IMED1004 - Macronutrients and Energy Balance (L16)
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
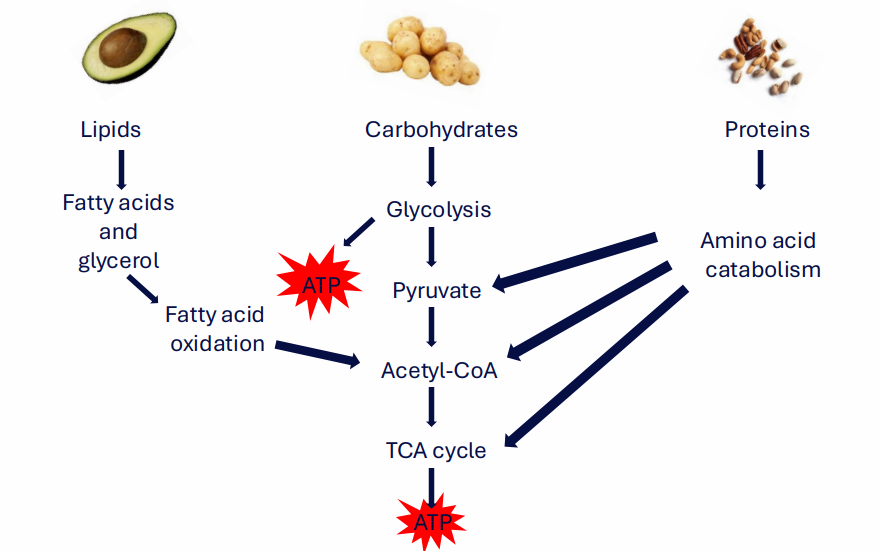
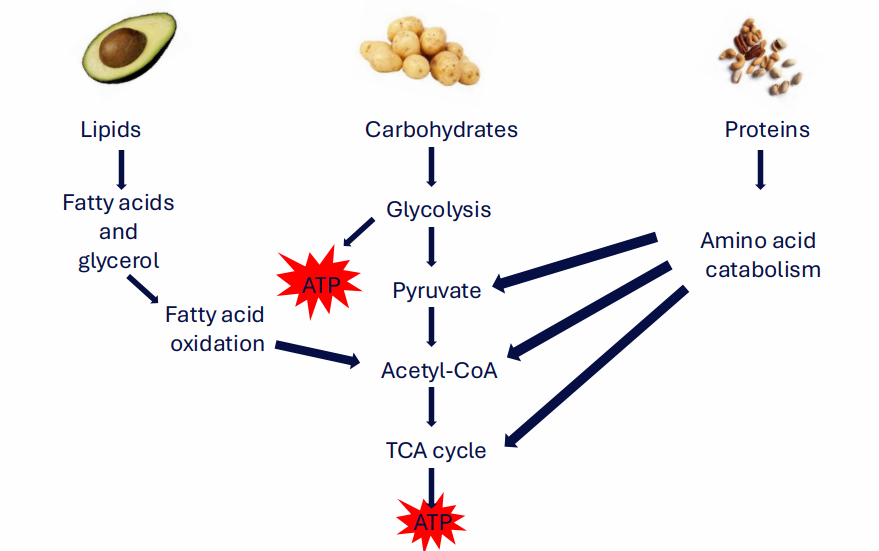
Energy comes from macronutrient metabolism
- Lipids -> Fatty Acids and Glycerol -> Fatty Acid Oxidation -> Acetyl CoA
- Carbohydrates -> Glycolysis -> Pyruvate -> Acetyl CoA -> TCA Cycle
- Proteins -> Amino Acid Catabolism -> Pyruvate and everuything
Evalulating Macronutrients
- Macronutrients provide energy and essential biomolecules
- Depends on the quantity of the macronutrient and quality of macronutrient
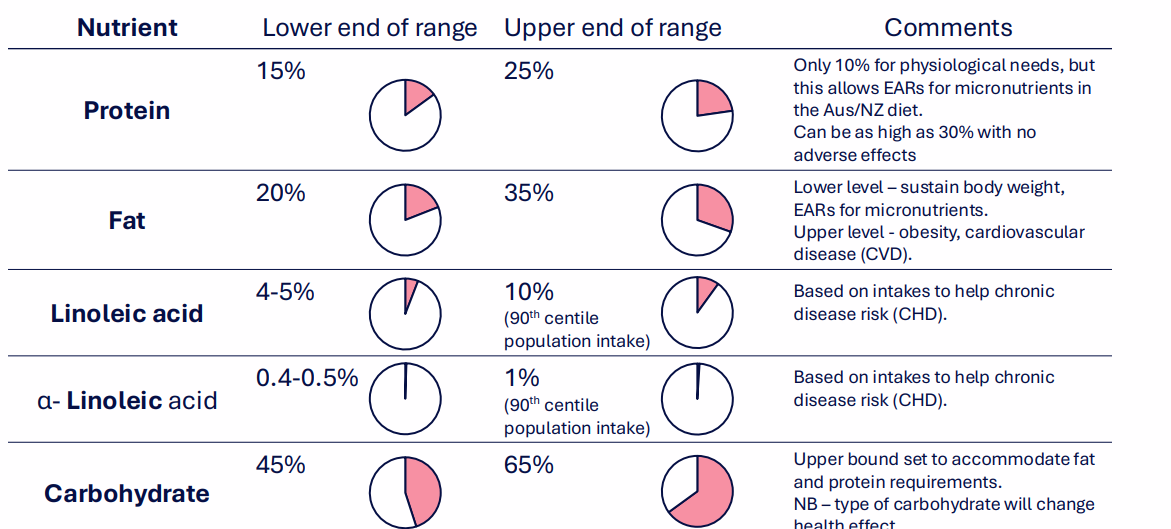
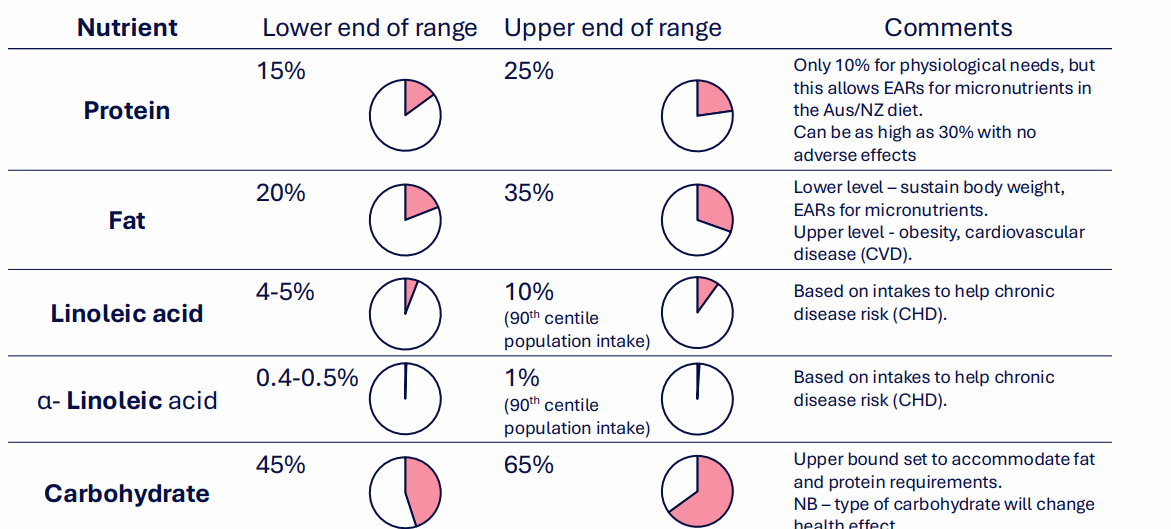
Acceptable Macronutrient Distribution Ranges (ADMR)
DIAGRAM ON SLIDE 6
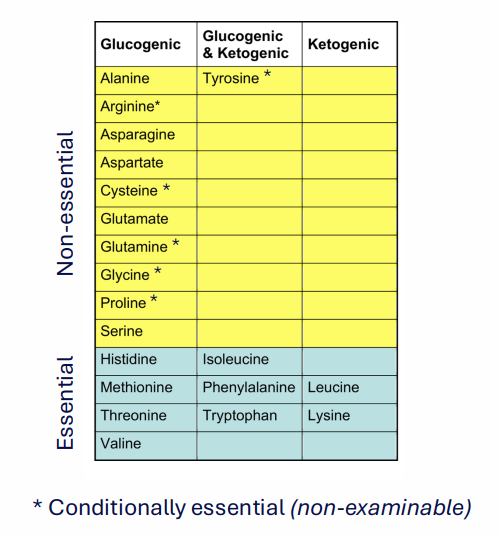
Role of Protein
- Provides essential (indispensable) amino acids (9 essential, 6 conditionally essential)
- Provides nitrogen for protein synthesis (growth, maintenance, repair)
- Source of energy (covered in 1003)
- Very important in growth and development
- Protein quality is dictated by: amino acid composition and digestibility
- There is no storage of amino acids
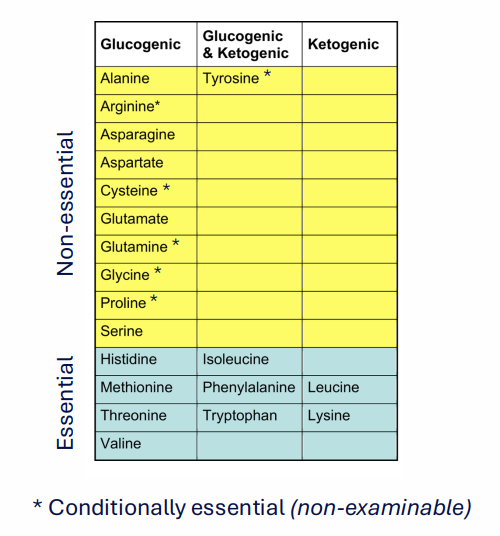
Protein Metabolism
- Carbon backbone is used to produce energy
- Glucogenic -> pyruvate or TCA cycle intermediates
- Ketogenic -> acetoacetate or Acetyl CoA
- Some AA - both categories

Carbohydrates
- primary source of energy for most people
- Types of carbohydrates: fibres, starches, sugars
- Carbohydrate metabolism: Glycolysis, Pentose Phosphate Pathway, Glycogenesis/Glycogenolysis (Storage), FA Synthesis (storage)

