MLP II Unit 3: Hematology
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
Erythrocytes (RBCs)
Main function is carrying oxygen from lungs to the rest of the body
Also carry CO2 back to lungs to be exhaled
Main constituent of RBCs is hemoglobin
Hemoglobin is made up of iron + protein
Hemoglobin is what carries O2 and CO2
Small, round, biconcave disk
Area of central pallor
Lifespan of about 120 days
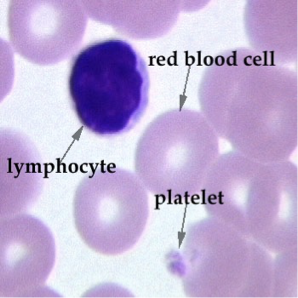
Leukocytes (WBCs)
Primary function is to protect the body against disease
5 types:
Segmented Neutrophil
Lymphocyte (T & B cells)
Monocyte
Eosinophil
Basophil
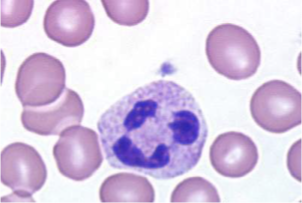
Segmented Neutrophils
Make up large percentage of WBCs in the body
Main function is phagocytosis — eating foreign pathogens
Can migrate to the tissues to eat pathogens
Increase in these cells on a differential indicates bacterial infection
Eosinophils
Pink/red on blood smear
Primary function is to protect against allergic reactions and parasitic infections
Basophils
Have dark purple granules that contain heparin and histamine
Involved in allergic/anaphylactic reactions — granules release heparin & histamine which causes smooth muscle contraction, vasodilation, edema, bronchospasms in anaphylactic reactions
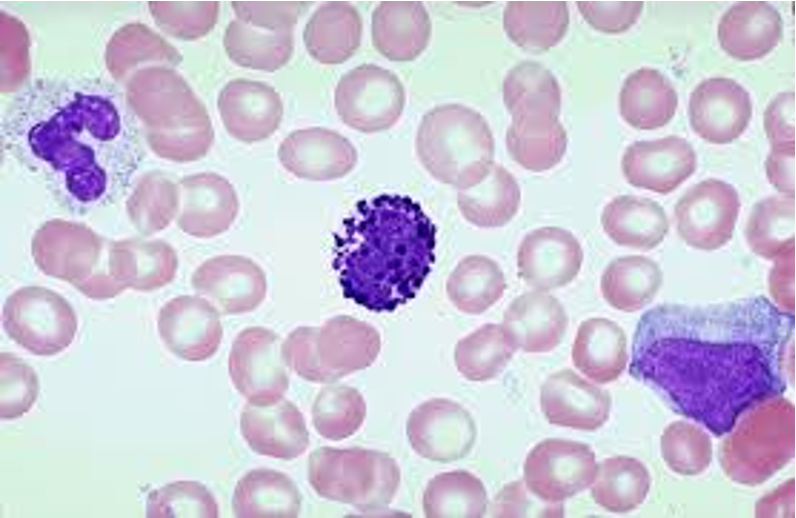
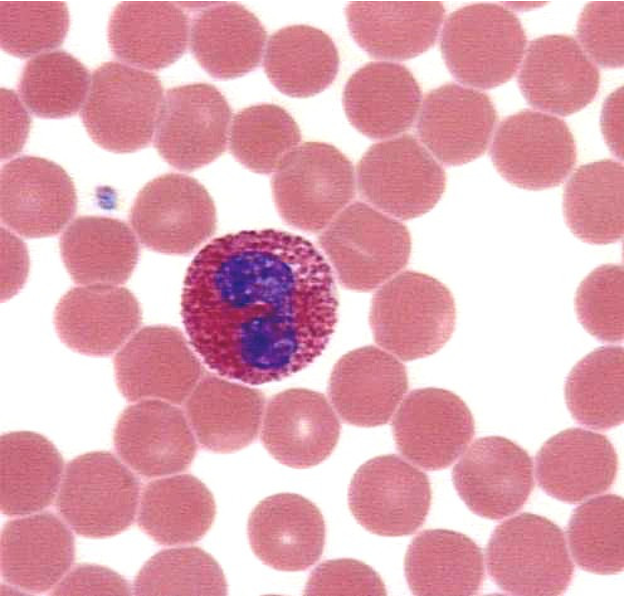
Monocytes
Largest WBC in the peripheral blood
Mono in peripheral blood, macrophage when it migrates to the tissues
Primary functions are phagocytosis and antigen presentation
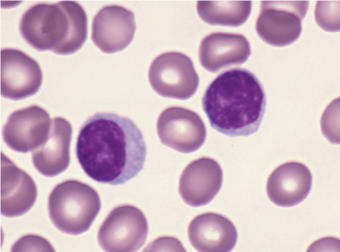
Lymphocytes
Other predominant WBC in the body
Function is to provide immunity
Increase in lymphs indicates viral infection
Two types:
T cells — secrete chemical messengers that tell other cells what to do & kill virally infected cells
Cell-mediated immunity
B cells — make antibodies to provide immunity
Humoral immunity
Natural Killer (NK) cells are large granular lymphs and are the first line of defense against tumors — they can kill without prior exposure to an antigen
T cells
Two types:
Helper T cells secrete cytokines to tell other cells what to do
Cytotoxic T cells kill virally infected cells
B cells
Must first be exposed to an antigen before they can make antibodies
Once exposed, B cells remember that antigen and produce antibodies against it
Next time person is exposed, antibodies attack the antigen before it can cause infection
Called humoral immunity
Thrombocytes (platelets)
Fragments of an actual cell called a megakaryocyte
Main function is clot formation
Work along with 30 different clotting proteins (found in the plasma) to promote coagulation
