Anatomy and Physiology II - Section 4, Lesson 3
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
Q: What is the primary function of the ureters?
A: The ureters drain urine from the renal pelvis into the urinary bladder.
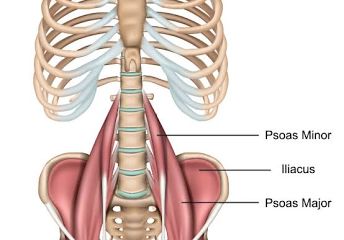
Q: Where do the ureters descend along in the body?
A: The ureters descend on the surface of the psoas major muscle, behind the ovarian or testicular vessels, and along the lateral wall of the pelvis.
Q: What is the role of peristalsis in the ureters?
A: Peristalsis moves urine from the renal pelvis to the urinary bladder, rather than relying on gravity.
Q: What causes the one-way valve effect at the entry of the ureters into the bladder?
A: The oblique course of the ureters through the bladder wall creates a physiological sphincter, preventing urine reflux.
Q: What is vesicoureteral reflux and when is it most likely to occur?
A: Vesicoureteral reflux is the backward flow of urine from the bladder into the ureters, which can occur in children born lacking the oblique ureteral course or during pregnancy.
Q: How long are the ureters, and what is their inner mucosa lined with?
A: The ureters are approximately 30 cm long and have an inner mucosa lined with transitional epithelium and goblet cells that secrete protective mucus.
Q: What is the structure of the muscular layer of the ureter?
A: The muscular layer consists of longitudinal and circular smooth muscles that create peristaltic contractions to move urine.
