Excretory System Extended Response - Yr 11 ATAR
1/61
Earn XP
Description and Tags
Chapter 7
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
62 Terms
What does the excretory system do?
. regulates the chemical composition of body fluids by removing metabolic wastes + regulating water, salts and nutrients
What does the excretory system aim to do?
. rid the body of waste products that accumulate as a result of cellular metabolism
What system does the major task of excretion belong to?
. The Urinary system
—> if it fails, other organs cannot take over + compensate adequately
—> Reason: the Kidneys maintain the constant concentration of materials in the body fluids, removing nitrogenous wastes like urea, uric acid, and creatinine
Apart from the Kidneys, what other organs contribute to the excretory function?
Lungs: in the respiratory system excrete some waste products (CO2 + H2O)
Sweat glands: in skin secrete sweat, which largely contains salts, urea, lactic acid
Liver: processes many substances that body can’t excrete
Describe the structure of the Urinary System?
. consists of specialised structures + capillary networks that assist in the excretory process
. includes the kidney + its functional unit, the nephron
Describe the function of the Urinary System
. to remove waste from the human body in the form of urine
—> during this process, animals get rid of nitrogenous waste products of metabolism, including ammonia, urea and uric acid
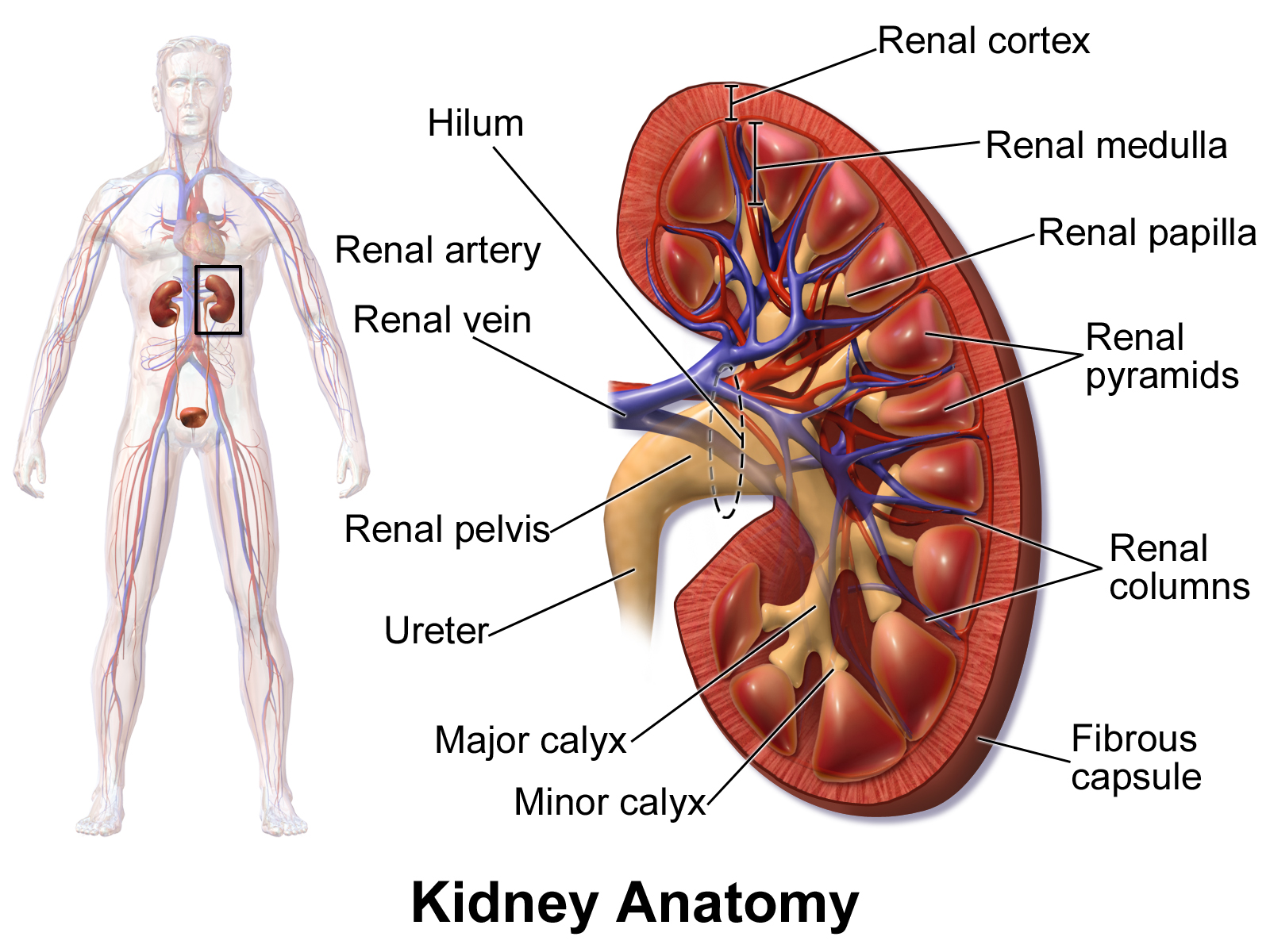
Describe the path blood follows through the Kidney to be excreted outside of the body as urine
. the kidneys are a pair of reddish-brown organs located in the abdomen
—> blood enters the kidneys through renal arteries (oxygenated blood) + leaves through renal veins (deoxygenated blood)
—> tubes called ureters carry waste products from the kidneys to the urinary bladder for storage or release
—> during urination, urine is expelled from the urinary bladder through the urethra
Describe the 7 general structures/regions in the kidney’s anatomy
Renal capsule: fibrous membrane that encloses kidney
Cortex: outer protective portion
Medulla: inner soft portion
Pyramids: located in the medulla
Columns: separated by the pyramids, blood vessels lie
Renal Pelvis: sits in the concave side of the kidney
Hilum: Lies on the concave side of kidney, blood vessels enter and leave
Describe the Ureters
. a tube 6-7 inches long attached to each kidney
