Muscle Physiology
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
The three muscles types
Striated Cardiac Muscle
Striated Skeletal Muscle
Smooth Muscle
Skeletal Muscle Disorders: Myopathies
INHERITED MYOPATHIES
Congenital myopathies
Muscular dystrophies (e.g. Duchenne)
Metabolic myopathies (e.g. glycogen storage diseases such as McArdle and Pompe diseases)
Mitochondrial myopathies
Channelopathies
ACQUIRED MYOPATHIES
Autoimmune/inflammatory myopathies (e.g. Dermatomyositis)
Toxic myopathies (e.g. caused by statins)
Endocrine myopathies
Infectious myopathies
Critical illness myopathy (complication in critical care)
Neuromuscular junction disorder
Primary cause: Communication between the nerve and muscle is disrupted
Secondary: Affects muscle
Examples:
Congenital myasthenic syndromes (genetic disorder)
Myasthenia gravis (autoimmune disorder)
Botulism toxin
Neurogenic atrophy
Primary cause: Nerve disorder or damage
Secondary: Affects muscle
Examples:
Nerve and spinal cord injuries
Motor neuron diseases (brain and spinal cord motor nerves die prematurely)
Sensory and autonomic neuropathies (affect sensory involuntary functions)
Nerve tumours
Sacropenia
Loss of skeletal muscle mass (atrophy) with aging
Muscle mass peaks between 25 and 30 years
Usually, 0.5 to 1% per year after the age of 50 years
By the age of 65 years muscle mass is reduced by approximately 25 to 30%
Extent of atrophy is muscle specific and is influence by several factors such as muscle activity
Results in a decrease of muscle strength and power
Skeletal muscle
660 muscles in adult human
Constitutes to 45% of our body weight
Functions of skeletal muscle
Converts chemical energy into force and mechanical work (movement and locomotion)
Maintains posture and body position.
Support soft tissues (abdominal wall, floor of the pelvic cavity)
Encircle openings of the digestive and urinary tracts
Heat production.
Reservoir for protein storage
MTU (Musculotendinous Unit)
The (musculotendinous unit) draws one articulating bone toward the other
Origin – the attachment to the stationary bone (or the bone that moves the least)
Insertion – the attachment to the moveable bone (or the bone that moves the most)
Types of levers
Class 1: Effort - Fulcrum - Load (seesaw)
Class 2: Effort - Load - Fulcrum (wheelbarrow)
Class 3: Fulcrum - Effort - Load (tweezzer)
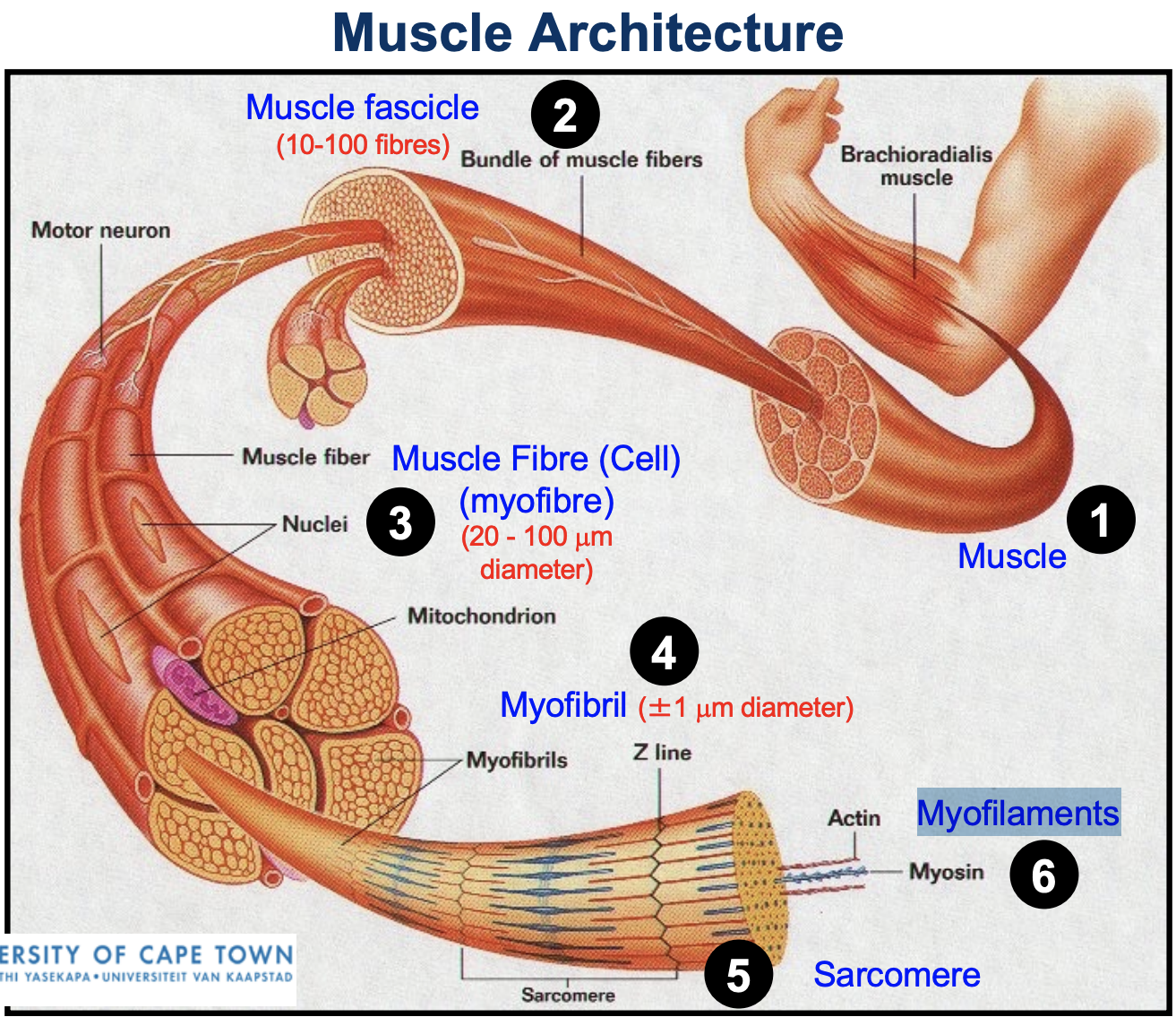
Muscle architecture
Muscle
Muscle fascicle
Muscle fibre/cell / myofibre
Myofibril
Sarcomere
Myofilaments
Three layers of connective tissue around skeletal muscle
Epimysium = a sheath of dense irregular connective tissue, covers each muscle.
This allows the muscle to contract and move while maintaining structural integrity
Separates individual muscles from each other and other structures.
Allows for independent movement
Perimysium = covers fascicles (10 to 100 muscle fibres per fascicle)
Endomysium = covers each muscle fibre (cell) forming the basement membrane.
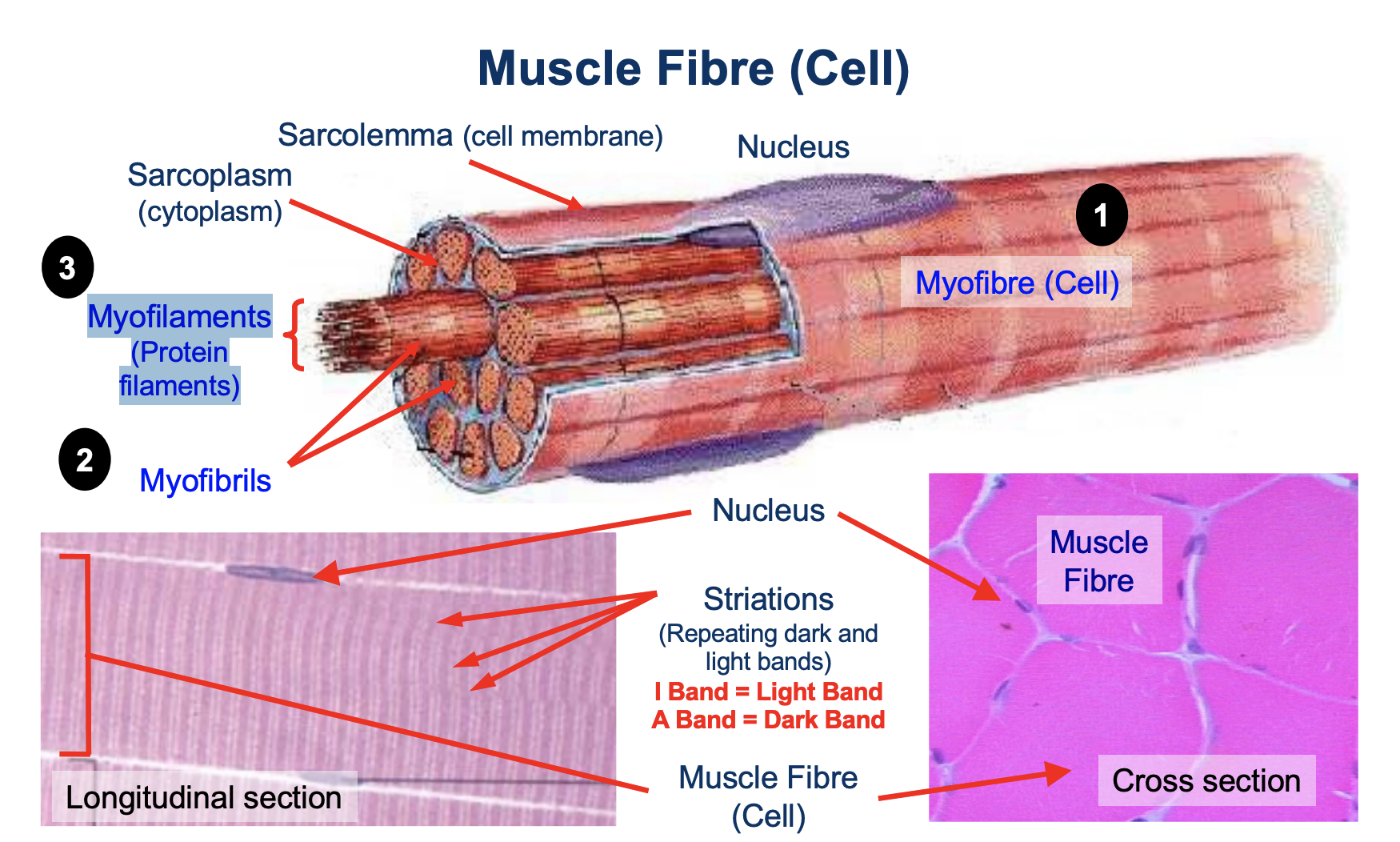
Skeletal Muscle Fibre (Cell)
Skeletal muscle fibres are highly differentiated elongated multinucleated (200-300 nuclei/mm).
Post-mitotic - therefore muscle fibres are unable to divide to repair muscle tissue
Fast twitch fibre diameter > slow twitch.