Deficiencies in platelets or coagulation factors can cause major problems (ex: hemophilia)
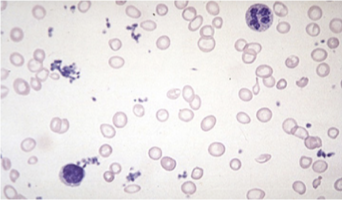
Anemia
Insufficient healthy RBCs and/or HGB to carry adequate O2 to cells and tissues
Most common blood disorder in U.S.
Etiology (varies by type)
Inadequate vitamins or minerals needed to produce RBCs (inadequate intake, malabsorption, or increased demand)
Acute or chronic blood loss
Chronic illness
Medication, NSAIDs, contraceptives, anticonvulsants, antineoplastics)
Bone marrow suppression r/t toxins, chemo, radiation (aplastic anemia)
Destruction of RBCs (hemolytic anemia, Sickle Cell anemia)
Symptoms
Weakness
Fatigue
Shortness of breath
Pallor
Tachycardia
Numb or cold hands and/or feet
Diagnosis
Medical history & PE
Lab
CBC (HGB, HCT, reticulocyte count r/t bone marrow function)
Peripheral smear: RBCs look smaller and pale
Serum iron
Treatment
Correct nutrient deficiencies
Iron (ferrous sulfate)
IM B12 (lack of intrinsic factor secreted by stomach needed for B12 absorption
Treat underlying conditions
Stop bleeding
Replace RBCs (transfusion)
Leukemia
Cancer affecting bone marrow (myeloid tissue)
WBCs mutate quickly
Crowd out normal cells
Do not provide adequate immunity
Etiology
Unknown
Risk factors
Family history of leukemia
Prior tx for CA (chemo/radiation)
Exposure to radiation or chemicals
Smoking (AML)
4 main types — based on two criteria
Speed of progression
Acute: immature cells, rpaid onset, fast progression, aggressive tx
Chronic: mature cells, slower onset
WBC affected
Myelogenous: bone marrow cells that become RBCs, WBCs, and PLTs
Lymphocytic: lymphocytes
Symptoms
Fatigue
Dyspnea
Chronic fever, chills, night sweats
Unexplained weight loss
Frequent infections, slow wound healing
Swollen, non-tender lymph nodes (especially neck and armpits)
Enlarged liver (Hepatomegaly)
Enlarged spleen (Splenomegaly)
Abnormal bleeding, bruising, petechiae
Bone pain
Additional symptoms if organs affected
Diagnosis
History identifying risk factors & sx
PE revealing fever, wt loss, pallow, bone pain, enlarged lymph nodes, hepatomegaly, splenomegaly
Lab: CBC
Tissue bx of lymph nodes
Bone marrow bx
Treatment: usually by hematologist-oncologist; depends on type and stage
Chemo and/or radiation
Biological therapy: meds to boost immunity
Targeted therapy: PO med imatinib (Gleevec) for CML
Bone marrow transplant
Stem cell transplant (stem cells in bone marrow become blood cells)
Diseased bone marrow exposed to radiation or chemo, then stem cells transplanted from healthy donor
Prognosis
Depends on type and stage at diagnosis
If fatal, cause is usually infection
Hemophilia
Rare bleeding disorder in which blood doesn’t clot normally (little or no clotting factor)