. Peristalsis, a rhythmic contraction of the ureter smooth muscle helps to move the urine into the bladder
Describe the Urinary Bladder
. hollow, muscular organ that stores urine
. holds 300-400mL of urine (normal capacity) before emptying - max capacity = 500-700mL
. walls contain epithelial tissue that stretch to allow the bladder to hold twice its capacity
Describe the Urethra
. a tube of smooth muscle that carries urine from the bladder to the outside of the body
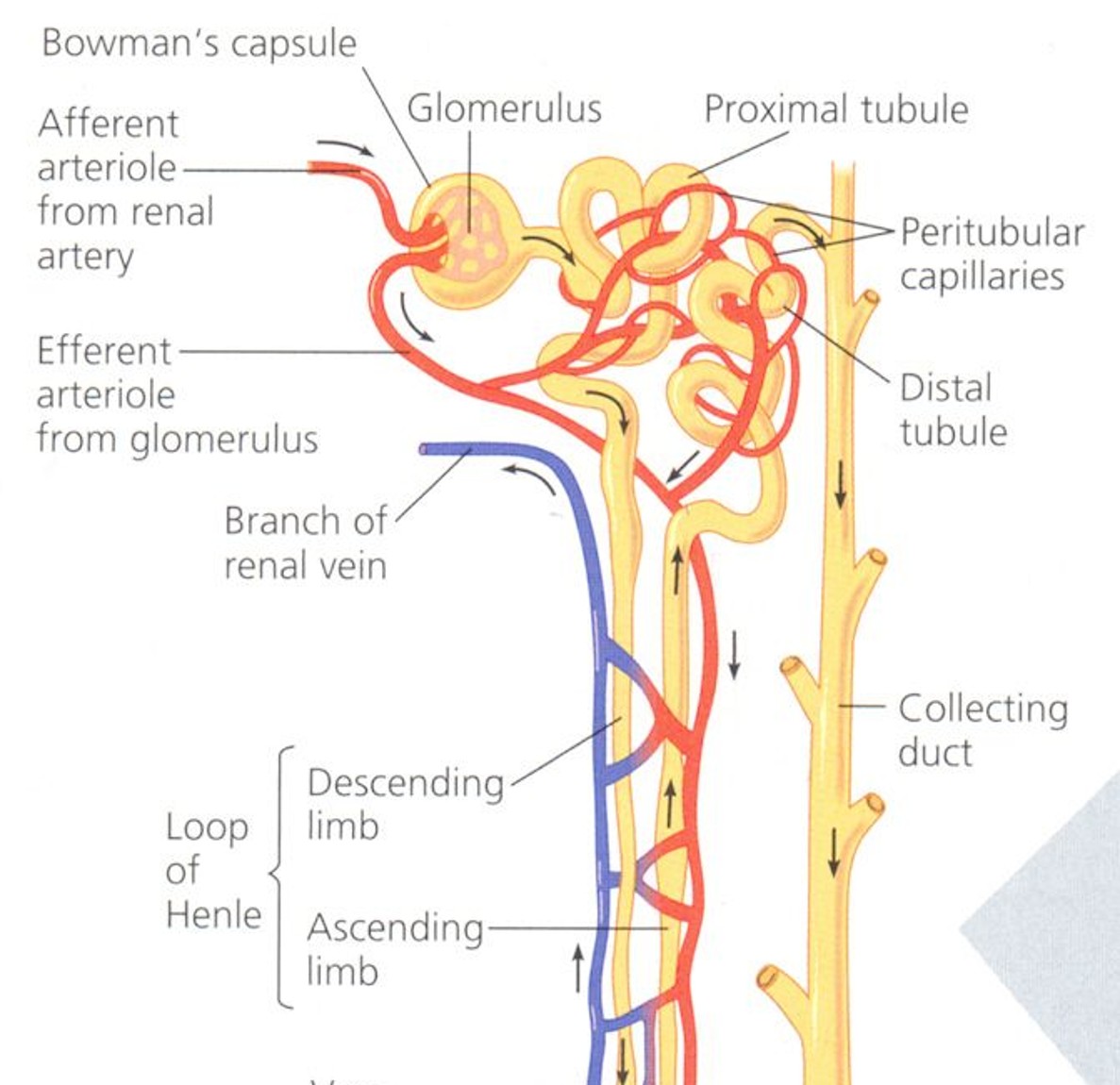
What are nephrons and where are they located?
. the functional units of the kidney
. located in the renal cortex (renal corpuscle, PCT, DCT), except for their loops of Henle + collecting ducts, which descend into the renal medulla
Describe the 2 parts of the kidney and the function of their structures
Renal corpuscle:
—> Bowman’s capsule: double-walled, cup-shaped structure that surrounds the glomerulus, collects the filtered fluid (filtrate) and directing it towards the proximal convoluted tubule for further processing
—> Glomerulus: mass of thin-walled (suited for diffusion) capillaries, filters blood, allowing smaller molecules, waste, and fluid to pass into the tubule, while larger molecules like proteins and blood cells remain in the capillaries.
