Chapter 25: Assessment of Respiratory System Lewis: Medical-Surgical Nursing, 10th Edition
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
A patient with acute shortness of breath is admitted to the hospital. Which action should the
nurse take during the initial assessment of the patient?
a. Ask the patient to lie down to complete a full physical assessment.
b. Briefly ask specific questions about this episode of respiratory distress.
c. Complete the admission database to check for allergies before treatment.
d. Delay the physical assessment to first complete pulmonary function tests.
ANS: B
When a patient has severe respiratory distress, only information pertinent to the current
episode is obtained, and a more thorough assessment is deferred until later. Obtaining a
comprehensive health history or full physical examination is unnecessary until the acute
distress has resolved. Brief questioning and a focused physical assessment should be done
rapidly to help determine the cause of the distress and suggest treatment. Checking for
allergies is important, but it is not appropriate to complete the entire admission database at
this time. The initial respiratory assessment must be completed before any diagnostic tests or
interventions can be ordered.
DIF: Cognitive Level: Apply (application) REF: 459
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
The nurse prepares a patient with a left-sided pleural effusion for a thoracentesis. How should
the nurse position the patient?
a. High-Fowler's position with the left arm extended
b. Supine with the head of the bed elevated 30 degrees
c. On the right side with the left arm extended above the head
d. Sitting upright with the arms supported on an over bed table
ANS: D
The upright position with the arms supported increases lung expansion, allows fluid to collect
at the lung bases, and expands the intercostal space so that access to the pleural space is
easier. The other positions would increase the work of breathing for the patient and make it
more difficult for the health care provider performing the thoracentesis.
DIF: Cognitive Level: Apply (application) REF: 471
TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity
A diabetic patient's arterial blood gas (ABG) results are pH 7.28; PaCO2 34 mm Hg; PaO2 85 mm Hg; HCO3- 18 mEq/L. The nurse would expect which finding?
a. Intercostal retractions c. Low oxygen saturation (SpO2)
b. Kussmaul respirations d. Decreased venous O2 pressure
ANS: B
Kussmaul (deep and rapid) respirations are a compensatory mechanism for metabolic
acidosis. The low pH and low bicarbonate result indicate metabolic acidosis. Intercostal
retractions, a low oxygen saturation rate, and a decrease in venous O2 pressure would not be
caused by acidosis.
DIF: Cognitive Level: Apply (application) REF: 467
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
On auscultation of a patient's lungs, the nurse hears low-pitched, bubbling sounds during
inhalation in the lower third of both lungs. How should the nurse document this finding?
a. Inspiratory crackles at the bases
b. Expiratory wheezes in both lungs
c. Abnormal lung sounds in the apices of both lungs
d. Pleural friction rub in the right and left lower lobes
ANS: A
Crackles are low-pitched, bubbling sounds usually heard on inspiration. Wheezes are
high-pitched sounds. They can be heard during the expiratory or inspiratory phase of the
respiratory cycle. The lower third of both lungs are the bases, not apices. Pleural friction rubs
are grating sounds that are usually heard during both inspiration and expiration.
DIF: Cognitive Level: Apply (application) REF: 468
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
The nurse palpates the posterior chest while the patient says "99" and notes absent fremitus.
Which action should the nurse take next?
a. Palpate the anterior chest and observe for barrel chest.
b. Encourage the patient to turn, cough, and deep breathe.
c. Review the chest x-ray report for evidence of pneumonia.
d. Auscultate anterior and posterior breath sounds bilaterally.
ANS: D
To assess for tactile fremitus, the nurse should use the palms of the hands to assess for
vibration when the patient repeats a word or phrase such as "99." After noting absent fremitus,
the nurse should then auscultate the lungs to assess for the presence or absence of breath
sounds. Absent fremitus may be noted with pneumothorax or atelectasis. The vibration is
increased in conditions such as pneumonia, lung tumors, thick bronchial secretions, and
pleural effusion. Turning, coughing, and deep breathing is an appropriate intervention for
atelectasis, but the nurse needs to first assess breath sounds. Fremitus is decreased if the hand
is farther from the lung or the lung is hyperinflated (barrel chest). The anterior of the chest is
more difficult to palpate for fremitus because of the presence of large muscles and breast
tissue.
DIF: Cognitive Level: Apply (application) REF: 464
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
A patient with a chronic cough is scheduled to have a bronchoscopy with biopsy. Which
intervention will the nurse implement directly after the procedure?
a. Encourage the patient to drink clear liquids.
b. Place the patient on bed rest for at least 4 hours.
c. Keep the patient NPO until the gag reflex returns.
d. Maintain the head of the bed elevated 90 degrees.