Skeletal Muscle Fibre Types
SLOW TWITCH:
Type 1: Slow Oxidative (SO) - red fibre
FAST TWITCH:
2A: Fast Oxidative Glycolytic (FOG) - red fibre
2X: Fast Glycolytic (FG) - white fibre
2B
*in red fibres there is high myoglobin and mitochondria content
Muscle architecture
Myofibre (Cell)
Myofibrils
Myofilaments (Protein filaments)
Myofibrils
Each muscle fibre (cell) is densely packed with myofibrils
Myofibrils run in parallel rows from one end of the muscle fiber to the other
Other organelles are restricted to the narrow cytoplasmic spaces that remain between adjacent myofibrils
Each myofibril contains myosin (thick) and actin (thin) filament AKA myofilaments
Thick and thin filaments overlap causing striated appearance (banding pattern)
Repeating I (light) and A (dark) bands along the myofibril
The functional unit of muscle contraction (sarcomere) is located between two Z discs
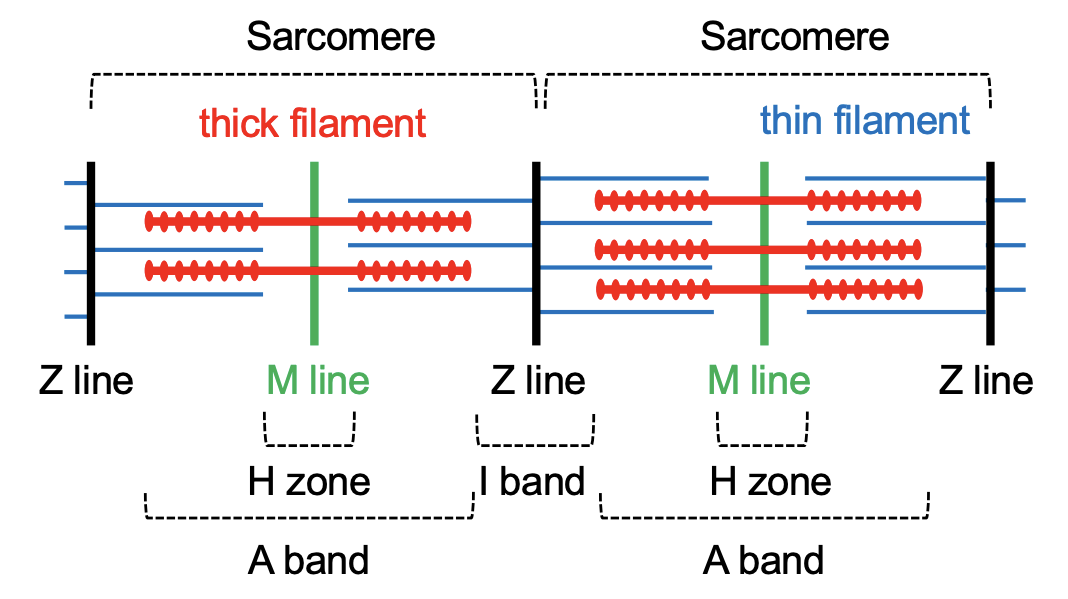
Sarcomere
Repeating functional unit within the myofibril of skeletal muscle cells
Divided into the I band (2 halves), A band, H-zone, M line (located in the middle of the sarcomere where it bisects the A band and H zone) and Z line (bisects the I band and is the structure between adjacent sarcomeres)
Made from two fibres: thin and thick which are called actin and myosin
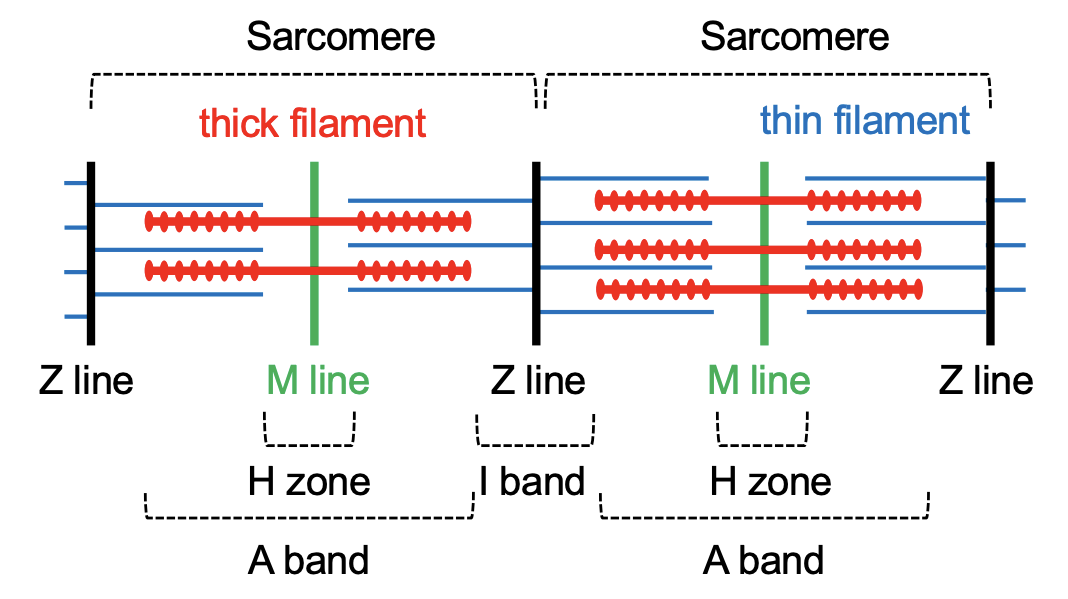
I (Light) Band
Consists of only thin (actin) filaments
Shortens during contraction due to the increasing overlap of actin and myosin filaments
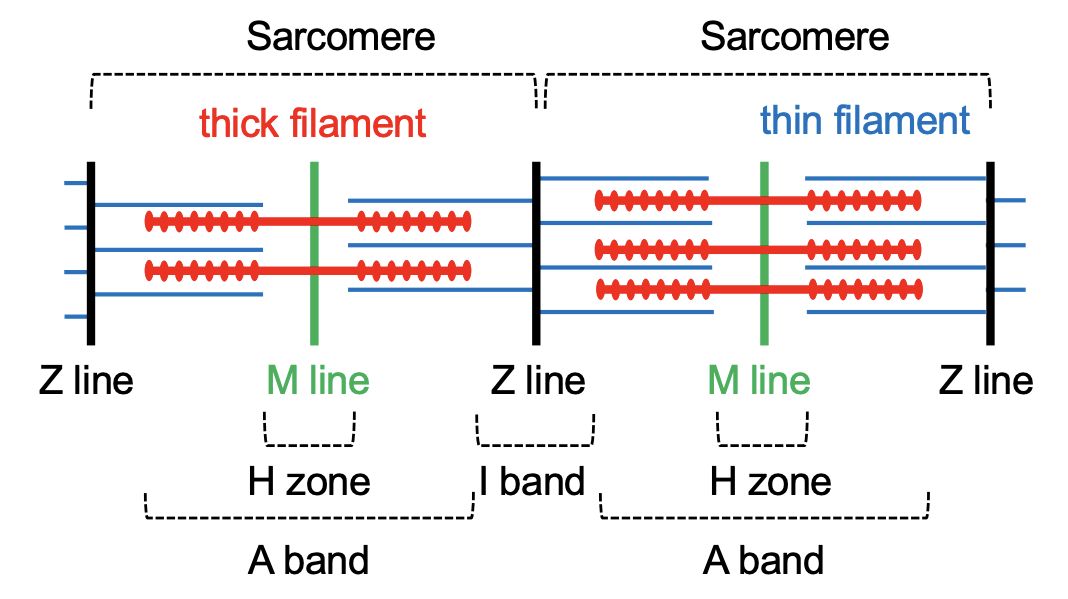
A (Dark) Band
Contains both thin (actin) and thick (myosin) filaments
The myosin and actin filaments overlap in peripheral regions of the A band
the middle region (called the H zone) contains only myosin filaments
Remains the same size during muscle contraction
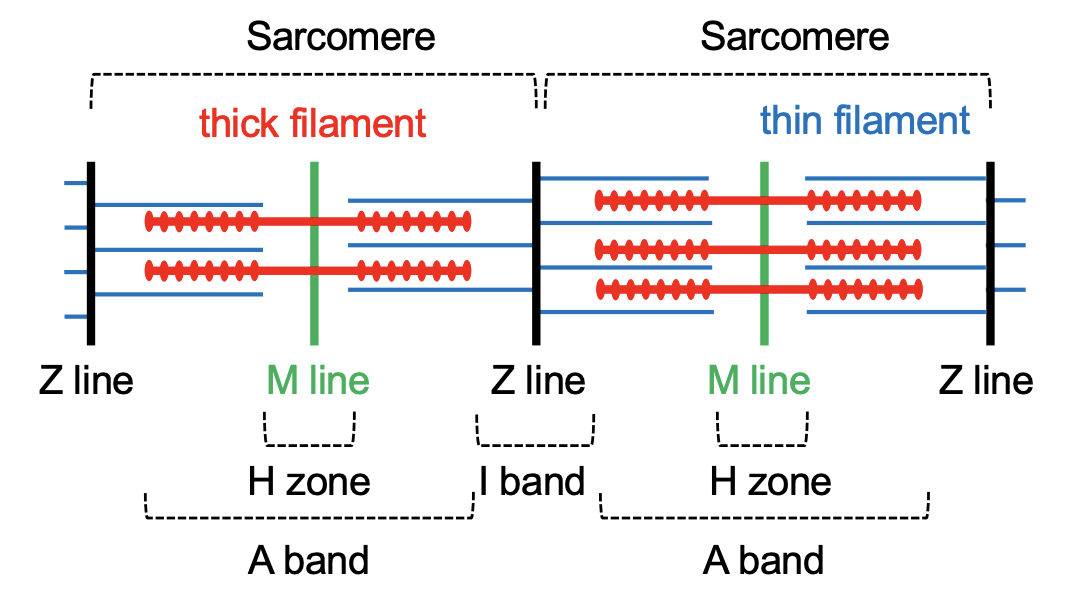
H Zone
The central region of the A band
Contains only thick (myosin) filaments
Shortens during contraction due to the increasing overlap of actin and myosin filaments
No longer visible when the muscle is fully contracted
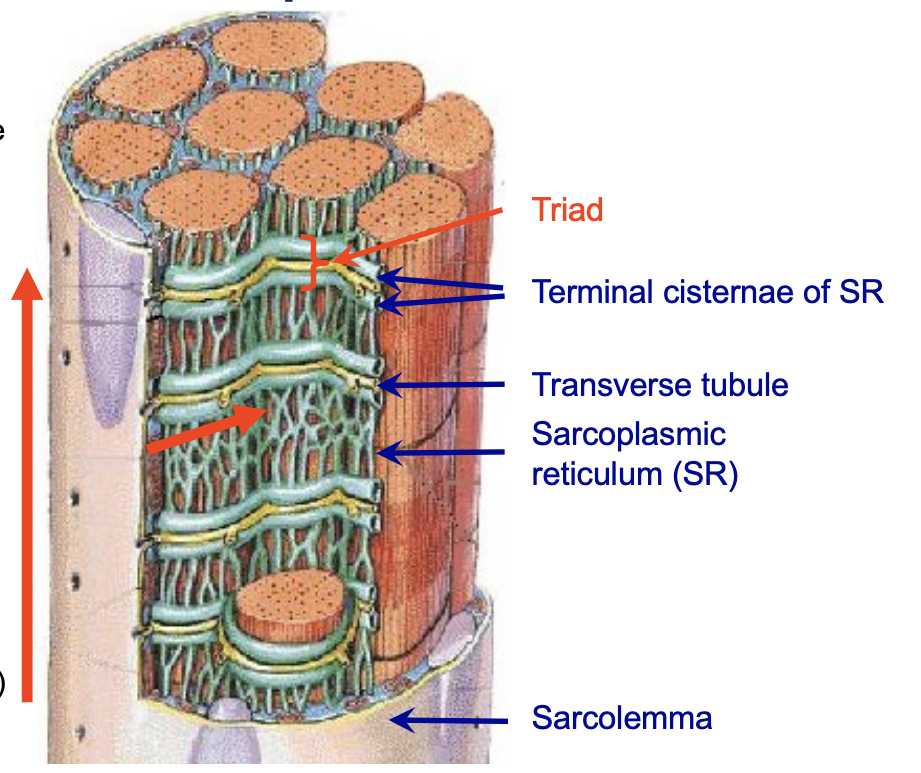
Sarcoplasmic Reticulum (SR)
The sarcoplasmic reticulum (SR) is a modified smooth ER
Consist of interconnected sacs and tubes that surround each myofibril
At the end of each SR there is an expanded portion known as terminal cisternae
Two terminal cisternae for each SR
Stores Ca2+ - used for muscle contraction
Most of the Ca2+ is stored in the terminal cisternae in the relaxed muscle
[Ca2+] is higher in SR compared to cytoplasm
SR membrane contains Ca2+ calcium release channels called ryanodine receptors (RyRs)