Q: What is the role of the adventitial layer of the ureter?
A: The adventitial layer anchors the ureters between the parietal peritoneum and the posterior abdominal wall with collagen and fat.
Q: What is the renal pelvis?
A: The renal pelvis is the area at the center of the kidney where urine collects and is funneled into the ureter.
Q: What is the difference between a physiological sphincter and an anatomical sphincter?
A: A physiological sphincter is a smooth muscle with differential innervation that functions as a sphincter, while an anatomical sphincter is a muscle surrounding the lumen that can restrict flow when contracted.
Q: What is the renal pelvis?
A: The renal pelvis is the area at the center of the kidney where urine collects and is funneled into the ureter.
Q: What is the urinary bladder?
A: The urinary bladder is a temporary storage reservoir for urine located in the pelvic cavity.
What are the layers of the ureter?
Adventitia, two muscular layers, and two transitional epithelium.
Two adventitia, two muscular layers, and a transitional epithelium
Adventitia, one muscular layer, and a transitional epithelium
Adventitia, two muscular layers, and a transitional epithelium
Adventitia, two muscular layers, and a transitional epithelium
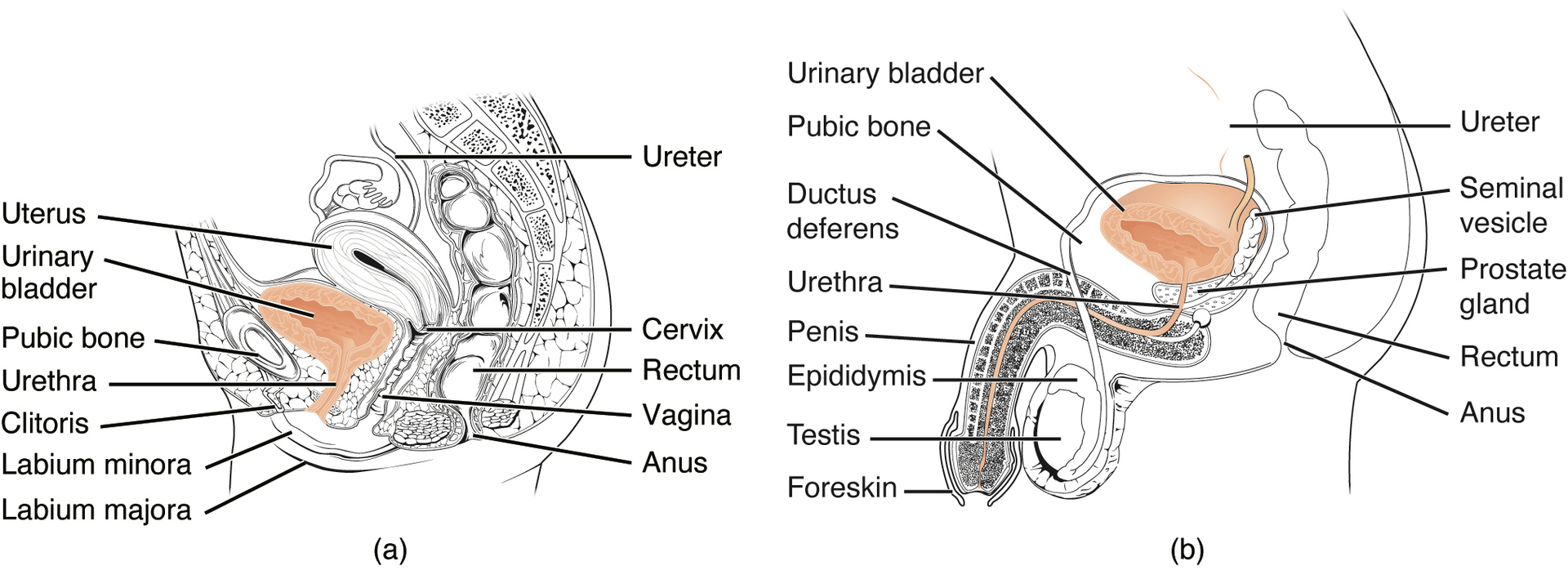
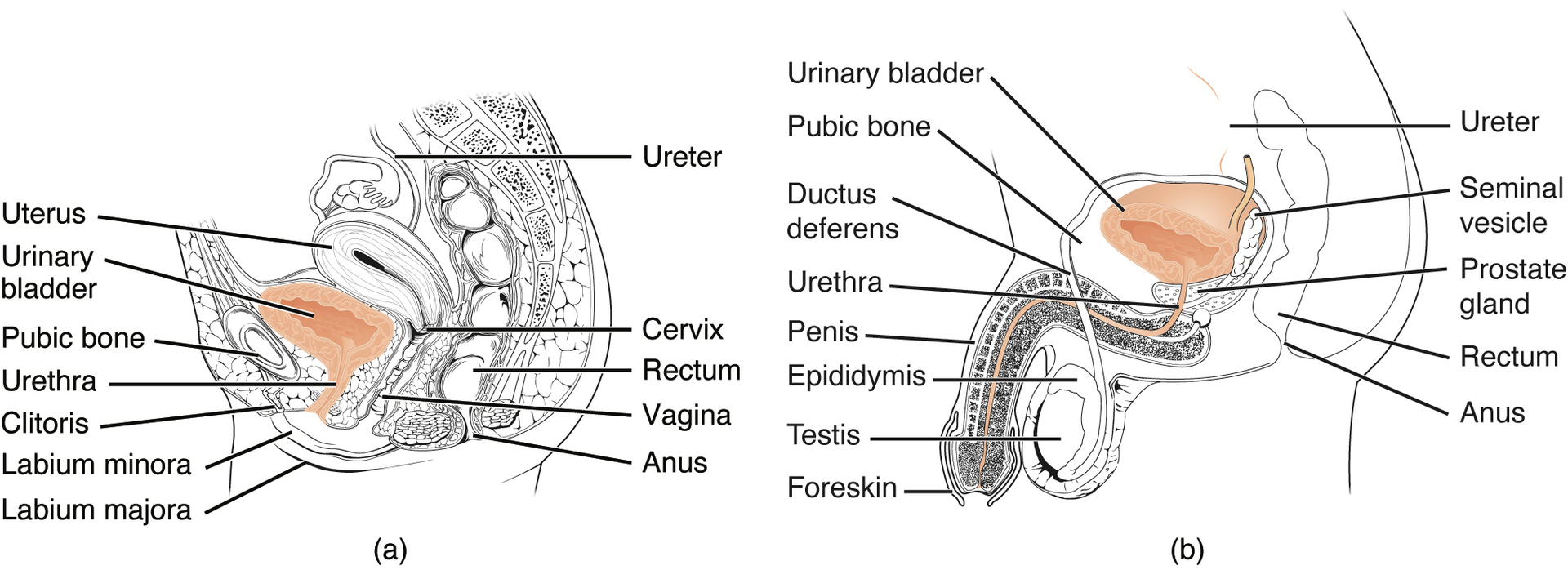
Q: Where does the urinary bladder lie in females and males?
