Central Nervous System (CNS)
1/302
Earn XP
Description and Tags
help me.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
303 Terms
Neurons
Functional unit of the nervous system, generate action potentials.
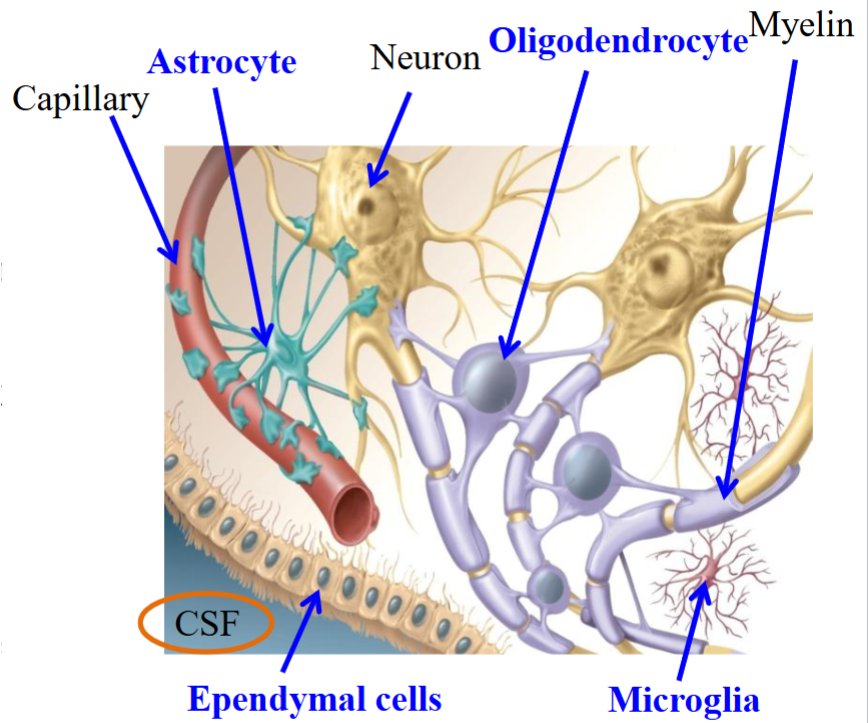
Gila
Non-neuronal cells that support neurons (do not generate action potentials).
Provide scaffolding; allows neurons to line up closely with each other for neuronal communication, insulation, nutrients, waste, and mediate immune responses.
Supportive cells in the CNS.
Nerve
Bundle of axon or fibers that travel together.
Not a neuron.
Central Nervous System (CNS)
Integrating and command center; brain and spinal cord.
The integrating center that evaluates incoming information and initiates a response through APs in efferent neurons.
Peripheral Nervous System (PNS)
Nerves connecting brain to peripheral structures.
Divided into the afferent/sensory division and the efferent/motor division, which is further divided into subcategories.
Afferent/Sensory Division
A division of the PNS.
Axons of afferent neurons carry sensory information from peripheral receptors to the CNS.
Divided into three parts for somatic information:
Somatic sensory, visceral sensory, and special sensory.
Somatic Sensory Division
A subcategory of the afferent/sensory division, which is a part of the peripheral nervous system.
Brings information on the spatial limits of the body.
Visceral Sensory
A subcategory of the afferent/sensory division, which is a part of the peripheral nervous system.
Information on the internal organs, especially the abdominal organs.
Special Sensory
A subcategory of the afferent/sensory division, which is a part of the peripheral nervous system.
Information from sight, hearing, equilibrium, taste, and smell (the five senses).
Efferent/Motor Division
A subdivision of the PNS.
Neurons carry motor information to the periphery.
"Motor" refers to causing movement.
Divided into further subdivisions:
Somatic motor → skeletal muscles.
Autonomic motor (sympathetic, parasympathetic, and enteric) → smooth & cardiac muscle, glands.
Ganglion
A collection of cell bodies (soma) located outside the CNS.
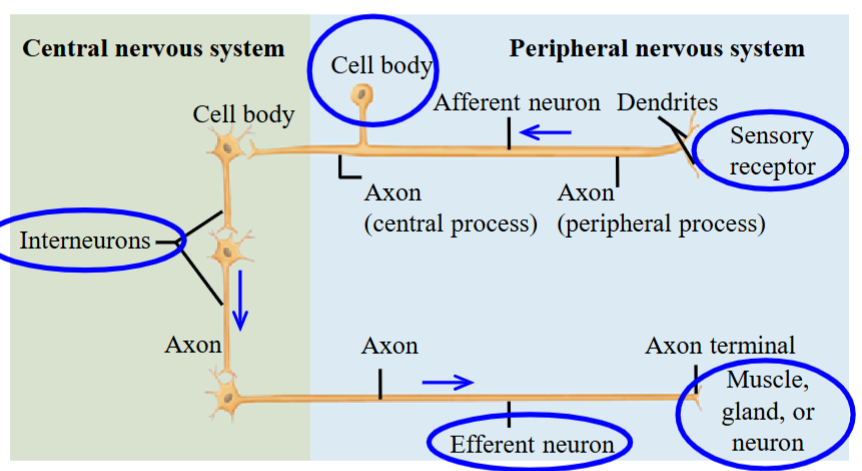
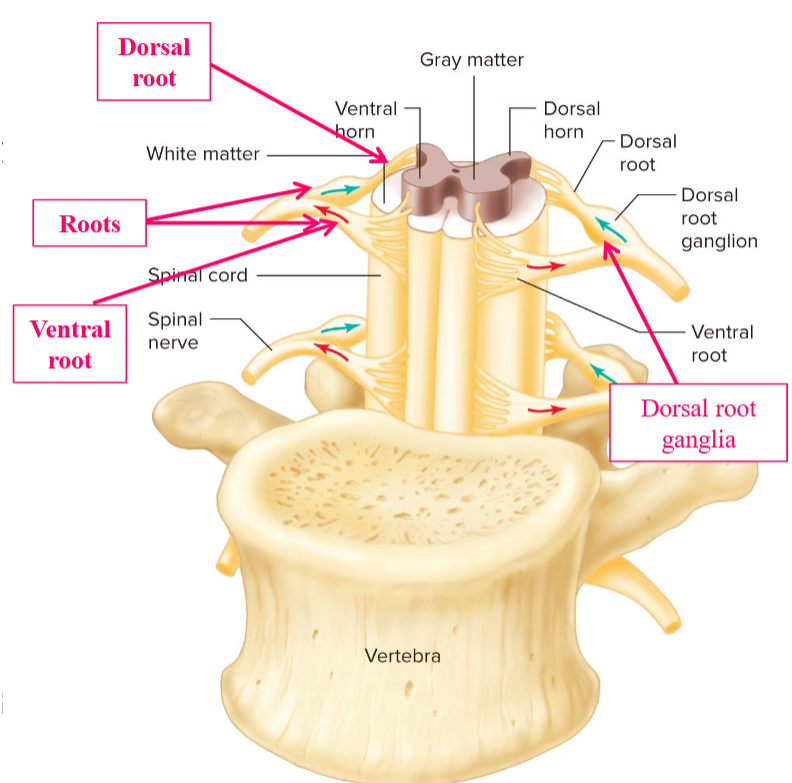
CNS/PNS Pathway
The sensory receptor sends a stimulus to the afferent neuron, which is located outside the spinal cord.
Called the posterior root ganglion, also known the dorsal root ganglion.
The AP goes to the interneurons, which sends it to the efferent neurons.
The efferent neurons innervate effector organs.
Includes skeletal muscles in the somatic division, smooth muscle, cardiac muscle, and glands in the autonomic division.
Astrocytes
Physically support neurons (“scaffold”) → holds neurons together.
Forms blood-brain barrier.
Repair: form scar tissue (which unfortunately inhibits regeneration of severed axons) → this inhibition is a barrier of the recovery of function.
Turnover (recycle) neurotransmitter molecules.
Maintain electrolyte balance ([Na⁺], [K⁺], [Ca²⁺], pH, etc).
H⁺ ions determines the acidity of the fluids around the cells in the CNS.
![<ul><li><p>Physically support neurons (“scaffold”) → holds neurons together.</p></li><li><p>Forms blood-brain barrier. </p></li><li><p>Repair: form scar tissue (which unfortunately inhibits regeneration of severed axons) → this inhibition is a barrier of the recovery of function.</p></li><li><p>Turnover (recycle) neurotransmitter molecules. </p></li><li><p>Maintain electrolyte balance ([Na⁺], [K⁺], [Ca²⁺], pH, etc). </p><ul><li><p>H⁺ ions determines the acidity of the fluids around the cells in the CNS. </p></li></ul></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/fe4ab496-456f-4c83-9abf-eb96cf0ee4fa.png)
Oligodendrocytes
Form myelin sheaths that electrically insulate axons.
∴ Increases conduction velocity.
Means “relatively few branches.”
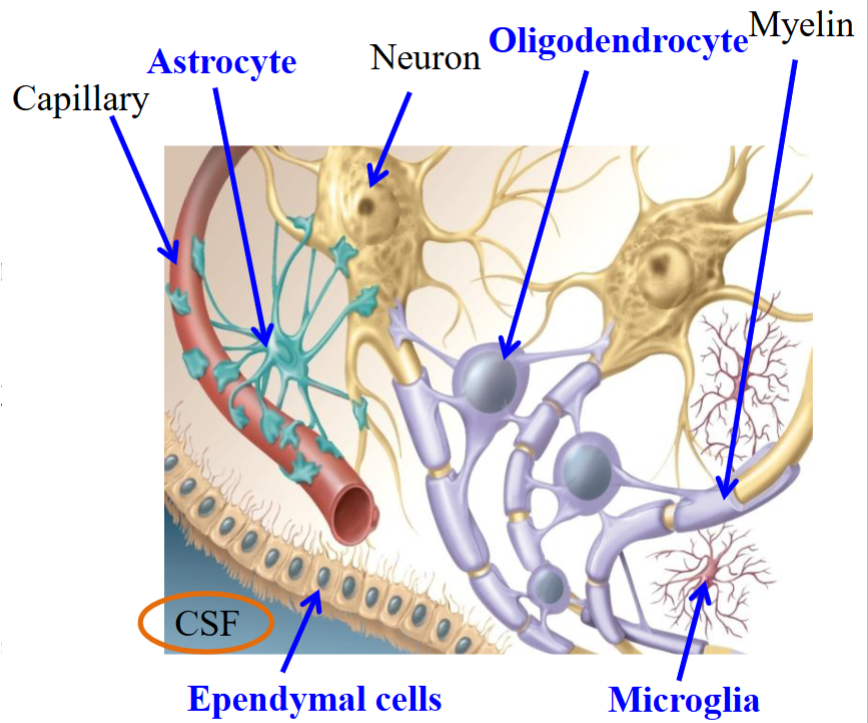
Ependymal Cells
Produce cerebrospinal fluid (CSF).
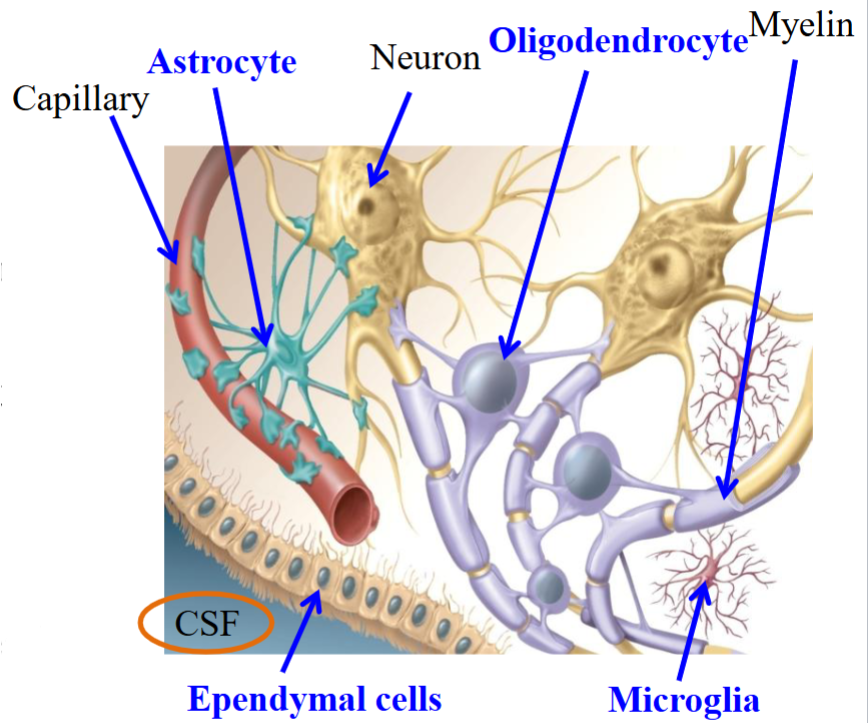
Microgila
Scavengers: ingest bacteria and debris.