Glycaemic Response
- Glycaemic Response: change in blood glucose concentration in response to a meal
Factors which impact on glycaemic response:
- amount and types of carbohydrate consumed in a meal
- presence of other critical components of the meal (impact on digestion - fat slows down release)
- ease with which starch sources are digested
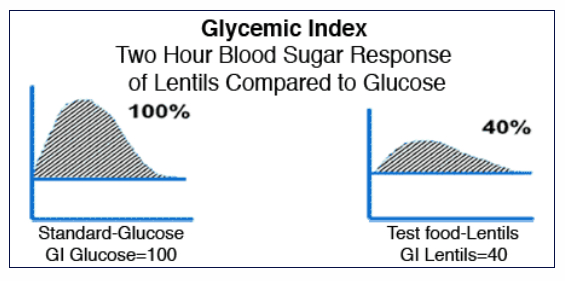
Assessing Carbohydrate Quality - Glycaemic Index (GI)
- High GI food causes rapid rise in blood glucose
- Low GI food causes gradual, lower rise in blood glucose
- Can be used to assist individuals in maintaining glycaemic control
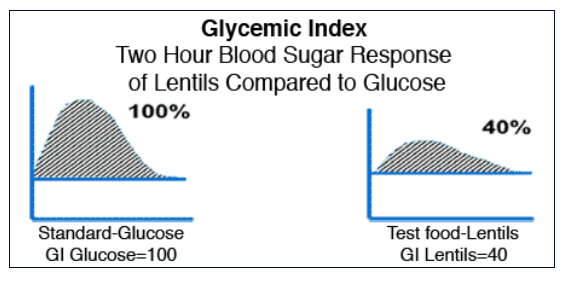
GI gives a measure of the quality of carbohydrate
- Food with a high GI will cause a greater glycaemic response
- This is standardised to the amount of carbohydrate in the food, however
- If we want to take into account the quality and quantity of the carbohydrate, we can calculate its glycaemic load
Added Sugars1
- dietary guidelines state to reduce intake of added sugar
- Added sugar has no additional nutrients, and overconsumption can eventually lead to type 2 diabetes
- Added sugar consumption occurs almost exclusively through consumption of sweetened beverages, and in snack foods
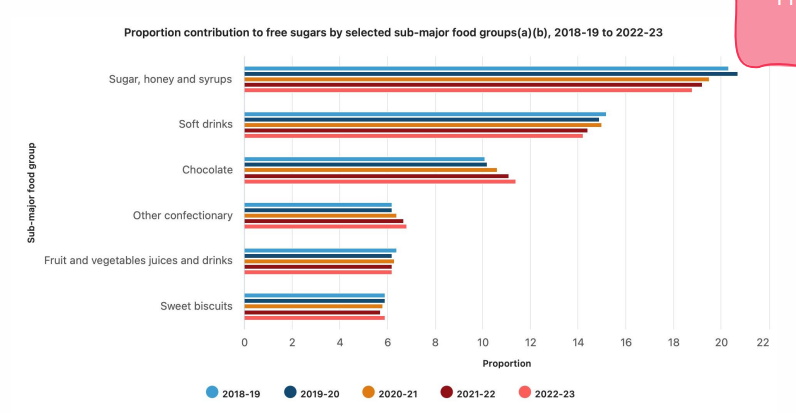
Excessive Intake of added sugar is common
- recommendation: free sugar is <10% of dietary energy
- reality: around 67g/day added sugar (12.3% of dietary energy)
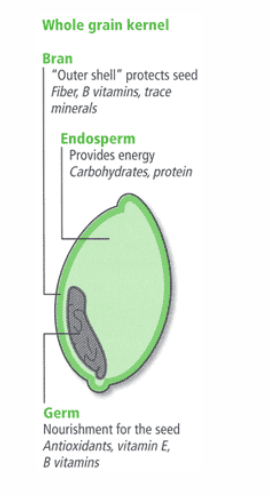
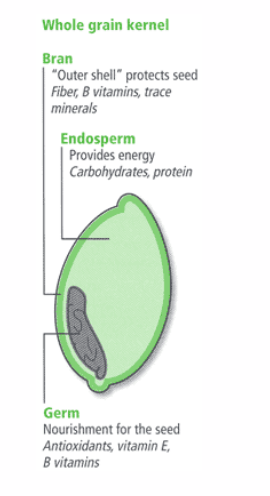
Whole and refined carbohydrates