A: In females, the urinary bladder lies anterior to the uterus, posterior to the pubic bone, and anterior to the rectum. In males, it lies similar but with the addition of the prostate inferior to the bladder.
Q: How does the capacity of the urinary bladder change during late pregnancy?
A: During late pregnancy, the bladder's capacity is reduced due to compression by the enlarging uterus, leading to an increased frequency of urination.
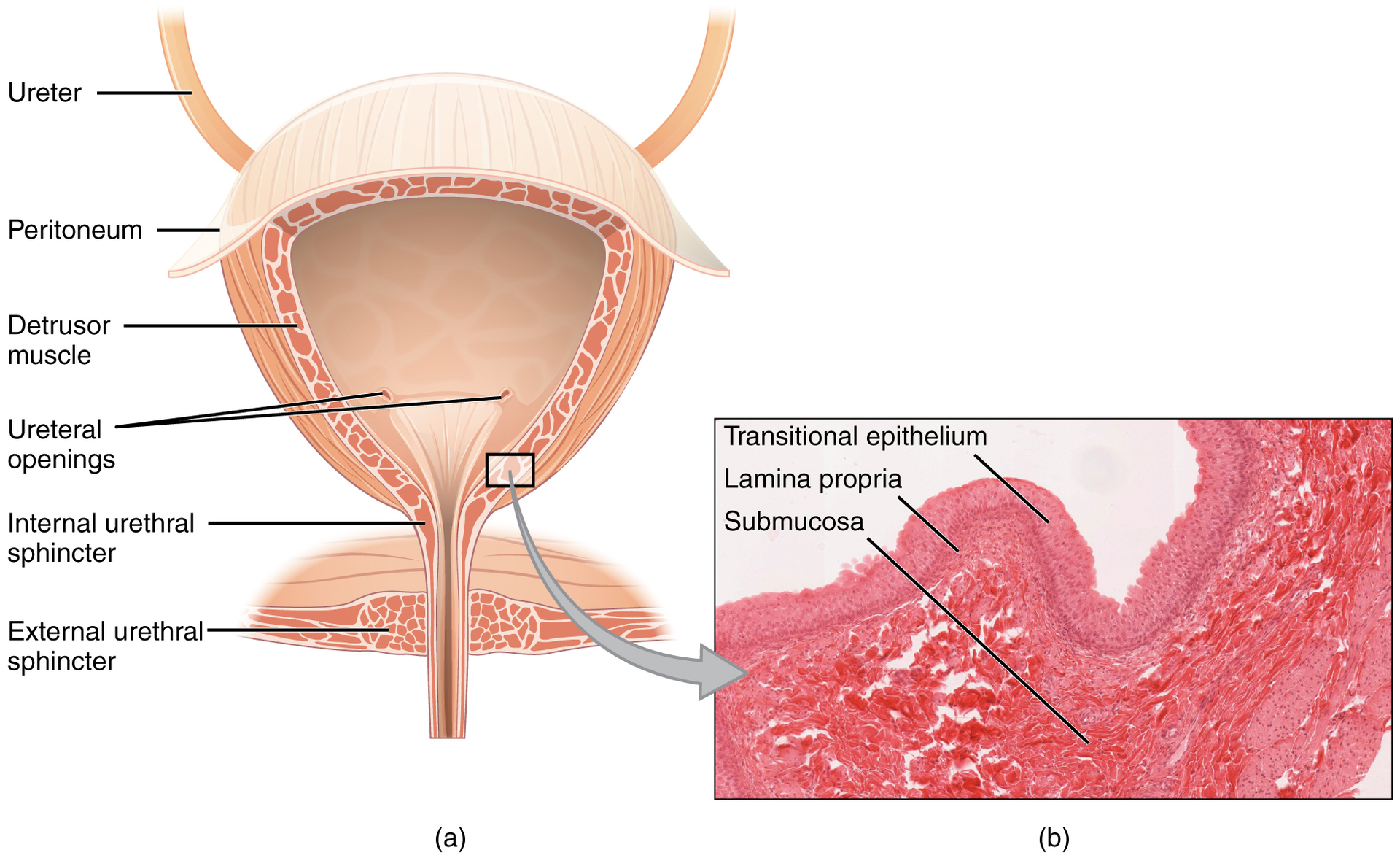
Q: What is the detrusor muscle in the urinary bladder?
