The menstrual cycle
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
What happens during the follicular phase (pre-ovulatory)?
Primary oocyte = frozen at prophase 1
Primary follicle: primary oocyte surrounded by granulosa cells + theca cells → release oestrogen
Early secondary follicle: surrounded by zona pellucida (glycoprotein membrane) → produce oestrogen
Late secondary follicle: same as early secondary follicle with pockets of fluid containing hyaluronic acid
Graafian follicle:
primary oocyte → secondary oocyte (frozen at Metaphase II)
surrounded by corona radiata (cells differentiated from granulosa cells)
Pockets of fluid combine to form the antrum
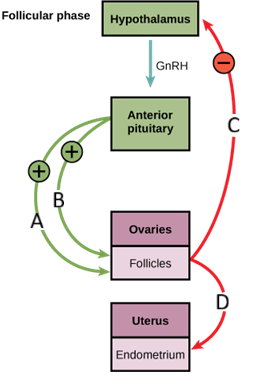
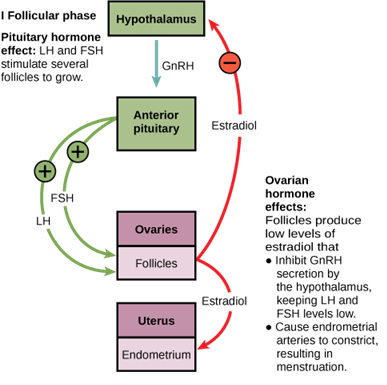
How is the follicular phase initiated?
Hypothalamus → GnRH → ant pituitary →
FHS → granulosa cells → androgens to oestrogen
LH → theca cells → cholesterol to androgens
** 2-cell, 2-gonadotrophin hypothesis
What feedback mechanism is in place during the mid follicular phase?
Levels of oestrogen slowly increase → negative feedback to ant pituatry → LH + FSH decrease (to not make more follicles mature)
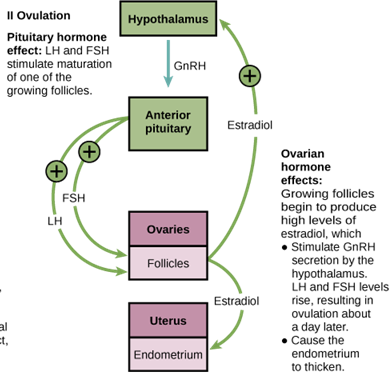
What feedback mechanism is in place during the late follicular phase?
Graafian cells produce inhibin to stop FSH secretion
Graafian cells produces lots of oestrogen so oestrogen remains consistently high → positive feedback on ant pituitary → pituitary is very sensitive → LH surge
How is ovulation initiated?
LH surge → removes mature egg from graafian cells → mature egg released into fallopian tube
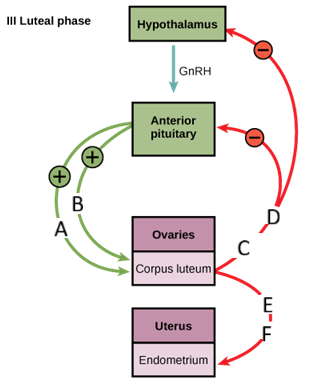
What happens during the luteal phase?
Corpus haemorrhagicum → corpus luteum → produces progesterone due to LH + Inhibin A → negative feedback to ant pituitary → stop LH


What are the phases of the ovarian cycle?
Follicular/pre-ovulatory phase (Day 1 – 14)
Ovulation (day 14)
Luteal phase (day 14-28)
What are the phases of the uterine cycle?
Menstrual phase (day 1-5)
Proliferative phase (Day 6-14 )
Secretory phase (Day 14-28)
What happens during the menstrual phase?
Stratum functionalis shed (Stratum Basalis remains)
What happens during the proliferative phase?
o Rebuild stratum functionalis
o Rebuild spiral arteries
o Rebuild uterine glands
o Cervical glands produce thin mucous
o DUE TO OESTROGEN
What happens during the secretory phase?
o Uterine gland secrete nutrient rich fluid
o Cervical glands produce thick mucous
o Thick layer of stratum functionalis
o Longer spiral arteries
What happens if during the ovulation phase you fall pregnant?