- Whole grains contain fibre: can be milled (remove endosperm, germ, bran), as long as product contains those elements
- Refined: only the starch component
- Recommendation: 50% of carbohydrate intake should be as whole grains.
.
- wholegrain bread contains fibre as well, instead of white flour which just contains starch
- its the outer layer thats really good for us
Dietary Fibre
- non-digestible component of diet
- carbohydrates, gums and lignin
- Provided in the diet by whole grain foods, cooked dry beans and peas, vegetables, fruit and nuts
- Viscous fibres, non-fermentable fibres, fermentable fibres
THESE ARE THE FOLLOWING EFFECTS OF THE ABOVE FIBRES:
- blunt glycaemic response
- lower serum cholesterol
- essential for digestive health: colonic lubrication and transit
- Increase satiety
- IMPORTANT: protect against cardiovascular disease, obesity, type 2 diabetes
.
- main reasons: promoting a healthy gut microbiome, lowering blood cholesterol and blood sugar, increasing satiety for weight management, and binding with carcinogens for elimination from the body.
Viscous Fibres
(delay gastric emptying, reduce nutrient digestion, reduce nutrient absorption, Reduce bile acid reabsorption)
Non-fermentable fibres
(increase water holding, more frequent bowel movements (delay gastric emptying)
Fermentable fibres
promote growth of GI bacteria, increased stool size, short chain FA production

Simialr Foods can vary substantially when it comes to dietary fibre
- Refined foods lack dietary fibre as well as vitamins

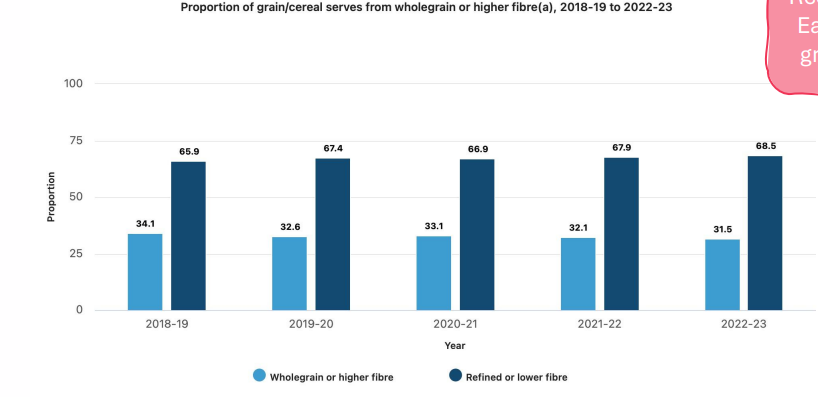
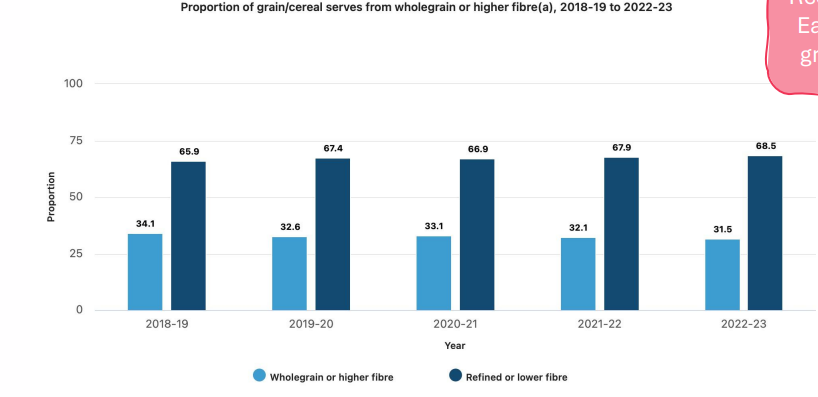