Renal Tubule
—> Proximal convoluted tubule: leads from the Bowman’s capsule to the Loop of Henle, reabsorbs some water, essential ions, nearly all glucose + amino acids, but no urea + actively secretes ammonia into the tubular fluid for excretion in urine
—> Loop of Henle: a long loop which extends into the medulla, reabsorbs water and sodium chloride from the filtrate, conserving water and enabling the production of highly concentrated urine
—> Distal Convoluted Tubule: connects loop of Henle to the collecting duct, active reabsoprtion of sodium ions + water (depending on body’s water needs), secretion of H + K ions, creatinine and certain drugs (penicillin)
Nephron Fully Labelled
Skin Role in excretion
. sweat glands are located in the lower layers of the skin
. a duct carries the sweat to a hair follicle or skin surface where it opens at a pore
. cells surrounding the gland contract to squeeze sweat to the skin surface
. sweat glands secrete 500mL of water/day
. dissolved in the water is sodium chloride, lactic acid and urea
Liver: Proteins to Carbohydrates for Energy 4 steps
Proteins are broken down in digestion to amino acids
These can be built back up into proteins that form cell structures, enzymes and antibodies
Excess protein from the diet cannot be stored in cells, so processes are required to remove it from the body
Protein can be converted into carbohydrates for storage or energy
Liver Role in Excretion
. Preparation of materials for excretion, processing chemicals into a safer form
Protein excretion:
—> excess protein from the diet can’t be stored in cells, so processes are required to remove it from body
—> Worn out RBCs broken down into the constituent amino acids, most used to make new proteins but some lost from body via the urine, skin, hair and fingernails
—> if other energy sources have been used up, body able to metabolism large amounts of proteins, breaking them down to produce energy through deamination
Detoxifies alcohol + many other drugs (eg antibiotics)
Deactivates many hormones + converts them into a form that can be excreted by the kidneys
Breaks down haemoglobin from dead RBCs to produce bile pigments, which are then passed out of the body with the faeces
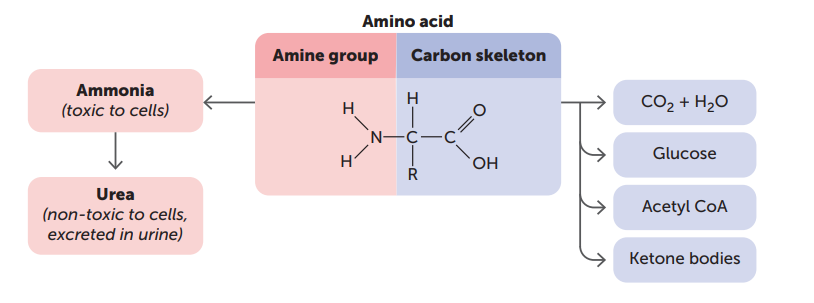
Describe the 4 steps in Deamination, including word equations
. the process whereby nitrogen/amino group (amino=NH2) is removed from the amino acid molecule
Amino group is removed from the amino acid (occurs in liver with aid of enzymes)
This is converted to ammonia by the liver cells (highly toxic to cells):
Amino acid + oxygen —>(enzymes)—>ammonia + carbohydrate
Ammonia combines with carbon dioxide to produce urea (less toxic) and water:
Energy + carbon dioxide + ammonia —> Urea + water
Urea is excreted in urine and sweat, and the remaining amino acid is converted into a carbohydrate (=energy)
What are the 3 major processes in the formation of urine by the nephrons?