![<ul><li><p>The sarcoplasmic reticulum (SR) is a modified smooth ER</p></li><li><p>Consist of interconnected sacs and tubes that surround each myofibril</p></li><li><p>At the end of each SR there is an expanded portion known as terminal cisternae</p></li><li><p>Two terminal cisternae for each SR</p></li><li><p>Stores Ca2+ - used for muscle contraction</p></li><li><p>Most of the Ca2+ is stored in the terminal cisternae in the relaxed muscle</p></li><li><p>[Ca2+] is higher in SR compared to cytoplasm</p></li><li><p>SR membrane contains Ca2+ calcium release channels called ryanodine receptors (RyRs)</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/43f4fb5d-5e13-4fa7-9222-ed87ce116f40.png)
Transverse Tubules (T-Tubules)
Terminal cisternae of adjacent SRs are separated by only a very narrow gap
Gap contains the transverse tubules (T-tubules)
T-tubules are extensions of the sarcolemma that enter the cell
Contain extra-cellular fluid
The internal membranes of the Ttubules are extensions of the sarcolemma
They contain voltage-gated Ca2+ channels - dihydropyridine (DHP) receptor
T-tubule allow action potentials to moves into the interior of the muscle cell
The structure where a T-tubule and two terminal cisternae meet are called a triad
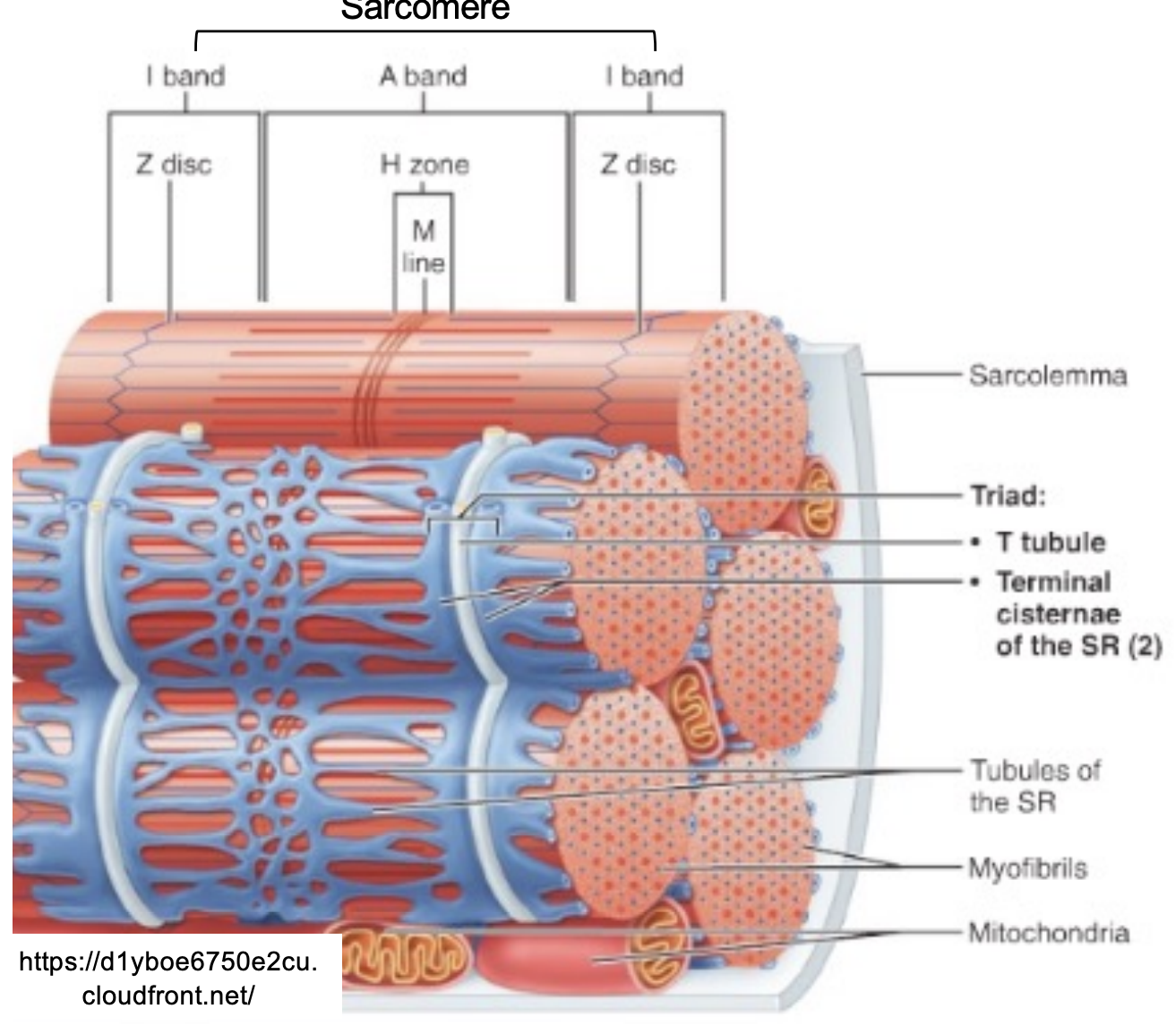
Mitochondria
Mitochondria are found just beneath the plasma membrane and between the myofibrils
Oxidative enzymes are found in the mitochondria
More mitochondria in slow twitch muscle
Endurance training may double the mitochondrial content
Sliding Filament Theory
Thin filaments slide over the thick filaments resulting in shortening of the the sarcomere and muscle
ATP hydrolysis and Ca2+ required
Myosin heads bend back and forth step by step (cross bridge cycle)
Z discs move towards each other
The myofilaments do not change length, merely slide over one another
Width of A band remains constant
Width of the I band and H zone changes
Shortening of all sarcomeres results is muscle shortening
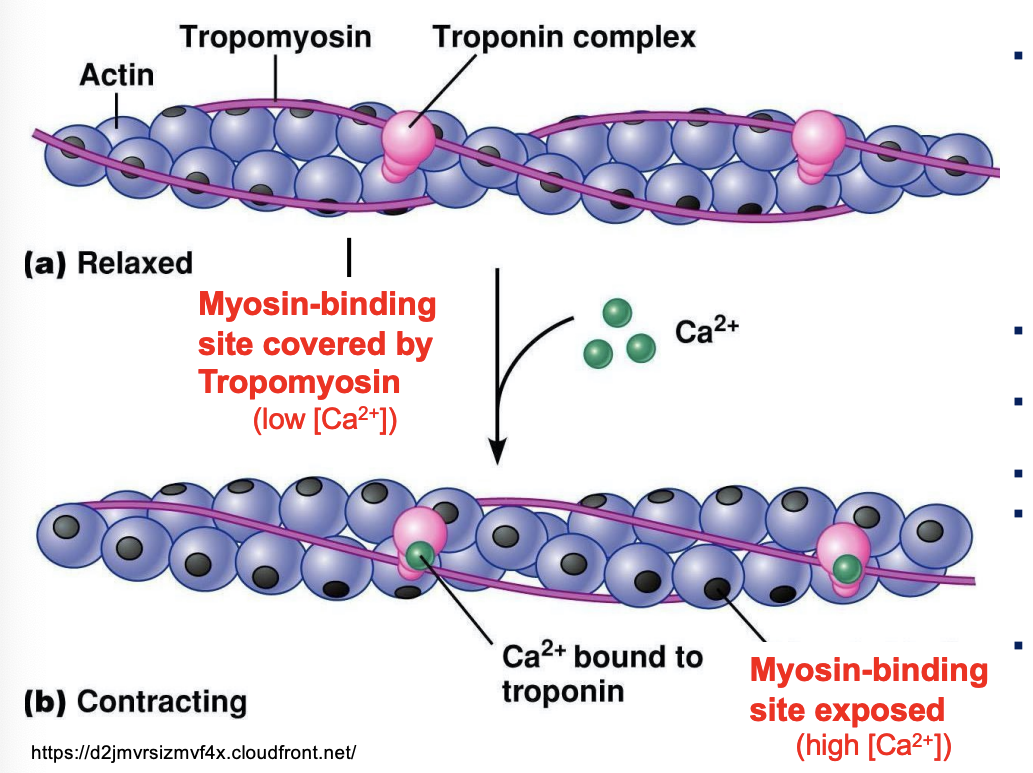
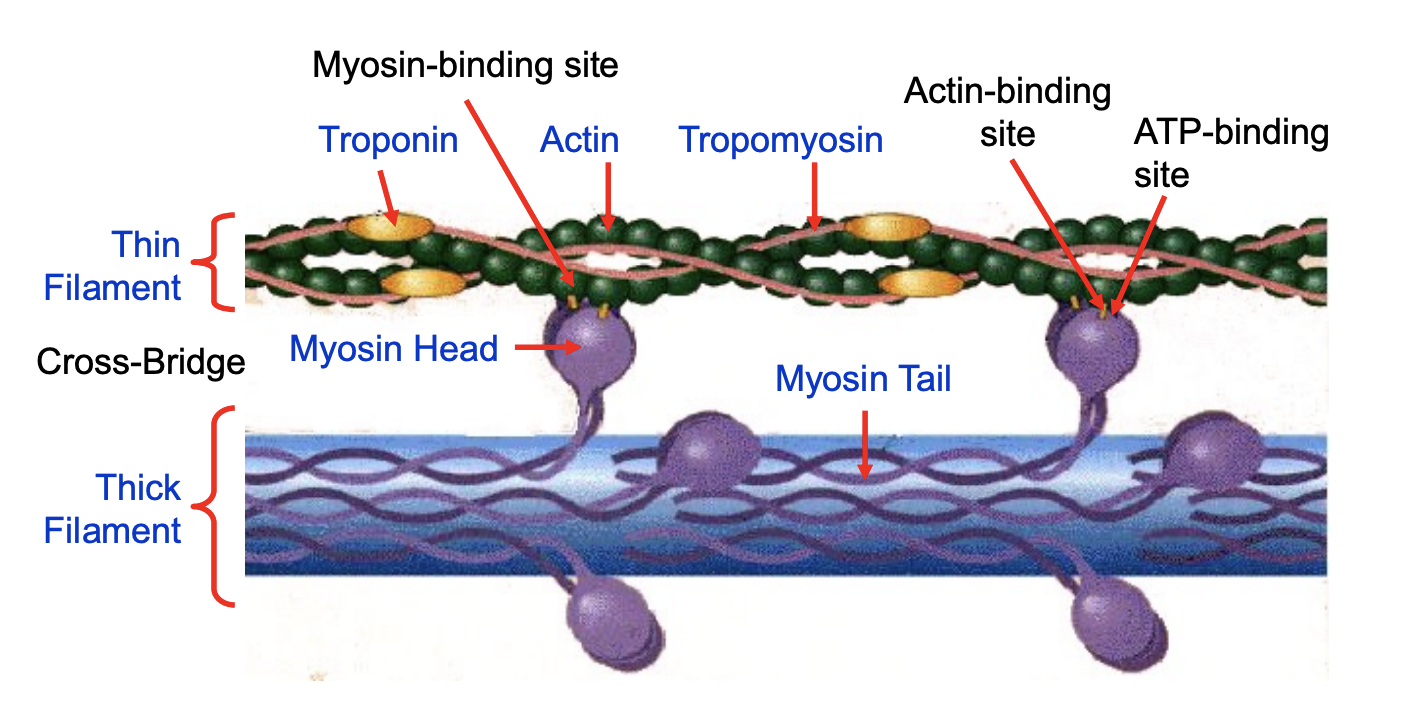
Thin Filament (Actin) Structure
Actin filaments consist of three proteins:
One structural:
Actin
Two regulatory:
Tropomyosin
Troponin
Actin monomers form a double stranded filament
Actin has a myosin-binding site
Troponin is able to bind Ca2+
In relaxed muscle, the tropomyosin physically covers the myosin-binding site of the of actin filament
Troponin and tropomyosin work together to regulate the binding to actin to myosin
Myosin binding site
a specific region on the actin protein where the myosin head can attach, forming a cross-bridge
it allows myosin to pull on the actin filaments, causing them to slide past each other