Insufficient intake of dietary fibre is common
- Recommendation: eat mostly whole grains or cereals
Role fo fat
- some fats are essential (linoleic acids, alpha-linolenic acids)
- Fat soluble vitamins are absorbed and transported with fats
- Metabolism of fat provides energy
- fats are necessary for the production of steroid hormones, bile salts and lipoproteins
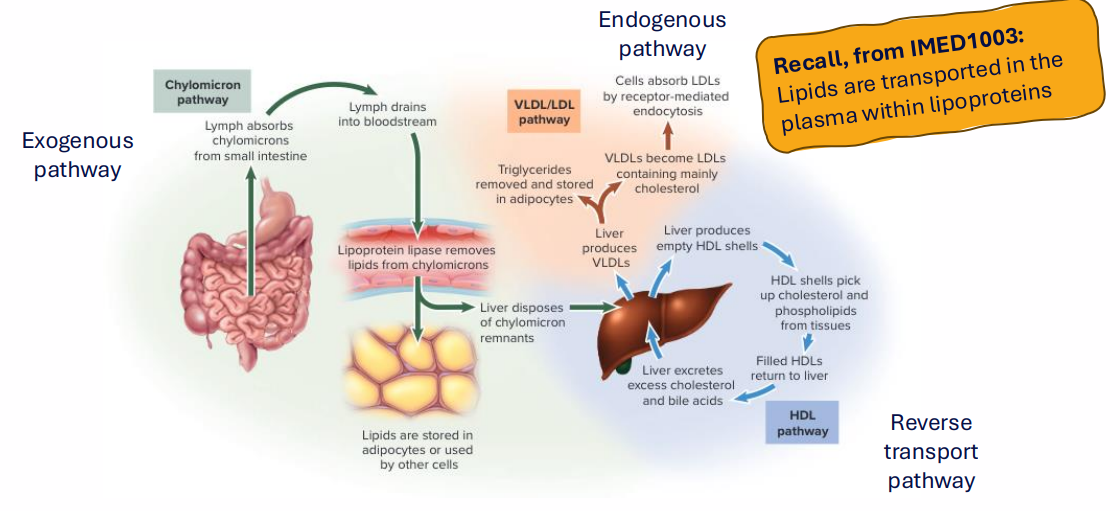
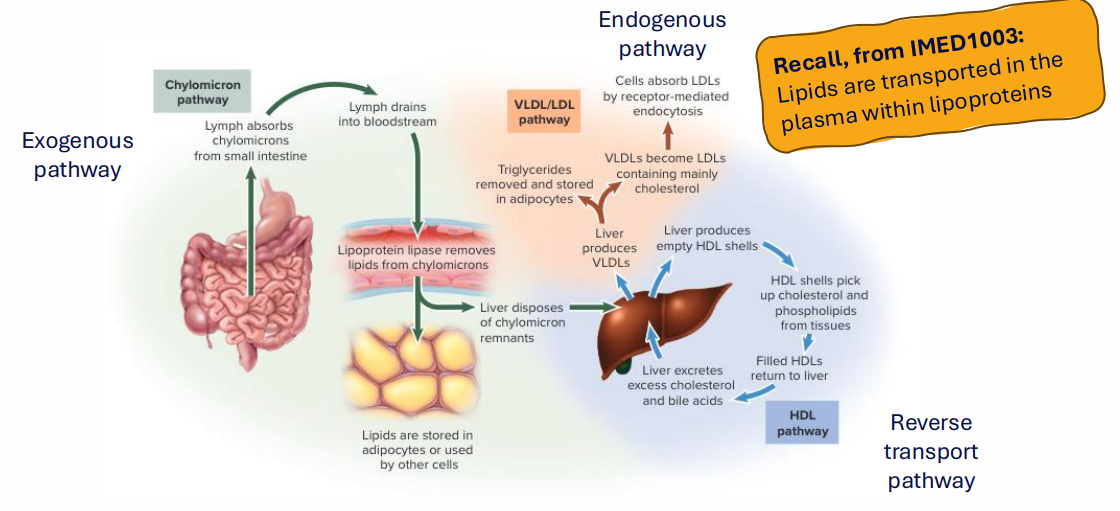
Cholesterol Distribution: Lipid transport between tissues
- Lipids are transported in the plasma within lipoproteins
NO LEARNING OUTCOME
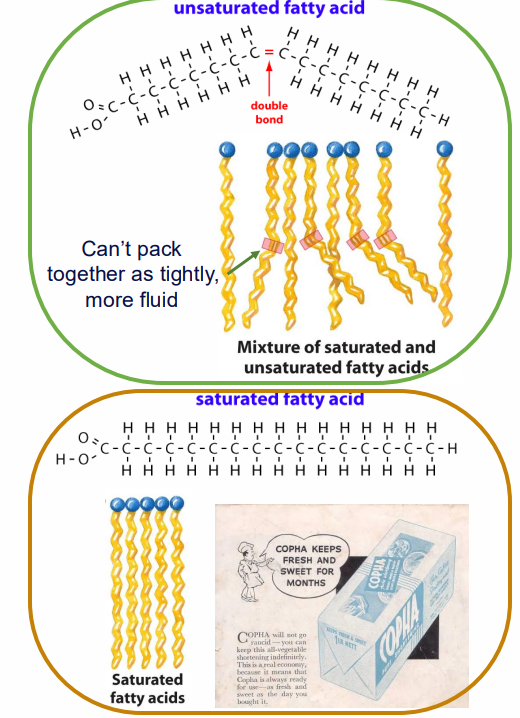
Why are some fats "good" and some "bad"
- Different types of fat promote the formation of different kinds of cholesterol
- Remember, "cholesterol" can refer to either: the family of chemical compounds or lipoproteins which carry cholesterols and other fats
LDL - low density lipoprotein = "bad cholesterol"
- causes formation of atherosclerotic plaques in arteries
- saturated fatty acid (SFA) consumption increases LDL
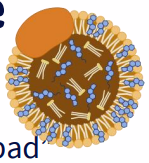

HDL - high density lipoprotein = "good cholesterol"
- scavenges lipoproteins, decrease in atherosclerotic plaques
- unsaturated fat consumption increases HDL
- recommendation to consume more monounsaturated, polyunsaturated fatty acids

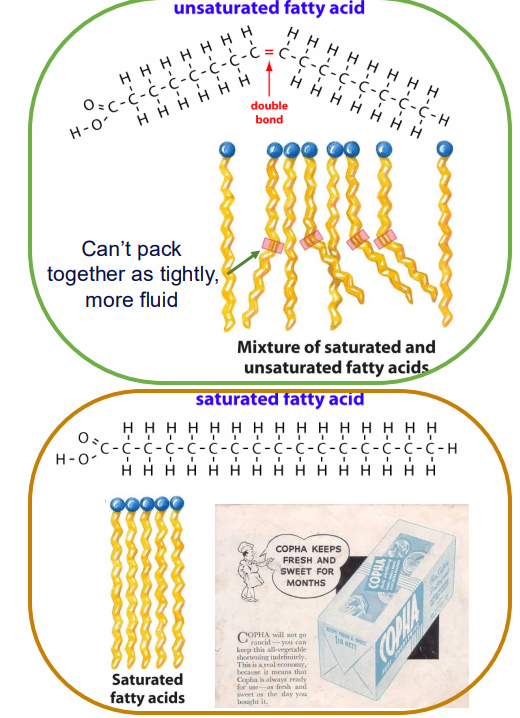
Hydrogenated Fats
- unsaturated fats can become rancid - unpalatable (chemically: spontaneous conversion to ketones)
- can be prevented by converting unsaturate fats to saturated fats (hydrogenation - adding hydrogens across double bond)
.