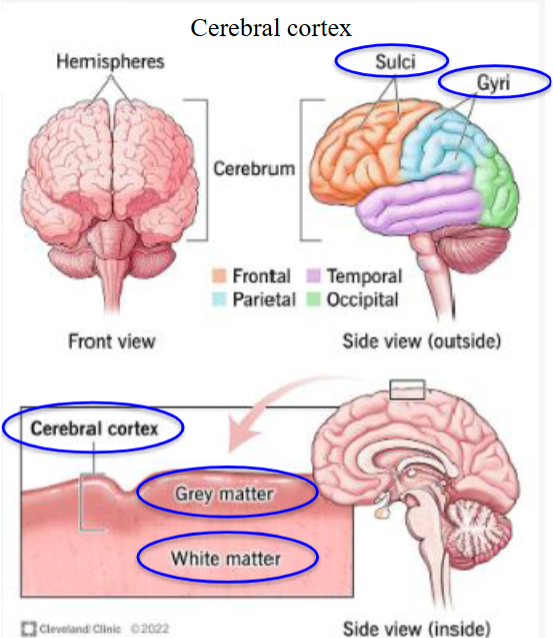
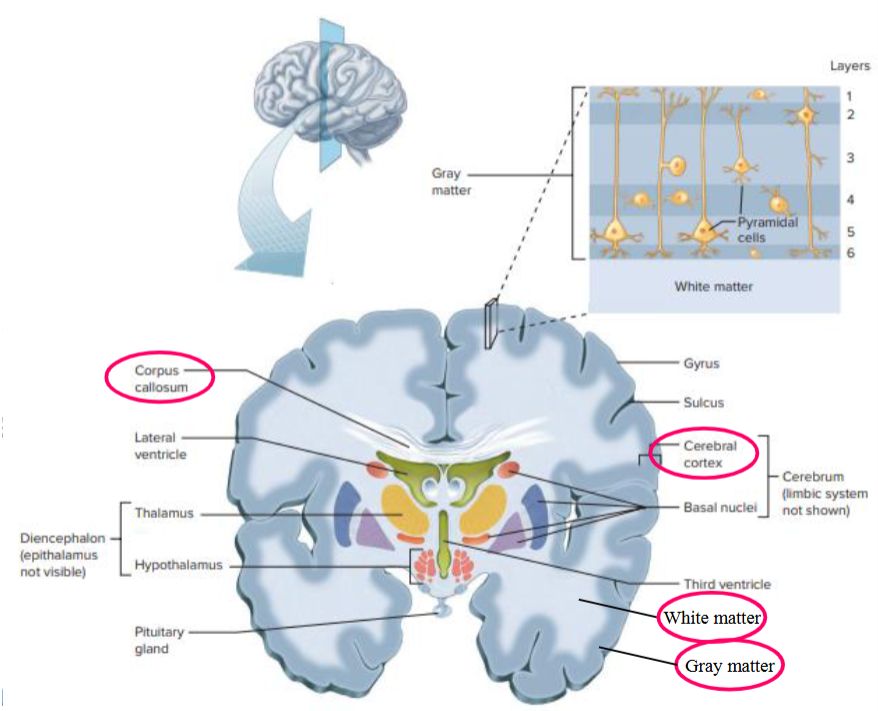
Gray Matter
Consists of unmyelinated nerve cell bodies, dendrites and axon terminals.
Cell bodies are assembled in a organized fashion in both the brain and spinal cord.
Nuclei → clusters of cell bodies in the brain and spinal cord: usually identified by specific names.
Nuclei forms layers in some parts of the brain and in other parts, they cluster into groups of neurons with similar functions.
White Matter
Consists mostly of myelinated axons and very few cell bodies.
Myelin sheaths that surround the axons give the white colour.
Surrounds gray matter; contains axon bundles that carry ascending sensory signals or descending motor commands.
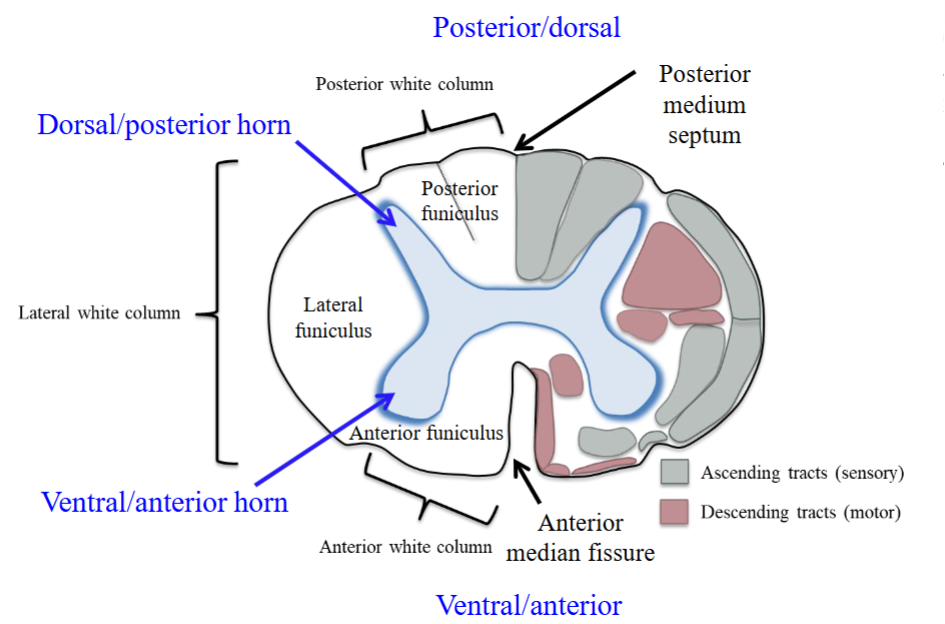
In each half of the spinal cord, the white matter is divided into 3 parts, called columns or funiculi.
Tracts
Bundle of axons that connect different regions of the CNS.
Tracts in the CNS are equivalent to nerves in the PNS.
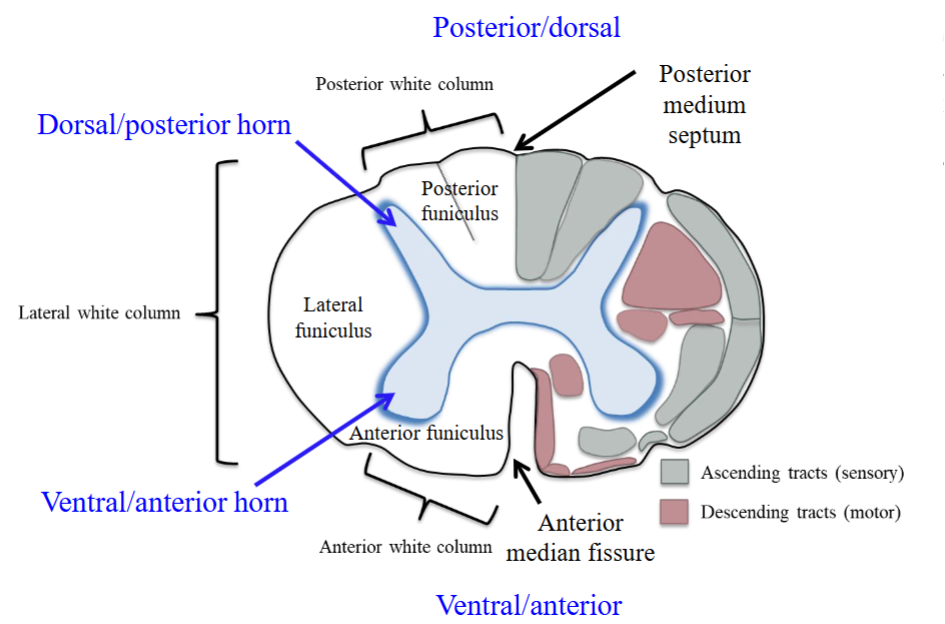
Fasciculus
A distinct collection of nerve fibers in the CNS.
These collections are named according to their origin and termination.
Each white column (funiculus) is subdivided into fasciculi—tracts that are either ascending (sensory) or descending (motor).
Plural: fasciculi.
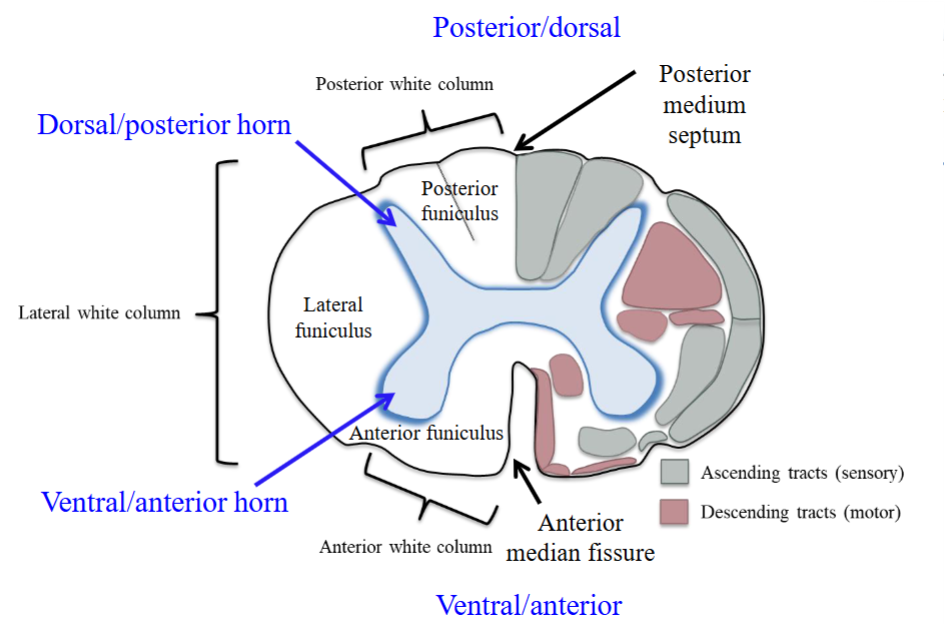
Columns/Funiculi
Three pairs of these white matter bundles.
Posterior/dorsal, lateral, and anterior/ventral columns on each side.
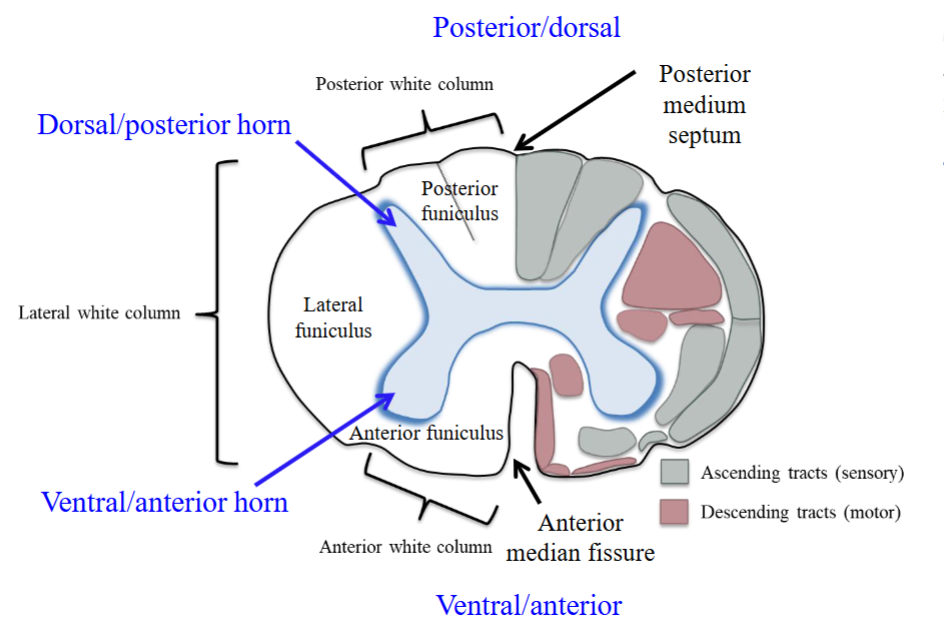
Posterior/Dorsal Funiculus
Found between the posterior medium septum and the dorsal/posterior horn.
Also called the posterior white column.
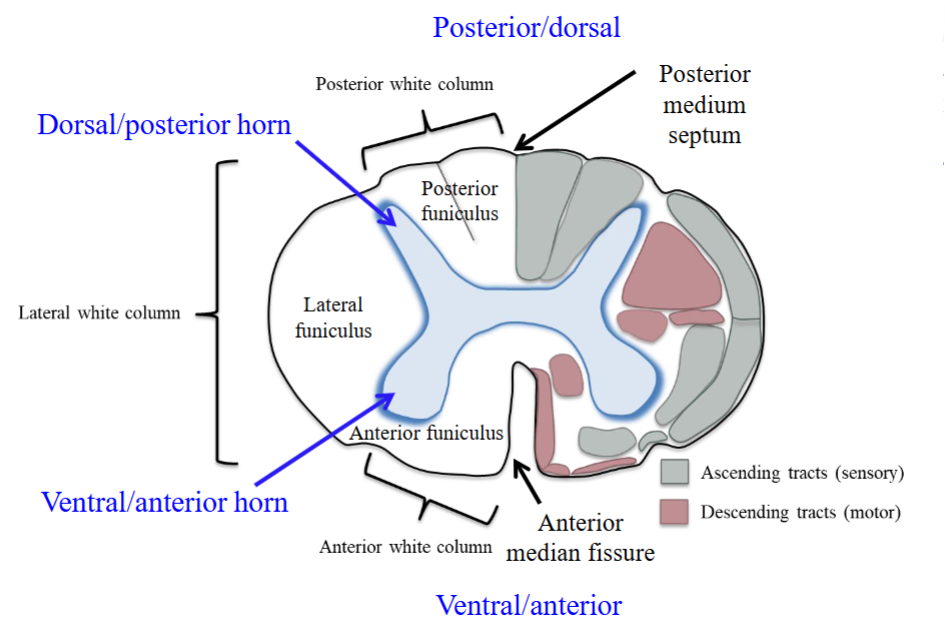
Lateral Funiculus
Found between the ventral/anterior horn and the dorsal/posterior horn.
Also called the lateral white column.