Thick (Myosin) Filament Structure
Major component of thick filaments within the sarcomere
Large protein with a molecular weight of 500 kDa
Thin rod-like molecule (200 nm long; 2-3 nm Diameter)
Different isoforms: MHC1, MHC2A, MHC2X
Myosin is a hexamer consisting of
2 identical myosin heavy chains (MHC) of about 220 kDa each
2 pairs of (i.e. 4) non-identical myosin light chains (MLC)
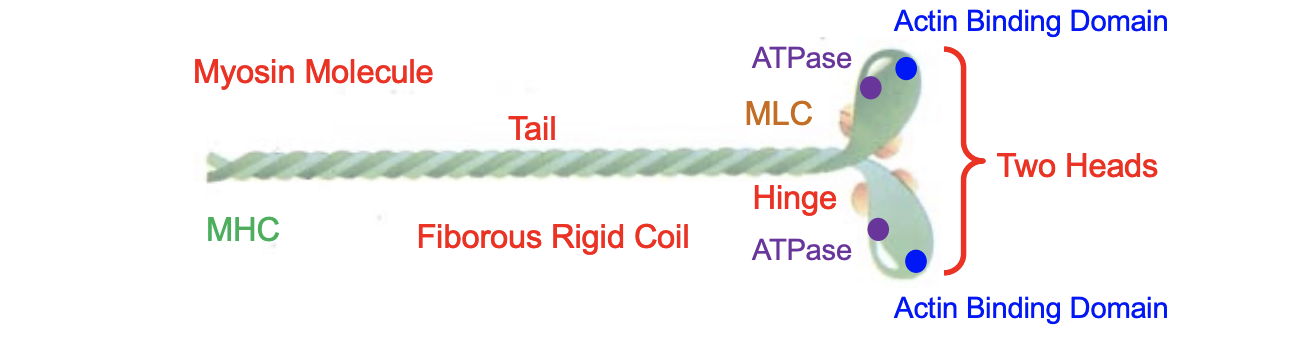
Assembled Thick Filament
approx. 300 molecules of myosin in one thick filament
The thin rod-like tails overlap to form the thick filament with the heads protruding out of the filament
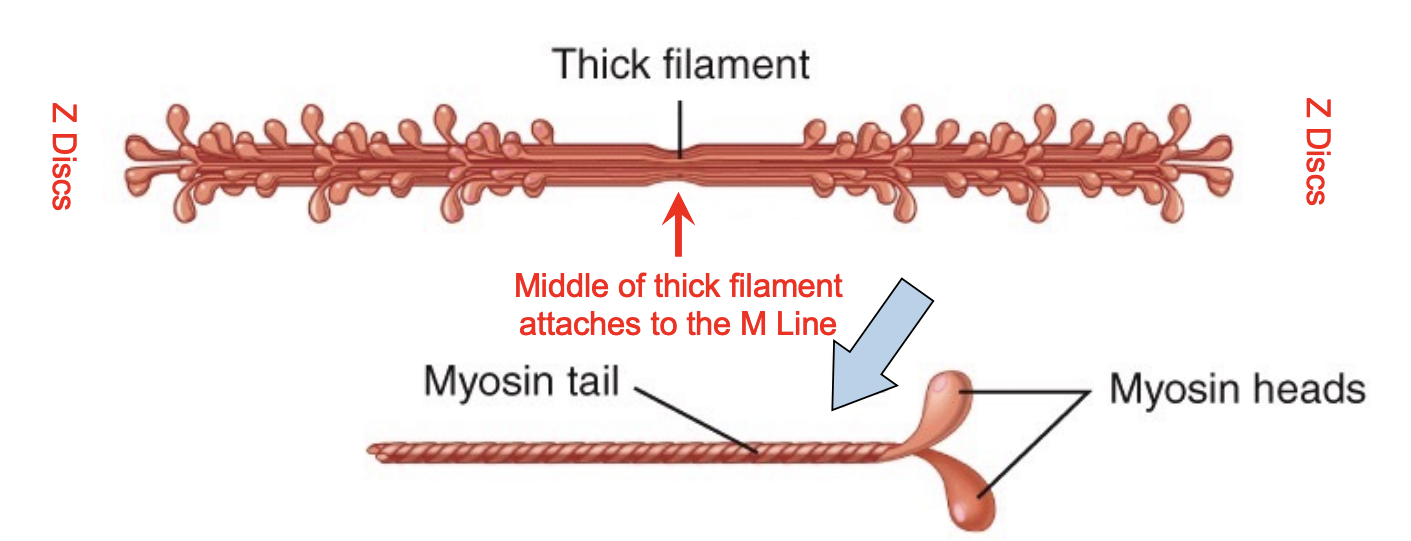
Cross-Bridge between the Thick and Thin Filaments
the myosin head of the thick filament binds to the actin (thin filament) during muscle contraction, forming a connection that allows the filaments to slide past each other, resulting in muscle shortening
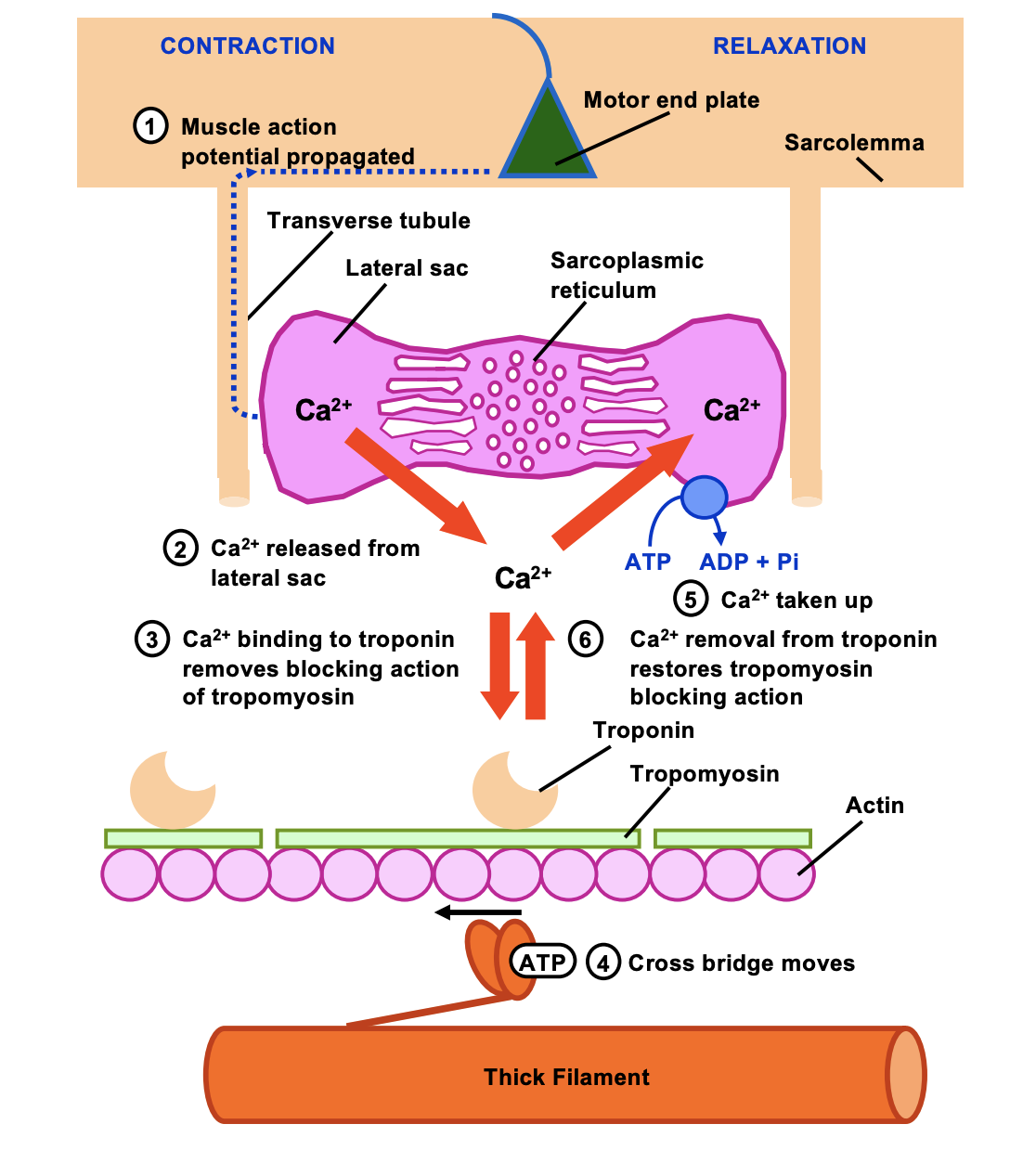
T-Tubule and Sarcoplasmic Reticulum (muscle fibre depolarization)
Muscle fibre depolarization starts at the motor end plate
Action potential (AP) transmitted along the sarcolemma
AP descends into the fibre via the T-tubules
Depolarization of the Ttubule membrane
Ca2+ channels open in the SR cisternae
Rapid release of Ca2+ from sarcoplasmic reticulum (SR)
WHY:
because it triggers the release of calcium ions, which are the key initiators of the contraction process
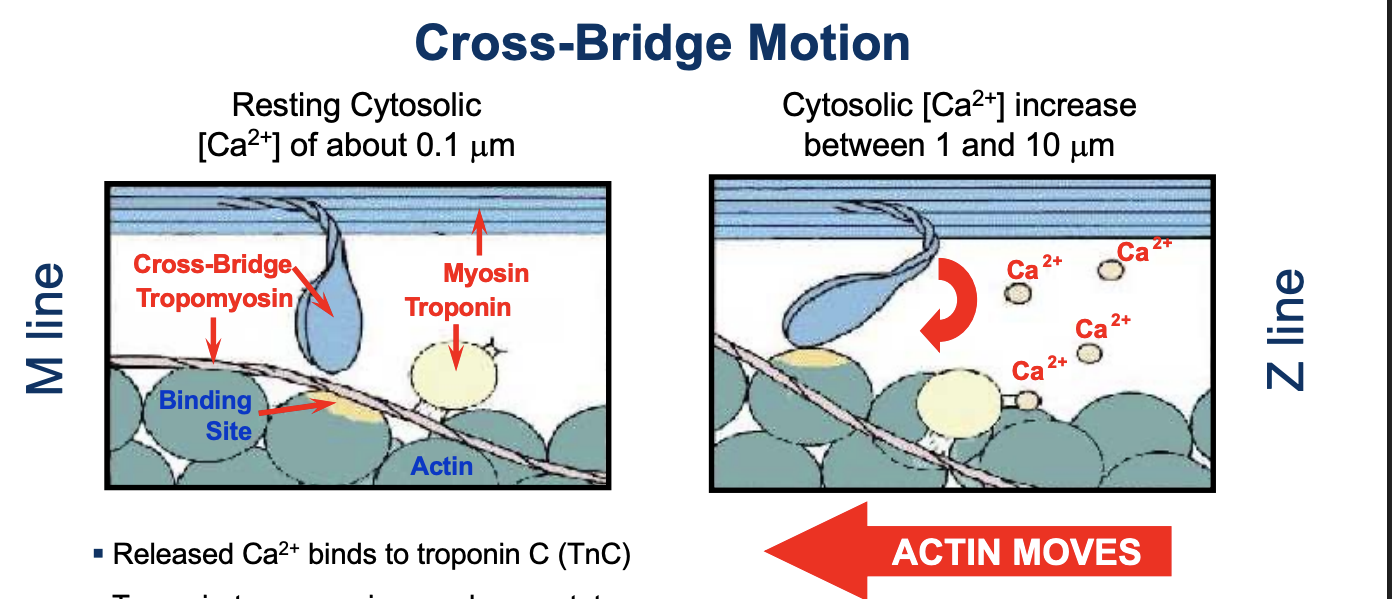
Cross-Bridge Motion
Released Ca2+ binds to troponin C (TnC)
Troponin-tropomyosin complexes rotate
Uncovering of myosin-binding sites on actin
Myosin head binds actin to form a cross-bridge
Myosin head moves 45 degrees
Pulling the actin filament towards the M line (±12 nm)
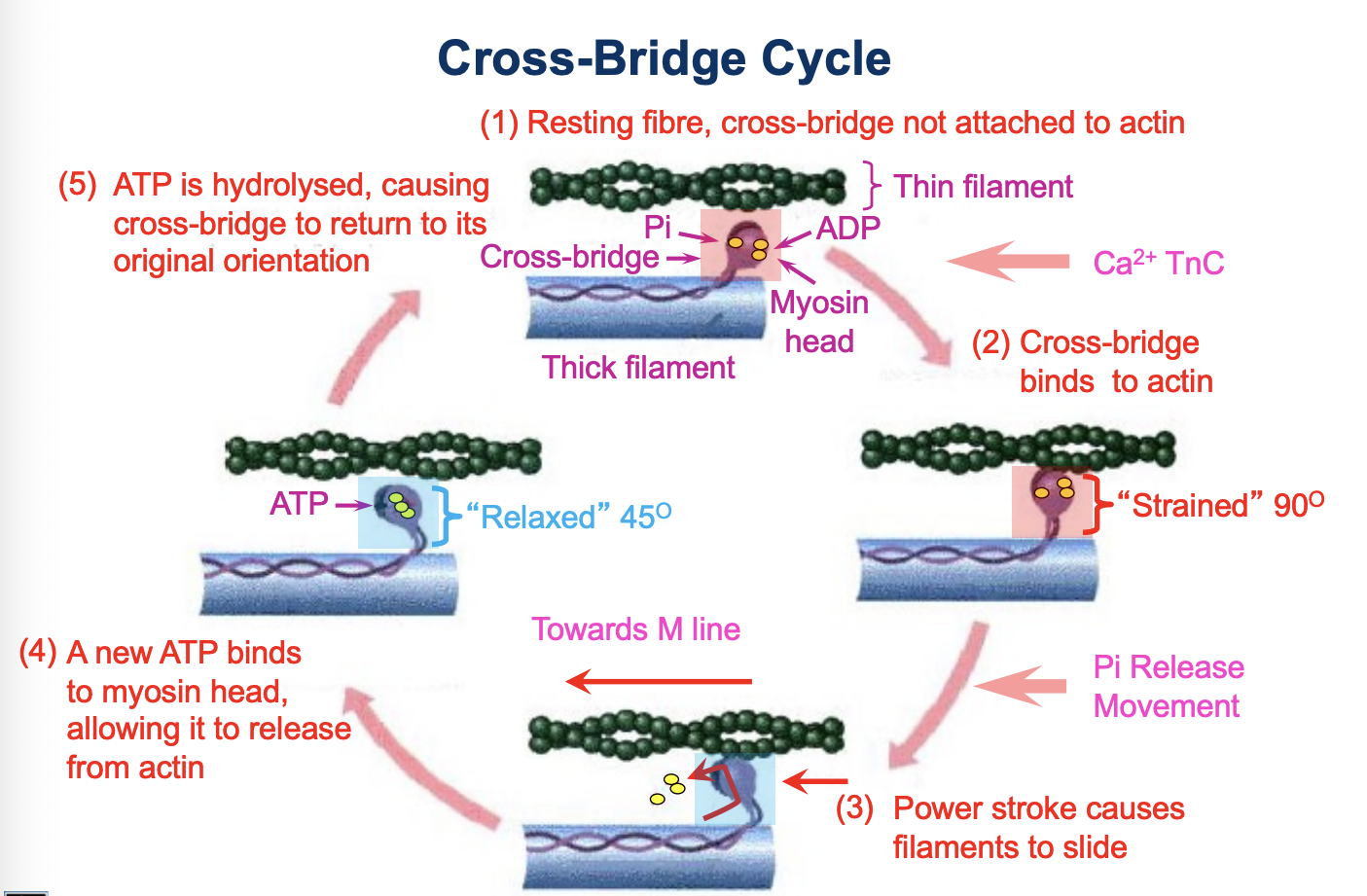
Cross-Bridge Cycle
Resting fibre, cross-bridge not attached to actin
Cross-bridge binds to actin (Pi is released)
Power stroke causes filaments to slide
A new ATP binds to the myosin head allowing it to release from actin
ATP is hydrolysed, causing cross-bridge to return to its original orientation
Sarcomere Length-Tension Relationship
cross-bridge formation responsible for force generation
there is a direct relationship between the force developed by a muscle and the number of overlapping cross-bridges
Sequence of events in skeletal muscle relaxation
Ca2+ pumped back into sarcoplasmic reticulum
Active (ATP) dependent process
Release of Ca2+ from troponin
Cessation of interaction between actin and myosin
IF Inhibit active transport of Ca2+:
Relaxation does not occur
Even if there are no more action potentials
ATP provides energy for both?
