Lymphatics II
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
immune system
barriers, cells, and proteins involved in the defense of the human body
immune system phases
barrier defense
innate immune response
adaptive immune response
barrier defense
instantaneous prevention
innate immune response
rapid but nonspecific response
adaptive immune response
slower but specific and effective response
innate (non-specific) response time
immediate, pre-formed
innate (non-specific) range of targets
effective against a wide variety of targets
innate (non-specific) body structures
barrier to invasion (skin, mucous membrane)
chemicals
cells (phagocytes, NK cells)
adaptive (specific) response time
some delay
adaptive (specific) range of targets
selective
adaptive to each target
adaptive (specific) body structures
B lymphocytes
T lymphocytes
antigen presenting cells
barriers to infection
classed as “innate immunity” as it is immediate and non-specific
barriers to infection consists of
intact skin
mucous membrane
intact skin characteristics
30-50 rows of stratified keratinized epithelium
slightly acidic pH (3-5)
salty due to NaCl in sweat (discourages most bacterial growth)
relatively dry
skin secretions contain antibacterial chemicals (lysozyme, fatty acids)
mucous membrane characteristics
non-keratinized, stratified squamous epithelium
acidic pH (stomach, vagina during childbearing years)
hair, cilia, mucous which helps to trap foreign particles
saliva contains lysozome
normal flora compete with pathogens
innate internal defense
inflammatory response
phagocytes
natural killer cells
complement system
inflammatory response
process begins with tissue injury, which is recognized by mast cell and basophils
inflammatory response characteristics
heat
redness
pain
swelling
what does mast cell release?
histamines
leukotrienes
prostaglandins
heat
capillary widening
increased blood flow
redness
increased permeability
fluid release into tissues
swelling
inbetween redness and tenderness
what is tissue injury caused by?
physical/chemical agent or pathogenic microorganism
tenderness
attraction of leukocytes
extravasation of leukocytes to site of injury
pain
systemic response
fever and proliferation of leukocytes
inflammatory response stages
tissue injury
vasodilation
increased vascular permeability
recruitment of phagocytes
what do phagocytes include?
macrophages (derived from monocytes)
neutrophils
eosinophils (weakly phagocytic)
mast cells
phagocytes
these cells can perform phagocytosis
first event of phagocytosis
phagocyte adheres to pathogens or debris
second event of phagocytosis
phagocyte forms pseudopods that eventually engulf the particles forming a phagosome
third event of phagocytosis
lysosome fuses with the phagocytic vesicle, forming a phagolysosome
fourth event of phagocytosis
lysosomal enzymes digest the particles, leaving a residual body
fifth event of phagocytosis
exocytosis of the vesicle removes indigestible and residual material
phagocytosis
the process of using cytoplasmic extensions to pull and engulf pathogens toward it
what happens during phagocytosis?
adherence
opsonisation
adherance
phagocytes must adhere to microbes
can be done by carbohydrates on the pathogen’s surface via opsonisation
opsonisation
the coating of a pathogen with antibodies or complement proteins
natural killer cells
a group of lymphocytes
they lyse and kill cancer cell and virus infected cells by releasing perforins and granzyme B
natural killer cells function
create defects in the plasma membrane and nuclear membranes of pathogens (perforins poke holes)
stimulates apoptosis (programmed cell death)
complement system
proteins made in the liver that are found in the plasma
what activates the complement system?
the innate immune response via thte alternative pathway
the adaptive immune response in the classical pathway
what can the complement system do once activated?
bind to pathogens for opsonization
act as chemotactic agents to attract more phagocytes/inflammation
form damage pores in plasma membrane in pathogens called “membrane attack complex”
c reactive protein
acute phase protein made by the liver
it binds to surfaces of pathogens and damaged body cells and then binds to C1, activating complement in the classical pathway
interferons
produced by a variety of cell types
α (alpha) IFN
β (beta) IFN
γ (gamma)
α (alpha) IFN
produced by all leukocytes except lymphocytes
β (beta) IFN
produced by fibroblasts (beta, blasts)
γ (gamma) IFN
produced by lymphocytes
interferon stages
antiviral effects
activate microphages
activate natural killer cells
first interferons step
virus enters cell
second interferons step
interferon genes switch on
third interferons step
cell produces interferon molecules
fourth interferons step
interferon binding stimulates cell to turn on genes for antiviral proteins
fifth interferons step
antiviral proteins block viral reproduction
antiviral effects
blocks viral replication
what do body cells infected with virus secrete?
interferon (IFN)
how is Protein Kinase R (PKR) synthesized?
interferon diffuses to nearby healthy cells and induces them
what does PKR do?
blocks the production of proteins the virus needs to replicate
types of adaptive immunity
humoral
cell-mediated
cell-mediated immunity
mostly managed by t cells that develop in the thymus
defend against infected cells, transplant tissues, cancers
2 types of cell-mediated immunity
helper t cells (Th)
cytotoxic t cells (Tc)
helper t cells (Th)
CD4 molecules on them
they release cytokines to activate macrophages, other t cells, and b cells
cytotoxic t cells (Tc)
CD8 molecules on them
these kill target cells via apoptosis, similar to NK cells, but can kill multiple at once
humoral immunity
b cells develop in the bone marrow, each one is specialized to recognizing a specific antigen
if it is activated by its antigen, it develops into a plasma cells
plasma cells secrete antibodies into body fluids
what happens when antibodies form complexes with antigens?
activate complement (classical pathway)
neutralize the antigen
immobilize the antigen by precipitation or agglutination
what do b cell become
memory cells—so we can mount a faster response if we see that pathogen again
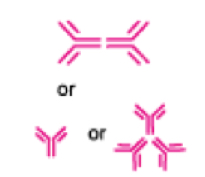
antibodies (immunoglobins)
IgG
IgM
IgA
IgD
IgE
IgG
highest opsonization and neutralization activities
classified into four subclasses

subclasses of IgG
IgG1
IgG2
IgG3
IgG4

IgM
produced first upon antigen invasion
increases transiently

IgA
expressed in mucosal tissues
forms dimers after secretion
IgD
unknown function

IgE
involved in allergy
