anatomy and physiology chapter 5
1/250
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
251 Terms
integumentary system
the skin, hair, nails, and cutaneous glands
dermatology
branch of medicine that treats the integumentary system
integument
the skin
how much percent of the body weight does skin account for?
8%
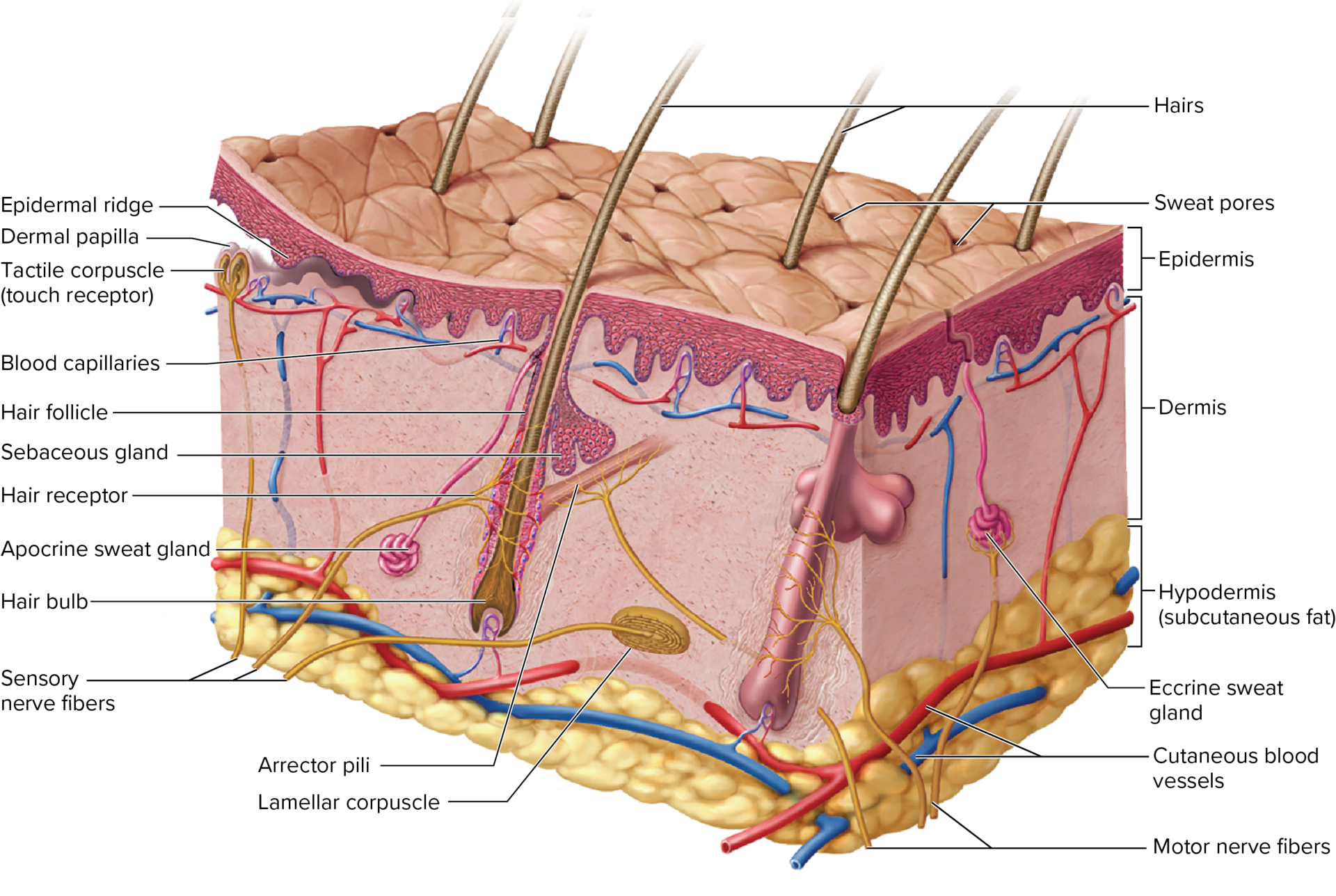
what are the 2 layers of the skin?