Glomerular Filtration
Selective Reabsorption
Secretion by the tubules
Describe where Glomerular Filtration (GF) takes place and the 4 main steps to its process
. takes place in the renal corpuscle
Fluid is forced out of the blood + is collected in the glomerular capsule (GC)
—> process is enhanced by the high pressure of blood in the glomerulus due to larger diameter of the afferent arteriole compared to the efferent arteriole
The blood in the glomerulus is separated from the GC by 2 layers of thin cells:
—> One layer makes up capillary wall and other the wall of the capsule
Thus, when blood enters glomerulus, high pressure forces water + dissolved blood components through differentially permeable cell membranes + into the capsule
—> resulting fluid = filtrate (in healthy, consists of all materials present in blood except RBCs + WBCs + plasma proteins, as too large to pass through differentially permeable membranes—> consists of water, salts, amino acids, fatty acids, glucose, urea, uric acid, creatinine, hormones, toxins and various ions)
As blood flows through the capillaries of the glomerulus, only 20% of the plasma is filtered through the capillary walls into GC (due to the speed the blood passes through glomerulus, prevents all plasma moving through capillary walls, AS blood in capillaries continually being pushed on by the blood behind it)
—> equates to 125mL of filtrate per min (180L/day)
—> As 1.2 million nephrons/kidney, large amount of plasma is filtered, but only 1% leaves the body as urine, most is reabsorbed back into the blood
Describe what the filtrate produced from the nephrons contains
. contains all materials in the blood except red + white blood cells + plasma proteins
—> includes: water, salts, amino acids, fatty acids, glucose, urea, uric acid, creatinine (product of muscle metabolism), hormones, toxins, various ions
Describe the process of selective reabsorption in the nephron
. some of the filtrate is useful to the body and thus selective reabsorption of the filtrate takes place so materials that are needed aren’t excreted from body
—> returns them to the blood in the peritubular capillaries
. carried out by cells that line the renal tubule
. Reabsorbed materials include
—> water, glucose, amino acids
—> some ions (Na, K, Ca, Cl, HCO3)
—> some wastes partially reabsorbed (eg urea)
. a large SA is required to exchange materials, achieved as:
The nephrons have a long length of kidney tubule (2 sets of convolutions + loop of Henle)
there are a large number of nephrons in each kidney
Describe the process of reabsorption of water in the nephron
. reabsorption of the water component of the filtrate can be regulated depending on the body’s water requirements
—> the permeability of the plasma membranes of the cells making up parts of the tubule can be changed, thus more or less water can be reabsorbed
—> is an active process controlled by hormones (ADH: anti-diuretic hormone) released by the hypothalamus = facultative reabsorption
Describe the process of tubular secretion
. opposite to selective reabsorption (removes substances from filtrate into blood), tubular secretion ADDS materials to the FILTRATE from the blood
—> materials secreted include: potassium + hydrogen ions, creatinine, and drugs (eg penicillin)
—> can be either active or passive, has 2 main effects:
It maintains the blood pH
—> body needs to maintain the blood within its normal pH range of 7.4-7.5
—> diets usually contain many acid-producing foods that tend to lower pH, THUS kidneys must remove the excess hydrogen + ammonium ions
It maintains the urine pH
—> the presence of hydrogen + ammonium ions in urine makes urine slightly acidic, with a normal pH of 6
Describe the urine formation that occurs after glomerular filtration, selective reabsorption and secretion by the tubules takes place
. water + other substances that aren’t reabsorbed back into the blood, drain from the collecting ducts into the renal pelvis
—> from pelvis, the urine then drains into ureters + is pushed by muscular contractions to the bladder
—> urine is then carried from bladder by the urethra to the exterior of the body
Describe Urine composition
. half a L of water must be lost each day to excrete water-soluble wastes (eg, urea, sulfates, phosphates)
. when water content in body fluids is low, urine is concentrated
Under normal conditions:
99% of water that enters nephron is reabsorbed
Urine doesn’t usually contain significant amounts of protein
Urine doesn’t usually contain any glucose
Main materials in urine: urea, ions, uric acids, and creatinine
. Healthy adult usually passes 1.5L of urine/day but can vary enormously depending on a range of factors
Describe how the structure of the kidney is suited to its function
. structure of kidney is related to its function of excretion of waste + regulation of water content:
