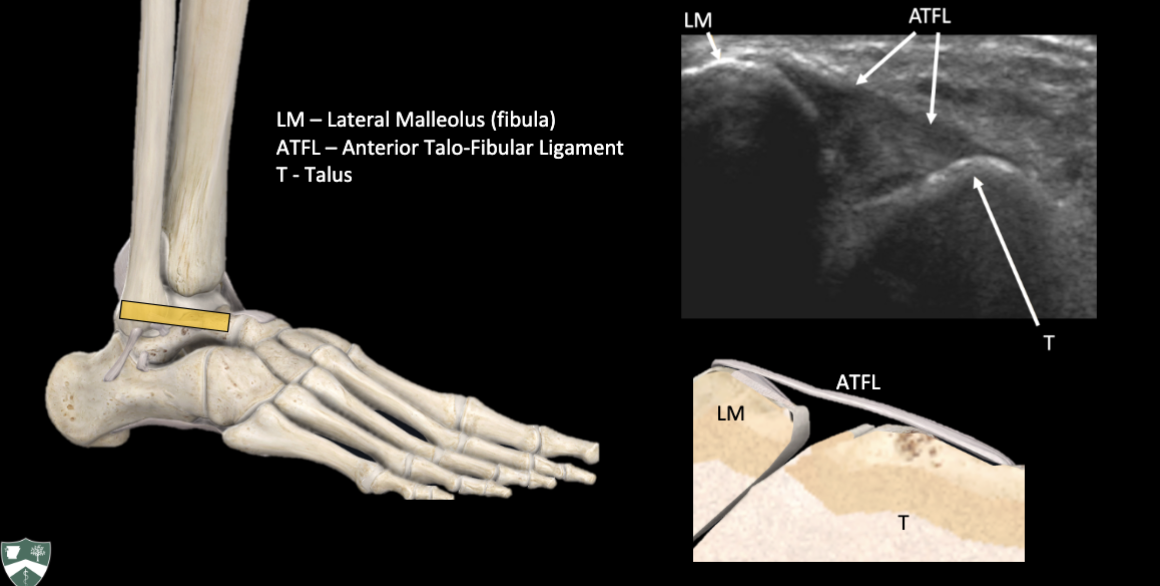
ATFL Ultrasound
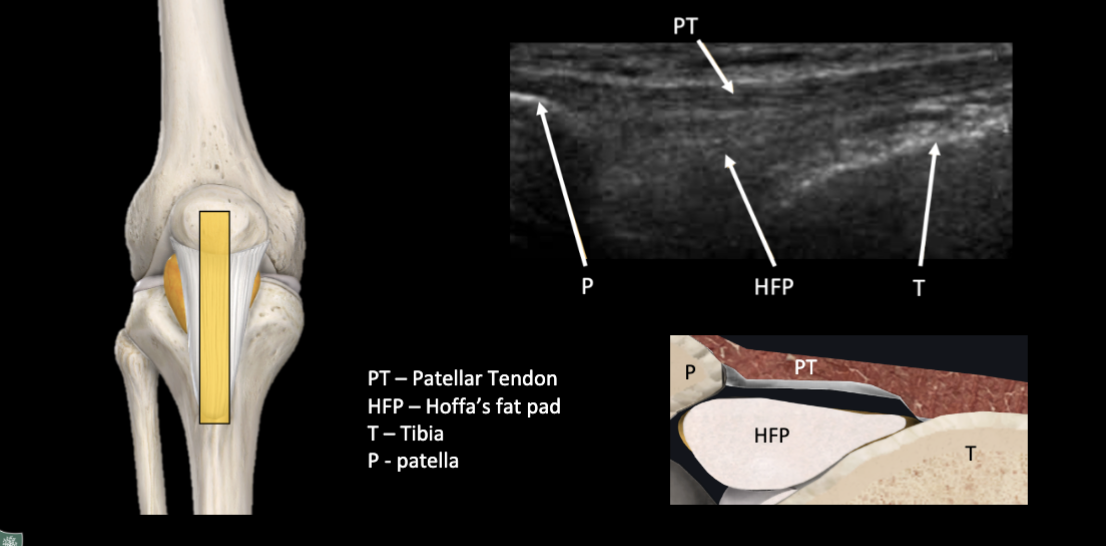
Patellar Tendon Ultrasound
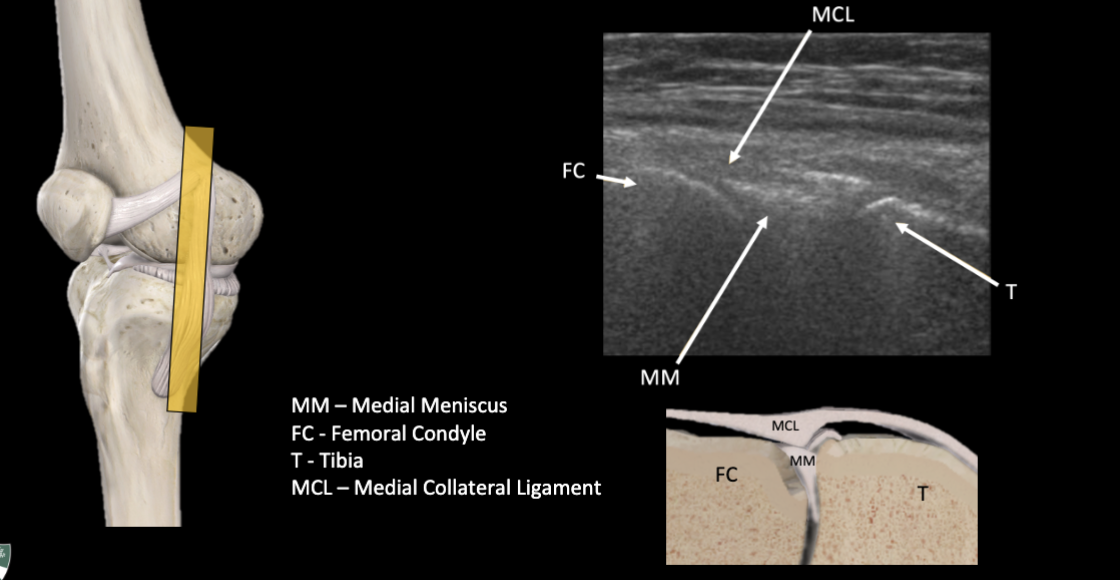
Medial Meniscus Ultrasound
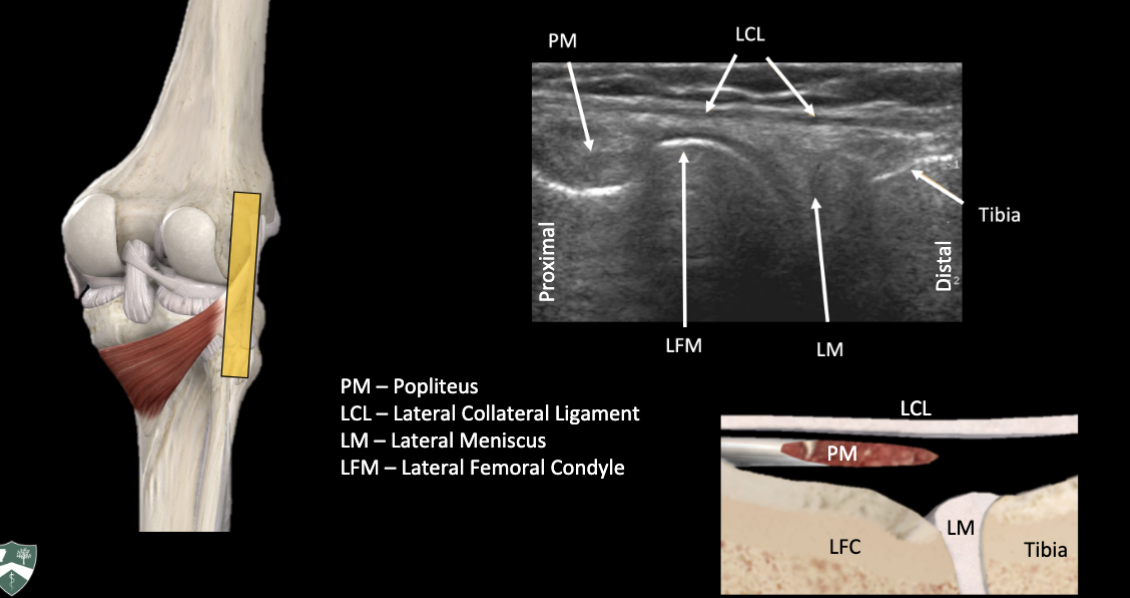
Lateral Meniscus, Lateral Collateral Ligament, Popliteus Tendon Ultrasound
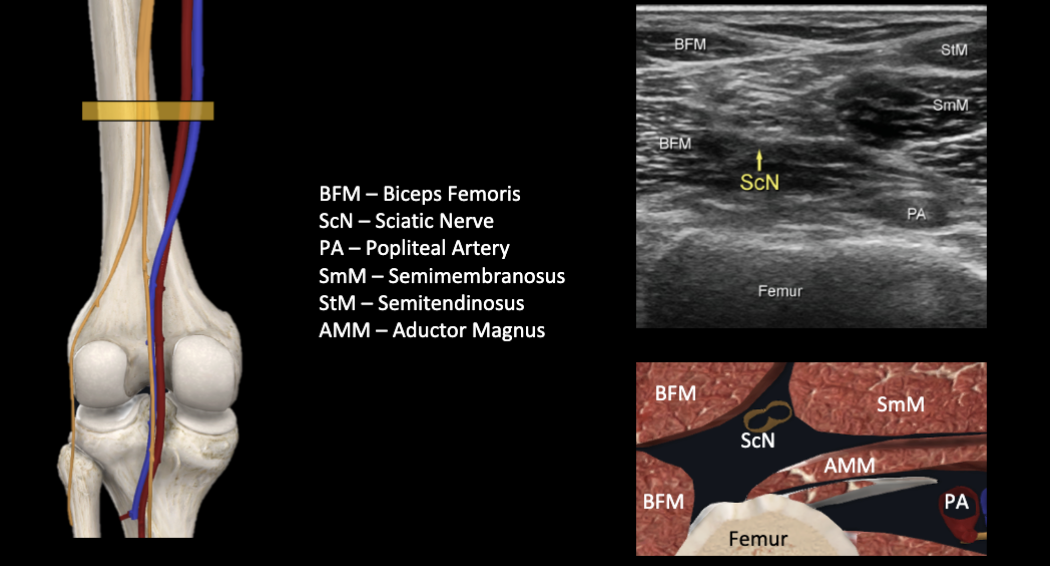
Sciatic Nerve Ultrasound
Log Roll Test
The log roll test is a physical exam technique for hip disorders. It's used to assess the integrity of the hip joint and help identify potential hip pathology such as: Labral tears, Ligament laxity.
To perform the log roll test, the examiner:
Grasps the mid thigh and calf
Gently rolls the thigh internally and externally
Attempts to move the limb into maximal range of motion
A positive test is pain, clicking, or popping suggesting intra-articular disease. Other positive results include:
Hip or groin pain
Clicking or crepitus
Increased or decreased joint mobility
Thomas Test
Purpose: Assesses hip flexion contractures and identifies potential issues with the iliopsoas muscle.