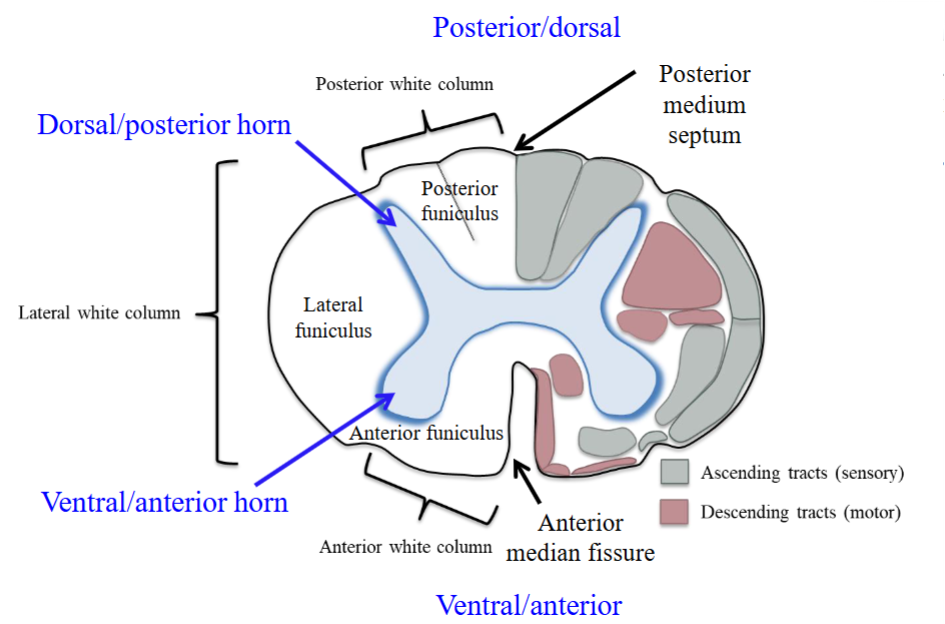
Ventral/Anterior Funiculus
Between the ventral horn and median fissure.
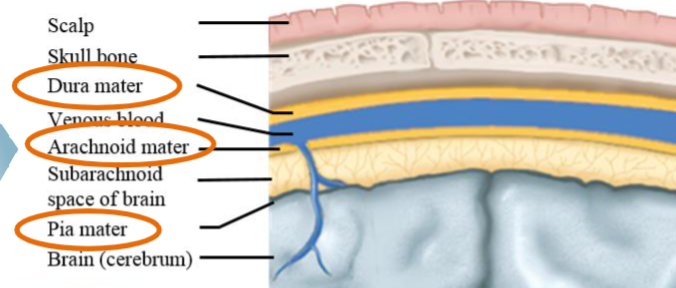
Protective Elements of the CNS
Neural tissue has minimal extracellular matrix and must rely on external support for protection from trauma.
Comes from a outer casing of bone, three layers of tissue membrane, fluid b/w membranes.
Consists of bone, meninges, cerebrospinal fluid, and blood brain barrier (BBB).
Bone
The first protective layer for the CNS.
Skull (cranium) for brain.
Vertebrae for spinal cord.
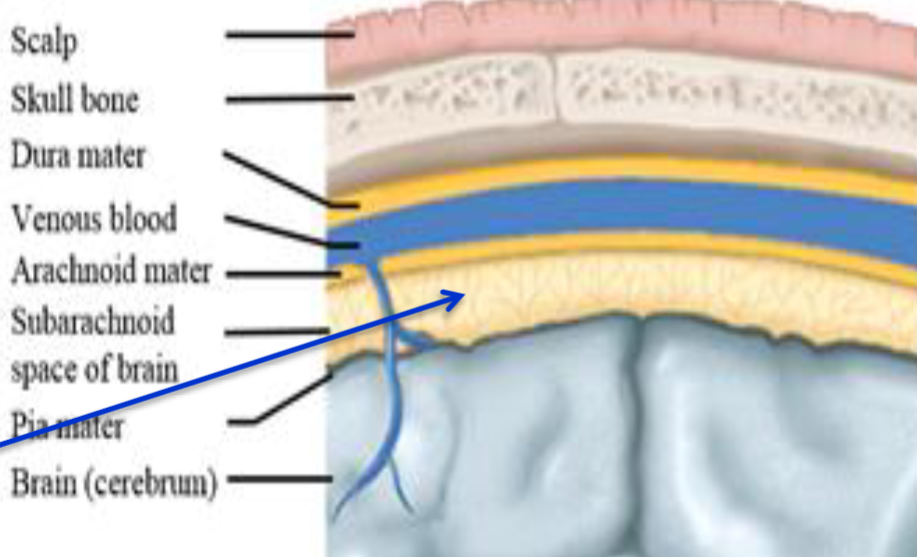
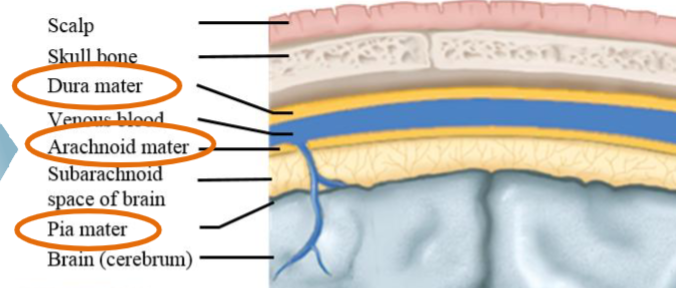
Meninges
Three layers of membranes lie between the bone and the tissue of the CNS, helping to stabilize the neural tissue and protect it from bruising against the bones of the skeleton.
These layers are the dura mater, arachnoid mater, and pia mater.
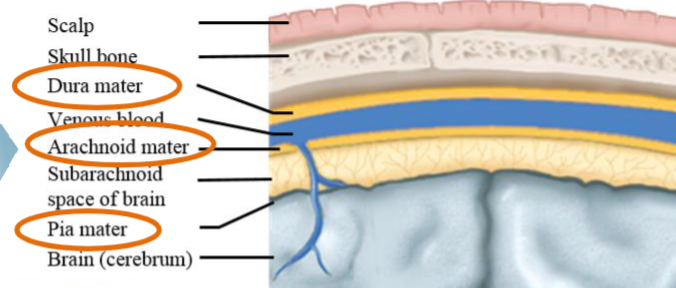
Dura Mater
The tough outer layer of the meninges.
Loosely tied to the pia mater, leaving a subarachnoid space between the two layers.
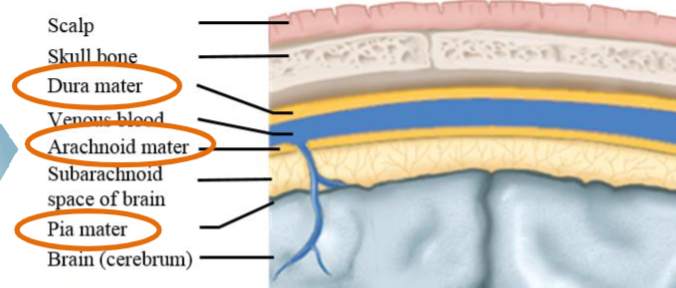
Arachnoid Mater
Spidery intermediary mesh.
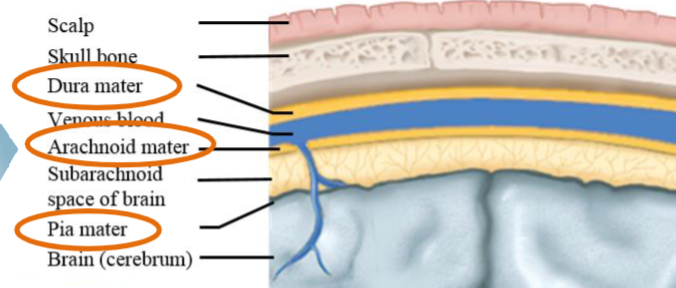
Pia Mater
Delicate inner layer.
Adheres to the surface of the brain and spinal cord.
Meningitis
Infection of the meninges.
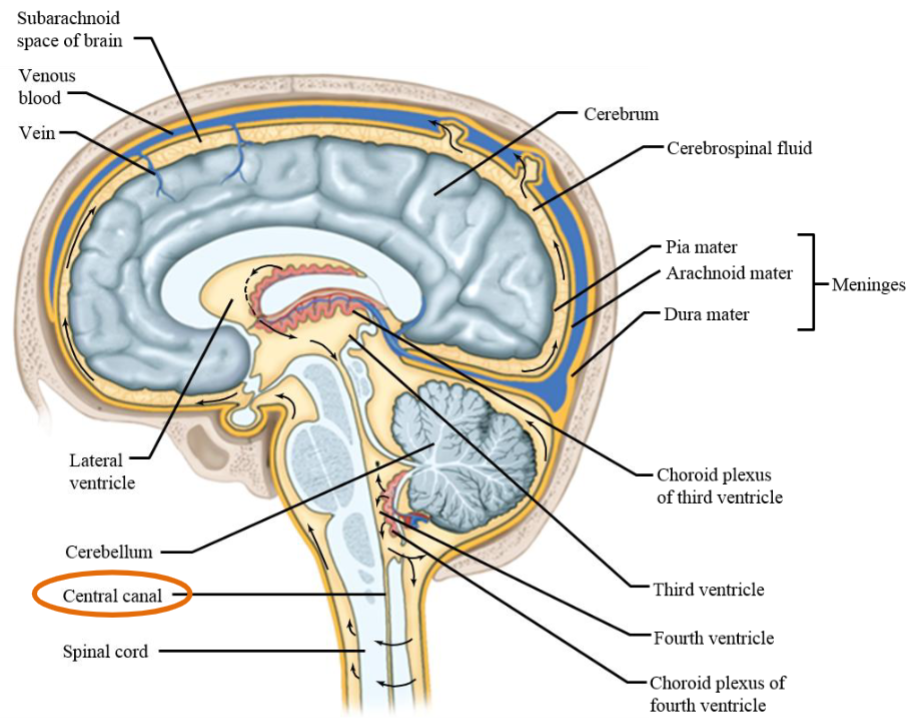
Cerebrospinal Fluid (CSF)
Produced in brain ventricles by the choroid plexus.
Helps cushion from injury and provide nutrients.
The CSF provides mechanical protection → supports neural tissues. When the head tilts, the fluid must be compressed before the brain can tilt inside the cranium.
Maintains electrolyte balance around neurons.
Reabsorbed into venous blood.
Choroid Plexus
A complex network of capillaries lined by specialized cells.
Ventricles produce CSF, produced by a thin layer of cells that line the ventricles.
Consists of capillaries and a transporting epithelium.
Produces CSF at a relatively steady rate.
Ventricles
An interconnected series of cavities filled with CSF.
CSF Reabsorption
CSF flows around the neural tissue and is absorbed into the blood by special villi on the arachnoid membrane in the cranium.
The CSF gets reabsorbed into the blood via the venous system at the same rate is produced.
Hydrocephalus
“Water in the brain.”
Occurs when reabsorption is blocked, CSF accumulates; treated surgically with drainage tubes.
This creates increased pressure in the cavities of the CNS, which includes the ventricles and a canal that runs down the spinal cord.
If untreated, brain tissue is crushed against the inner surface of the skull.
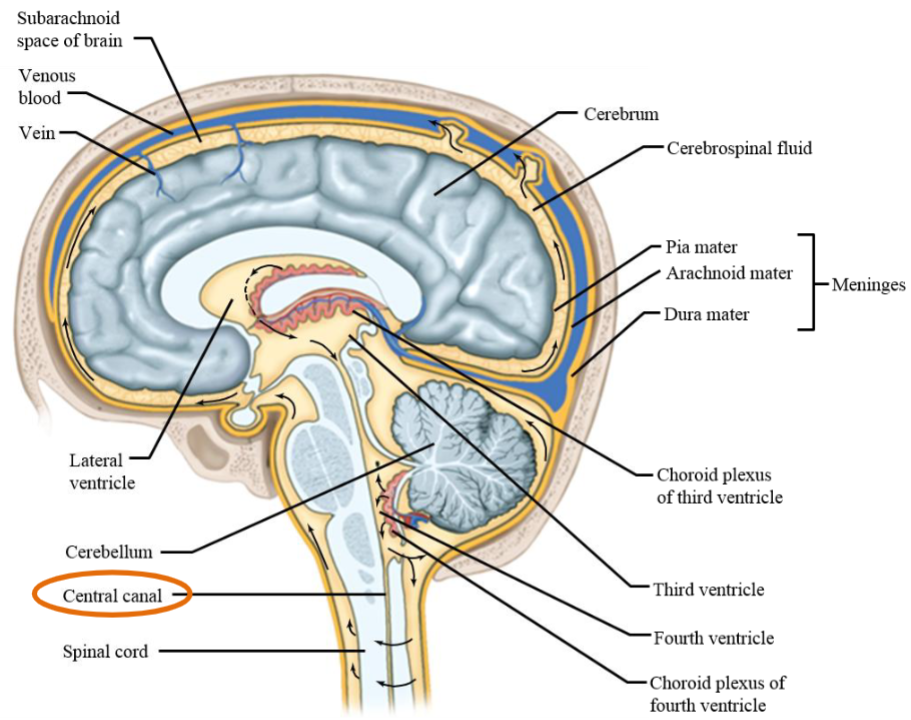
Spinal Central Canal (SCC)
Plays a crucial role in cushioning the spinal cord and facilitating the exchange of nutrients and waste products.
Hydrocephalus occurs in the SCC.
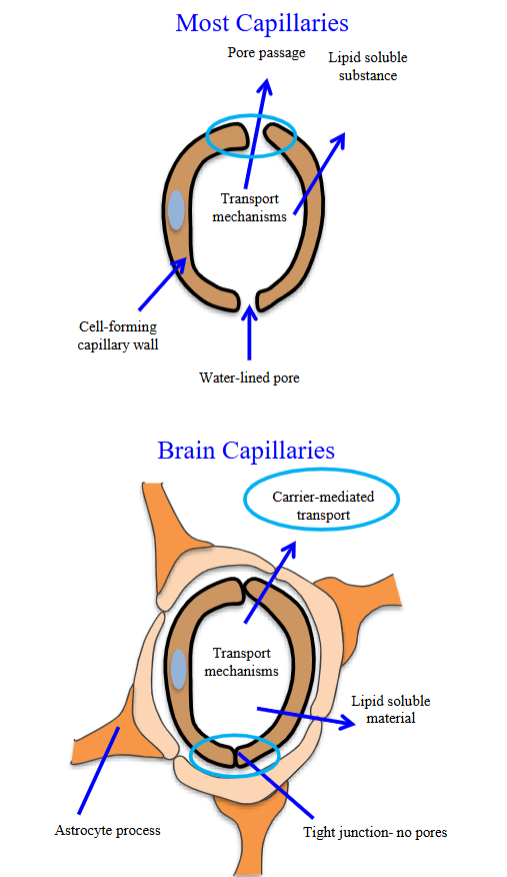
Blood-Brain Barrier (BBB)
Capillaries in CNS are less porous than in rest of body.