the GC surrounds the glomerulus to collect fluid filtered out of the blood capillaries
Afferent arteriole has larger diameter than efferent arteriole = an increased blood pressure in the afferent arteriole so more fluid is filtered out of the blood
Tubule has 2 sets of convolutions + a long loop increasing SA for reabsorption
1.2 million nephrons/kidney = total SA available for reabsorption + excretion is extremely large
Briefly list and describe the 4 organs of excretion and what they excrete
Lungs: water, volatiles like ethanol, CO2
Skin: sweat (water, salts, urea)
Kidneys: urine (water, drugs, salts, urea, uric acid)
Liver: bile pigments, fat-soluble drugs and substrates
Describe the general process of urine formation
. as blood enters the nephron through the arteriole, impurities are filtered out + emptied into the collecting duct
—> the purified blood exits the nephron through the venule
—> the mechanism of blood purification involves 3 processes:
Filtration: mainly in the glomerulus, fluid from blood flows into Bowman’s capsule, materials filtered from blood = water, urea, glucose, salts, amino acids, some vitamins - plasma proteins, cells, platelets remain in blood as too large to pass through capillary walls
Reabsorption: most of material removed from blood at Bowman’s capsule reabsorbed into blood, process of returning nutrients back into blood vessel
Secretion: adds materials to the filtrate from the blood, including potassium + hydrogen ions, creatinine and drugs (penicillin). Removal of potassium + hydrogen ions to the urine, maintains the blood pH within normal range
Outline what the features of Urine are
. is the remaining material after filtration, reabsorption and secretion
. is emptied into a collecting duct
. is primarily concentrated in the loop of henle
—> loop of Henle is a section of the nephron tubule in which water is conserved + volume of urine is minimised
. as kidney works, purified blood is returned to circulation while urine is collected in the urinary bladder
How can lifestyle choices have an impact on the effectiveness of excretion in a human?
Lifestyle choices such as being active or sedentary, diet, alcohol consumption, water intake and drugs can lead to damage to the kidneys and liver, having an impact on the effectiveness of excretion.
What are kidney stones?
. a hard mass of crystals that can form in the kidney, ureters, bladder or urethra
Kidney Stones formation
. From solid crystals that build up inside the kidneys
. Form when urine becomes too concentrated
. Crystals may combine to form stones
. urine contains compounds consisting of calcium, sodium, potassium, oxalate, uric acid and phosphate
—> if levels of these particles get too high or if urine becomes too acidic/basic, particles can clump together + crystallise
—> over weeks, months, years, crystals grow into detectable stones
Kidney stones Causation
Insufficient fluids in the diet
Kidney Stones: How do smaller stones/crystals pass?
. If crystals are small enough, they may pass down the ureter + out of the body through the urethra without being noticed
. While painful, may pass with the aid of fluids, pain relief and muscle relaxants
Kidney Stones: How do larger stones pass and how can doctors pass them?
. May get stuck in the ureter, bladder or urethra, causing INTENSE PAIN
. May need to be broken up with sound waves or physically removed during surgery
Kidney Stones Symptoms and detection
. kidney stone may go undetected until it starts to move
. as it travels through the kidney and into the ureter, its sharp edges scratch the walls of the urinary tract, causing:
. excruciating pain, blood in urine, nausea, vomiting, burning sensation during urination
. if stone blocks the flow of urine, can lead to infection or kidney damage
Treatment options for Smaller kidney stones
. stones less than 5mm in diameter usually pass on their own
—> drink large amounts of water + take painkillers
Treatment options for Medium size stones
. stones up to 10mm:
Alpha blockers: relax muscles in ureter, making it easier for stone to pass
Potassium citrate: dissolves stones by making urine less acidic
Extracorporeal shock wave lithotripsy: uses high-intensity sound waves to pulverize stones into smaller pieces that can pass more easily
Treatment options for larger Kidney stones
Stent placement to expand ureter
Laser pulses to break up stone (by optical fibres)
surgical removal through incision in back/groin
3 ways to prevent the formation of Kidney stones
Drinking plenty of water to dilute calcium oxalate + other compounds that build up
Limiting foods high in oxalate (potato chips, spinach, rhubarb, beets)
Consuming calcium rich foods + beverages to bind to oxalate in the digestive tract (before it can be absorbed + reach the kidneys)
Describe calcium oxalate and struvite stones?