Contraction (cross-bridge cycle)
Relaxation (active transport of calcium into SR)
Effects of Muscle Architecture on Force Production and Shortening Velocity
An increase in the number of sarcomeres in series within a myofibril causes an increase in the overall velocity of shortening of the fibre
The sarcomeres arranged in parallel to each other, the greater the capacity for maximum force production (less shortening velocity)
Skeletal Muscle Motor Unit Innervation
The minimum functional unit of neural control of muscle
contraction is called the motor unit
A motor unit consists of:-
1. a cell body
2. the outgrowing (alpha) α-motor neuron (axon,
efferent nerve, “movement” nerve)
3. Muscle fibres it innervates
The number of muscle cells in a single motor unit ranges
(known as the innervation ratio)
When an action potential is propagated in a single axon all the fibres in the motor unit are stimulated to contract
Motor units in skeletal muscle
each individual motor unit consists of the sample fibre types
groups of motor units work together to coordinate the contractions of a single muscle
force of muscle contraction is controlled by the number of activated motor units
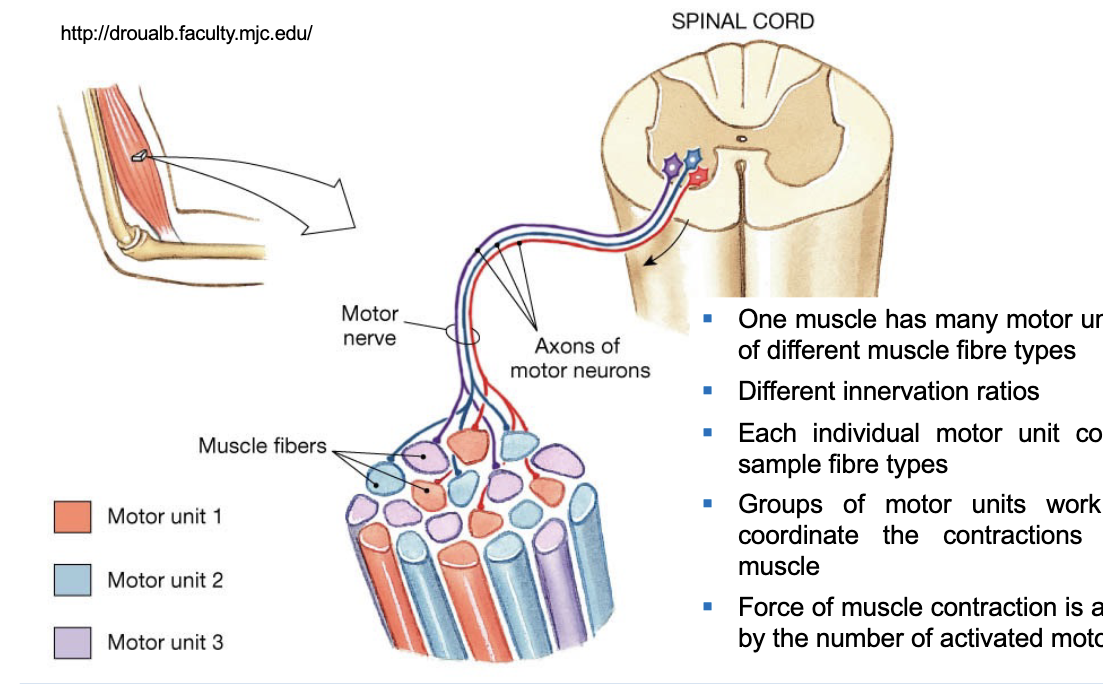
Motor units recruitment and force production
increase contraction force by increasing the number of motor units
smaller units recruited first
larger units are then added
individual motor units are responsible for each contraction and occur between the contraction and relaxation
Resting Membrane Potential and Action Potential
Resting membrane potential: At rest, nerve and muscle cells have an electrical potential difference across their membranes (negatively charge inside and positively charged outside the cell).
Action potential (AP): A wave of depolarization that moves along the surface of the nerve or muscle cell membrane