Procedure: The patient lies on their back, and one leg is flexed toward the chest while the other leg is extended. The examiner observes the angle of hip flexion and to see if the extended leg lifts.
Piriformis Test
Purpose: Assesses the piriformis muscle for tightness or irritation.
Procedure: The patient lies on their back with the hips and knees flexed. The examiner externally rotates the patient's hip, which can provoke pain or discomfort if the piriformis is involved.
Trendelenburg Test
Purpose: Assesses hip abductor strength, especially the gluteus medius muscle.
Procedure: The patient stands on one leg, and the examiner observes for a drop or tilt of the pelvis on the unsupported side.
Femoroacetabular Impingement (FAI) Test
Purpose: Used to assess for hip impingement, which can lead to pain and limited range of motion.
Procedure: Brings the patient's knee up to their chest, Rotates the knee inward towards the opposite shoulder, Flexes the hip and knee to 90°, Progressively rotates the hip from external rotation to internal rotation while moving from abduction to adduction, Raises the affected leg so that the knee and hip are bent at 90 degrees
Labral Loading & Distraction Test
Purpose: Assesses labral tears or hip joint instability.
Procedure: The examiner applies force to load or distract the hip joint to elicit pain or discomfort.
Scour Test
Purpose: Helps evaluate labral tears, cartilage damage, and impingement in the hip joint.
Procedure: The patient's hip is flexed, and the examiner applies a compressive and rotational force to the joint.
Apprehension Test
Purpose: Detects hip instability or potential dislocation in individuals with a history of hip instability.
Procedure: The examiner flexes and abducts the hip while assessing the patient's reaction to the potential sensation of instability.
FABER Test
Purpose: Assesses hip joint mobility, pain, and potential issues involving the sacroiliac joint.
Procedure: The patient's hip is flexed, abducted, and externally rotated, and the examiner observes for pain or discomfort.