epidermis which is a stratified squamous epithelium
dermis which is a deeper connective tissue
hypodermis
connective tissue just underneath skin
examples of variation in skin thickness
0.5 mm of thick skin on palms, soles, and corresponding surfaces of fingers and toes
0.1 mm of thin skin on most of the body
characteristics of thick skin
adaptive for high friction
hairless
no sebaceous glands
capable of sweating
characteristics of thin skin
contains hair, sebaceous glands, and sweat glands
stratum corneum
a thick surface layer of dead cells
functions of skin
resistance to trauma and infection
prevents penetration of water
protects from UV rays and some chemicals
carries out first step for vitamin d synthesis which is then completed by livers and kidney
sweat glands excrete urea, metabolites, and some chemicals in perspiration
sensation
thermoregulation for regulating body temperature through vasodilation or vasoconstriction
nonverbal communication
keratin
a tough protein formed by keratinocytes that constitutes the hair, nails, and stratum corneum of the epidermis
thermoreceptor
neuron specialized to respond to heat or cold, found in the skin and mucous membranes, for example
epidermis
a stratified squamous epithelium that constitutes the superficial layer of the skin, overlying the dermis
characteristics of epidermis
surface has dead cells packed with keratin
lacks blood vessels and needs diffusion of nutrients from underlying connective tissue
nerve sensations due to dermis location
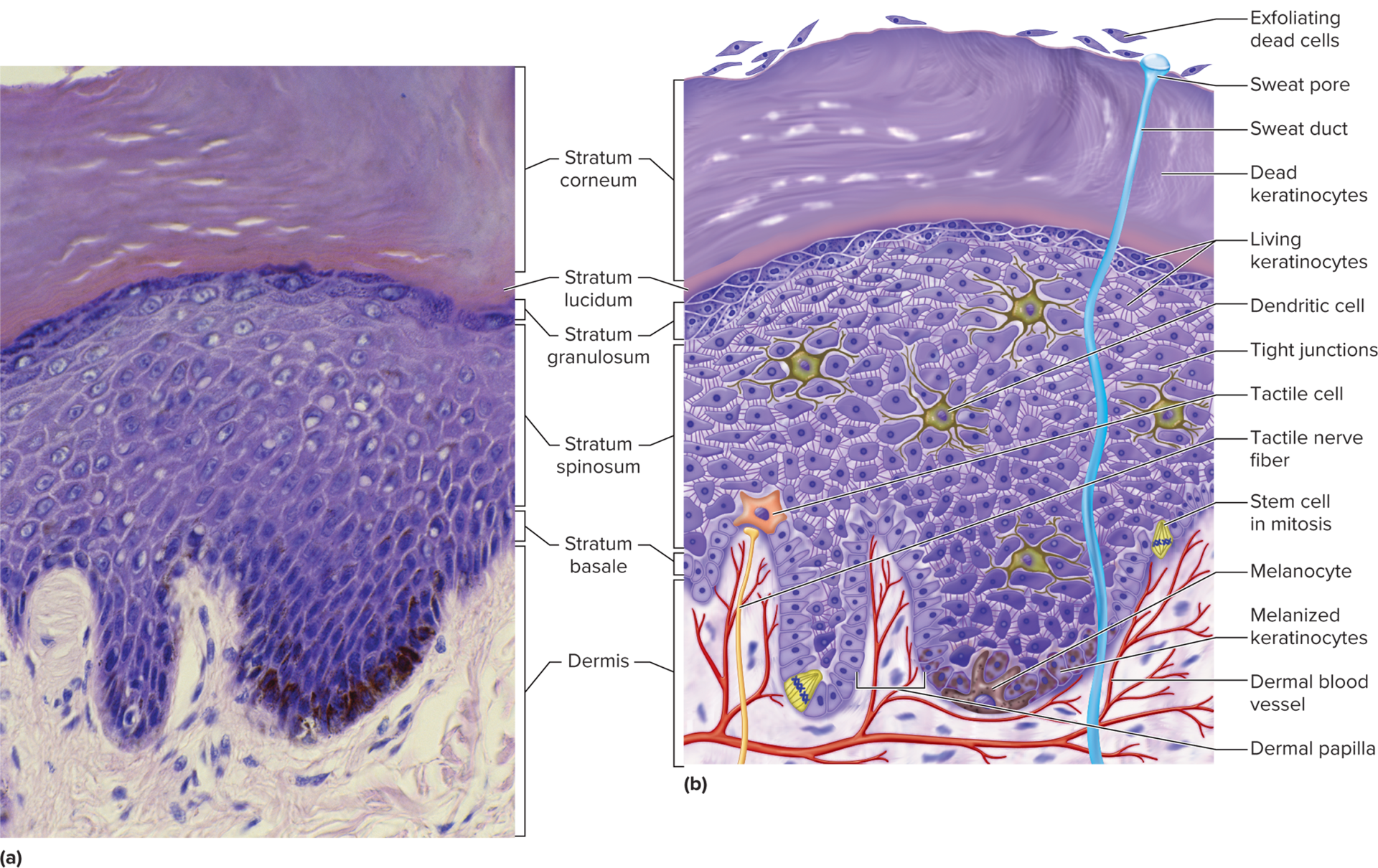
list the epidermis cells
keratinocytes
stem cells
melanocytes
tactile cells
dendritic cells
keratinocyte
a cell of the epidermis that synthesizes keratin, then dies; most cells of the epidermis are keratinocytes, with dead ones constituting the stratum corneum
stem cell
any undifferentiated cell that can divide and differentiate into more functionally specific cell types such as blood cells and germ cells
melanocyte
a cell of the stratum basale of the epidermis that synthesizes melanin and transfers it to the keratinocytes