AP is due to the sudden change in the resting membrane potential (inside of the cell becomes positively charged)
Caused by a sudden transient increase in permeability of the membrane to Na+ influx of Na+ into the cell from the ECF (extracellular fluid)
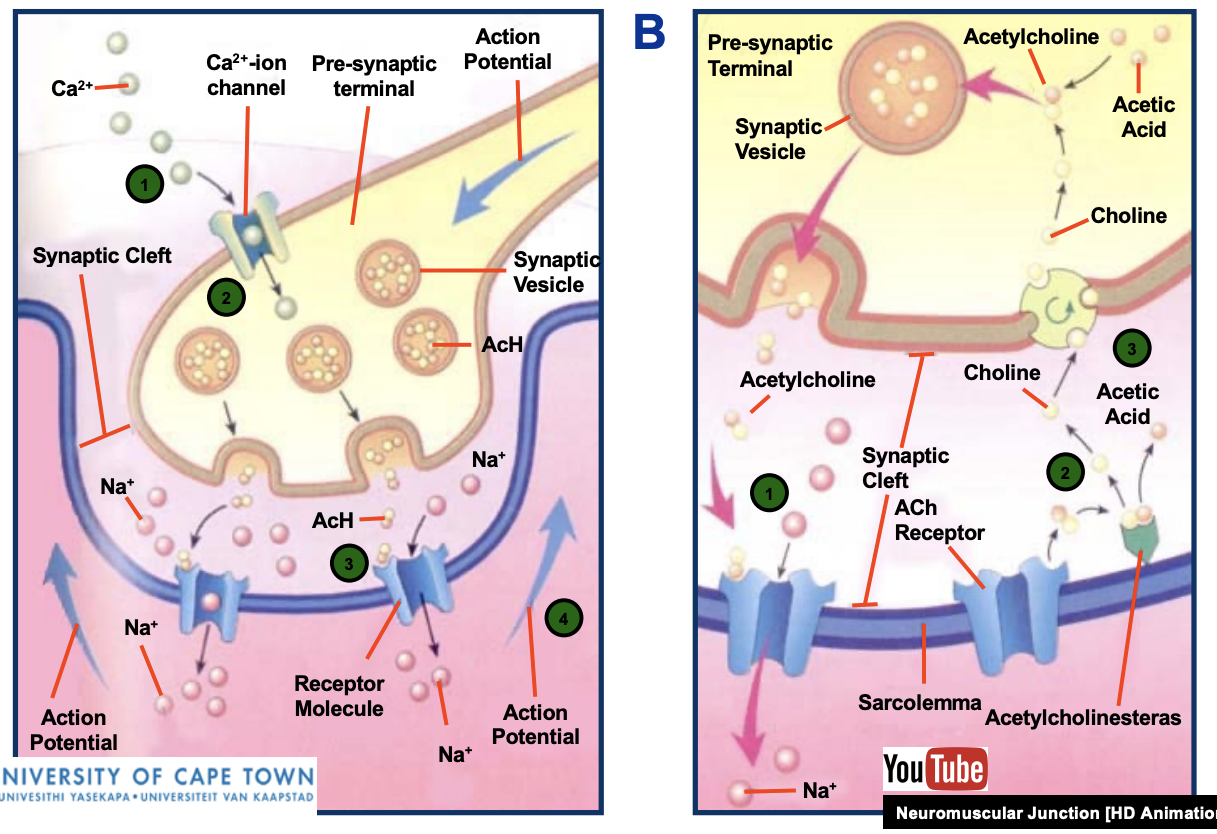
Neuromuscular Junction (Motor End Plate)
Neuromuscular junction or motor end plate – the terminal branches of the axon of a motor neuron contacts the target muscle fibre
No direct physical contact between the membranes of the nerve and muscle cells
found near the middle of the muscle fibre
Acetylcholine is stored in pre-synaptic vesicles
An action potential initiates the release of 300 molecules of acetylcholine
After crossing the gap, acetylcholine is broken down by acetylcholinesterase
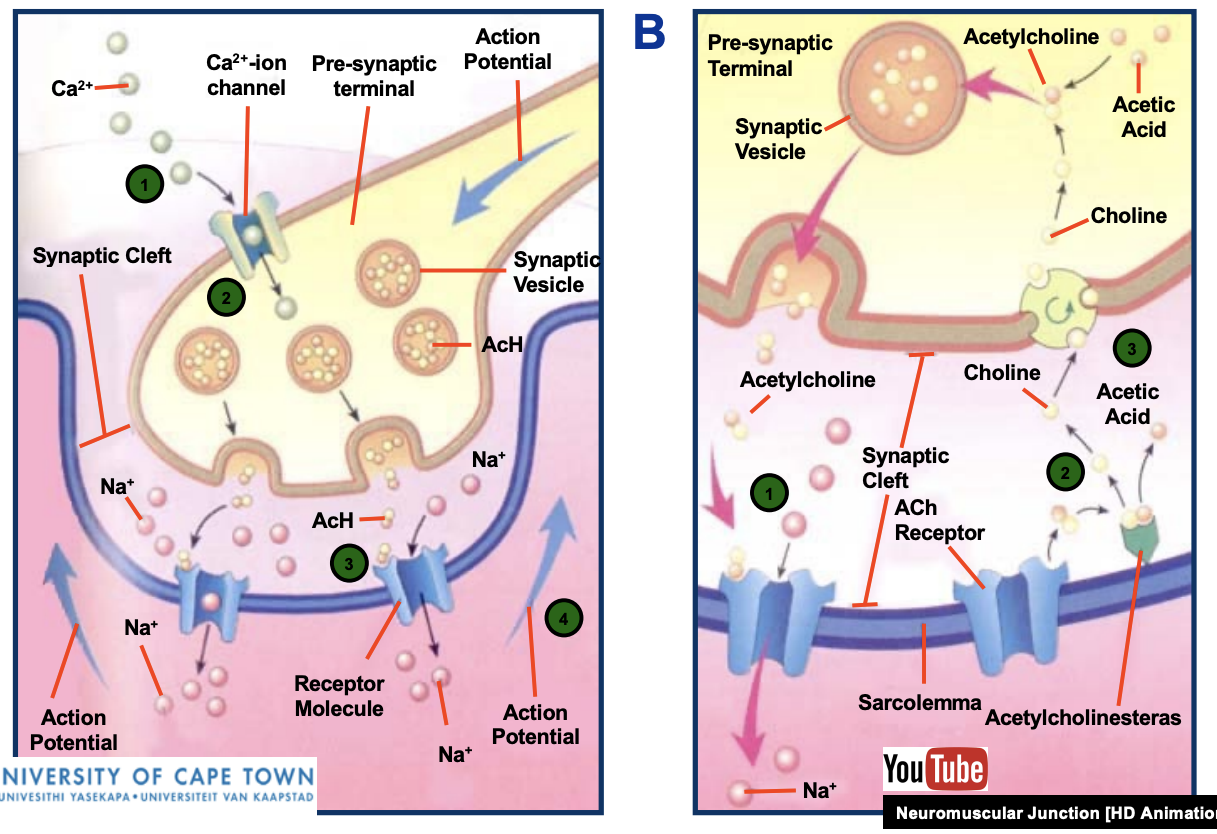
Release of ACh and Na+
when acetylcholine (ACh) is released during muscle contraction, sodium (Na+) ions are released into the muscle cell
This influx of sodium ions is what initiates the process of muscle contraction
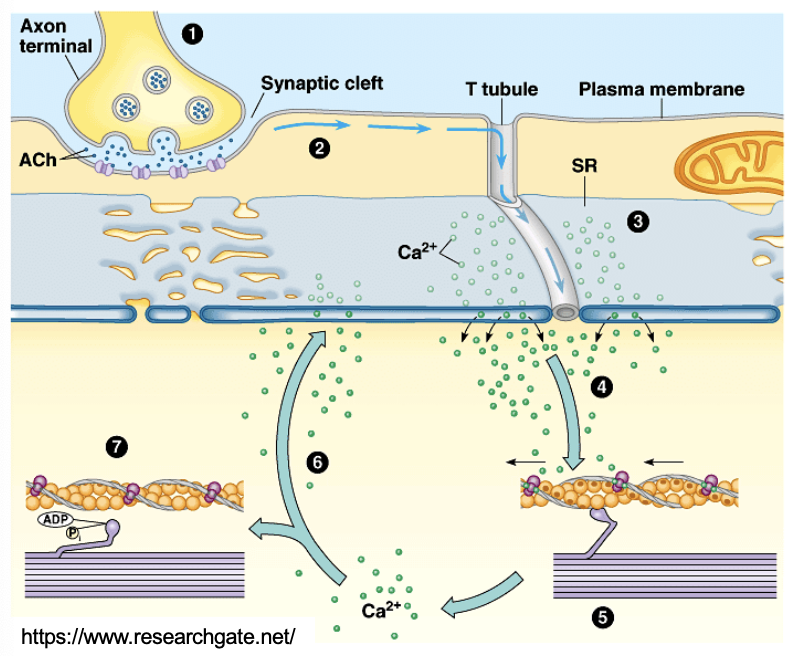
Excitation-Contraction (E-C) Coupling
the process by which an electrical stimulus triggers the release of Ca2+ from the SR, initiating the mechanism of muscle contraction by sarcomere shortening
Process of EC
(1) AP arrives at the neuromuscular junction and triggers ACh release, ACh diffuses across the synaptic cleft, binds to its receptors on the plasma membrane
(2) the post-synaptic action potential propagates along the sarcolemma and down the T-tubules
(3) triggers Ca2+ release from the SR
(4) Ca2+ binds to troponin which undergoes a conformational change, removing the blocking action of tropomyosin
Cross bridge cycle is triggered
(5) contraction occurs
(6) Ca2+ is actively removed and moved back into the SR when the action potential ends
(7) tropomyosin blockage is restored, and the muscle relaxes.