. Calcium oxalate: most common type, 80% of stones
—> less common stones = made of calcium phosphate + uric acid
Struvite Stones: composed of magnesium ammonium phosphate, can be caused by bacterial infection
What may rare kidney stones result from
. genetic disorders or certain medications
Kidney Failure: 2 general facts
. 1 in 3 adult Australians is at risk of developing kidney disease
. A person can lose up to 90% of kidney function without realising it (by that stage it's almost impossible to prevent serious problems occurring)
Kidney disease described (where + what happens)
. Most kidney diseases affect the glomeruli, reducing their ability to filter the blood
. Protein and sometimes RBCs may leave the blood at the glomerulus + will then be present in the urine
. If excessive proteins are lost in the urine, blood protein levels fall + fluid accumulates in the tissues, causing swelling of the hands, feet, face or other areas
Kidney disease treatment
. mild kidney disease = medication
What are 5 lifestyle measures to maintain healthy kidneys?
Regulate diet to maintain a healthy weight: being overweight can lead to the development of diabetes or high blood pressure, which are major risk factors for kidney disease
Do NOT smoke: compared with non-smokers, people who smoke are 3x more likely to have impaired kidney function
Drink water instead of drinks containing sugar
Drink alcohol in moderation: 1 standard drink/day for women and 2/day for men
Do NOT use performance-enhancing drugs: as they may upset the water balance in the body – in particular, anabolic steroids can cause scarring inside the kidneys + eventual kidney failure
What is Kidney Failure? (when can it develop, what factors contribute, treatment)
. When the kidneys lose their ability to excrete waste + to control the level of fluid in the body on their own
. May happen suddenly, BUT is more likely to develop over a period of years
. Factors such as diabetes, high blood pressure or kidney diseases slowly destroy the nephrons in the kidneys
. Eventually, the only way to maintain life is by DIALYSIS or a KIDNEY TRANSPLANT
2 main consequences of Kidney Failure
waste substances build up in the bloodstream
unable to regulate water + ion levels
—> patient becomes sick + if untreated, could lead to death
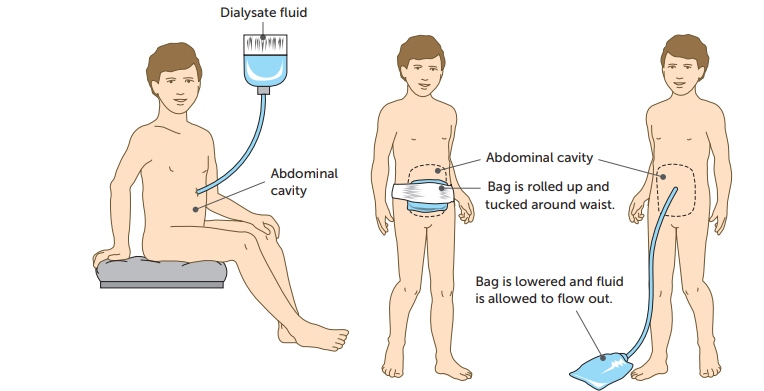
What is dialysis?
. A method of removing wastes from the blood when kidney failure occurs
. 2 types = peritoneal dialysis and haemodialysis
What is the Peritoneum and what does it have?