Ober’s Test
Purpose: Assesses the iliotibial band (ITB) tightness and tensor fasciae latae (TFL) syndrome.
Procedure: The patient lies on their side, and the examiner assesses the ability to adduct the hip past neutral.
When asking about duration and timing during an abdominal exam you should relate it to:
Eating/drinking
Melena
Dark, tarry stools
Hematochezia
Bright, red stools
Patterns of Pain
Visceral-Precipitated by stretch of or pressure within viscera. Usually referred to midline due to innervation.
Colicky-Due to contraction of a muscular tube against an obstruction. Perceived as waxing and waning or coming in waves.
Referred-Inflammation or pathology results in pain in another location.
Parietal-Localized pain caused by inflammatory process affecting somatic nerve fibers. (Dermatomal)
Important factors when noting N/V during an Abd exam.
Onset relative to pain
Frequency
Relation to eating/drinking
Ability to tolerate intake
Presence/Absence of Blood
Hematemesis, Coffee ground
Presence/Absence of Bile
Important factors when noting diarrhea during an Abd exam.
Frequency
Consistency
Relationship to pain
Presence/Absence of Blood
Hematochezia
Melena
Acholic – grey colored stool
Amber colored stools – bile duct obstruction
Three important associated symptoms to ask when a patient presents with abdominal pain.
Fever, Chills, Weight loss
What other history is important with an abd exam?
Surgical, medical, health maintenance, medications, social, family
Auscultation for abdominal exam
Perform before percussion or palpation
Bowel sounds due to movement of air and fluid
Heard as gurgling and clicks under normal circumstances
Listen with stethoscope lightly on skin
Listen for bowel sounds in all four quadrants
Also listen for abdominal bruits
Describing bowel sounds
Absent-none heard for 3 minutes
Hypoactive-fewer than 5 sounds in a minute
Normoactive-5 to 30 sounds in a minute
Hyperactive-greater than 30 sounds/minute (sounds almost continuous)
Rushes-sound of fluid being forced
Tinkles-higher pitched sounds that occur infrequently
Tympany vs. Dullness
Tympany-underlying air
Dullness-underlying fluid, organs, or solid mass
What are signs of possible peritonitis.
Guarding -Voluntary contraction of abdomen to protect an area you are trying to examine
Rigidity - Involuntary contraction of abdominal wall from peritoneal inflammation, usually sustained
Rebound Tenderness
Shifting Dullness
"Shifting dullness" is a medical term used in physical examination to assess for the presence of ascites, which is an abnormal accumulation of fluid in the abdominal cavity. Ascites is often associated with various underlying medical conditions, such as liver disease, heart failure, kidney disease, or certain cancers.
The presence of shifting dullness during this examination is suggestive of ascites. It's an important clinical sign that may prompt further evaluation, including diagnostic imaging (such as ultrasound or CT scans) and blood tests, to determine the underlying cause of ascites.
Fluid Wave Testing
Have assistant apply pressure in midline with edge of hand
Tap one side of abdomen firmly and feel on opposite side for transmitted pulsation
Feeling pulsation signifies presence of ascites
A rarely used test
Do not perform if patient has signs of peritonitis!
Document as “Positive Fluid Wave”
Rovsing Sign
Used specifically to evaluate for peritoneal inflammation in right lower quadrant
Palpate in left lower quadrant toward right side
Ask patient where they feel it most
If they feel it more in right lower quadrant than at site of palpation, then test is
positive (suggests appendicitis)
Describe as “Positive or Negative Rovsing”
Psoas Sign
Used to evaluate for inflammation adjacent to psoas muscle on right side
Two techniques-active flexion and passive stretch
Have patient flex hip with leg straight
Alternatively, have patient on left side.
Place hand on hip and extend hip.
Increased pain with either maneuver suggests appendicitis.
If positive, document as “Positive Psoas Sign”
Obturator Sign
Used to evaluate for peritoneal inflammation in right lower quadrant and pelvis
With hip and knee flexed, internally rotate the hip
Increased pain in right lower quadrant suggests irritation of the internal obturator muscle by appendix
Very low sensitivity
Document as “Positive Obturator Sign”
Murphy Sign
Used to evaluate for gallbladder inflammation (cholecystitis)
With patient supine, have patient exhale completely
Palpate under costal margin as deeply as possible, then have patient inhale
Arrest of inspiration due to pain is a positive
Murphy sign (tenderness alone inadequate)
Costovertebral Angle significance
Location: The CVAs are situated on both sides of the spine, where the 12th rib descends to meet the vertebrae of the lower thoracic and upper lumbar regions of the back. They are located on the posterior (back) aspect of the body.