Etiology
Usually genetic (mother to sons)
Two main types (A and B)
Most common is type A (missing factor VIII); type B (missing factor IX)
Rarely, hemophilia can be acquired if antibodies form against clotting factors
Symptoms
Excessive bleeding (internal or external)
Procedures (circumcision)
Bleeding from mouth (losing a tooth)
Nosebleeds
Bleeding from minor cut
Hematuria, melena
Large bruises (bleeding into large muscle)
Bleeding into joints
Bleeding in brain
Diagnosis
Pt history
Lab
Hemophilia A and B are classified as mild, moderate, or severe, depending on amount of clotting factor
Severe hemophilia (usually dx during infancy)
Pregnant carriers: in vitro; only embryos tested neg for hemophilia are implanted
Treatment
Replacement therapy: concentrates of clotting factor VIII (for hemophilia A) or clotting factor IX (for hemophilia B) IV
Human blood or recombinant clotting factors
Hematology testing
CBC is the most common hematology test
Includes:
Hgb
Hct
RBC count
RBC indices (MCV, MCH, MCHC)
WBC count
WBC diff
Plt count
Other common hematology tests:
Prothrombin time (PT)
Activated partial thromboplastin time (aPTT)
Hematocrit
Measurement of the percentage of packed RBCs in a volume of blood
Can either be done as a part of CBC or as a microhematocrit
Normal range: 36-45% (women)
Decreased in: Anemia
Increased in: Polycythemia vera
Hemoglobin (Hgb)
Measures O2-carrying capacity
Can either be done as part of a CBC or POCT
Normal range: 12-16 g/dL (women)
Increase: Polycythemia vera
Decrease: Anemia
H&H must agree according to the rule of 3
Hgb x 3 ±3 = Hct
WBC count
Counts the TOTAL number of WBCs in sample (all 5 types)
Normal range: 4,000-11,000/mm3
Increased (leukocytosis) in bacterial infections
Can also indicate diseases like leukemia
Decreased (leukopenia) in viral infections, chemotherapy
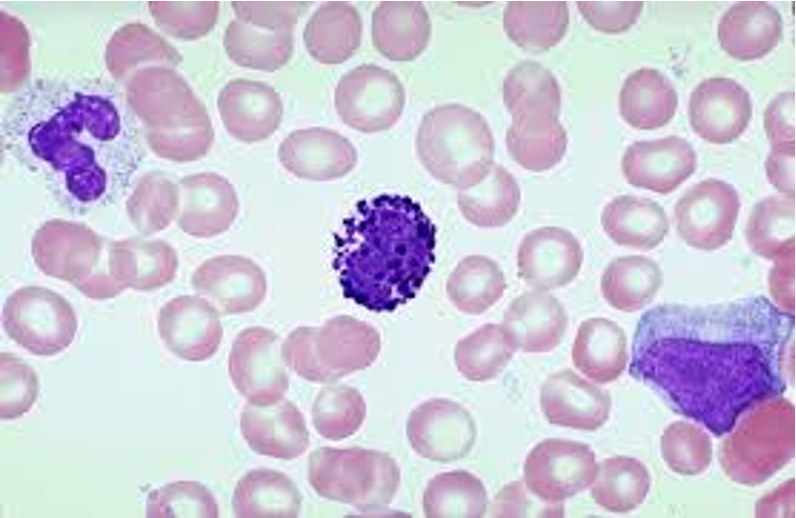
WBC diff
Tells us the percentage of each of the 5 types of WBCs
Increased segs = possible bacterial infection
Increased lymphs = possible viral infection
Increased eosinophils = allergic reaction/parasitic infection
Abnormal cells can indicate diseases like leukemia
Also look at size & shape of RBCs & PLTs
PLT count
Normal range is 150,000-400,000/mm3
Decrease means patient may have trouble with blood clotting
ESR
Not specific for particular disease
Used as a general indicator of inflammation — can help monitor effectiveness of treatments
Increased in infections, RA, Multiple Myeloma, lupus, and more
Fill designated tube completely to line, invert several times
Place in machine for 60 minutes, machine will print results
CLIA-Waived
Coag testing
Protime (PT) is most common — measures how many seconds it takes for blood to clot