Embryo produces HcG (acts as LH) → maintains corpus luteum → maintains progesterone for first 12 wks
What happens if during the ovulation phase you DON’T fall pregnant?
o Corpus luteum degenerates→ corpus albicans → Progesterone stops
o Spasms in spiral arteries, becomes weak and rupture → ischaemia in stratum functionalis → becomes necrotic → sheds as period
Cervical plug removed
How does the body decide if it is ready to be pregnant?
Adipocytes→ leptin→ signals brain fat stores enough for reproductive function → menarche
How is GnRH released and why is it important?
o pulsatile GnRH release important: Continuous release leads to insensitivity of receptors
Define:
Amenorrhea
Oligomenorrhoea
Menorrhagia
Dysmenorrhea
Amenorrhea – Absence or cessation of menstruation
Oligomenorrhoea – ‘Few or scanty’ irregular and inconsistent menstrual bleeding – if menstrual cycle length >35 days
Menorrhagia – Heavy menstrual bleeding
Dysmenorrhea – Painful menstrual bleeding
Key terminologies
Primary vs secondary Amenorrhea
Primary amenorrhoea: Failure to menstruate by 15 with normal secondary sexual characteristics OR by 13 years of age with no secondary sexual characteristics
Secondary amenorrhoea: Cessation of menstruation for 3 – 6 months
What is Kallmann syndrome and what are the symptoms?
Failed migration of GnRH neurons from the nasal placode into the brain.
Characterised by GnRH deficiency + anosmia
Symptoms
• Primary amenorrhea
• Anosmia (loss of smell)
• Midline facial defects
• Renal agenesis
What is Sheehan syndrome and how can it cause amenorrhea?
complication of severe postpartum haemorrhage that damages the pituitary gland
does not release LH + FSH…
Ovarian causes of amenorrhea
Characterised by high FSH/LH
• Surgical removal (Oophorectomy )
• Radiation
• Pharmacological (Contraceptive pills)
• Idiopathic (Premature ovarian failure)
What are the different outflow obstructions that can cause amenorrhea?
Imperforate hymen
Transverse vaginal septum
Atresia of cervix (closed/absent)
** primary amenorrhea
What are the main categories of causes for amenorrhea?
Hypothalamic/ pituitary
ovarian
outflow obstruction
What are some suspected diagnoses with Oligomenorrhoea and how can you rule each out?
Hypothalmic Hypogonadotrophism if:
↓ FSH and LH / ↓ E2
Often caused by stress, diet, excess exercise
Polycystic Ovarian Syndrome (PCOS) if:
Normal FSH, normal/↑ LH, ↑ Testosterone
thyroid dysfunction if:
Abnormal TFTs ( can be hypo or hyper)
What is the criteria to be diagnosed with Polycystic Ovarian Syndrome (PCOS)?
two of the following three criteria:
Oligo-anovulation (infrequent or absent ovulation)
Clinical and/or biochemical signs of androgen excess
Polycystic ovarian morphology (PCOM)
What are some complications with PCOS?
Infertility
Cardiovascular disease
Metabolic disorders:
• Impaired glucose tolerance
• Type 2 diabetesEndometrial cancer (due to no period (anovulation) but still having high oestogen)
How is Menorrhagia diagnosed?
Objective: > 80 ml of blood loss each period + / last longer than 7 days
Subjective: Reports of period becoming heavier, changing sanitary products every 1-2 hrs, or passing clots
What causes menorrhagia?
PALM COEIN
Polyp
Adenomyosis
Leiomyoma
Malignancy
Coagulopathy
Ovulatory dysfunction
Endometrial
Iatrogenic (Anticoagulants, Antiplatelets, copper IUD)
Not-yet-classified
What are Uterine fibroids?
Benign tumours of the myometrium.