Palpation: Healthcare professionals often perform a physical examination of the CVAs by palpating (pressing or tapping) this area. This examination is typically done to assess for tenderness or pain, particularly in the context of evaluating the kidneys.
Clinical Significance: Tenderness or pain upon palpation of the CVA can be indicative of various medical conditions, including kidney problems, such as kidney infection (pyelonephritis), kidney stones, or other kidney-related disorders. Pain in the CVA can also be caused by musculoskeletal issues, spinal problems, or referred pain from other organs.
Diagnosis: Tenderness or pain in the CVA is often evaluated alongside other clinical signs and symptoms, medical history, and diagnostic tests like urinalysis, blood tests, and imaging (such as ultrasound or CT scans) to determine the underlying cause of discomfort or tenderness.
What are some common GI symptoms in children?
Difficulty swallowing (dysphagia) and/or painful swallowing (odynophagia)
Abdominal pain, acute or chronic. Associated with/without indigestion, substernal discomfort, nausea, vomiting, hematemesis, anorexia, early satiety
Changes in bowel habits
Diarrhea, constipation
Jaundice
Dyspepsia
is a chronic or recurrent discomfort or pain centered in the upper abdomen
It can be associated by epigastric pain, burning, postprandial fullness, satiety, bloating, nausea or belching
Delayed gastric emptying, peptic ulcer disease (PUD) or H. Pylori can cause dyspepsia
In toddlers, a crampy abdominal pain associated with elongated mass in the right abdomen suggests
intussusception
Cramping pain radiating to the flank or groin accompanied by urinary symptoms is suggestive of
nephrolithiasis
RLQ pain that migrates from the periumbilical region, combined with nausea, vomiting and loss of appetite is suspicious for
appendicitis
What can be a diagnosis of exclusion for chronic abdominal pain?
Inflammatory Bowel Disease (IBS) is a diagnosis of exclusion
It requires intermittent pain and changes of form and frequency of stools for 12 weeks of the preceding 12 months
If it presents with changing bowel habits and alternating diarrhea and constipation, consider Cystic Fibrosis
If accompanied by an elongated mass at the LLQ, it usually is due to constipation
What is due to elevated plasma bilirubin >3 mg/dl?
Icterus
Unconjugated Bilirubin occurs in:
a. Increased production of bilirubin, like in hemolytic anemia
b. Decreased uptake of bilirubin by hepatocytes
c. Decreased ability of the liver to conjugate bilirubin
Conjugated Bilirubin occurs in:
a. Extrahepatic jaundice from obstruction of the extrahepatic bile ducts, most commonly in the common bile ducts
b. Impaired excretion of conjugated bilirubin as in viral hepatitis, cirrhosis, drug induced cholestasis such as oral contraceptive, methyl testosterone, and chlorpromazine
What is the order of the pediatric abdominal physical exam?
Inspection
Auscultation
Percussion
Palpation, Light/Deep
Hirschsprung's Disease
Hirschsprung disease is a birth defect in which some nerve cells are missing in the large intestine, so a child's intestine can't move stool and becomes blocked.
How do you assess CVA tenderness?
It can be elicited by placing the palm of one hand on the CVA area and strike with the other hand on it.
What are heart murmurs?
Audible variations
What are three types of heart murmurs?
Stenotic value: obstructs blood flow & causes a characteristic murmur
Regurgitant valve: value that DOES NOT fully close
Septal defects: abnormal opening btw heart chambers (ASD, VSD, PFO patent foreman ovale)
What makes the following sounds: S1, S2?
S1: mitral and tricuspid valve closure, systole
S2: Aortic & Pulmonary valves close, diastolic
Where is the best place to access the jugular venous pressure?
R internal carotid vein
Where is the point of maximal impulse?
5th intercostal space
7-9cm lateral to midsternal line
Classification of murmurs
Innocent - No detectable anomaly
Physiologic - related to demand supply ie: anemia, pregnancy, fever
Pathologic - tangible cardiac disorder ie: valvular lesions
Who is the father of the ECHO?
Inge Elder
Where do you hear the heart valves?
Aortic, right 2nd intercostal space
Tricuspid, right 5th intercostal space
Pulmonary, left 2nd intercostal space
Mitral, left 5th intercostal space