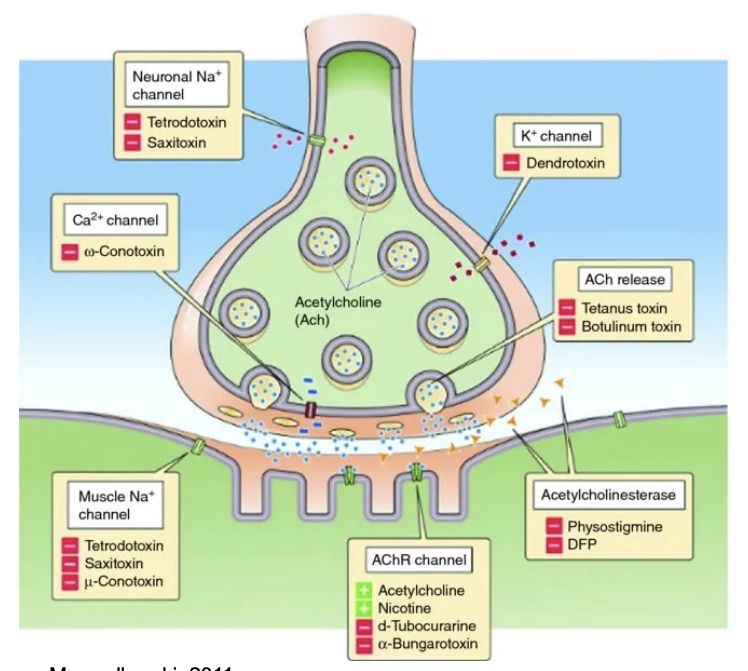
Toxins associated with Junctionopathies
Junctionopathies - Disorders of the Neuromuscular Junction
Several proteins involved in synaptic transmission within the neuromuscular junction are the targets of naturally occurring or synthetic drugs
Antagonists (inhibits or interferes) are shown as minus signs highlighted in red.
Agonists (mimics) are shown as plus signs highlighted in green
EXAMPLE: Botox - Botulinum Toxin
Muscle Cramps
are involuntary and forcible uncontrollable muscle contractions that can’t relax
can affect any muscle/ groups of muscles
exercise associated muscle cramp (EAMC)
nocturnal muscle cramps
In Vitro Muscle Contraction Experiments
Contractile behaviour of skeletal muscle (muscle twitch) is easily studied in vitro. Include:
1. Isometric Twitch (Contraction) of an Isolated Muscle
2. Summation and Tetanus
3. Concentric Twitch (Contraction) of an Isolated Muscle
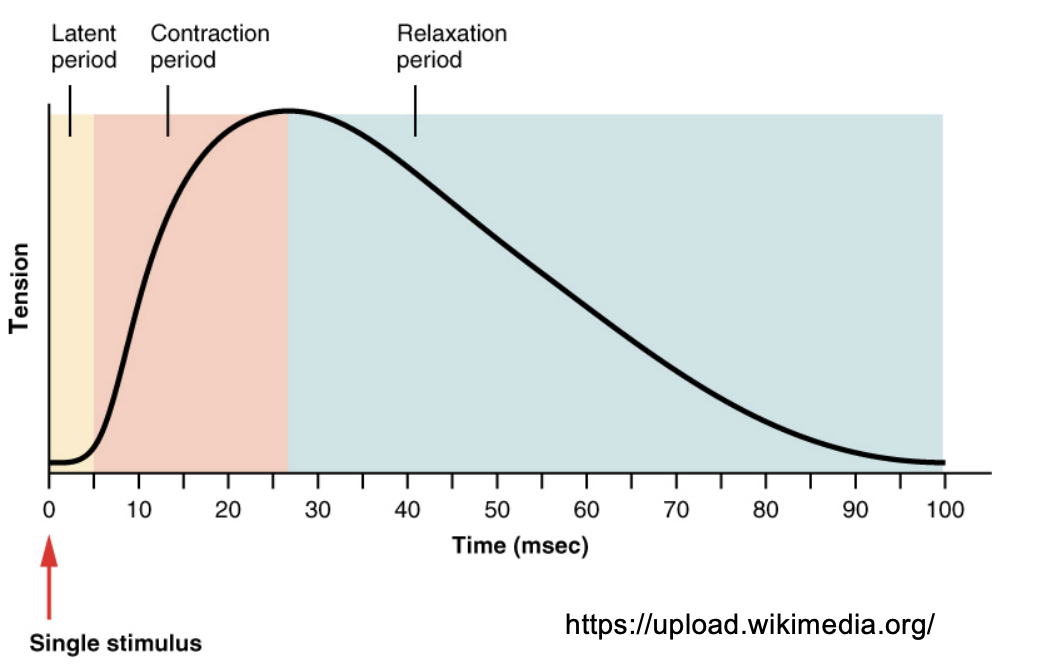
Muscle Twitch
simplest contract
Shortening response to a single action potential or electrical stimulus (msec).
Three phases (periods) of a muscle twitch:
1. Latent Phase (2 msec) Membrane activation, Ca2+ release from SR, diffusion in interfilament space, deinhibition of actomyosin ATPase
2. Contraction Phase
3. Relaxation Phase
Summation
If the muscle is stimulated before it fully relaxes, the force produced by the second twitch will be greater than the first
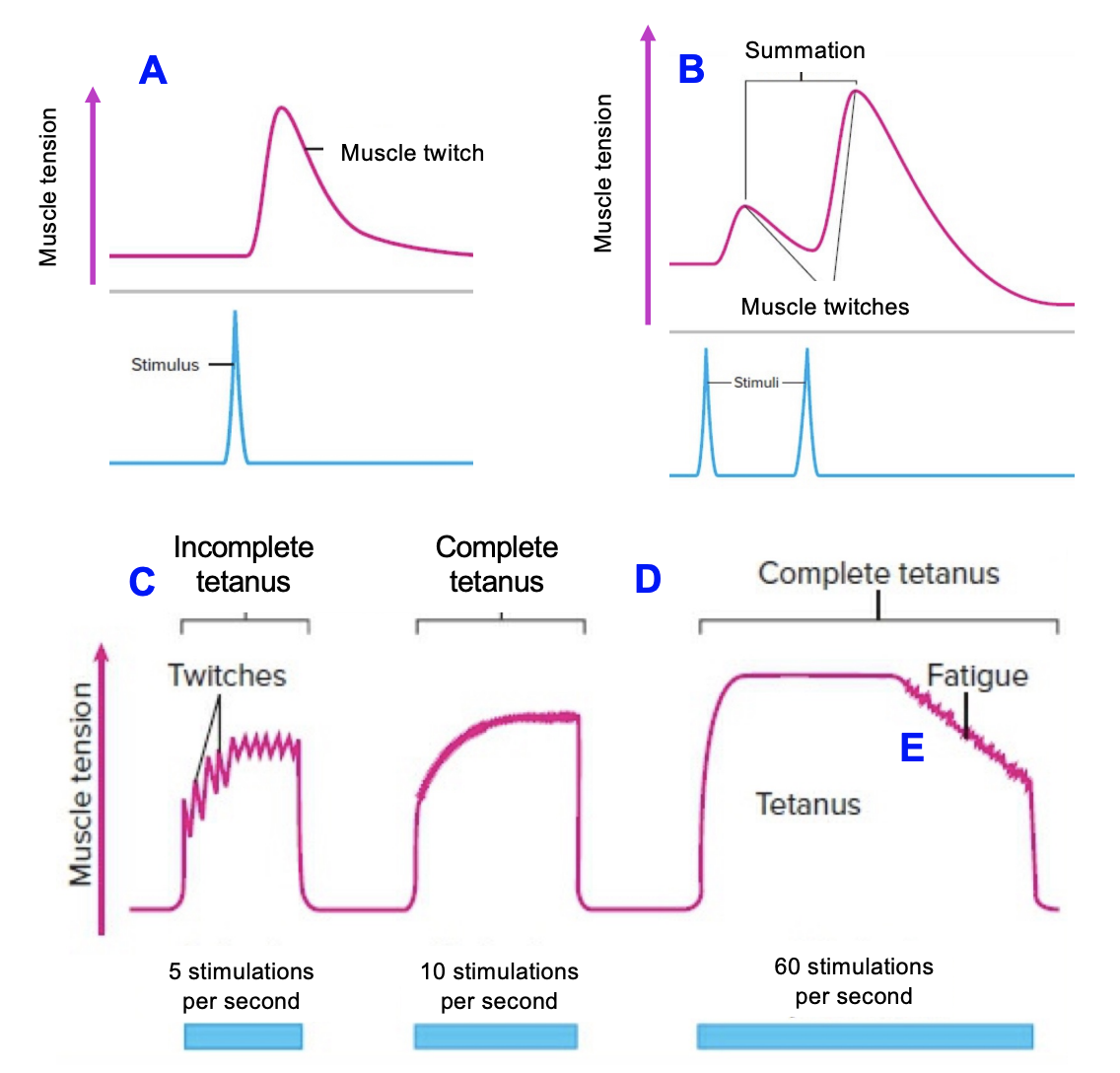
Incompleted Tetanus (Unfused tetanus)
If we increase the frequency of stimulation the relaxation time between successive twitches will get shorter and shorter as the strength of contraction increases in amplitude. When there is still a partial relaxation
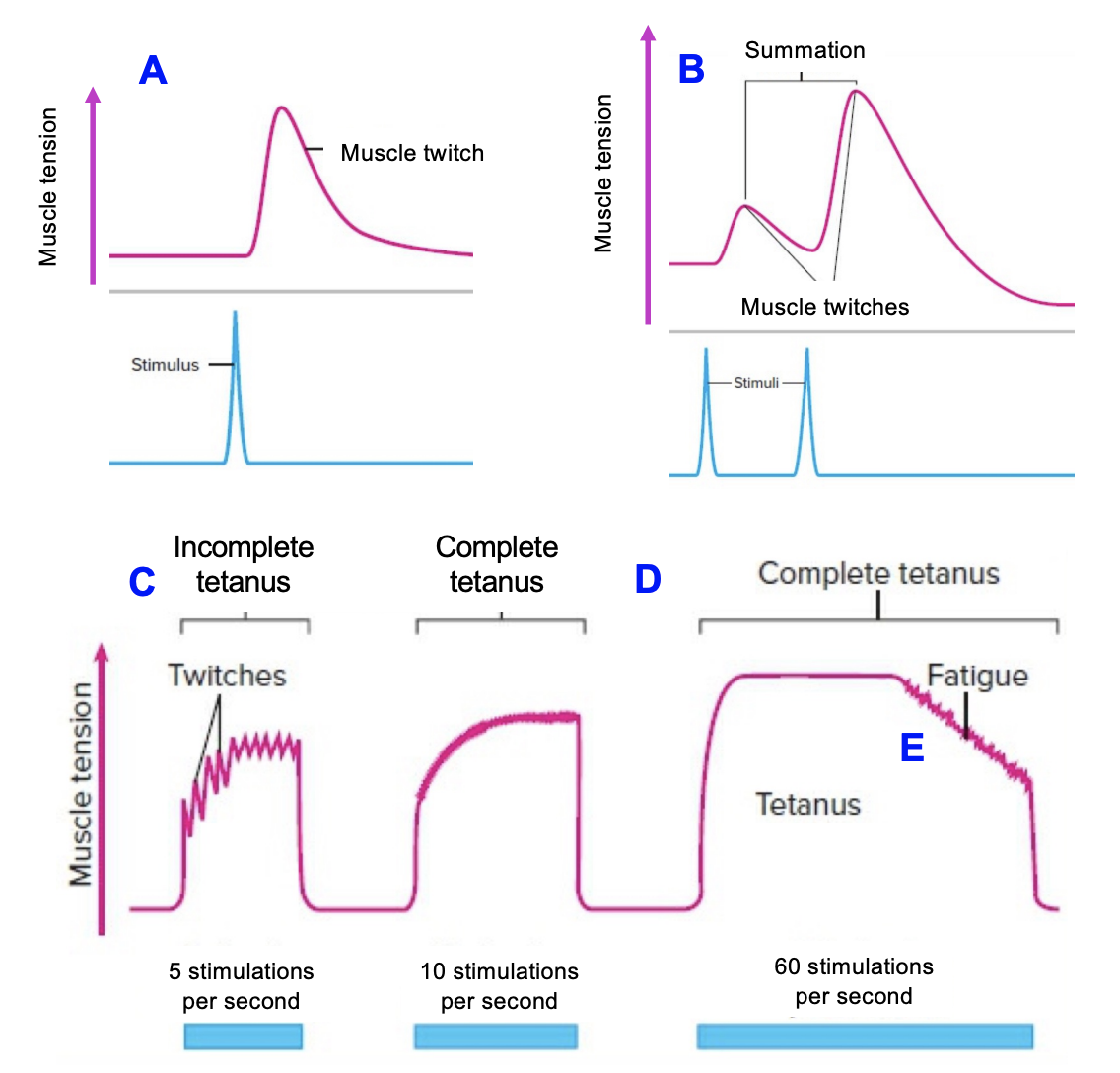
Complete tetanus (Fused tetanus)
A stimulation frequency is eventually reached where there is no visible relaxation between successive twitches. The contraction becomes smooth and sustained