Protects neurons from chemical fluctuations.
Provides oxygen and glucose.
Selectively transports molecules.
BBB Chemical Fluctuations
Protects neurons from chemical fluctuations and harmful agents.
This is a good thing because neurons are protected from large molecules that may be harmful.
BBB Oxygen and Glucose
The BBB provides oxygen and glucose; the brain does not have glycogen stores.
This is done through carrier-mediated transport. As a result, oxygen and glucose are able to enter the brain.
BBB Selective Transport
The BBB selectively transports molecules needed by brain (i.e. glucose) while excluding harmful ions, hormones, etc.
Molecules are selectively transported to the neurons from the capillaries, while harmful molecules are not transported.
However, this is a problem for delivering specific drugs to the brain (i.e. dopamine in Parkinson’s disease).
Cannot cross the BBB, so the precursor form of dopamine, L-dopa, is used.
Capillaries
Porous.
They have passages b/w the cells that make up the walls.
This allows fluid-containing electrolytes or much larger molecules (even WBCs) to exit from the interior of the capillary.
Capillaries in the brain are the exact opposite; requires carrier-mediated transport and is tightly joined together.
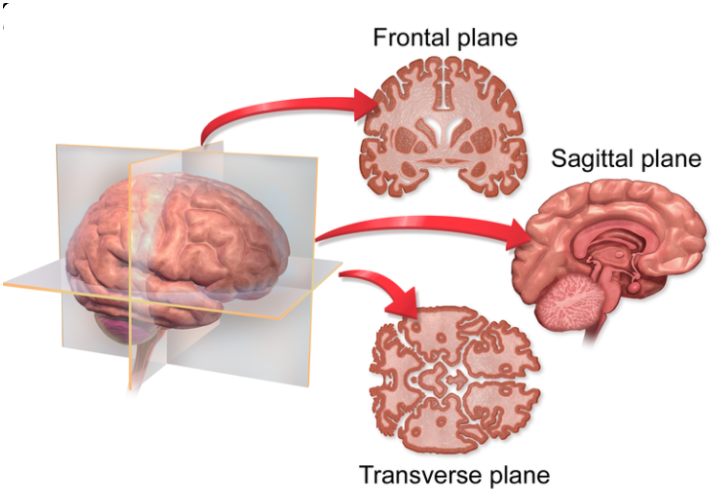
Coronal/Frontal Plane
A vertical plate which splits the brain into front and back sections.
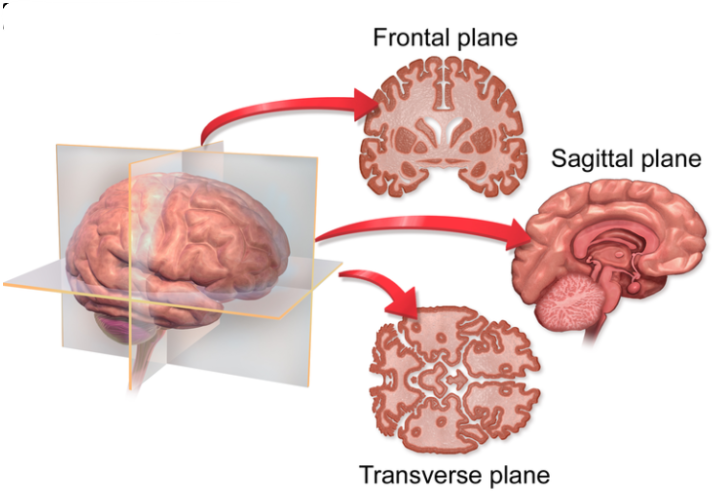
Sagittal Plane
A vertical plane which splits into left and right sections.
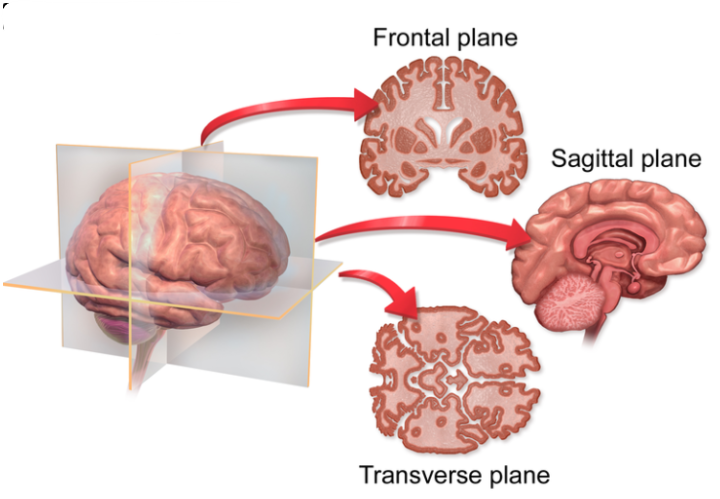
Horizontal/Transverse Plane
Splits the brain into the upper and lower sections.
Cephalic Flexure
The bend in the CNS arose in the long axis of the CNS as humans evolved upright posture.
This flexure leads to approx. 120° that forms in the region of the midbrain, b/w the hindbrain and forebrain.
Seen along this pathway in the region of the midbrain.
The longitudinal axis of the body and the longitudinal axis of the NS intersect at approximately the midbrain region.
The flexure has consequences for the application of standard anatomical terms used to specify location.
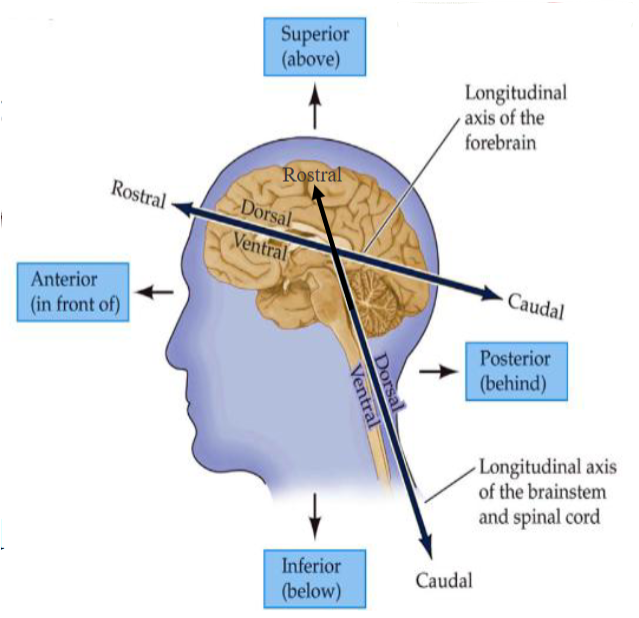
Long Axis of Body
The upright position of the body; does not include the neural bend.
Anterior — in front of.
Posterior — behind.
Superior — above.
Inferior — below.
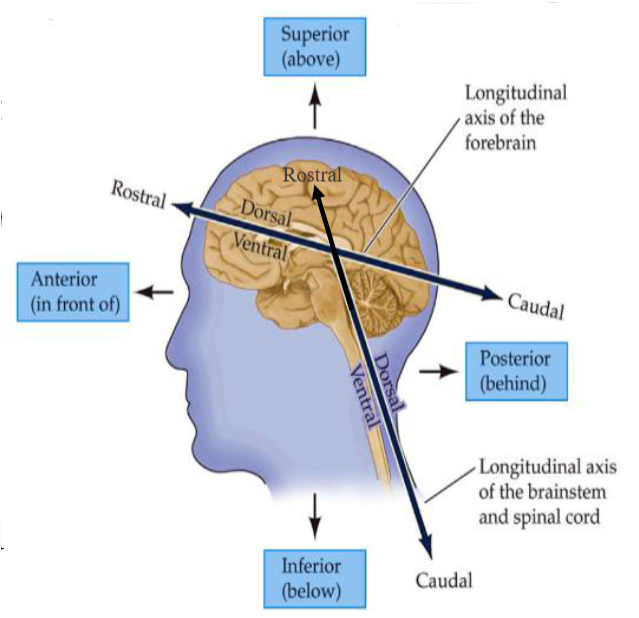
Long Axis of NS
Unlike the body, the long axis of the central nervous system bends at the midbrain.
Dorsal – toward the back (or top of the brain in the forebrain region)
Ventral – toward the front (or bottom of the brain in the forebrain region)
Rostral – toward the nose (front of the head/forebrain)
Caudal – toward the tail (spinal cord or back of the head)
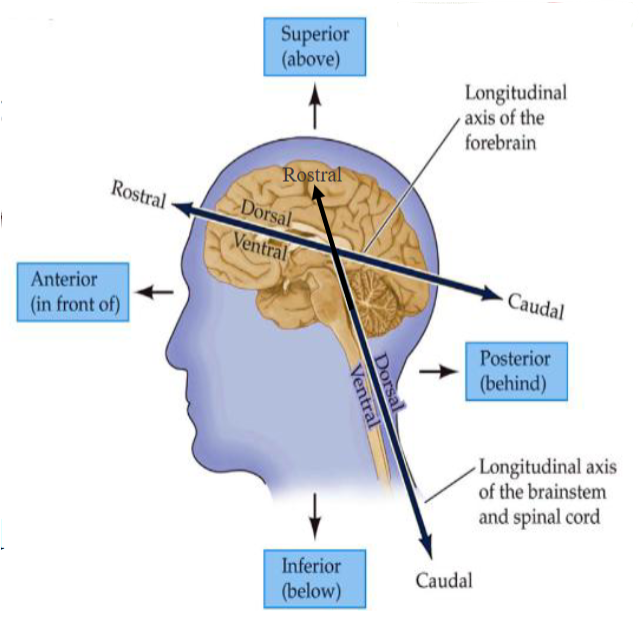
Embryonal Brain
During development, the CNS forms from a long tube.
The lumen of the tube remains in the adult brain as a fluid-filled space.
The fluid-filled space, known as the ventricular system, is filled with CSF and provides a important landmark in the NS.
∴ The entire brain is formed from the walls of the hollow tube.
As the brain grows, the shape of the central space changes from a simple tube to its complex adult form.
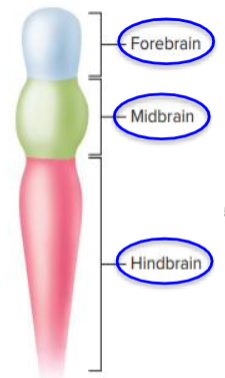
Cerebrum
Is a collective term that refers to the largest part of the 4 main parts of the brain.
It receives sensory information, processes it, regulates motor and conscious activity, and is responsible for a broad range of cognitive processes.
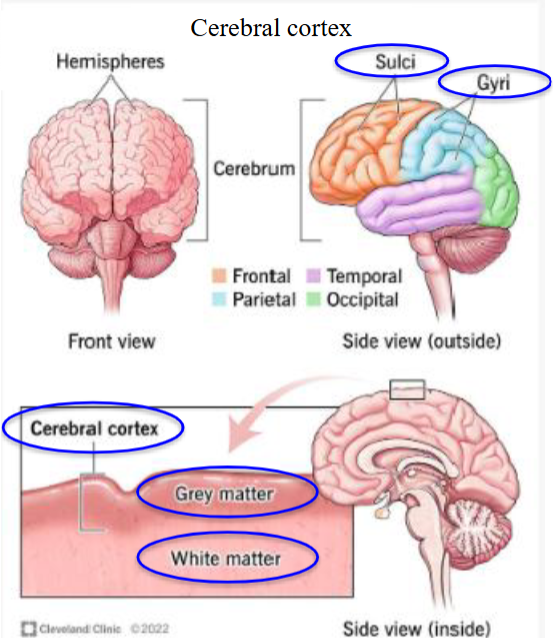
Cerebral Cortex
The outer layer of neural tissue of the cerebrum of the brain; folded into peaks called gyri and grooves called sulci; thin outer shell of gray matter.
Deals with sensory perception, motor control, language, cognitive functions such as thinking, memory, willed action, self-awareness, and the mind (the mind is hard to define).
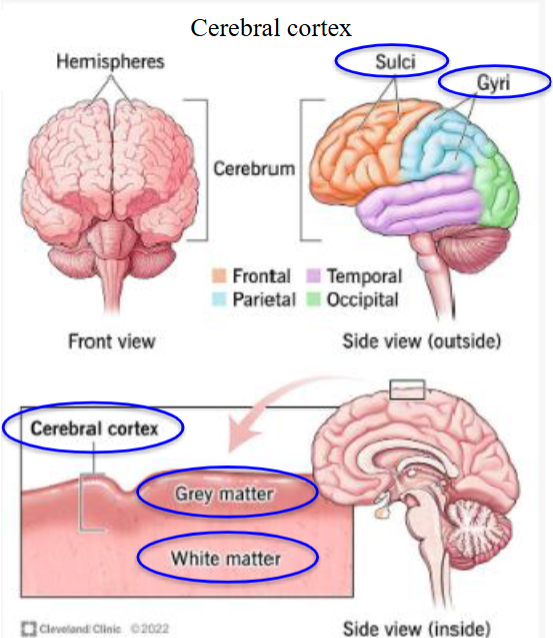
Sulcus and Gyrus
Plural is gyri, it is a fold or ridge in the cortex.
The plural is sulci, it is a groove in the cortex.
Corpus Callosum
Massive bundle of nerve fibers connecting left and right hemispheres.
Cranium
Part of the skull that encloses the brain and is made up of the 8 cranial bones.
Frontal bone, two parietal bones (right and left), two temporal bones (right and left), occipital bone, sphenoid bone, and ethmoid bone.
The lobes underneath the bones are named the exact same (i.e. frontal lobe, parietal lobe, etc).
Diencephalon
The region of embryonic vertebrate neural tube that gives rise to anterior forebrain structures such as the thalamus, epithalamus, hypothalamus (including posterior pituitary) and subthalamus.