- because they can spontaneously convert to ketones, its the reason you shouldn't hoard olive oil, this can spontaneously change
Problem with hydrogenation
- some cis double bonds are converted to trans double bonds
.
TRANS FATS:
- increase risk of cardiovascular disease (CVD)
- increase LDL ("bad") cholesterol, decrease HDL ("good") cholesterol
- increase inflammatory response, further increasing risk of CVD
- are rare in australia, but no legal requirement to declare them in nutritional information
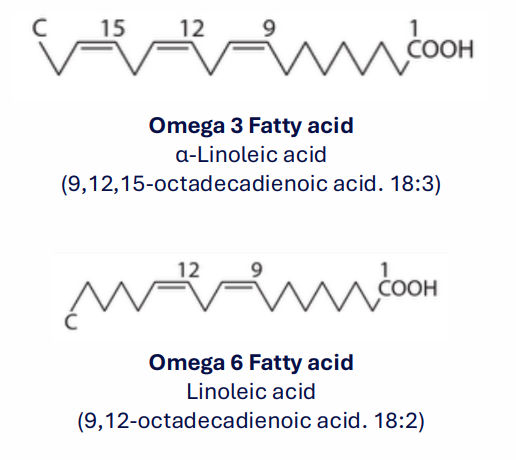
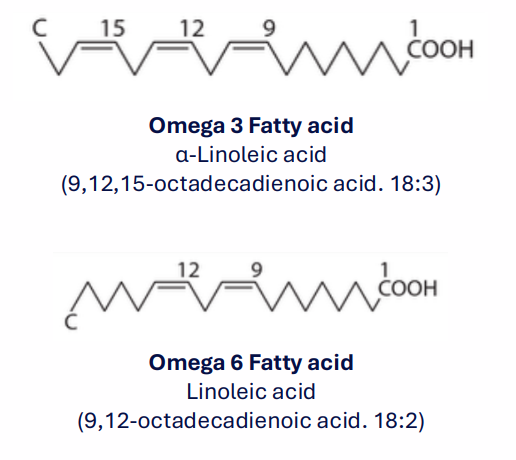
Essential PUFAs: Omega 3 and 6 fatty acids
- Polyunsaturated Fatty Acids (PUFA) - more then one double bond
- the double bond closer to the methyl end of the chain is of greater biological importance
- "omega" indicates we are counting from the methyl end
- We cannot synthesise Omega 3 (alpha-linolenic) and Omega 6 (linoleic) fatty acids, and therefore they must be taken in through the diet
- These are Phospholipids in cell membranes
- Their Derivatives are signalling molecules involved in mediating inflammation, vasoconstriction, platelet aggregation
.
- we lack the enzymes that allow us to make double bonds past carbon 9, so we need to consume some of these particular PUFAs which have more then one double bond and have that past carbon 9 as well
- IMPORTNAT NOTE: normally we name fatty acids from the carboxyl, which is why she put the conventional name in brackets. However, for these we start from the methyl end)
How Omega 3 and Omega 6 fatty acids relate to arachidonic acid metabolites
- FROM L9
- it mentioned how it was formed from arachidonic acid via enzymatic reactions
- these enzymatic reactions are actually using these linoleic acids
.
arachidonic acid and linoleic acid are not the same; linoleic acid is a precursor, meaning it is converted in the body into arachidonic acid. Both are omega-6 polyunsaturated fatty acids, but linoleic acid is an essential dietary fatty acid (18 carbons, 2 double bonds), while arachidonic acid is a longer-chain, more unsaturated fatty acid (20 carbons, 4 double bonds).
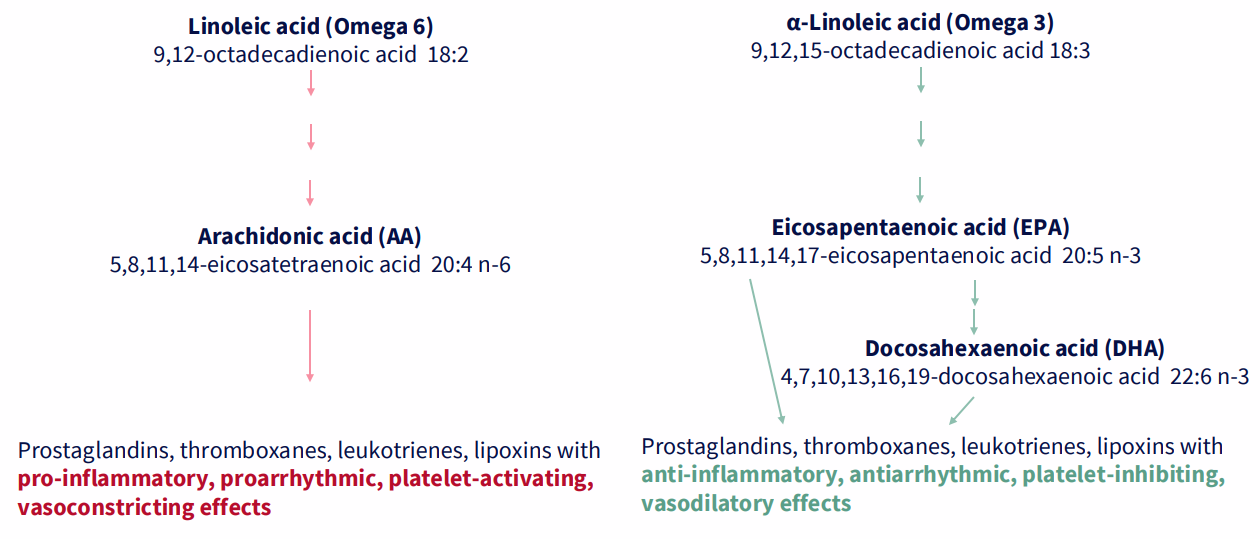
Omega 3-, Omega 6-derived messengers have opposing effects
Linoleic acid (omega 6) --> arachidonic acid (AA) --> these have pro-inflammatory, proarrythmic, platelet-activating, vasoconstricting effects
.