ANS: C
Risk for aspiration and maintaining an open airway is the priority. Because a local anesthetic
is used to suppress the gag and cough reflexes during bronchoscopy, the nurse should monitor
for the return of these reflexes before allowing the patient to take oral fluids or food. The
patient does not need to be on bed rest, and the head of the bed does not need to be in the
high-Fowler's position.
DIF: Cognitive Level: Apply (application) REF: 470
TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity
The nurse completes a shift assessment on a patient admitted in the early phase of heart
failure. When auscultating the patient's lungs, which finding would the nurse most likely
hear?
a. Continuous rumbling, snoring, or rattling sounds mainly on expiration
b. Continuous high-pitched musical sounds on inspiration and expiration
c. Discontinuous, high-pitched sounds of short duration during inspiration
d. A series of long-duration, discontinuous, low-pitched sounds during inspiration
ANS: C
Fine crackles are likely to be heard in the early phase of heart failure. Fine crackles are
discontinuous, high-pitched sounds of short duration heard on inspiration. Course crackles are
a series of long-duration, discontinuous, low-pitched sounds during inspiration. Wheezes are
continuous high-pitched musical sounds on inspiration and expiration.
DIF: Cognitive Level: Apply (application) REF: 468
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
The nurse observes that a patient with respiratory disease experiences a decrease in SpO2 from
93% to 88% while the patient is ambulating. What is the priority action of the nurse?
a. Notify the health care provider.
b. Administer PRN supplemental O2.
c. Document the response to exercise.
d. Encourage the patient to pace activity.
ANS: B
The drop in SpO2 to 85% indicates that the patient is hypoxemic and needs supplemental O2
when exercising. The other actions are also important, but the first action should be to correct
the hypoxemia.
DIF: Cognitive Level: Analyze (analysis) REF: 459
OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation
MSC: NCLEX: Physiological Integrity
The nurse teaches a patient about pulmonary spirometry testing. Which statement, if made by
the patient, indicates teaching was effective?
a. "I should use my inhaler right before the test."
b. "I won't eat or drink anything 8 hours before the test."
c. "I will inhale deeply and blow out hard during the test."
d. "My blood pressure and pulse will be checked every 15 minutes."
ANS: C
For spirometry, the patient should inhale deeply and exhale as long, hard, and fast as possible.
The other actions are not needed. The administration of inhaled bronchodilators should be
avoided 6 hours before the procedure.
DIF: Cognitive Level: Apply (application) REF: 472
TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity
The nurse observes a student who is listening to a patient's lungs. Which action by the student
indicates a need to review respiratory assessment skills?
a. The student compares breath sounds from side to side at each level.
b. The student listens during the inspiratory phase, then moves the stethoscope.
c. The student starts at the apices of the lungs, moving down toward the lung bases.
d. The student instructs the patient to breathe slowly and deeply through the mouth.
ANS: B
Listening only during inspiration indicates the student needs a review of respiratory
assessment skills. At each placement of the stethoscope, listen to at least one cycle of
inspiration and expiration. During chest auscultation, instruct the patient to breathe slowly and
a little deeper than normal through the mouth. Auscultation should proceed from the lung
apices to the bases, comparing opposite areas of the chest, unless the patient is in respiratory
distress or will tire easily.
DIF: Cognitive Level: Apply (application) REF: 466
TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment
A patient who has a history of chronic obstructive pulmonary disease (COPD) was
hospitalized for increasing shortness of breath and chronic hypoxemia (SaO2 levels of 89% to
90%). In planning for discharge, which action by the nurse will be most effective in
improving compliance with discharge teaching?
a. Have the patient repeat the instructions immediately after teaching.
b. Accomplish the patient teaching just before the scheduled discharge.
c. Arrange for the patient's caregiver to be present during the teaching.
d. Start giving the patient discharge teaching during the admission process.
ANS: C
Hypoxemia interferes with the patient's ability to learn and retain information, so having the
patient's caregiver present will increase the likelihood that discharge instructions will be
followed. Having the patient repeat the instructions will indicate that the information is
understood at the time, but it does not guarantee retention of the information. Because the
patient is likely to be distracted just before discharge, giving discharge instructions just before
discharge is not ideal. The patient is likely to be anxious and even more hypoxemic than usual
on the day of admission, so teaching about discharge should be postponed.