Encloses the third cavity called the third ventricle.
Two main sections: thalamus and hypothalamus.
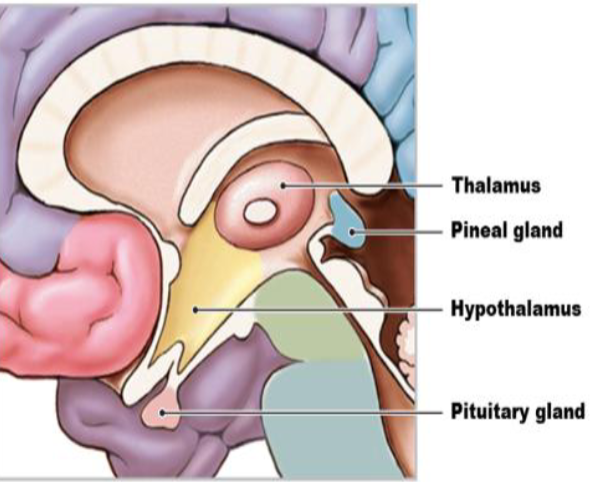
Thalamus
Integrating center and relay station for sensory and motor information.
Almost all sensory input from lower CNS regions passes through on its way to the cerebral cortex.
Shapes, selects, and relays sensory signals to the cerebrum (“sensory switchboard”).
Projects fibers to the cerebral cortex.
Participates in control of skeletal muscle coordination and plays a key role in awareness.
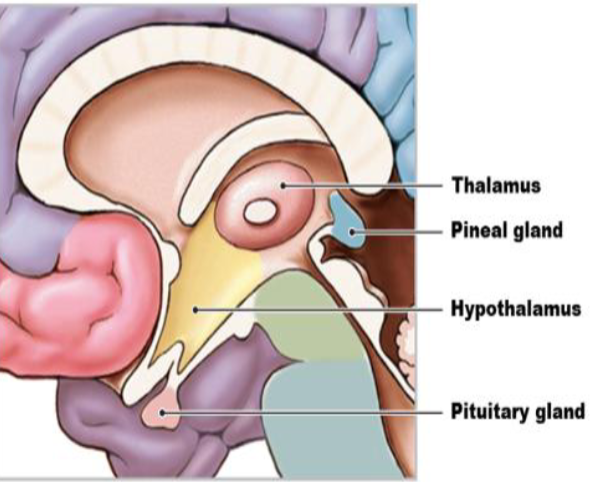
Epithalamus
Includes pineal gland.
Melatonin secretion.
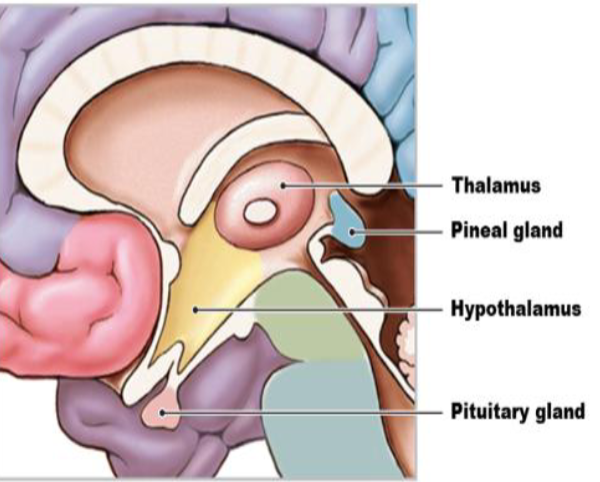
Hypothalamus
Homeostasis (temperature control, water balance, hunger) and behavioural drives.
Includes posterior pituitary.
Hormone secretion.
Emotions: fight/flight/freeze.
Subthalamus
Movement regulation.
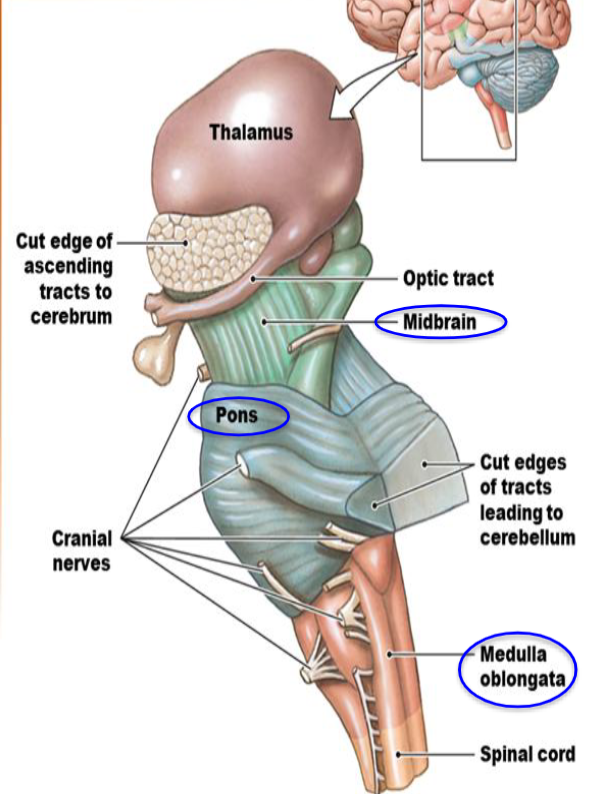
Midbrain
Also called mesencephalon.
A range of different clusters, pathways, and other structures.
In control of ocular movements.
Auditory and visual processing → recognizing and interpreting information through sight or sound.
Contains the substantia nigra → rich is dopamine neurons and part of the basal ganglia, which enables movement and coordination.
Part of the brainstem.
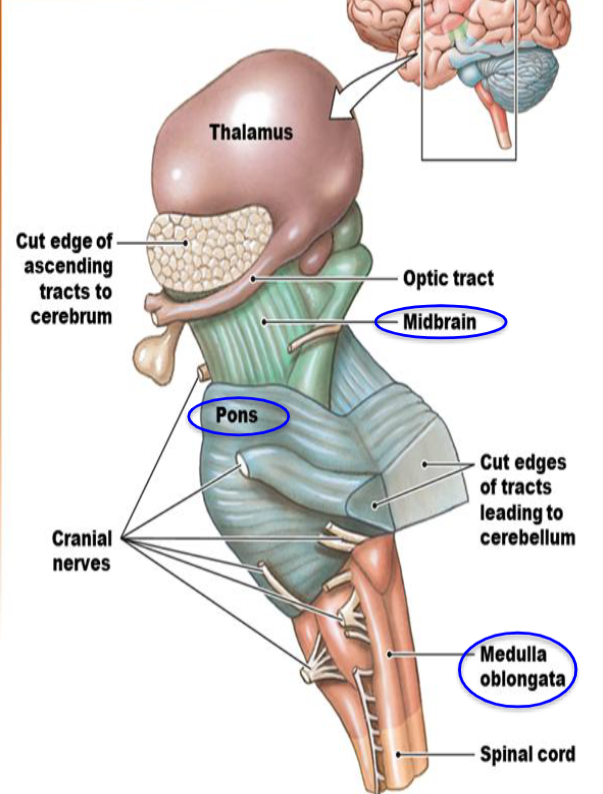
Pons
Connects the medulla oblongata with the midbrain.
Relay station between cerebrum and cerebellum.
Connects nerve fibers in cerebrum and cerebellum.
Plays a role in coordination of breathing along with centers in the medulla.
Part of the brainstem.
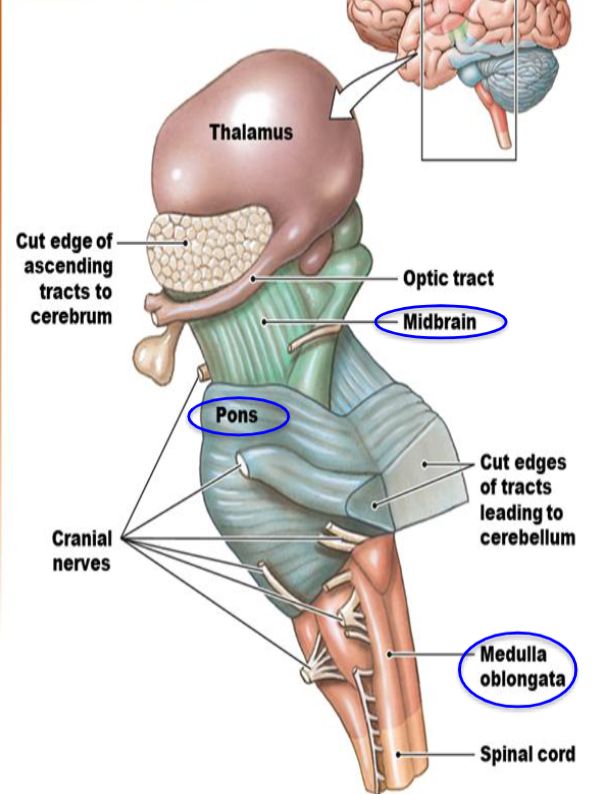
Medulla Oblongata
Control of involuntary functions.
Autonomic centers for regulation of visceral functions (Cardiovascular, respiratory, digestive activities).
Where the brainstem is connected to the spinal cord.
A part of the brainstem.
Frontal Section of Forebrain
Outer shell of gray matter composed of cell bodies (give the area a "grey” appearance”).
Inner layer of white matter composed of tracts of myelinated axons.
6 layers in the cerebral cortex.
Forebrain consists of cerebrum and diencephalon.
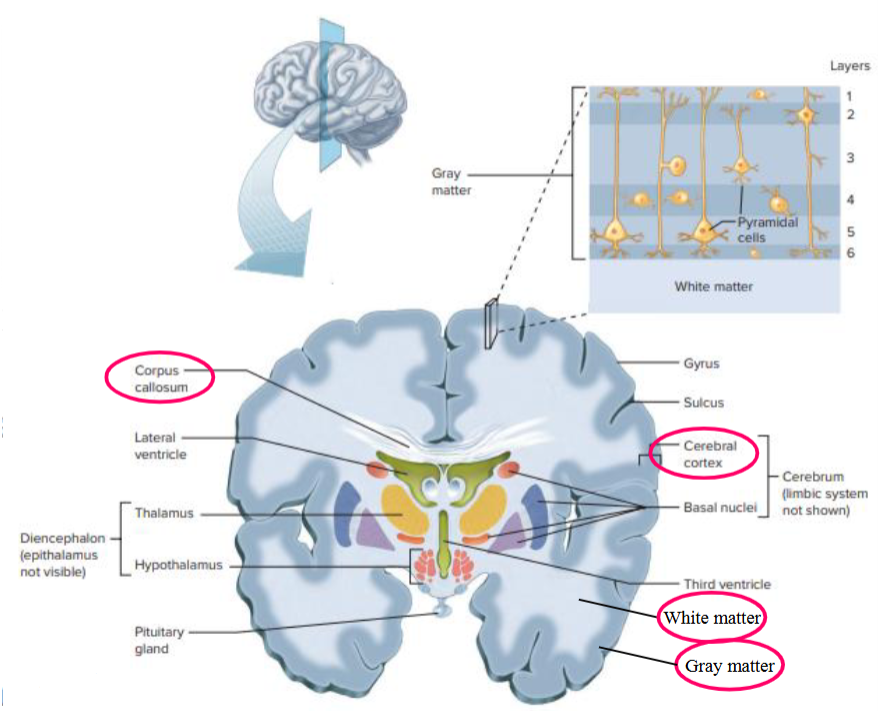
Cerebral Cortex
Refers to the outer layer of grey matter of the brain.
Contains trillions of neuronal cell bodies.
The inputs and outputs from the cell bodies are made of a huge number of nerve fibers.
6 layers of the cortex.
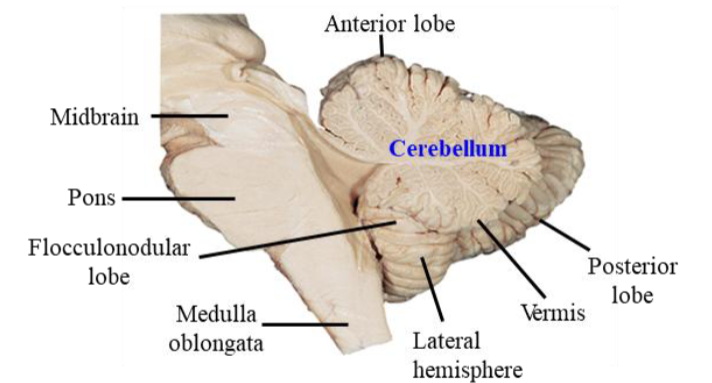
Cerebellum
Largely concerned with the control of movements, although recent studies have shown it also supports cognitive function.
Inputs:
Sensory input from spinal cord → for movement.
Motor commands from cerebral cortex → sends signals back into the brainstem and to the thalamus + cerebral cortex.
Functions: control of trunk and neck, locomotion, complex scaled movements (arms, hands, fingers), balance, and ocular movements.