alpha-linoleic acid (Omega 3) --> Eicosapentaenoic acid (EPA) --> Docosahexaenoic acid (DHA) --> these have anti-inflammatory, antiarrhythmic, platelet-inhibiting, vasodilatory effects
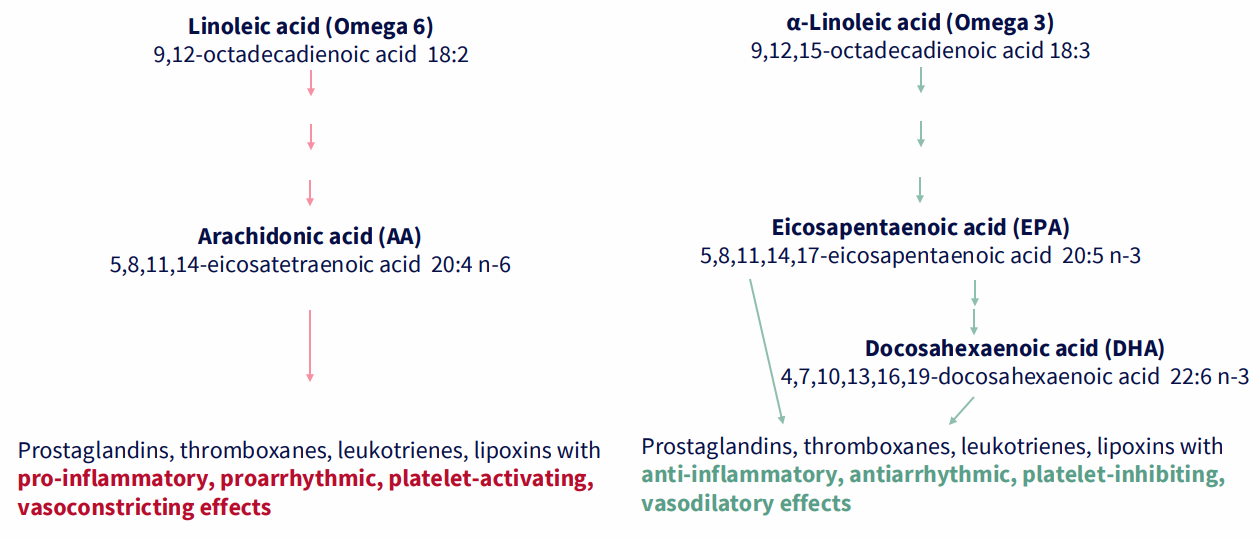
Essential PUFAs: Omega 3 and 6 fatty acid RATIOS
The ratio is important to health:
- 4:1 or 1:1 is optimal Omega 6 FAs : Omega 3 FAs
- The North American settler diet is closer to 30:1
.
- imbalance in this ratio is associated with inflammation, [LDL] >> [HDL], cardiovascular disease
- Omega 3 fatty acids are high in leafy salads and fish oils
What are the energy requirements?
WE NEED TO CALCULATE:
- the amount of energy in our food
- the amount of energy we need
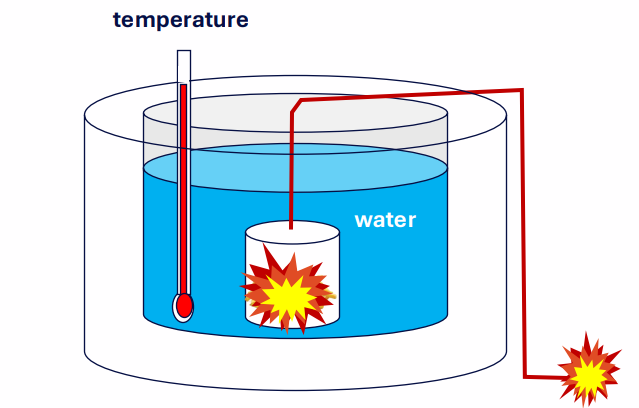
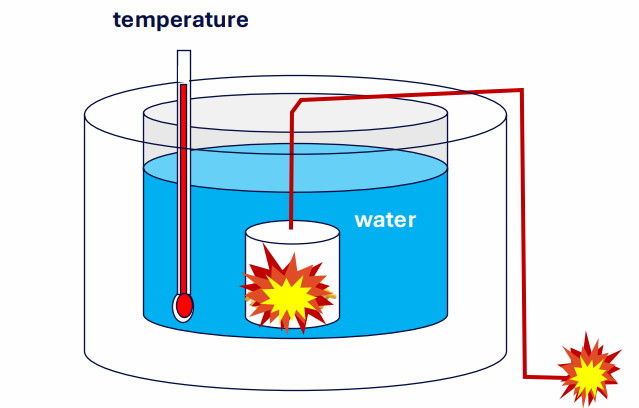
How much energy is in food (OLD METHOD)
- HISTORICALLY: use a bomb calorimeter to find out
- burn the food - how much does the temperature increase by?
- 1 Joule = heat required to raise 1g of water by 0.24C
.