Used to diagnose hereditary bleeding disorders and monitor pts on Coumadin (warfarin) which slows the liver’s production of clotting factors
INR was created to standardize PT results because they can vary depending on the reagent used in the test
Widely accepted as the standard for reporting PT results
Normal INR: 1-1.4
Patients on medication to prevent blood clots will have higher INRs (2-3)
Can be done on a coag analyzer or POCT
If done on analyzer, draw BLUE tube and fill to line!
Specimen collection
Most tests are performed on a well mixed EDTA tube, whole blood
Mix sample well after collection to evenly distribute EDTA — failure to do so will result in clotting
If clotting occurs, you cannot report the results
PLT count will be low and WBC may be high, analyzer will flag
Blood smear
Can be done on EDTA OR fresh capillary blood
Depending on time constraints, MA may do this
A good blood smear should cover ¾ of the slide and have a feathered edge
No ridges, holes, lines, clumps, streaks
Let air dry before staining
Stain with Wright stain (series of 3 stains)
Immunohematology (Blood Bank)
ABO
Involves transfusion of donor blood to recipient
Four major blood types
A — A antigens on RBCs
B — B antigens on RBCs
AB — A and B antigens on RBCs
O — lack of A or B antigens on RBCs
Antibodies are naturally made to the ABO antigens you lack!
YOU ONLY MAKE THE ANTIBODY IF YOU LACK THE ANTIGEN!
Rh
Patient is either Rh positive or negative:
Presence of D antigen = Rh pos (85% of population)
Absence of D antigen = Rh negative (15% of population)
Antibodies are NOT naturally made to the Rh blood group
You only make antibodies if you lack the antigen & are then exposed
Ex: mom is Rh neg, baby is Rh pos, mom is exposed to baby’s blood & makes an antibody
Next pregnancy, if baby is Rh pos, mom’s Anti-D will cross the placenta and attack baby causing miscarriage or fetal anemia
To treat this, we give Rh neg moms Rhogam (Anti-D) to prevent mom from making it on her own
Blood transfusions
ABO and Rh typing are usually performed before blood transfusion (only not performed in emergencies)
Then, the lab tests donor blood with recipient serum to determine whether the recipient will react to donor blood (Crossmatch)
Most blood transfusions come from another person, but a person can donate their own blood to be given later (after surgery) — autologous donation
There is always a risk for bloodborne pathogens, but donor blood undergoes rigorous testing via FDA guidelines to minimize the risk
Some religions do not believe in blood transfusions (Jehovah’s Witness) so MA should be aware of this and always ask consent