tactile cells
receptors found in the basal layer of the epidermis and associated with an underlying dermal nerve fiber
dendritic cell
an antigen-presenting cell of the epidermis, vaginal mucosa, and some other epithelia
where are keratinocytes located?
majority of epidermal cells
where are stem cells located?
deepest layer of the epidermis called stratum basale
where are melanocytes found?
stratum basale amid the stem cells and deepest keratinocytes
what are functions melanocytes do in the body?
brown and black pigment melanin are synthesized
the cells have long branching processes that spread among keratinocytes and keep shedding melanin-containing fragments from their tips
the keratinocytes phagocytize the fragments and accumulate melanin granules on the sunny side of the nucleus
the pigment shields DNA from UV radiation
tactile disc
tactile cell and its nerve fiber
where are dendritic cells found?
stratum spinosum and granulosum which are two layers in the epidermis
where do dendritic cells originate from?
bone marrow
how many dendritic cells in the epidermis?
1800 per square millimeter
what functions do dendritic cells carry out in the body?
guarding against toxins, microbes, and disease agents that penetrate into the skin
foreign matter fragments get taken to the lymph nodes and alert immune system for defense
what are the epidermis layers?
stratum basale
stratum spinosum
stratum granulosum
stratum lucidum
stratum corneum
stratum basale
mainly a single layer of cuboidal to low columnar karatinocytes resting on the basement membrane
what’s scattered among the stratum basale?
melanocytes
tactile cells
stem cells
what happens to stem cells that divide in stratum basale?
it gives rise to keratinocytes that migrate toward the skin surface and replace lost epidermal cells
stratum spinosum
consists of several layers of keratinocytes; in most places this is the thickest stratum but, on the palms and soles it is thinner than stratum corneum
what happens to the deepest cells of the stratum spinosum when they keep dividing?