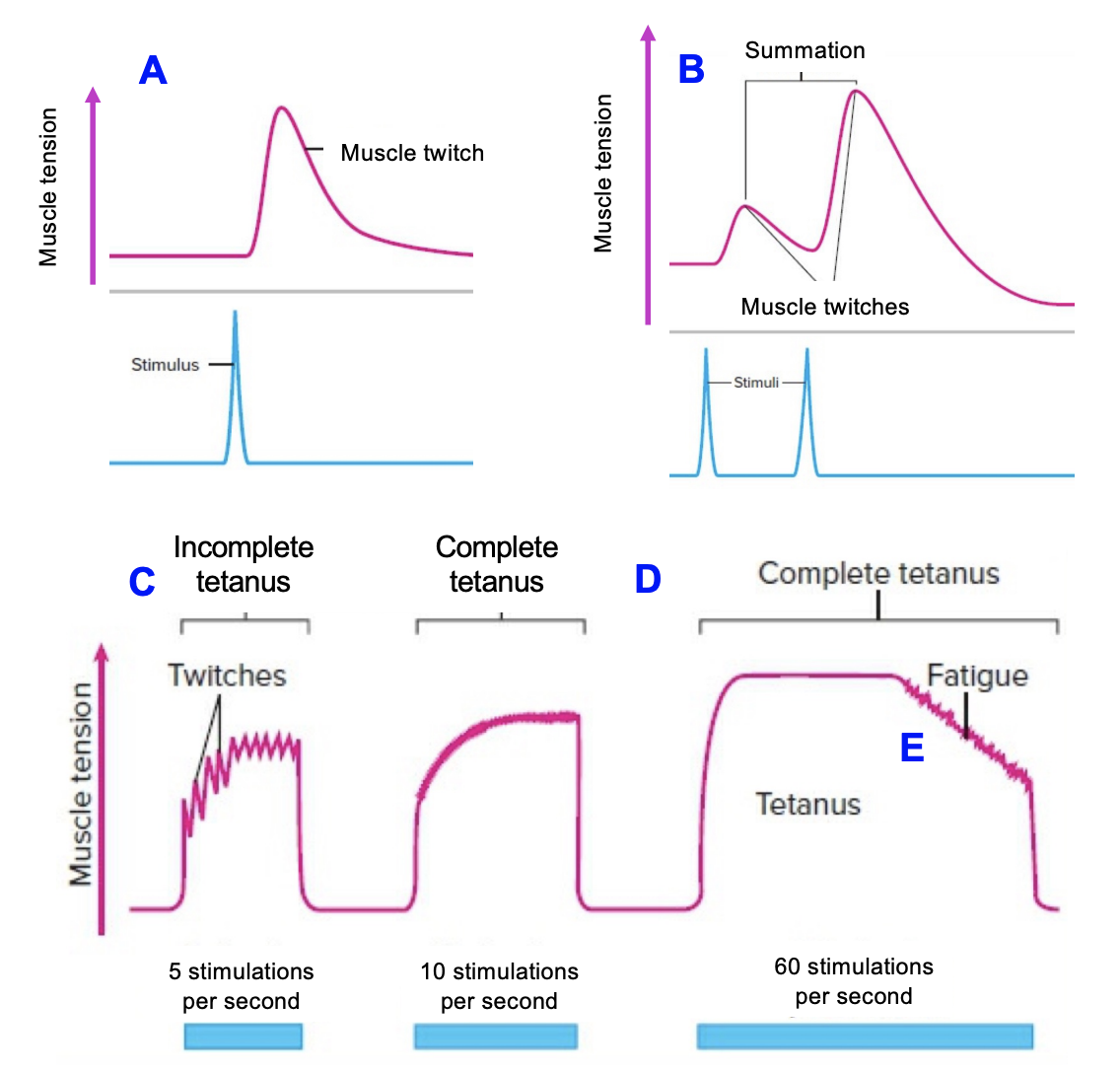
Fatigue
Eventually the stimulated muscle will start to fatigue due to the multiple muscle twitches
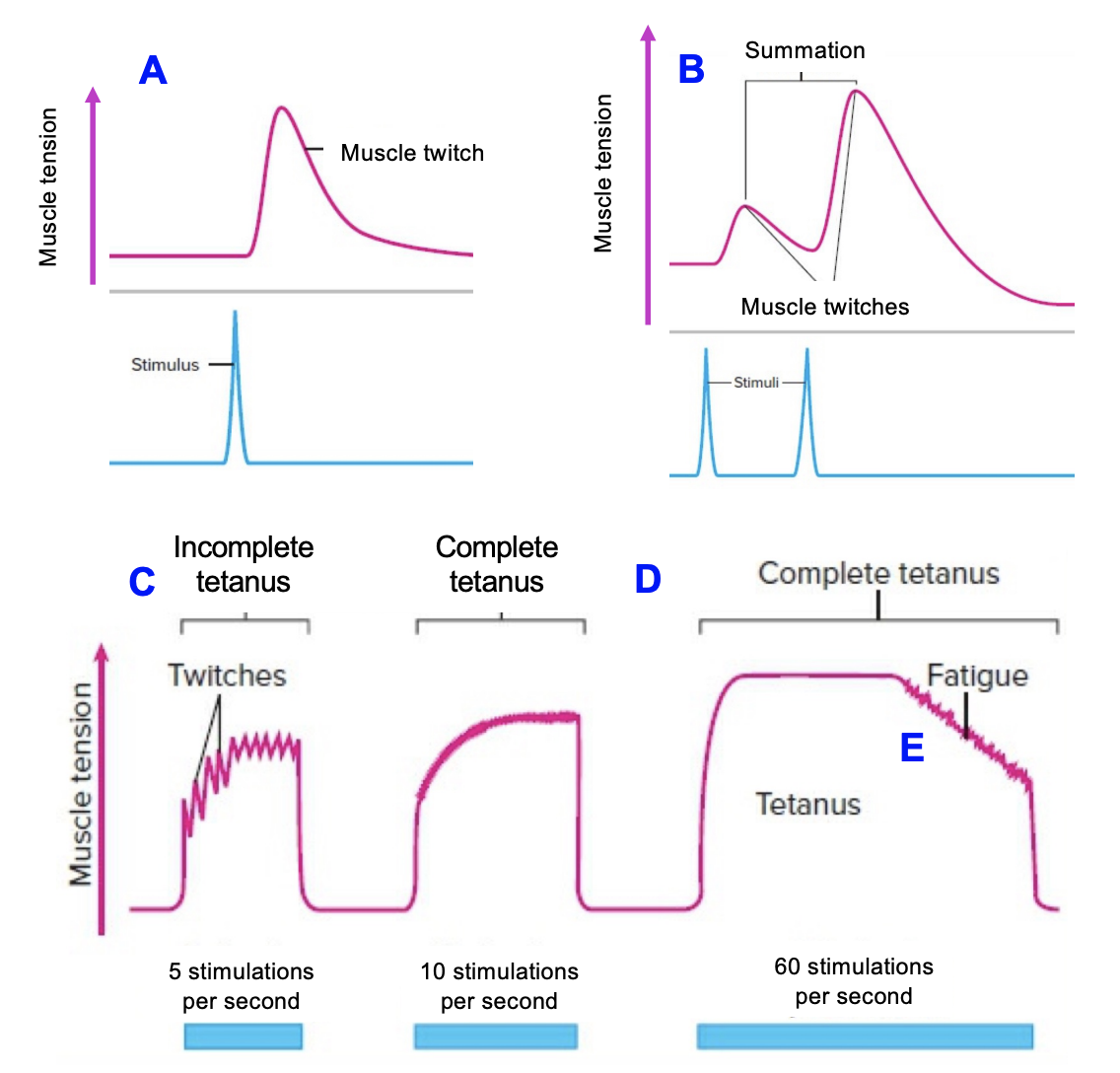
Load (force) velocity curve
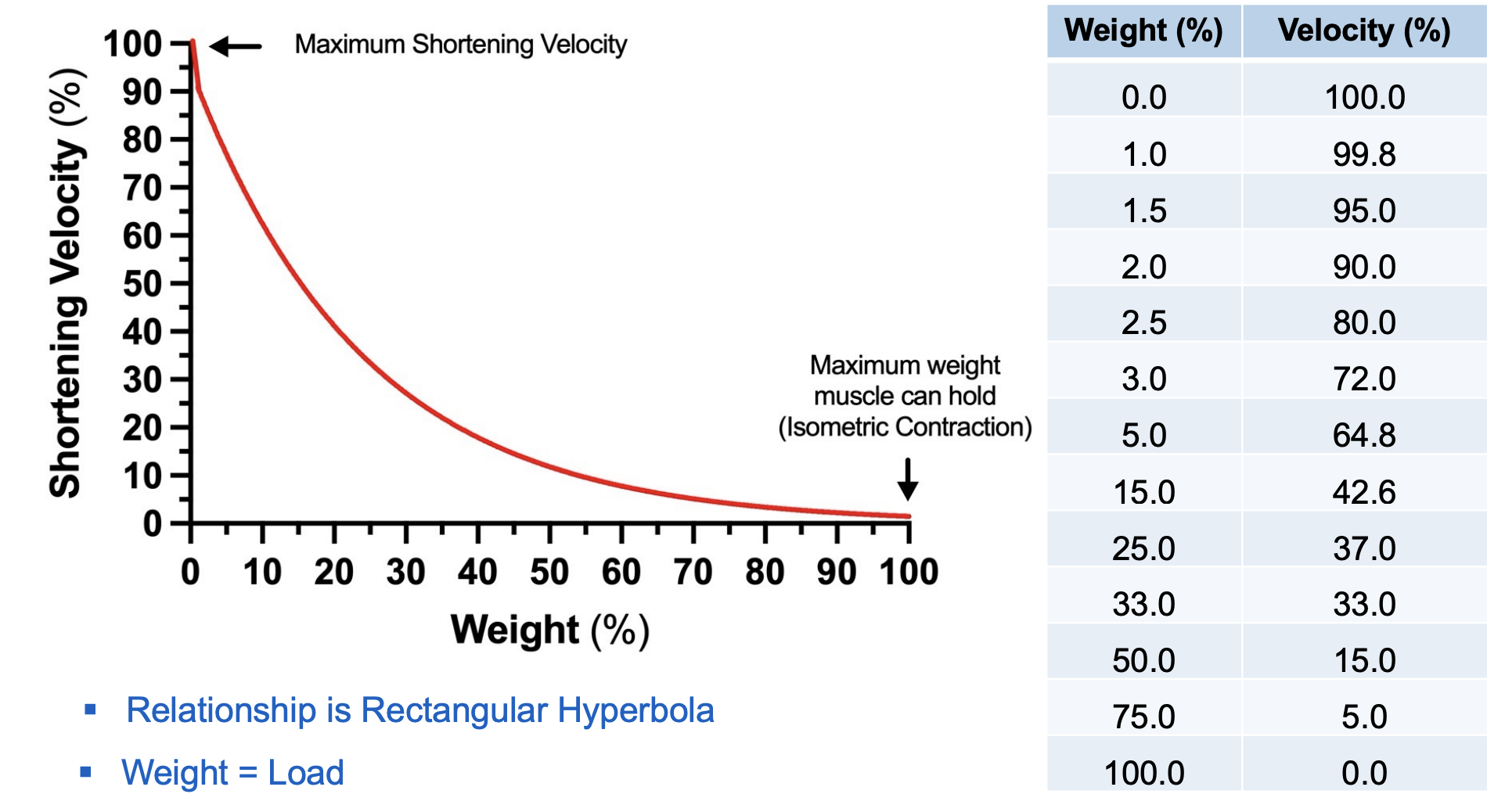
Load (force) power curve
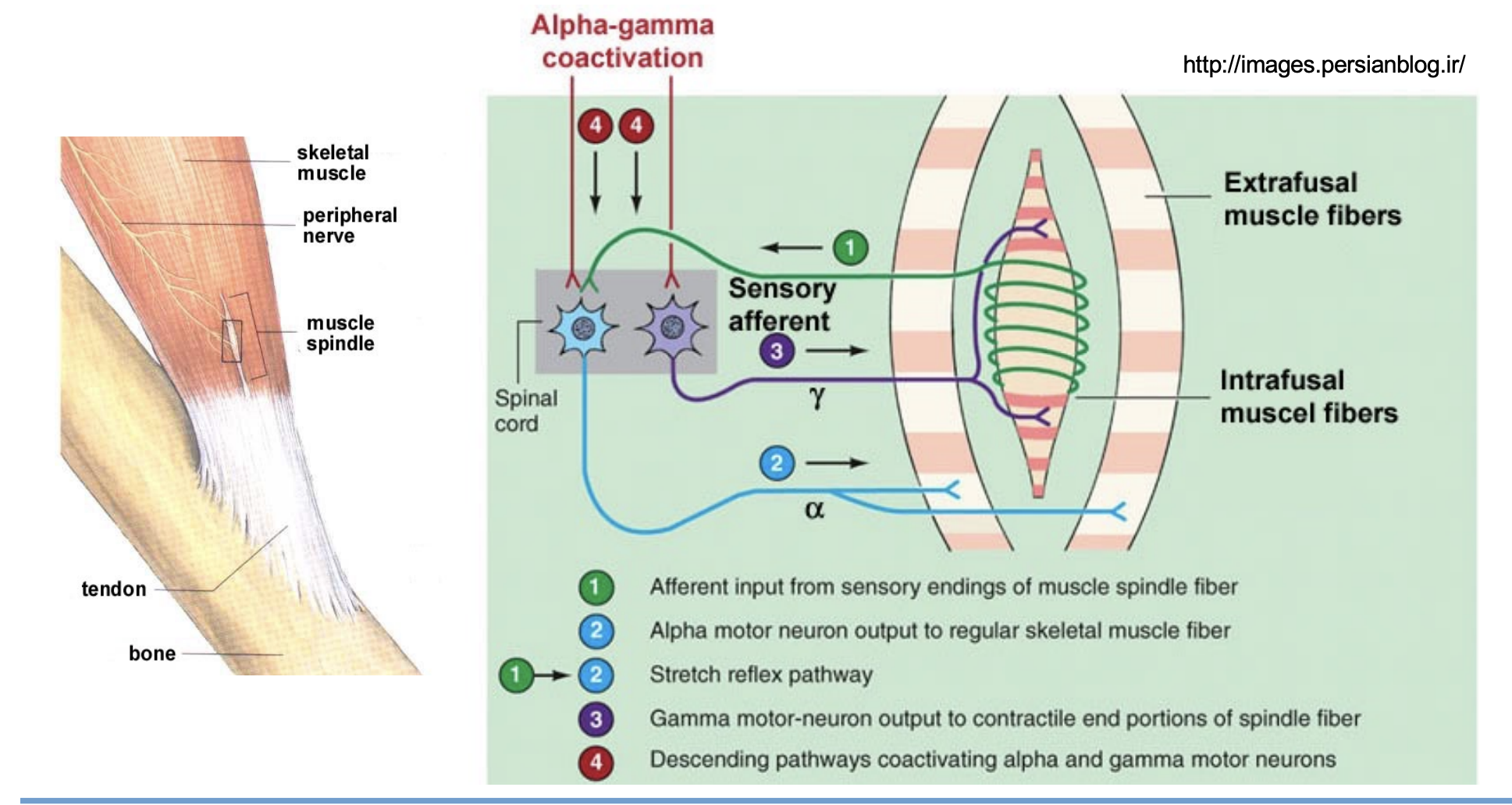
Neurons
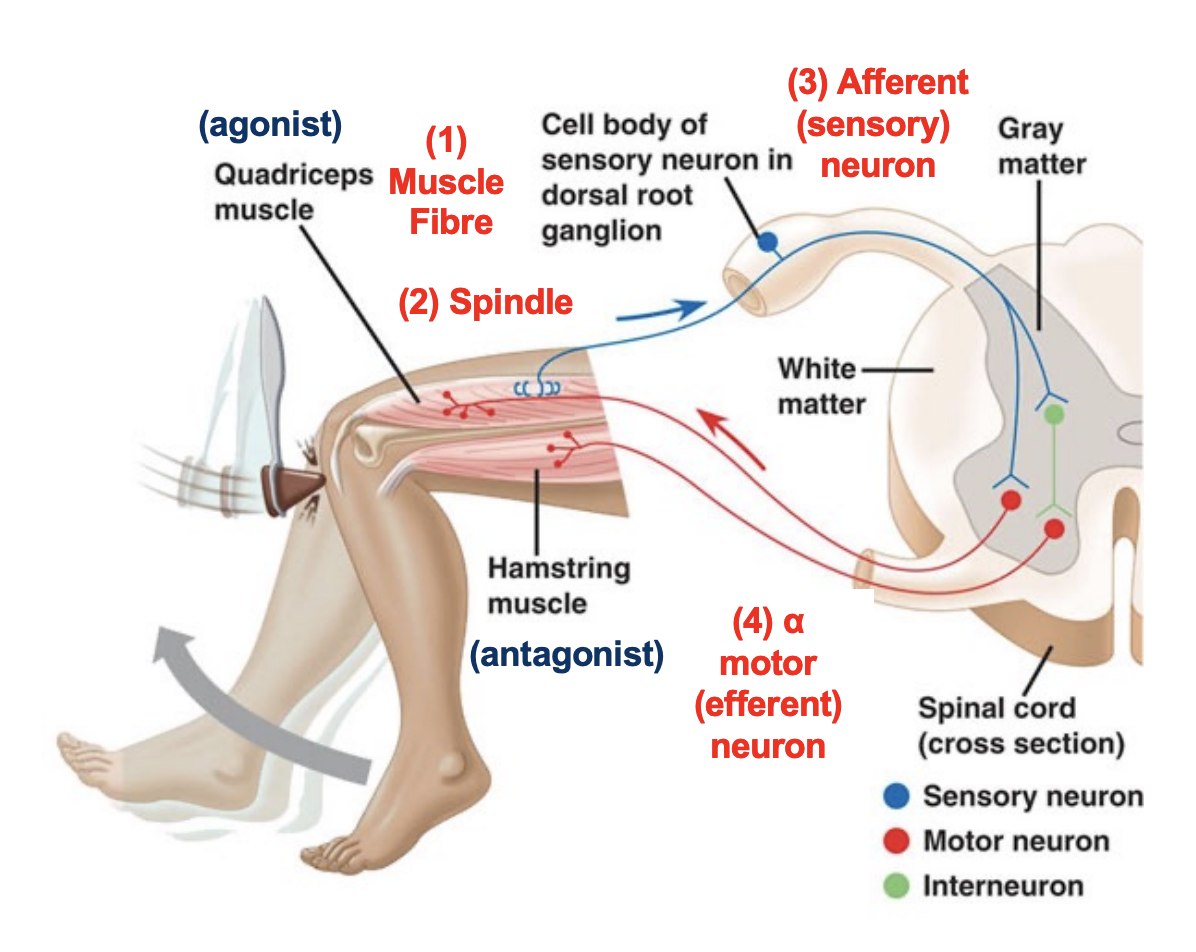
Afferent Neuron + Sensory Neuron:
Receives information from a receptor
Transmits information TOWARDS the CNS
Efferent Neuron + Motoneuron
Transmits information AWAY from the CNS towards a muscle or gland
1. alpha (a) motor neuron - supply skeletal muscle fibres (muscle contraction)
2. gamma (g) motoneuron - supply muscle spindles (keep them taut)
Muscle Proprioceptors
1. Muscle spindle 2. Golgi tendon organ
They determine the position of a limb in space from the following information:
1. joint angle 2. muscle length 3. muscle tension
Muscle Spindle
Muscle spindles are connective tissue capsules (receptors) found in the perimysium (around fascicles)
They contain specialized fibres (intrafusal) which have an afferent (impulses towards the CNS) and efferent (impulses away from the CNS) nerve supplies.
Spindles monitor muscle movement
γ (gamma) motorneurons cause contraction of spindle muscle fibres to bare the load during muscle contraction
Golgi Tendon Organ (GTO)
GTOs are receptors
Respond to tension rather than to length
When forces of muscle contraction and/or external forces can cause injury to muscle, tendon or bone or when joints could be damaged during the shortening of muscles GTO sends stimulatory signals to activate the antagonist (opposite action muscle) and inhibitory signals for the agonist (same action muscle).
Reflex Arc
the neural pathway that mediates a reflex action, which is a rapid, involuntary response to a stimulus