DIF: Cognitive Level: Analyze (analysis) REF: 462
TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity
A patient admitted to the emergency department complaining of sudden onset shortness of
breath is diagnosed with a possible pulmonary embolus. How should the nurse prepare the
patient for diagnostic testing to confirm the diagnosis?
a. Ensure that the patient has been NPO.
b. Start an IV so contrast media may be given.
c. Inform radiology that radioactive glucose preparation is needed.
d. Instruct the patient to expect to inspire deeply and exhale forcefully.
ANS: B
Spiral computed tomography scans are the most commonly used test to diagnose pulmonary
emboli and contrast media may be given IV. Bronchoscopy is used to detect changes in the
bronchial tree, not to assess for vascular changes, and the patient should be NPO 6 to 12 hours
before the procedure. Positron emission tomography scans are most useful in determining the
presence of malignancy and a radioactive glucose preparation is used. For spirometry, the
patient is asked to inhale deeply and exhale as long, hard, and fast as possible.
DIF: Cognitive Level: Apply (application) REF: 470
TOP: Nursing Process: Planning MSC: NCLEX: Physiological Integrity
The nurse admits a patient who has a diagnosis of an acute asthma attack. Which statement
indicates that the patient may need teaching regarding medication use?
a. "I have not had any acute asthma attacks during the past year."
b. "I became short of breath an hour before coming to the hospital."
c. "I've been taking Tylenol 650 mg every 6 hours for chest wall pain."
d. "I've been using my albuterol inhaler more frequently over the last 4 days."
ANS: D
The increased need for a rapid-acting bronchodilator should alert the patient that an acute
attack may be imminent and that a change in therapy may be needed. The patient should be
taught to contact a health care provider if this occurs. The other data do not indicate any need
for additional teaching.
DIF: Cognitive Level: Apply (application) REF: 460
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
A patient with acute dyspnea is scheduled for a spiral computed tomography (CT) scan.
Which information obtained by the nurse is a priority to communicate to the health care
provider before the CT?
a. Allergy to shellfish c. Respiratory rate of 30
b. Apical pulse of 104 d. O2 saturation of 90%
ANS: A
Because iodine-based contrast media is used during a spiral CT, the patient may need to have
the CT scan without contrast or be premedicated before injection of the contrast media. The
increased pulse, low oxygen saturation, and tachypnea all indicate a need for further
assessment or intervention but do not indicate a need to modify the CT procedure.
DIF: Cognitive Level: Analyze (analysis) REF: 470
OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation
MSC: NCLEX: Physiological Integrity
The nurse analyzes the results of a patient's arterial blood gases (ABGs). Which finding would require immediate action?
a. The bicarbonate level (HCO3-) is 31 mEq/L.
b. The arterial oxygen saturation (SaO2) is 92%.
c. The partial pressure of CO2 in arterial blood (PaCO2) is 31 mm Hg.
d. The partial pressure of oxygen in arterial blood (PaO2) is 59 mm Hg.
ANS: D
All the values are abnormal, but the low PaO2 indicates that the patient is at the point on the
oxyhemoglobin dissociation curve where a small change in the PaO2 will cause a large drop in
the O2 saturation and a decrease in tissue oxygenation. The nurse should intervene
immediately to improve the patient's oxygenation.
DIF: Cognitive Level: Analyze (analysis) REF: 457
OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment
MSC: NCLEX: Physiological Integrity
Which assessment finding indicates that the nurse should take immediate action for an older patient?
a. Weak cough effort c. Dry mucous membranes
b. Barrel-shaped chest d. Bilateral basilar crackles
ANS: D
Crackles in the lower half of the lungs indicate that the patient may have an acute problem
such as heart failure. The nurse should immediately accomplish further assessments, such as
O2 saturation, and notify the health care provider. A barrel-shaped chest, hyperresonance to
percussion, and a weak cough effort are associated with aging. Further evaluation may be
needed, but immediate action is not indicated. An older patient has a less forceful cough and
fewer and less functional cilia. Mucous membranes tend to be drier.
DIF: Cognitive Level: Analyze (analysis) REF: 468
OBJ: Special Questions: Prioritization TOP: Nursing Process: Assessment
MSC: NCLEX: Physiological Integrity
A patient in metabolic alkalosis is admitted to the emergency department and pulse oximetry
(SpO2) indicates that the O2 saturation is 94%. Which action should the nurse expect to take
next?
a. Complete a head-to-toe assessment.
b. Administer an inhaled bronchodilator.
c. Place the patient on high-flow oxygen.
d. Obtain repeat arterial blood gases (ABGs).
ANS: C
Although the O2 saturation is adequate, the left shift in the oxyhemoglobin dissociation curve
will decrease the amount of O2 delivered to tissues, so high oxygen concentrations should be
given. A head-to-toe assessment and repeat ABGs may be implemented later. Bronchodilators
are not needed for metabolic alkalosis and there is no indication that the patient is having
difficulty with airflow.