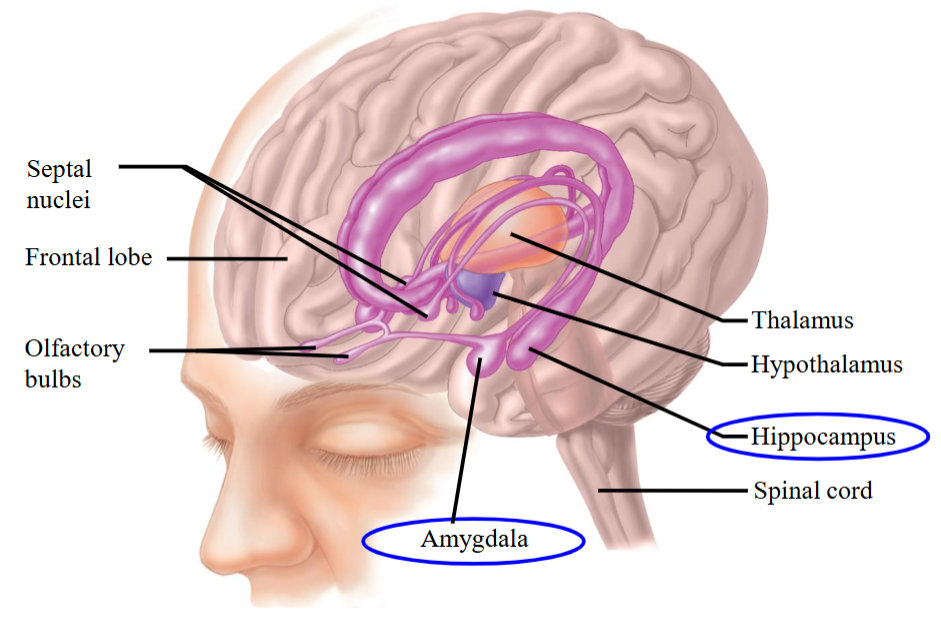
Limbic System
A ring of forebrain structures surrounding the brainstem, interconnected by complex neural pathways.
Involved in learning, emotion, sex, appetite (visceral), and endocrine integration.
Regulates behavioral and emotional responses, especially survival behaviors like feeding, reproduction, caring for young, and fight-or-flight.
Includes the thalamus, hypothalamus, basal ganglia, cingulate gyrus, hippocampus, and amygdala.
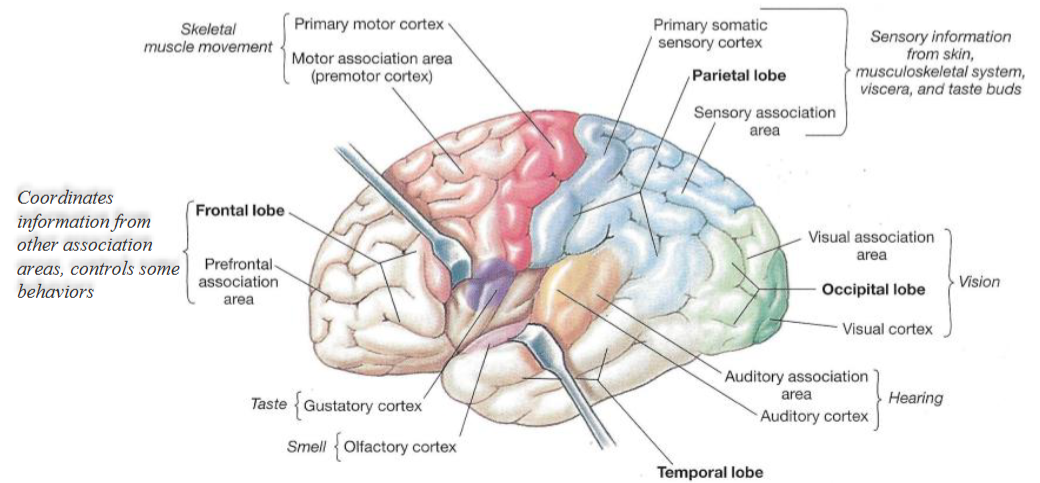
Frontal Lobe
Large area in humans associated with personality, emotions, and control of movement.
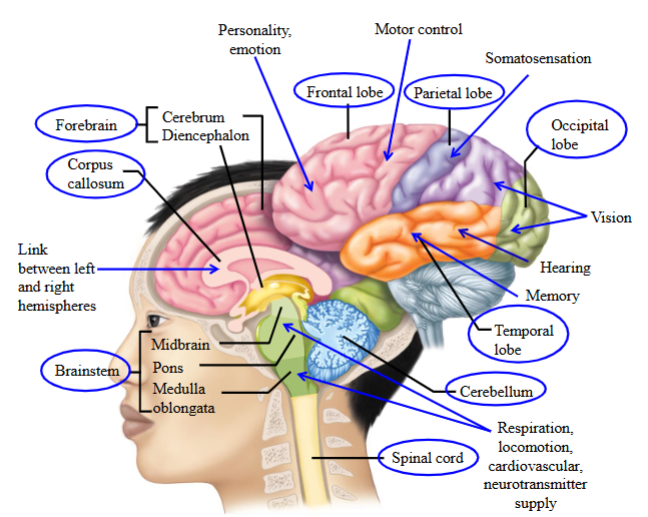
Parietal Lobe
Posterior to the frontal lobe, mediates skin and muscle sensation.
Somatosensation.
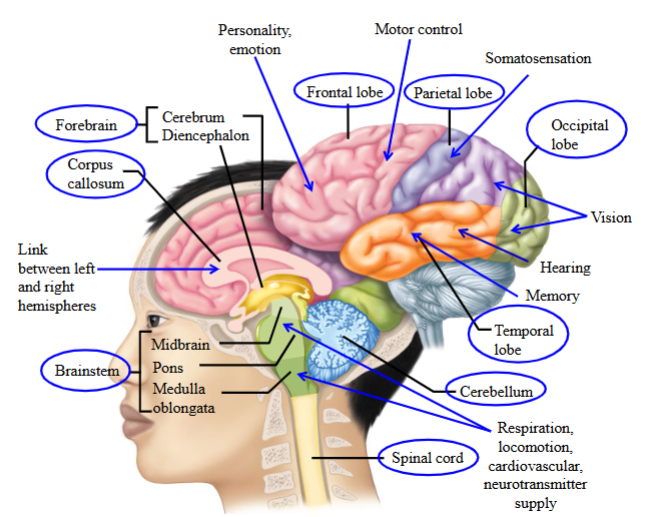
Occipital Lobe
Deals with vision.
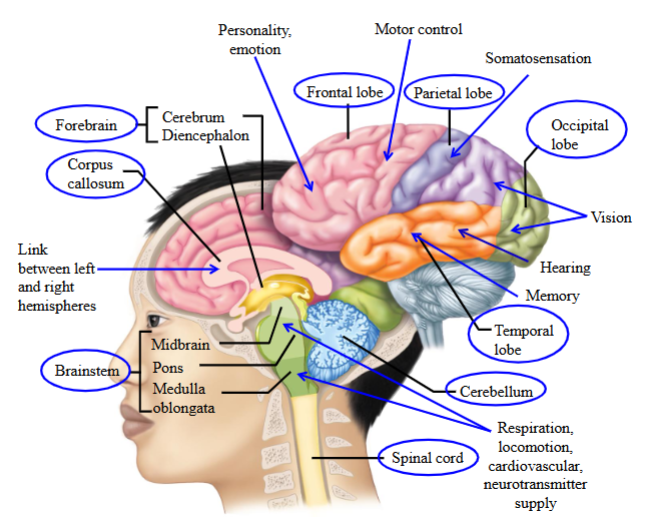
Temporal Lobe
Deals with hearing and memory.
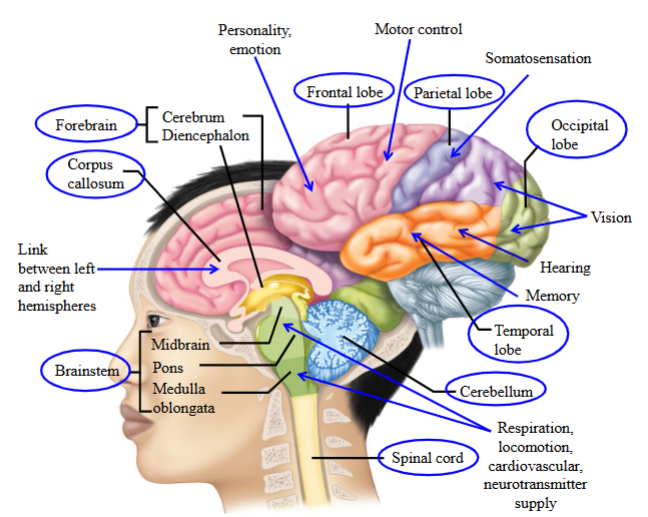
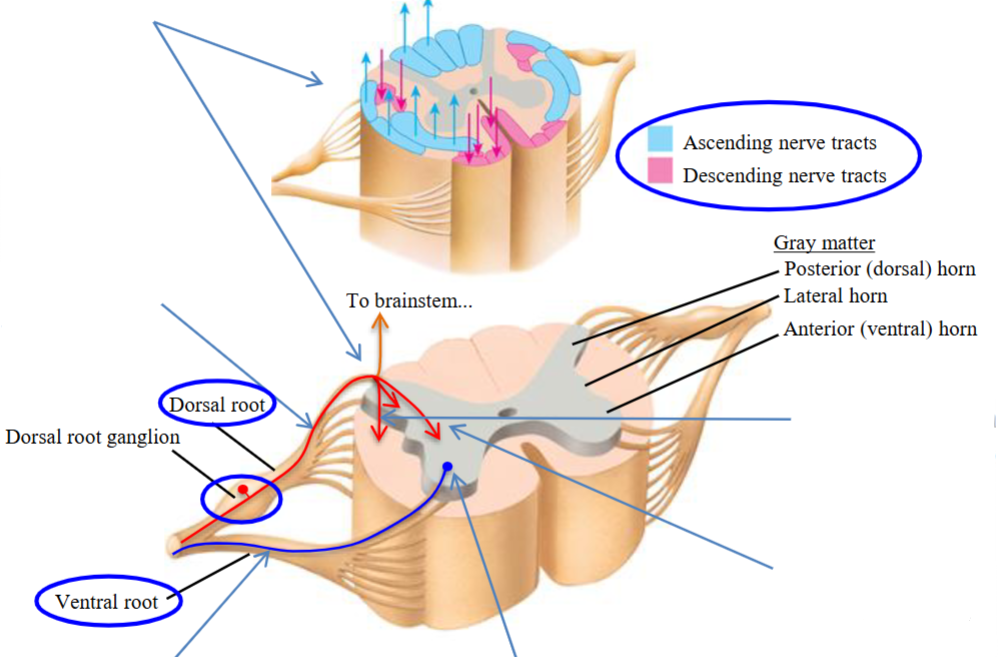
Spinal Cord
Ascending sensory axons send information from the body to the brain via the dorsal root.
Descending motor axons carry commands from the brain to the body via the ventral root.
The spinal cord also controls autonomic functions.
It contains central pattern generators (CPGs) that produce rhythmic movements like walking and breathing.
It helps coordinate reflexes without needing input from the brain (e.g. spinal reflexes).
It contributes to the timing and sequencing involved in locomotion.
Basal Ganglia/Nuclei
A paired group of 5 subcortical nuclei involved in motor, learning, reward, and emotional circuits, located deep within the cerebral hemispheres.
Receives cortical input and sends feedback via the thalamus to develop motor strategies and regulate movement.
Involved in initiating movement.
Involved in suppressing activity of muscles that would resist intended movement
Brainstem
Deals with cardiovascular, respiratory, and digestive control.
Is associated with the sleep/wake cycle and arousal.
Deals with balance, posture, and is a locomotor initiating center.
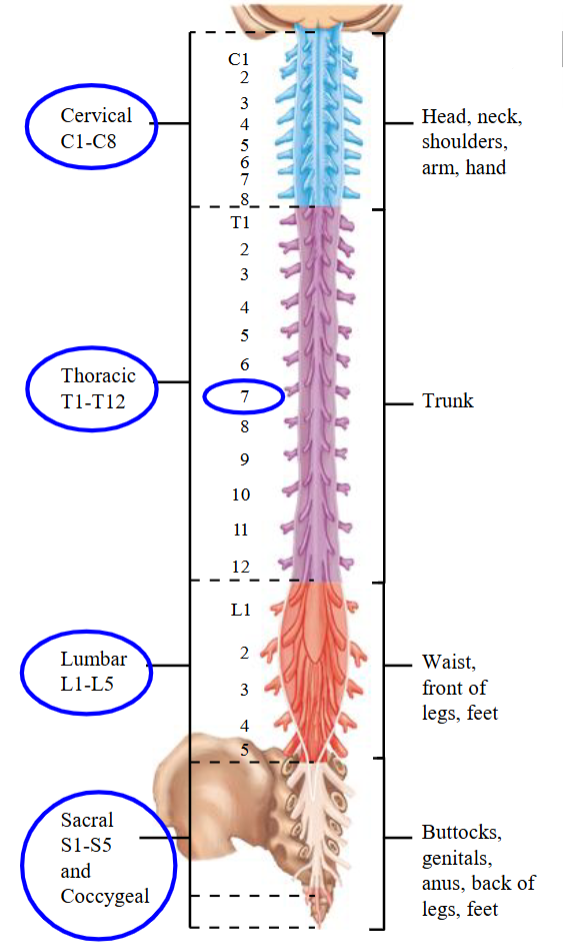
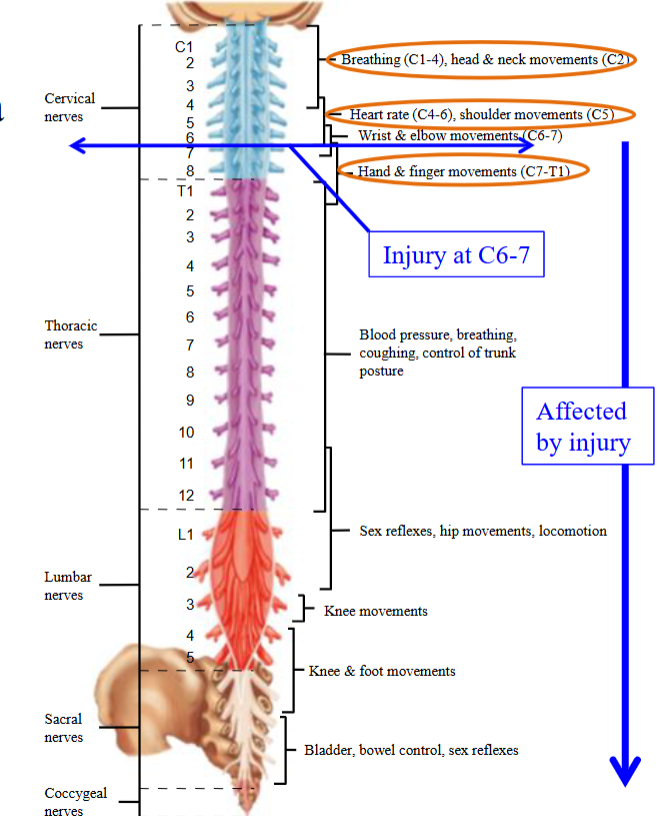
Spinal Nerves
31 spinal nerves convey signals to and from spinal cord.