when they’re pushed further up, they stop dividing and instead make more keratin filaments which flatten the cell
what keeps keratinocytes firmly attached to each other?
desmosomes which partly contribute to epidermis toughness
desmosomes create bridges from cell to cell
stratum granulosum
3-5 layers of flat keratinocytes (more common in thick skin) and has dendritic cells
where does stratum granulosum get its name from?
the coarse dark staining keratohyalin which is in the layer
stratum lucidum
a thin translucent zone seen only in thick skin where keratinocytes are densely packed with a clear protein named eleidin
what’s the structure of the stratum lucidum?
anucleate without organelles making it look pale and featureless without distinct cell boundaries
how many layers of dead keratinized cells are there for stratum corneum?
30
most superficial to deep skin layers
corneum
lucidum
granulosum
spinosum
basale
how are keratinocytes produced?
mitosis of the stem cells in the stratum basale
oxygen and nutrients acquired for mitosis from blood vessels in nearby dermis
when epidermal cells migrate 2-3 cells away from the dermis, mitosis stops
why is mitosis rarely seen in the skin slides?
it occurs at night while most histological sections are taken during the day
how long does it take for a keratinocyte to flake off?
30-40 days
what slows down the speed of flaking keratinocytes and what speeds it up?
old age and injured skin
manual labor or tight shoes
calluses or corns
thick accumulations of dead keratinocytes on the hands or feet
lamellar granules
found in keratinocytes, these granules release a lipid mixture that coats the cell surface, preventing water loss
in the stratum granulosum, what 4 developments occur for keratinocytes?
the keratohyalin granules release a protein called filaggrin which binds the cytoskeletal keratin filaments together into course and tough bundles
the cells produce a tough layer of envelope proteins beneath the plasma membrane which creates an indestructible protein sac around the keratin bundles
the lamellar granules release a lipid mixture that spreads out over the cell surface and waterproofs it
when the barriers cut the keratinocytes off from the nutrient supply from below, their nuclei and other organelles degenerate, and the cells die which leaves behind the tough waterproof sac of keratin.
epidermal water barrier
a barrier crucial to retaining water in the body and preventing dehydration
dander
dead keratinocytes
dermis
the deeper of the two layers of the skin, underlying the epidermis and composed of fibrous connective tissue
characteristics of dermis
ranges from 0.2-4 mm thick depending on the area
mostly made of collagen with elastic and reticular fibers as well as fibroblasts and other cells typical of fibrous connective tissue
has blood vessels, cutaneous glands, and nerve endings
hair follicles and nail roots are embedded in dermis
smooth muscle in association with hair follicle
skeletal muscles attach to dermal collagen fibers to make expressions
dermal papilla
a bump or ridge of dermis that extends upward to interdigitate with the epidermis, creating a wavy boundary that resists stress and slippage of the epidermis; a projection of the dermis into the bulb of a hair, supplying blood to the hair.
epidermal ridges
downward waves that are the extension of the epidermis
characteristics of the dermal and epidermal boundaries
resists slippage of the epidermis across the dermis under stress
dermal papillae produce raised areas between furrows that can be seen in hand and wrist
on fingertips the wavy boundary forms friction ridges
in lips and genitals tall dermal papillae allow nerve fibers and blood capillaries to be closer to skin surface causing more redness and sensitivity
tension lines
collagen bundles in the dermis arranged mostly in parallel rows that run longitudinally in the limbs while encircling the neck, trunk, wrists, and more
purpose of tension lines
keep the skin under constant tension
what happens to tension lines when an incision is made in the skin perpendicularly?
the wound gapes because the collagen bundles pull the edges of the incision apart
what happens when a tension line is punctured with a circular object?