DIF: Cognitive Level: Analyze (analysis) REF: 457
OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation
MSC: NCLEX: Physiological Integrity
After the nurse has received change-of-shift report, which patient should the nurse assess
first?
a. A patient with pneumonia who has crackles in the right lung base
b. A patient with chronic bronchitis who has a low forced vital capacity
c. A patient with possible lung cancer who has just returned after bronchoscopy
d. A patient with hemoptysis and a 16-mm induration after tuberculin skin testing
ANS: C
Because the cough and gag are decreased after bronchoscopy, this patient should be assessed
for airway patency. The other patients do not have clinical manifestations or procedures that
require immediate assessment by the nurse.
DIF: Cognitive Level: Analyze (analysis) REF: 463
OBJ: Special Questions: Prioritization | Special Questions: Multiple Patients
TOP: Nursing Process: Assessment MSC: NCLEX: Safe and Effective Care Environment
The laboratory has just called with the arterial blood gas (ABG) results on four patients.
Which result is most important for the nurse to report immediately to the health care
provider?
a. pH 7.34, PaO2 82 mm Hg, PaCO2 40 mm Hg, and O2 sat 97%
b. pH 7.35, PaO2 85 mm Hg, PaCO2 50 mm Hg, and O2 sat 95%
c. pH 7.46, PaO2 90 mm Hg, PaCO2 32 mm Hg, and O2 sat 98%
d. pH 7.31, PaO2 91 mm Hg, PaCO2 50 mm Hg, and O2 sat 96%
ANS: D
These ABGs indicate uncompensated respiratory acidosis and should be reported to the health
care provider. The other values are normal, close to normal, or compensated.
DIF: Cognitive Level: Analyze (analysis) REF: 456
OBJ: Special Questions: Prioritization TOP: Nursing Process: Implementation
MSC: NCLEX: Physiological Integrity
The nurse assesses a patient with chronic obstructive pulmonary disease (COPD) who has
been admitted with increasing dyspnea over the past 3 days. Which finding is important for
the nurse to report to the health care provider?
a. Respirations are 36 breaths/min.
b. Anterior-posterior chest ratio is 1:1.
c. Lung expansion is decreased bilaterally.
d. Hyperresonance to percussion is present.
ANS: A
The increase in respiratory rate indicates respiratory distress and a need for rapid interventions
such as administration of O2 or medications. The other findings are common chronic changes
occurring in patients with COPD.
DIF: Cognitive Level: Apply (application) REF: 460
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
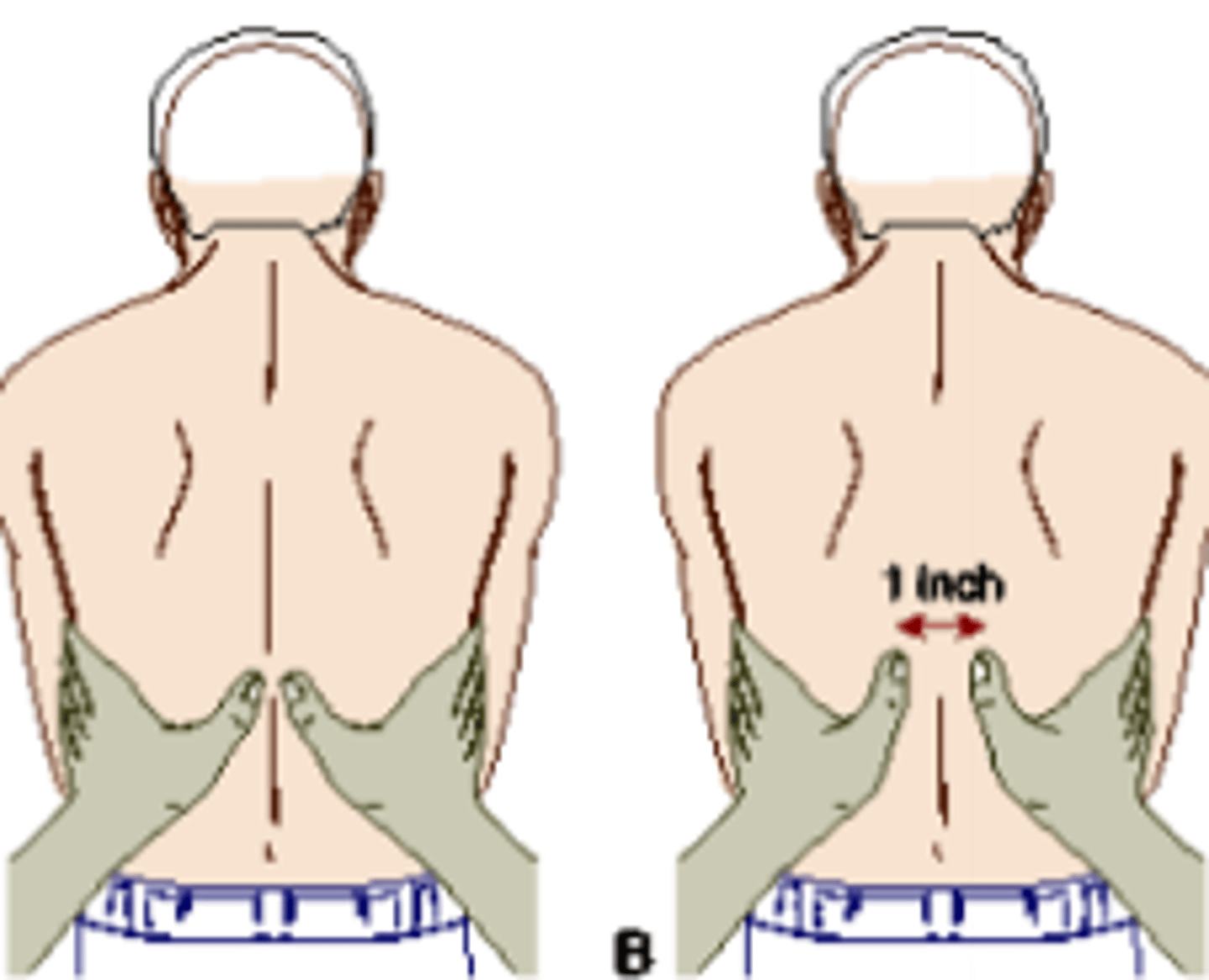
ANS: C
The technique for palpation for chest excursion is shown in the illustrated technique. Reduced
chest movement would be noted on palpation of a patient's chest with COPD.