Each spinal region is divided into segments and each segment leads to a bilateral pair of spinal nerves.
8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal.
Each spinal nerve innervates a specific area of skin (Dermatome) and muscles (Myotome).
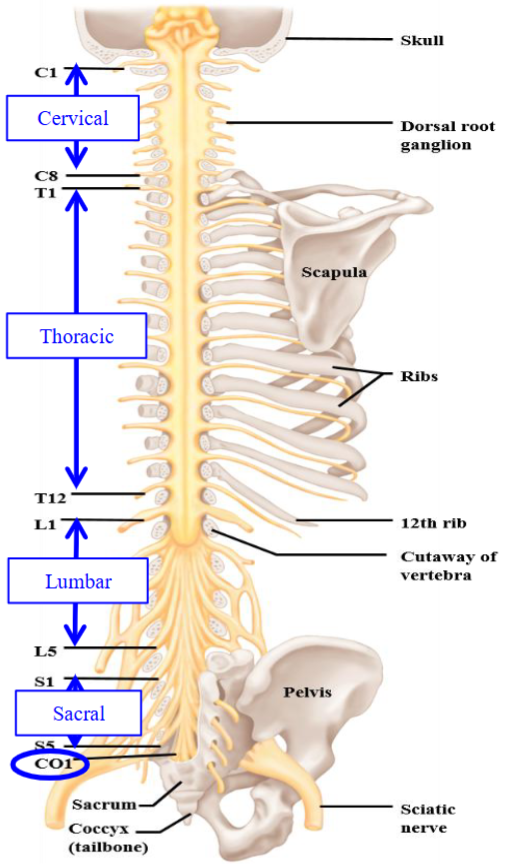
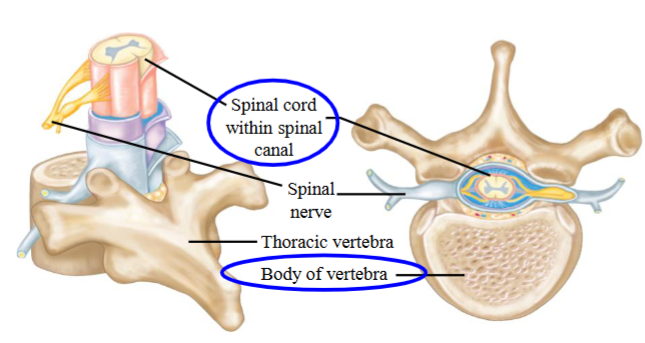
Vertebra
The body of the vertebra is the load-bearing structure of the spinal column.
Dermatomes
Skin areas whose sensation is supplied by afferent fibers from a single spinal nerve root, which connects the peripheral nerve to the spinal cord.
Knowledge of this can be used clinically to determine level of spinal cord injury.
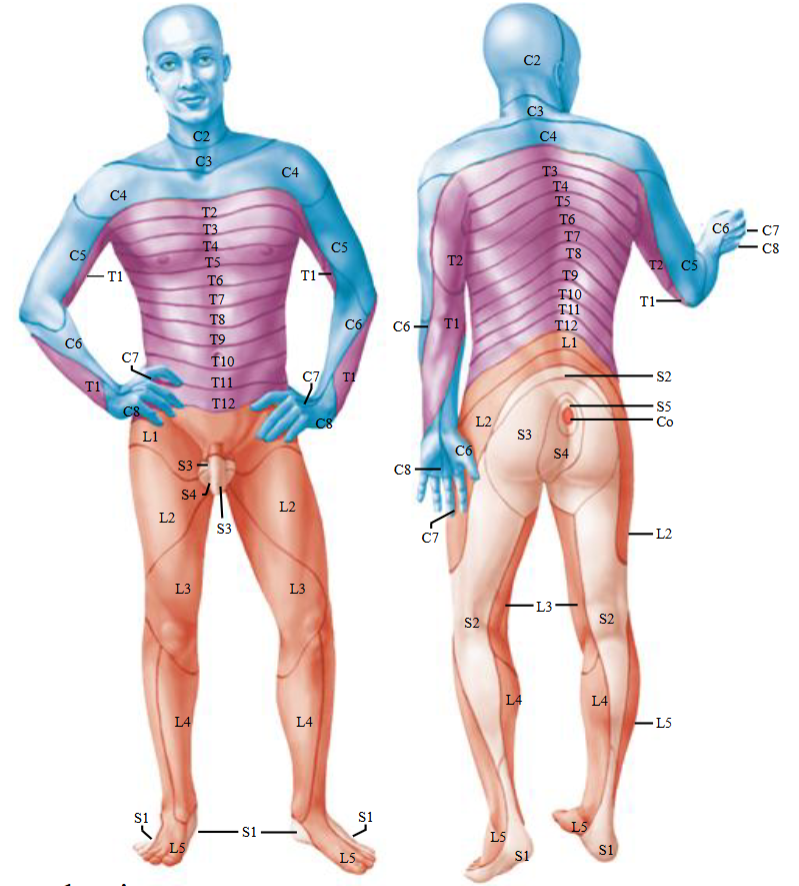
Myotomes
Defined as a group of muscles which is innervated by single spinal nerve root.
Each skeletal muscle is innervated by nerves derived from more than one spinal cord level.
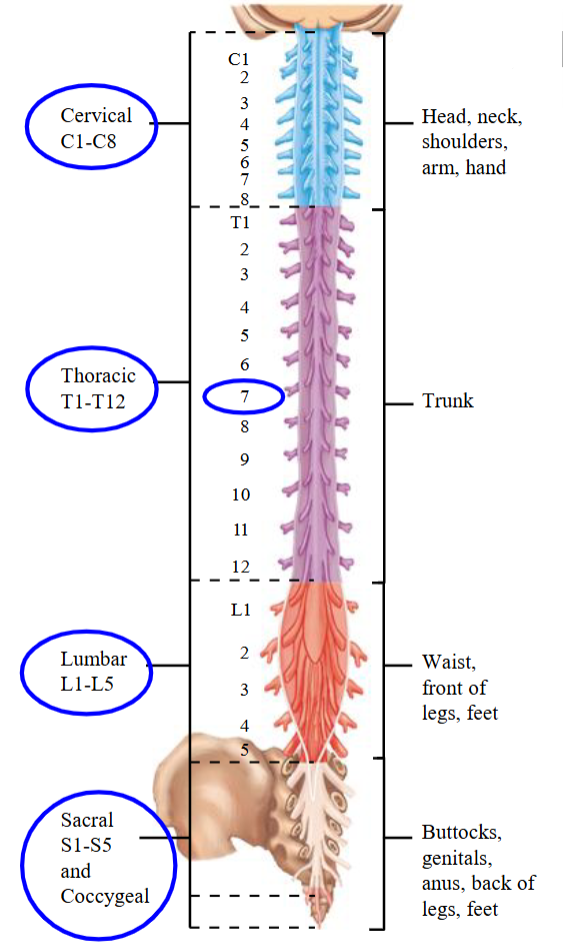
Cervical Nerves
Mediates sensory input from the head, neck, and arms.
Thoracic Nerves
Mediate sensory information from the trunk.
Lumbar + Sacral + Coccygeal Nerves
Mediate sensory information from the legs and feet.
Shingles
Neurons in the dorsal root ganglion—usually from just one or two spinal cord segments—become infected with the chickenpox virus.
In everyone who has had chickenpox, the virus lies dormant in the dorsal root ganglia.
In some cases, it can later reactivate causing bands of sores and excruciating pain along the affected dermatomes.
Spinal Cord Injury
When the spinal cord is damaged at a given level, sensation form and the motor control of functions below that level are likely to be abnormal/absent depending on severity.
i.e. if spinal cord is damaged at L2, sensation and movements of lower part of leg, bladder, bowel, and sexual functions are affected, but not breathing, trunk posture, etc.
Called paraplegia.
Dorsal Roots
The dorsal side of the cord where axons of afferent neurons enter the spinal cord.
As a spinal nerve joins the spinal cord, it divides into branches called rods.
Specialized to incoming sensory information.
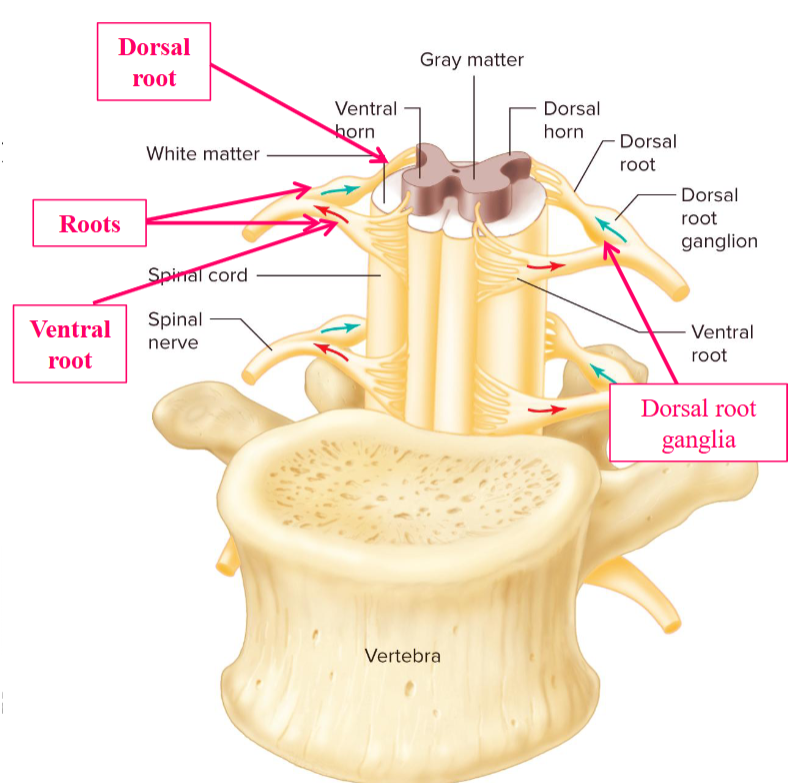
Dorsal Root Ganglia
Contains the cell bodies of the afferent neurons.
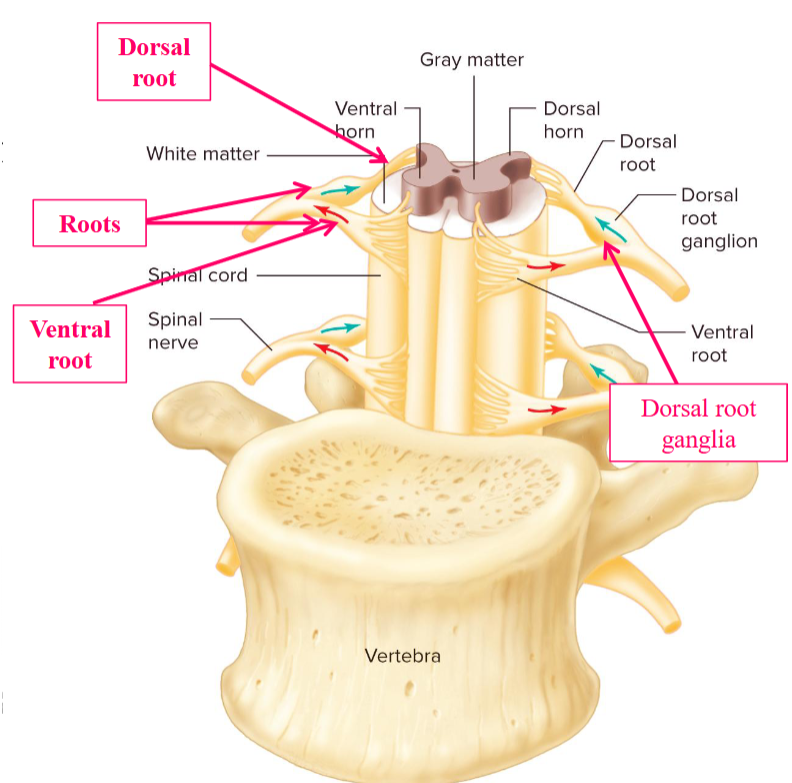
Ventral Roots
The ventral side of the cord where axons of efferent neurons leave the spinal cord.
Carries info from the CNS to muscles and glands.
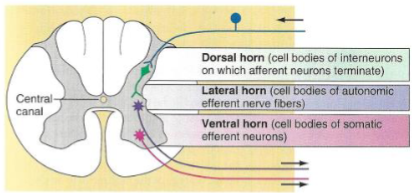
Horn
Projection of gray matter towards the outer surface of the spinal cord.
Each half of gray matter is divided into three parts:
Dorsal (posterior) horn.
Ventral (anterior) horn.
Lateral horn.
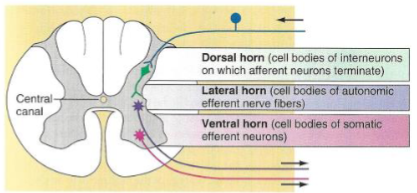
Dorsal (Posterior) Horn
Cell bodies of interneurons.
Where afferent neurons terminate.
Ventral (Anterior) Horn
Contains cell bodies of the efferent (motor) neurons supplying skeletal muscles.
Lateral Horn
Cell bodies of autonomic neurons supplying smooth muscle, cardiac muscle, exocrine glands.
Sensory Afferents - Dorsal Roots
Step 1 in the process.
Sensory afferents whose cell bodies are in the dorsal root ganglia, enter spinal cord via the dorsal roots.