the wound gapes with a lemon shaped opening which makes it hard to close and heals with excessive scarring
example of incision parallel to tension lines
c section
papillary layer
pertaining to or shaped like a nipple, such as the papillary muscles of the heart; having papillae, such as the papillary layer of the dermis
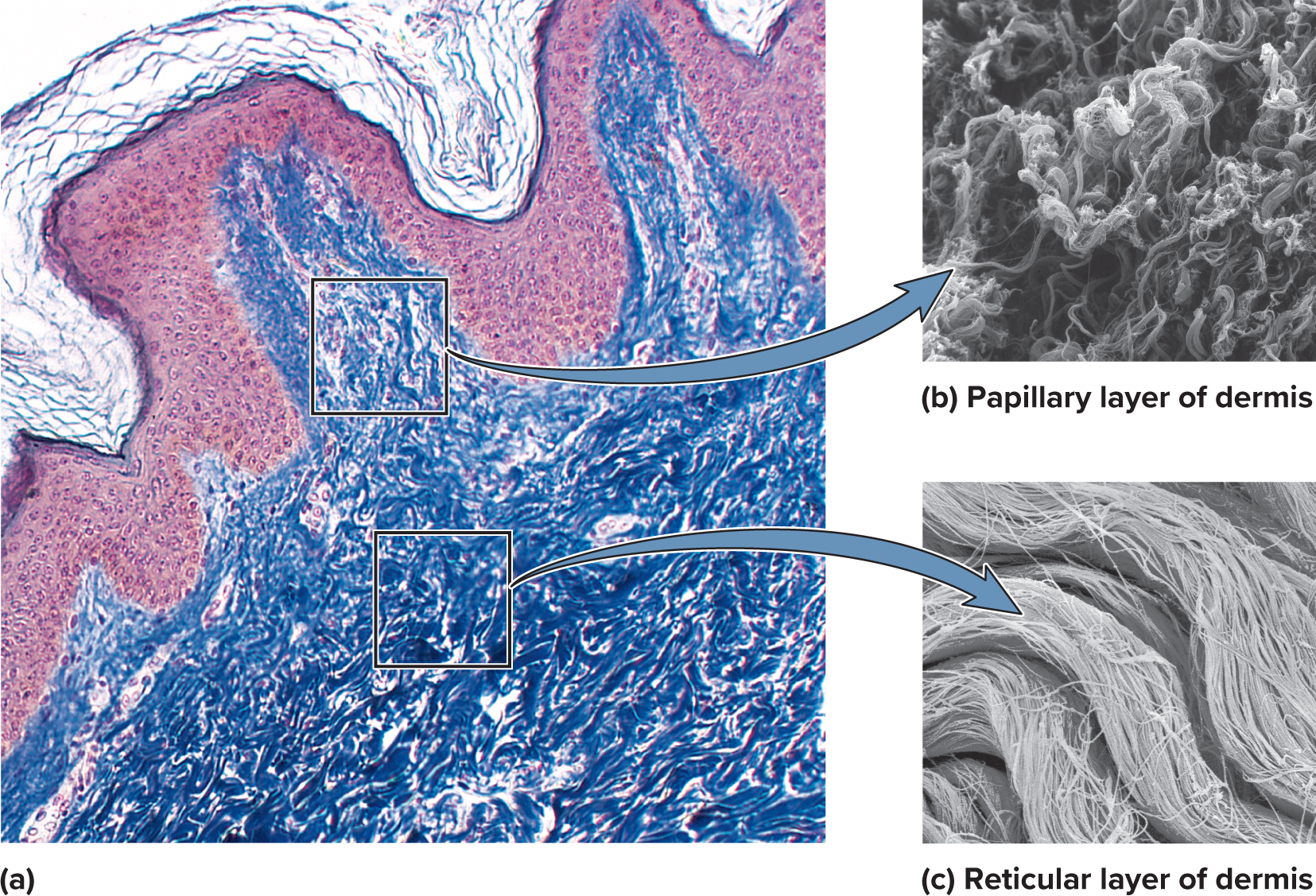
what does the loosely organized tissue of the papillary layer allow for?