A: The detrusor muscle is a crisscrossing band of smooth muscle in the bladder that contracts to expel urine.
Q: How does the internal surface of the urinary bladder change as it fills?
A: When the bladder is empty, the internal surface forms folds (rugae). As it fills, the surface stretches and transitions from columnar epithelium to squamous epithelium.
Q: What is the trigone in the urinary bladder?
A: The trigone is a triangular region in the bladder formed by the points of entry of the ureters and the internal urethral orifice. It remains smooth and rigid to avoid damaging the ducts.
Q: How much urine can the urinary bladder hold?
A: The urinary bladder can hold up to approximately 500-600 mL of urine, but it may feel full with only 250-300 mL.
Q: What does "retroperitoneal" mean in relation to the kidneys and ureters?
A: Retroperitoneal means located behind the peritoneum, in the case of the kidneys and ureters, between the parietal peritoneum and the abdominal wall.
Flashcard 2:
Q: What is the detrusor muscle?
A: The detrusor muscle is the smooth muscle found in the wall of the bladder that contracts to help expel urine.
Q: What are rugae?
A: Rugae are a series of ridges produced by the folding of the wall of an organ, such as the urinary bladder.
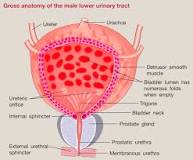
Q: What is the trigone in the urinary bladder?
A: The trigone is a smooth, triangular region in the bladder formed by the two ureteric orifices and the internal urethral orifice.
Q: What is the function of the urethra?
A: The urethra transports urine from the bladder to the outside of the body for disposal.
Q: What is the trigone?
A: The trigone is a smooth triangular region in the bladder formed by the two ureteric orifices and the internal urethral orifice.
Q: What is the difference between the female and male urethra?
A: The main difference is the length; the female urethra is about 4 cm long, while the male urethra averages 20 cm and passes through the prostate and penis.
Q: What type of epithelium lines the proximal urethra in both males and females?
A: The proximal urethra in both males and females is lined by transitional epithelium.
Q: What is the function of the internal and external urethral sphincters?
A: The internal urethral sphincter, controlled by the autonomic nervous system, is involuntary, while the external sphincter, controlled by the pudendal nerve, is voluntary and helps regulate urine flow.
Q: Where is the external urethral orifice located in females?
A: The external urethral orifice is embedded in the anterior vaginal wall, inferior to the clitoris, and superior to the vaginal opening.
Q: Why do females have a higher incidence of urinary tract infections (UTIs) than males?
A: The shorter length of the female urethra makes it easier for fecal bacteria to reach the bladder.
Q: What regions does the male urethra pass through?
A: The male urethra passes through the preprostatic, prostatic, membranous, and spongy (penile) regions.
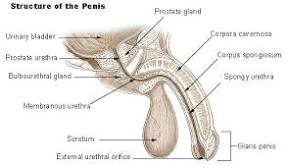
Q: What is the role of Cowper’s (bulbourethral) glands in the male urethra?
A: They produce and secrete mucus into the urethra to neutralize its pH and lubricate it during sexual stimulation.
Q: Which portion of the male urethra provides an outlet for the expulsion of urine from the urinary system?
A: The spongy (penile) urethra provides an outlet for the expulsion of urine.
Q: What is the trigone?
A: The trigone is a smooth triangular region of the internal urinary bladder formed by the two ureteric orifices and the internal urethral orifice.
Q: What are urethral sphincters?
A: Urethral sphincters are two muscles used to control the exit of urine from the urinary bladder through the urethra.
Q: What is micturition?
A: Micturition is the process of urination or voiding, resulting from the interplay of involuntary and voluntary actions by the internal and external urethral sphincters.
Q: At what bladder volume does the urge to void typically occur?
A: The urge to void is typically sensed when bladder volume reaches about 150 mL.
Q: What happens as the bladder fills and reaches 300-400 mL?
A: Voluntary constraint fails, resulting in incontinence as the bladder volume approaches 300-400 mL.
Q: What triggers the micturition reflex?
A: The micturition reflex is triggered by stretch receptors in the bladder wall, which send nerve impulses to the sacral region of the spinal cord.