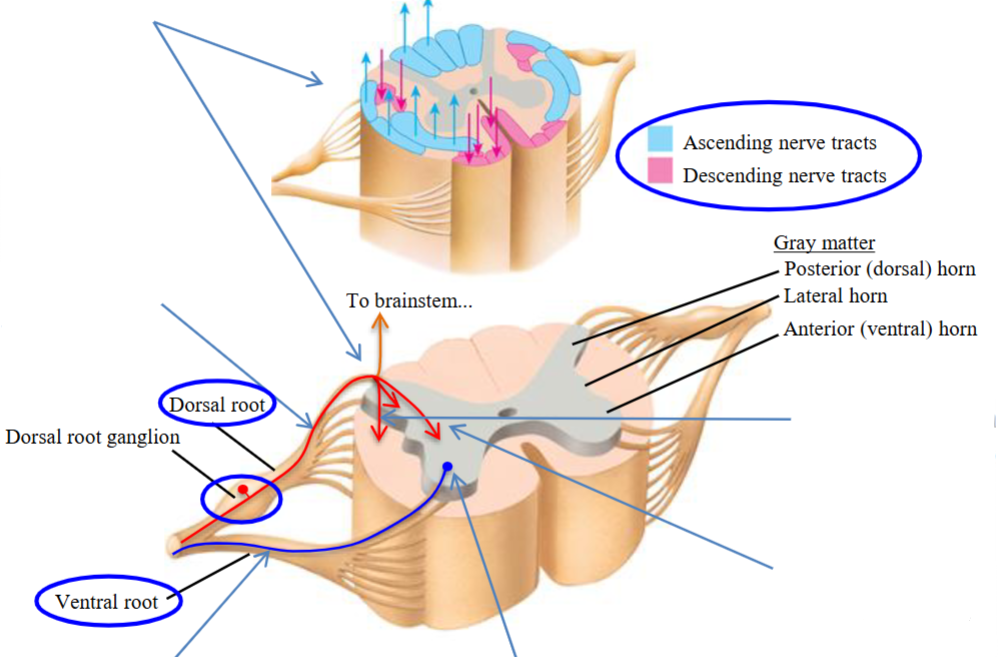
Sensory Afferents - Bifurcate
Step 2 in the process.
Sensory afferents bifurcate (split) into ascending and descending axons.
The ascending axons form the dorsal columns which ascend to the brainstem, carrying sensory information to the brain.
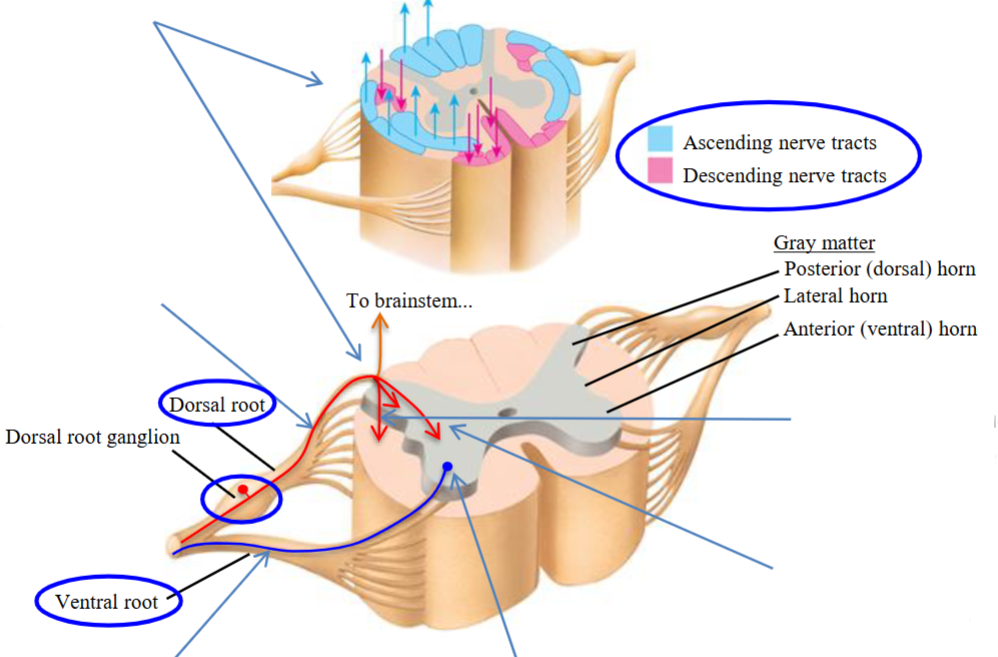
Sensory Afferents - Descending
The descending afferent axons travel caudally for 2-3 spinal segments (3-4cm).
Step 3 in the process.
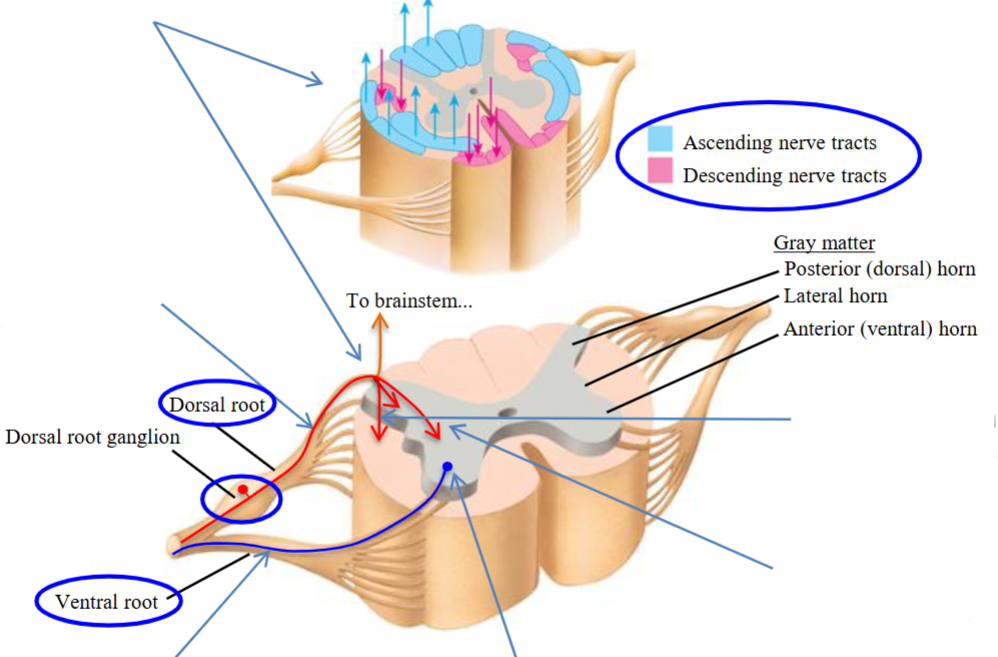
Sensory Afferents - Segments
After rostral (ascending) and caudal (descending) bifurcation, the ascending and descending axons each extend for roughly 2–3 spinal segments (≈50 mm in humans).
Every millimeter or so they send branches into the gray matter.
Those branches synapse onto interneurons and motor neurons in the gray matter.
Step 4 in the process.
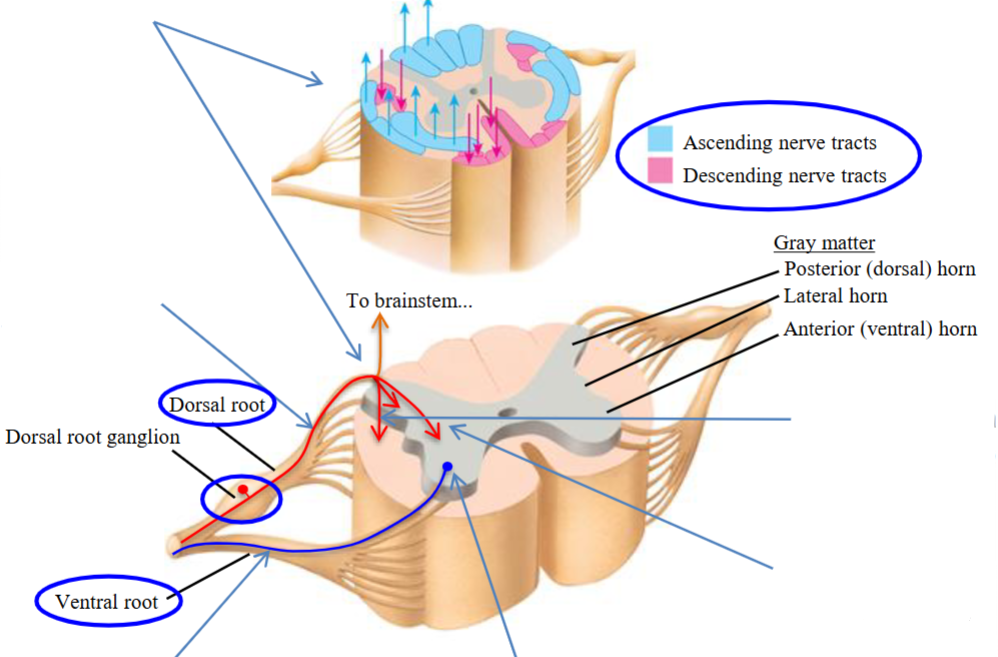
Sensory Afferents - Motoneuron
Motoneuron cell bodies are located in blue.
Motor efferent axons of the motor neurons leave the spinal cord and form the ventral roots.
They form the efferent axons that leave the spinal cord via ventral roots to innervate muscle.
Step 5 and 6.
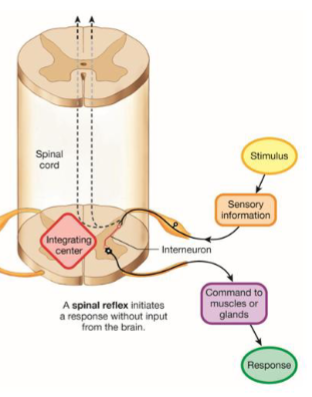
Spinal Reflex
Simple behaviour produced by the central nervous system (CNS) pathways that lie entirely within the spinal cord.
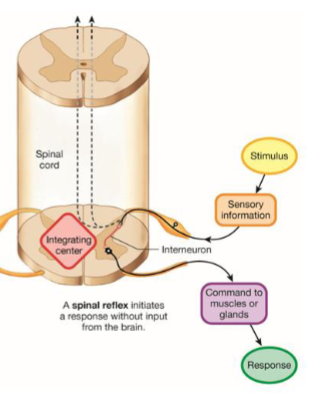
Spinal Reflex - Ascending
Afferent (sensory) fibers that evoke these reflexes enter the spinal cord and activate spinal motoneurons directly or through a chain or one or more spinal interneurons.
In addition, spinal interneurons may route sensory information to the brain through ascending tracts.
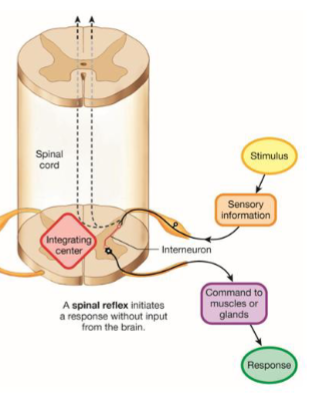
Spinal Reflexes - Descending
These pathways may be affected by descending pathways from the brain, either directly or indirectly through other spinal interneurons.
Brain exerts both short-term and long-term influence over spinal cord reflex function.
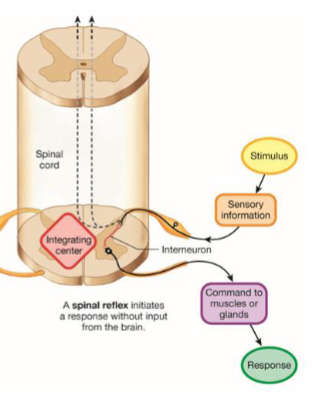
Brain Modulates Reflexes
In the short-term, the brain rapidly adjusts spinal reflexes to suit the needs of different tasks (i.e. standing vs. walking vs. running).
In the long-term, it gradually shapes spiral reflexes during development, during skill acquisition, and response to CNS trauma and disease.
Sensory Areas
The cerebral cortex can be divided into three areas.
Sensory input translated into perception (awareness).
All control functions linked with sensory functions.
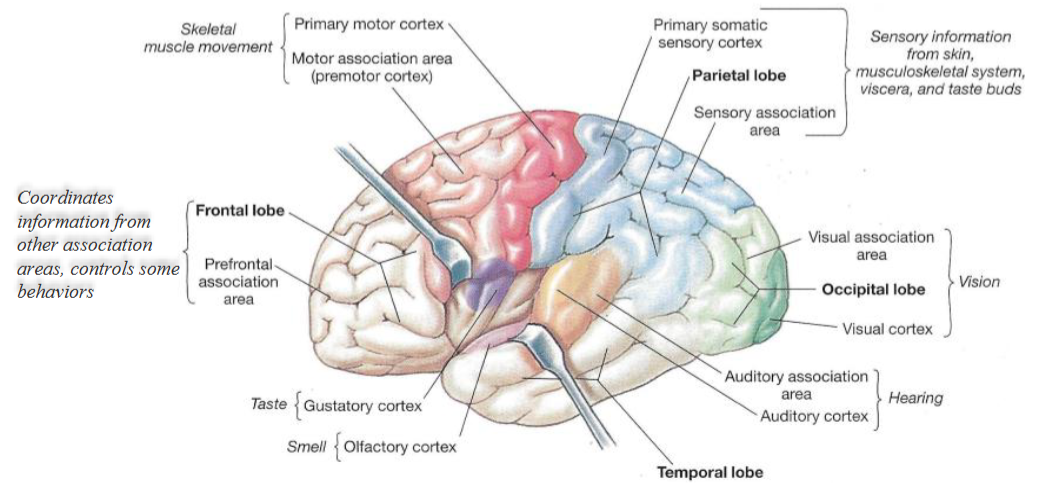
Motor Areas
Plan, control and execute voluntary movements.
Responsible for planning, controlling, and executing voluntary movements.