. A membrane that lines the inside of the abdominal cavity + covers abdominal organs such as the stomach, liver and intestines
. Has a very rich blood supply
Describe Peritoneal Dialysis: where occurs, how often done, outline the 6 steps
. Occurs inside the body using the peritoneum as a membrane across which waste can be removed
. Usually done each day
A tube (catheter) is placed through the wall of the abdomen
For an adult, 2-3L of fluid are passed through the catheter into the abdominal cavity
The fluid contains glucose + other substances at concentrations similar to those found in the blood, however there are no wastes in the fluid
Thus, because of the concentration difference, wastes will diffuse out of the blood into the fluid in the abdominal cavity
Useful substances stay in the blood because there's no concentration difference between the blood and the fluid
After a time, the fluid that was placed in the abdominal cavity is drained out through the catheter, along with any wastes + extra water that have diffused from the blood
What is Haemodialysis? (what involves, how often for how long, outline the 3 steps)
. Involves passing the blood through an artificial kidney or dialysis machine that filter a patient’s blood
. Patients spend 4-5hrs attached to the machine + dialysis is normally done 3 times/week
The blood passes through thousands of fine tubes, made of a differentially permeable membrane, and immersed in a bath of fluid
The concentrations of substances in the fluid are similar to those in the blood, except the fluid has no waste
Because of the concentration differences, wastes diffuse from the blood into the fluid
—> Brings patient’s blood levels back down to normal
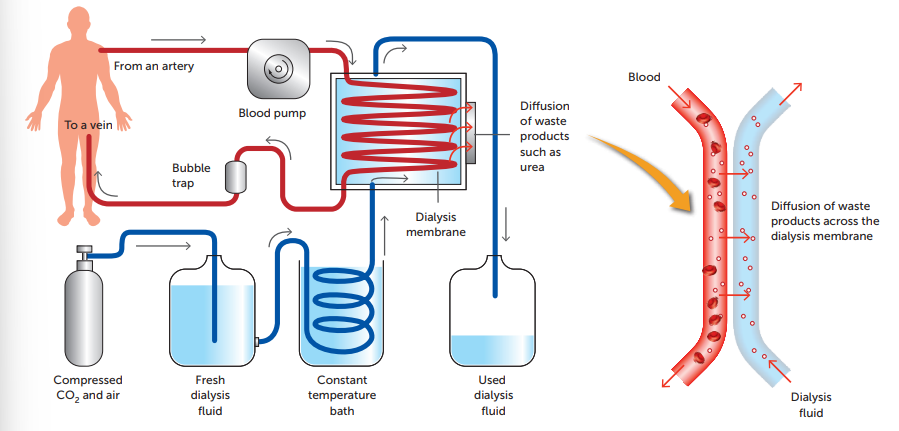
Issue with Haemodialysis and how this is solved
. after a while, the incoming blood and dialysis fluid would reach equilibrium, thus nothing would diffuse
—> Prevention: dialysis fluid is constantly replaced with new fluid being pumped in from the bottom + older fluid passing out of the top
—> means there’s always a concentration gradient so patient looses all the waste materials in their blood
Dialysis Problems in General
. time consuming
. unpleasant experience
. can cause blood clots + infection
. very expensive to run
. people have to have it continually for the rest of their life
Alternative to Dialysis: What is a Kidney Transplant
. a surgical procedure where a healthy kidney from one person is transferred to a patient that needs it
Where do donor kidneys come from?
. most donor kidneys come from people who have recently died, BUT living donors can also donate (as humans are born with 2 but can live perfectly well with 1)
What is one minor risk and one major risk of a kidney transplant?
Minor: small risk that something will go wrong in surgery
Major: Organ will be rejected
—> rejection: when a transplanted organ is attacked by patient’s immune system, treating organ as a foreign object to destroy
—> doctors help prevent this by administering medication to suppress patient’s immune system (but doesn’t always work)
Are kidney transplants or dialysis more preferable for Kidney Failure Patients?
. Transplants tend to be better + much cheaper than dialysis, BUT there’s not enough available organs to give all patients a transplant, thus many have to rely on dialysis
Liver disease: effects
. When the liver is not able to function effectively, it's unable to process toxins ready for elimination
Liver disease: causes
. Infection, autoimmune problems, genetic disorders, cancer, and lifestyle factors such as excessive alcohol consumption + a fatty diet
Liver disease: Symptoms (why shown + include what)
. Shown due to a build up of the toxins that would normally be eliminated
. Include: a yellow tinge to the skin (jaundice), abdominal pain + swelling, swelling in the legs + feet, nausea or vomiting, fatigue, dark urine, faeces that are pale or dark coloured