mobility of leukocytes and other defenses against organisms introduced through breaks in the epidermis
reticular layer
a deeper and much thicker layer of dense irregular connective tissue that’s more fibrous than cellular which makes it tougher than the papillary layer
describe the vague boundary between the papillary and reticular layers
in the reticular layer the collagen forms thicker bundles with less room for ground substance with small adipocyte clusters often
what causes stretch marks?
stretching of the skin which tears collagen fibers
where are stretch marks most common?
buttocks
thighs
abdomen
breasts
blister
serous fluids seeping out of the vessels and accumulating which separates the epidermis from the dermis
how do blisters go away?
the fluid is reabsorbed or expelled when ruptured
hypodermis
a layer of connective tissue deep to the skin; also called superficial fascia, subcutaneous tissue, or when it is predominantly adipose, subcutaneous fat
hypodermis structure
no sharp boundary between dermis and hypodermis
more areolar and adipose tissue
pads the body and binds the skin to the underlying tissues
how are drugs introduced to the body?
hypodermic injection because the subcutaneous tissues are highly vascular and absorb them quickly
subcutaneous fat
hypodermis composed mainly of adipose tissue
subcutaneous fat purpose
energy reservoir and thermal insulation
protects deeper tissue by absorbing pressure and blows to the body
characteristics of subcutaneous fat
not uniformly distributed
mostly absent in scalp
abundant in breasts, abdomen, hips, and thighs
50% of total body fat
8% thicker in women
infants and elderly have less making them sensitive to cold
what causes variation in hair and skin color?
varieties and amounts of melanin
two classes of integumentary melanin
dark eumelanin
reddish yellow pheomelanin
two subtypes of eumelanin
brown and black eumelanin
what do brown and black eumelanin do?
underlie the colors of tan, brown, and black skin including the effects of suntanning
where does pheomelanin get its color from?
higher sulfur content
which ethnic groups commonly have pheomelanin?
yellowish to reddish tones for Asians and native Americans
pinkish tones for white skin
what other factors contribute to skin color?
how close blood vessels are to surface