Hyperresonance would be assessed through percussion. Accessory muscle use and tripod
positioning would be assessed by inspection.
DIF: Cognitive Level: Understand (comprehension) REF: 467
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity
Using the illustrated technique, the nurse is assessing for which finding in a patient with chronic obstructive pulmonary disease (COPD)?
a. Hyperresonance c. Reduced excursion
b. Tripod positioning d. Accessory muscle use
Which action is appropriate for the nurse to delegate to unlicensed assistive personnel (UAP)?
a. Listen to a patient's lung sounds for wheezes or crackles.
b. Label specimens obtained during percutaneous lung biopsy.
c. Instruct a patient about how to use home spirometry testing.
d. Measure induration at the site of a patient's intradermal skin test.
ANS: B
Labeling of specimens is within the scope of practice of UAP. The other actions require
nursing judgment and should be done by licensed nursing personnel.
DIF: Cognitive Level: Apply (application) REF: 471
OBJ: Special Questions: Delegation TOP: Nursing Process: Assessment
MSC: NCLEX: Safe and Effective Care Environment
A patient is scheduled for a computed tomography (CT) scan of the chest with contrast media.
Which assessment findings should the nurse report to the health care provider before the
patient goes for the CT (select all that apply)?
a. Allergy to shellfish
b. Patient reports claustrophobia
c. Elevated serum creatinine level
d. Recent bronchodilator inhaler use
e. Inability to remove a wedding band
ANS: A, C
Because the contrast media is iodine based and may cause dehydration and decreased renal
blood flow, asking about iodine allergies (such as allergy to shellfish) and monitoring renal
function before the CT scan are necessary. The other actions are not contraindications for CT
of the chest, although they may be for other diagnostic tests, such as magnetic resonance
imaging or pulmonary spirometry.
DIF: Cognitive Level: Apply (application) REF: 470
TOP: Nursing Process: Implementation MSC: NCLEX: Physiological Integrity
http://static.us.elsevierhealth.com/lewis_9e/wheezing.mp3
While listening to the posterior chest of a patient who is experiencing acute shortness of
breath, the nurse hears these sounds. How should the nurse document the lung sounds?
(Click link to listen to audio clip)
a. Pleural friction rub
b. Low-pitched crackles
c. High-pitched wheezes
d. Bronchial breath sounds
ANS:
C
Wheezes are continuous high-pitched or musical sounds heard initially with expiration. The
other responses are typical of other adventitious breath sounds.
DIF: Cognitive Level: Understand (comprehension) REF: 468
TOP: Nursing Process: Assessment MSC: NCLEX: Physiological Integrity