- basically you put food in the middle, burn it and see how much energy it relesaes by calculating the energy change of the water
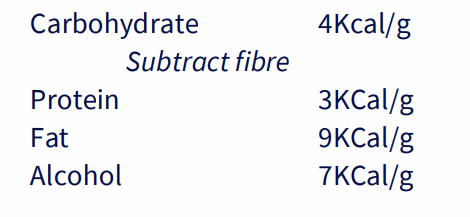
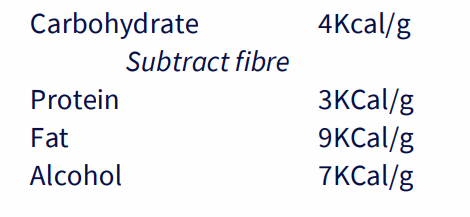
Measuring energy content - Atwater system
ADD UP THE AMOUNT OF THE COMPONENTS:
.
- these values were attained experimentally, by burning different foods of each category and averaging the values, and taking into account "apparent digestibility"
- NB: 1 calorie = 4.2 joules, 1 Calorie = 1 kilocalorie
- basically he determined that carbs had 4Kcal/g, protein had 3Kcal/g, Fat had 9Kcal/g and alcohol had 7Kcal/g. You could measure what was in ur food and measure the total energy content
How accurate was Atwater system
- think about the difference between eating a chocolate bar vs museli bar. The museli bar would take longer to chew
It takes energy to make energy from food
- The Atwater system provides us with a measure of metabolisable energy
- it does not account for the energy needed for digestion
- digesting a whole grain carbohydrate will require more energy than digesting a processed grain carbohydrate (chew more, gut moves more, more chemical energy needed to break things down)
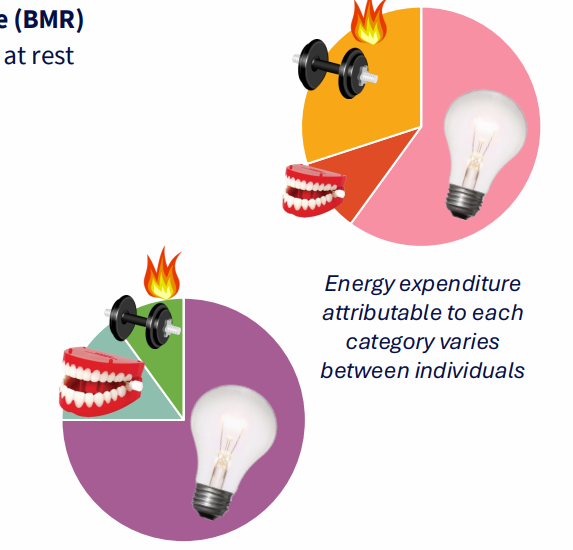
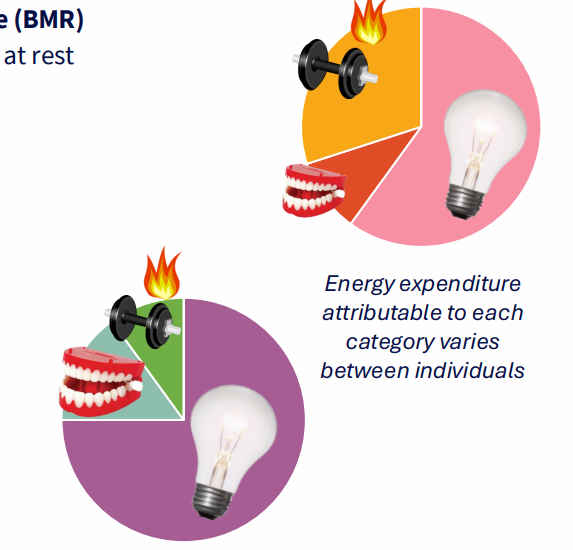
How much energy do we need?
BASAL METABOLIC LOAD (BML), OR BASAL METABOLIC RATE (BMR):
- amount of energy needed to keep body functioning at rest
- 60-75% of energy
- sometimes referred to as basal metabolic rate
.
DIET INDUCED THERMOGENESIS (DIT):
- digestion, absorption, storage
- composition effects DIT
- varies a lot between people
- 10-15%
.
EXERCISE ASSOCIATED THERMOGENESIS (EAT):
- varies a lot from person to person
.
NON-EXERCISE ACTIVITY THERMOGENESIS (NEAT):
- e.g thermoregulation. if ur in a cold place you might burn energy to keep urself warm
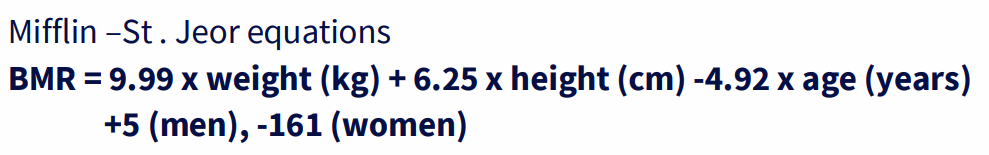
Calculating Basal Metabolic Load
- BMR = 9.99 x weight (kg) + 6.25 x height (cm) -4.92 x age (years) + 5 (men), -161 (women)
.
THE VALUE GIVEN by this equation is an approximation, and is less accurate for:
- obese subjects
- non-white ethnic groups
- and certain age groups (elderly)
.
NB: full equation is not examinable, but you should know what factors affect BMR
- if youre a larger person you need more energy to keep everything going, which is why hgiher mass or height gives higher BMR
Basal Metabolic Load is variable between individuals
- Average BMR: 1500kCal/day (around 6820kJ/day)
- Range: 1280-2500kCal/day (5395-10467 kJ/day)
- individuals with more fat-free muscle mass will have higher BML
- adipose (fat) tissue will also increase BML, but muscle has a much larger effect/kg
- age also affects BML - older people have lower BML
Non-Exercise Activity Thermogenesis
- NEAT is energy expenditure while: sitting, standing, moving (but not exercise)
- important to note: cumulative impact of low intensity activities may have a larger energetic impact then "exercise"
.
ADAPTIVE THERMOGENESIS:
- NEAT decreases during states of negative energy balance
- in overfeeding, the amount of energy stored is less then the excess consumed. This is partially due to NEAT increasing in this circumstance
.