show through of white collagen
carotene which can accumulate in stratum corneum, dermis, and subcutaneous fat
amount of UV exposure
carotene
pigments of yellow and orange vegetables
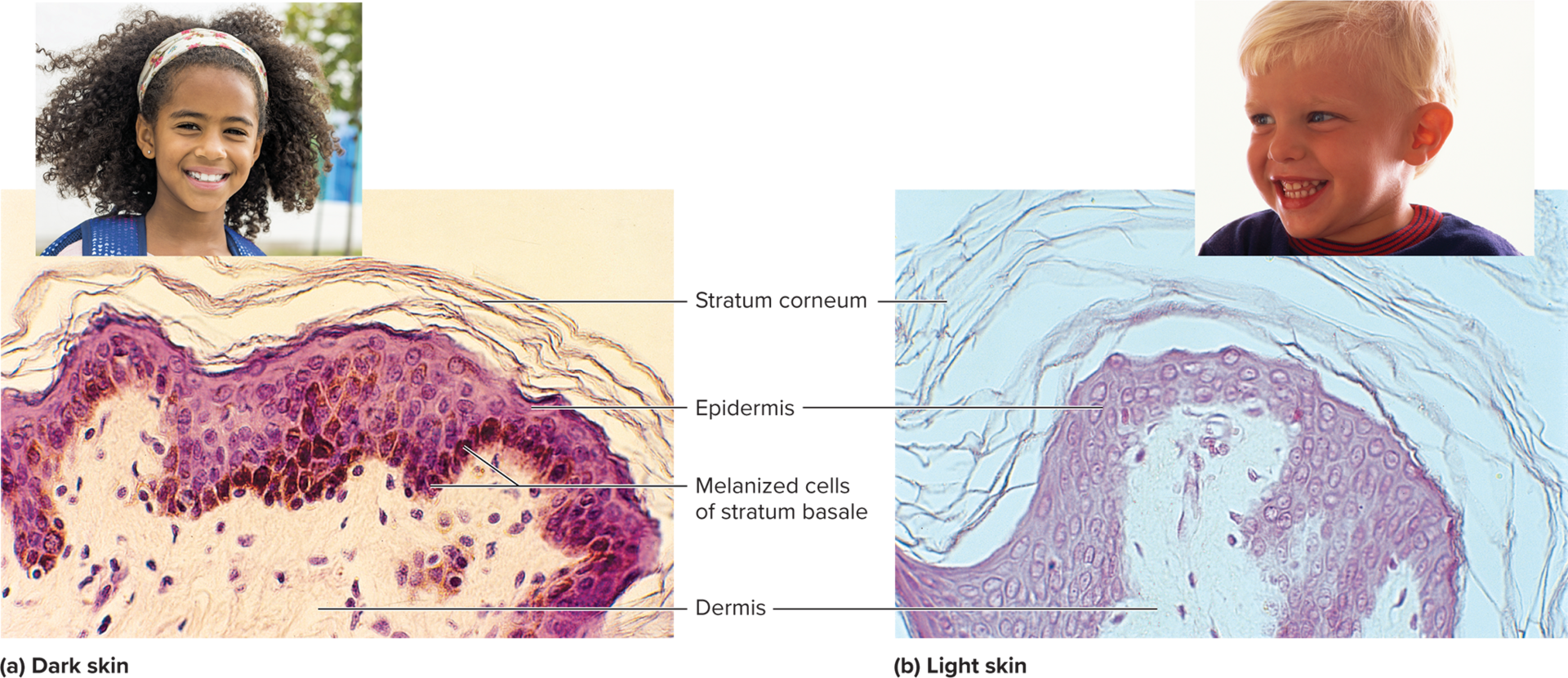
where is most of melanin located?
stratum basale but extends through the epidermal strata in dark complexions
what makes skin darker?
for darker skin melanocytes produce greater quantities of pigment
melanin granules in keratinocytes are more spread out
melanin breaks down slowly
what makes skin light?
melanin is less abundant and clumped near keratinocyte nucleus which means less color
breaks down more rapidly so little is seen beyond stratum basale
where is melanin more concentrated?
freckles and moles
dorsal surfaces of hands and feet
nipple and areola
around anus
on scrotum and penis
lateral surfaces of female genital folds (labia majora)
effects of ultraviolet radiation
skin cancer
free radicals that destroy immune dendritic cells of epidermis
damages protein and DNA
breaks down folate which is a B vitamin needed for normal cell division
what can a folate deficiency cause?
infertility
severe birth defects such as spina bifida and prenatal death
benefits of UVR
stimulates keratinocytes to make vitamin D
what does vitamin D do?
calcium metabolism
bone health
fetal and childhood development
cell growth
neuromuscular and immune functions
why do women worldwide on average have 4% lighter skin than men do?
greater need of vitamin D and calcium to support pregnancy and lactation
what makes UVR increase?
higher elevations and in dry air that’s thinner and filters out less of it
what outside factors can affect skin colors?
human migration
intermarriage between different geographic ancestries
cultural differences between clothing and shelter
preference for certain skin colors
mutations
abnormal skin conditions
cyanosis
erythema
pallor
albinism
jaundice
hematoma
hematoma
a mass of clotted blood in the tissues; forms a bruise when visible through the skin
hematoma causes
accidental trauma
hemophilia
metabolic or nutritional disorders
abuse
erythema
abnormal redness of the skin
erythema causes
exercise
hot weather
sunburns (dermal pooling of RBCs that escape from damaged capillaries)
anger
embarrassment
increased blood flow in dilated cutaneous blood vessels