Caused by proliferation of a mixture of smooth muscle cells and fibroblasts
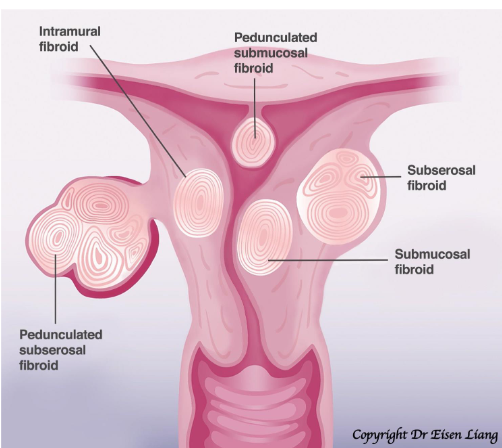
Symptoms of Uterine fibroids
menorrhagia +/ dysmenorrhoea
Pain, pressure, or discomfort
Urinary symptoms: frequency, urgency, urinary incontinence, or retention
Bowel symptoms: bloating, constipation, and/or painful defecation
Subfertility or infertility
Primary vs secondary Dysmenorrhoea
Primary dysmenorrhoea - pelvic pain during menstruation in the absence of pelvic pathology.
Secondary dysmenorrhoea - caused by an underlying pelvic pathology
causes of dysmenorrhoea
Endometriosis
Adenomyosis
Uterine fibroids
Pelvic inflammatory disease
Intrauterine device
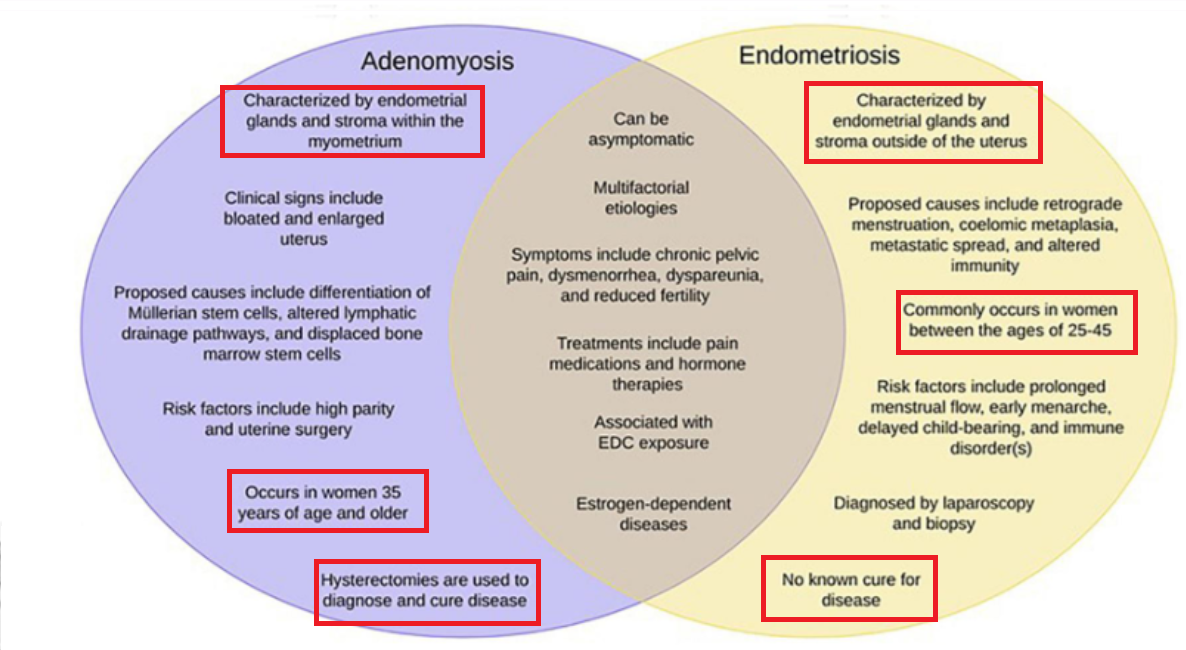
what is endometriosis?
Growth of endometrium-like tissue outside the uterus eg. on the ovaries, peritoneum, Uterosacral ligaments, Pouch of Douglas, Extra-pelvic
Hormonal changes → bleeding, chronic inflammation, and scar tissue formation
Symptoms of endometriosis
Secondary congestive dysmenorrhoea
Deep dyspareunia
Cyclical pelvic pain (peritoneal irritation)
Cyclical painful defecation / bleeding per rectum during menses
Irregular bleeding
Infertility
Difference between endometriosis and adenomyosis
How do we treat Kallmann syndrome?
Pulsatile administration of GnRH with a programmed infusion pump—can have normal folliculogenesis, ovulation, and pregnancy