- NEAT therefore has an important role in weight regulation
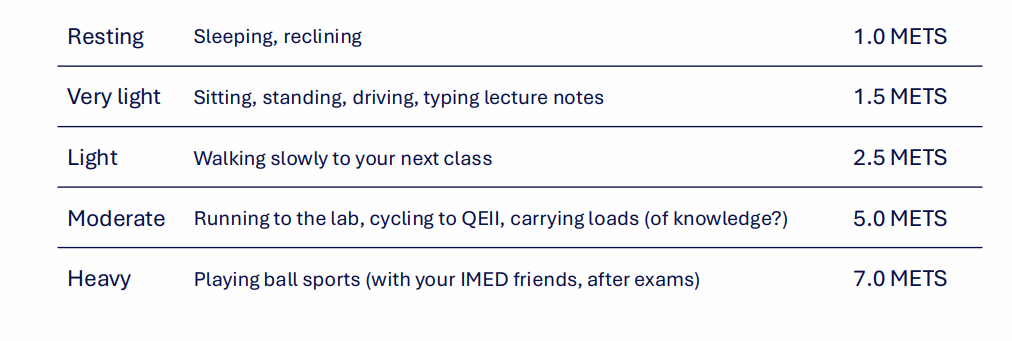
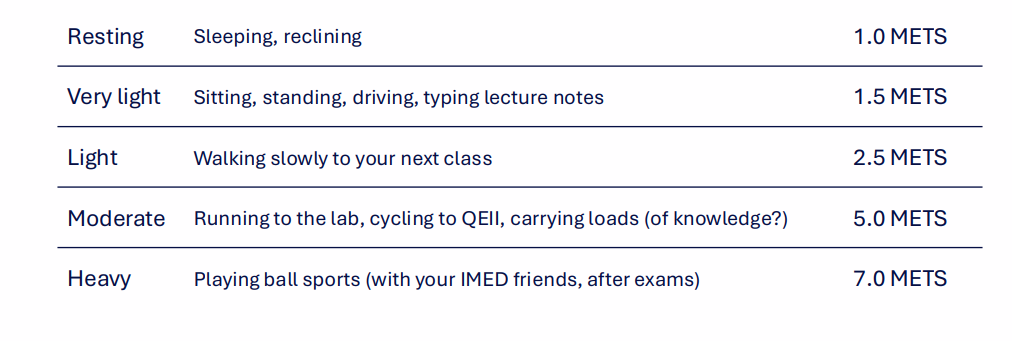
Calculating Energy used in activity
- the units for energy used in exercise are: METS - "metabolic equivalents"
- Assume that at rest, we use 1.2kcal/min for a 70kg person (rest is when activity is negligible - laying down, sitting quietly)
- 2 METS = an activity requiring twice the amount of energy consumed at rest
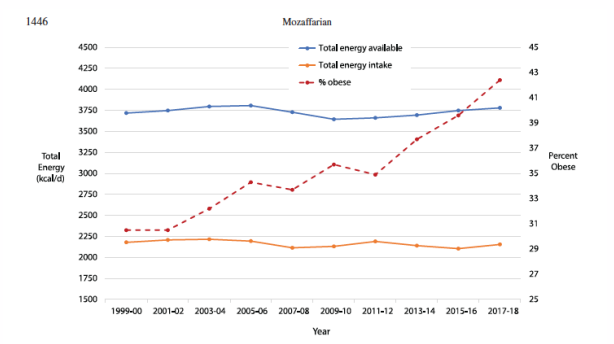
Addressing the "Obesity Epidemic"
GUIDELINE 1:
- to achieve and maintain a healthy weight, be physically active and choose amounts of nutritious food and drinks to meet your energy levels
- In Australia, the dietary guidlines are addressing the fact that the weight of Australians is increasing - and that this is because there is an excess of energy consumed beyond the energy requirements
- The advice is very simple, and everywhere in our culture - so why doesn't it work?
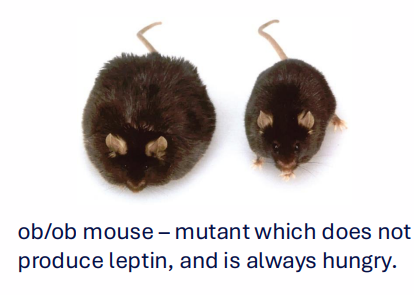
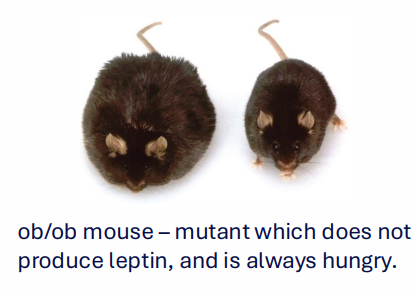
Why do we feel hungry
HORMONAL PEPTIDES SIGNAL IN RESPONSE TO FEEDING, STORED ENERGY
- Leptin: increases with adipose stores, reduces hunger
- PYY: increases after a meal, suppresses hunger
- Glucagon-like peptide 1 (GLP1): increases during, after meal, suppresses hunger
- Ghrelin: increases between meals, increases hunger
.
- these hormonal signals are released by GI tract, fat cells - and target the brain
- some individuals: signalling pathways are disrupted
- Neural signals: dietension of the GI tract triggers vagal afferent signal
- recall: fibre is important in satiety
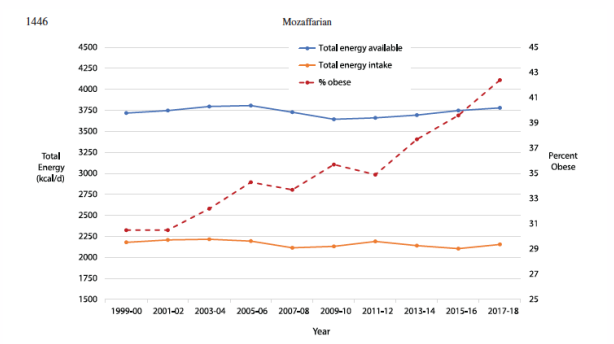
Addressing Obesity is an actively researched topic
- there my be more to this story - what can we do other then telling people to exercise more, eat less
- obesity epidemic cannot be explained by dietary habits along
- emerging role of "obesogens" - chemical pollutants which mimic hormonal signals related to satiety, hunger and metablic regulation