Q: What role do parasympathetic neural outflows play in micturition?
A: Parasympathetic neural outflows cause contraction of the detrusor muscle and relaxation of the internal urethral sphincter.
Q: How does the micturition reflex change with age and experience?
A: The micturition reflex is active in infants, but with maturity, children learn to override the reflex and gain voluntary control, often through potty training.
Q: What spinal cord and nerve functions are required for voluntary control of micturition?
A: Voluntary control of micturition requires an intact spinal cord and functional pudendal nerve arising from the sacral micturition center.
Q: What happens when the bladder volume is low (below 400 mL)?
A: The pontine storage center is activated, which enhances sympathetic innervation and inhibits parasympathetic innervation to prevent urination.
Q: What occurs when the bladder volume exceeds 400 mL?
A: The pontine micturition center is activated, causing parasympathetic fibers to stimulate the detrusor muscle to contract and the internal urethral sphincter to relax.
Q: What is the role of the external urethral sphincter in micturition?
A: The external urethral sphincter, controlled by the pudendal nerve, allows voluntary control over urination by contracting to maintain continence or relaxing to allow urine flow.
Q: What happens in Step 1 of micturition?
A: The bladder fills with urine, becoming distended, and stretch receptors in the bladder walls are activated, triggering nerve impulses.
Q: What happens in Step 2 of micturition?
A: Stretch receptors in the bladder wall send signals to the brain, triggering the urge to urinate.
Q: What happens in Step 3 of micturition?
A: Nerve impulses propagate along sensory neurons to the pons of the brainstem and higher centers in the brain, which provide conscious control of micturition.
Q: What happens in Step 4 of micturition?
A: If the bladder volume is low, the pontine storage center is activated, suppressing parasympathetic activity and enhancing sympathetic activity to inhibit urination. If the bladder volume is high (over 400 mL), the pontine micturition center is activated, allowing micturition to proceed.
Q: What happens in Step 5 of micturition?
A: The activation of the pontine micturition center excites parasympathetic fibers to the bladder and internal urethral sphincter, and inhibits sympathetic fibers. Somatic efferent signals to the external urethral sphincter are also inhibited.
Q: What happens in Step 6 of micturition?
A: Parasympathetic stimulation causes the detrusor muscle to contract, and the internal urethral sphincter to relax, allowing urine to be expelled. The inhibition of somatic efferent allows the external urethral sphincter to relax, permitting the passage of urine from the body.
What is involved in voluntary micturition?
Contraction of detrusor muscle
External urethral sphincter
Activation of parasympathetic nerves
Internal urethral sphincter
External urethral sphincter
When urine volume in the bladder is low, which center is activated, and which innervation is enhanced?
Micturition center, sympathetic
Pontine storage center, sympathetic
Micturition center, parasympathetic
Pontine storage center, parasympathetic
Pontine storage center
Term: Sacral micturition center
Definition: Group of neurons in the sacral region of the spinal cord that controls urination; acts reflexively unless its action is modified by higher brain centers to allow voluntary urination.
Term: Pontine storage center
Definition: A collection of neuronal cell bodies that help in the supraspinal regulation of micturition.
Term: Sympathetic innervation
Definition: Part of the nervous system that increases heart rate, blood pressure, breathing rate, and pupil size.
Term: Parasympathetic fibers
Definition: A type of nerve fiber of the parasympathetic nervous system.
Term: Spinal reflex
Definition: Involuntary and nearly instantaneous movement of the spine in response to a stimulus.
Voluntary constraint of micturition is overridden as bladder volume approaches which range, in mL?
50-100
100-200
200-300
300-400
300-400
Which area of the brain is activated if urine volume in the bladder is low?
Detrusor center
Pontine storage center
Urethral inhibition center
Pontine micturition center
Pontine storage center
Which part of the urinary system will initiate micturition reflux?
Kidneys
Ureters
Urinary bladder
Urethra
Urinary bladder
Which part of the urinary system is responsible for more UTI incidents in women as compared to men?
Kidney
Ureter
Bladder
Urethra
Urethra
Which structure is formed by the points of entry of each of the ureters and the internal urethral orifice?
Detrusor muscle
Trigone
Corpus spongiosum
Peritoneum
Trigone