HCS model Year 1
1/32
Earn XP
Description and Tags
ugh
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
What are zola’s 5 triggers? name them
These are events/factors which influence individuals to seek medical consultation. They are dependent on daily demands or interpretation of bodily symptoms. Zola’s 5 triggers are:
Interpersonal crisis
Perceived interference with physical or vocational activity
Perceived interference with personal or social relations
Sanctioning e.g. others pressure you to seek medical help
Temporalising (setting time limit before seeking help)
What are Mechanic & Volkart’s triggers? Name them
Describes a different set of factors which encourage patients to seek medical consultation. The triggers are:
Frequency of illness in the population
Familiarity of symptoms
Predictability of outcome
Amount of threat and loss likely to be suffered from illness
What is Lazarus transactional model of stress
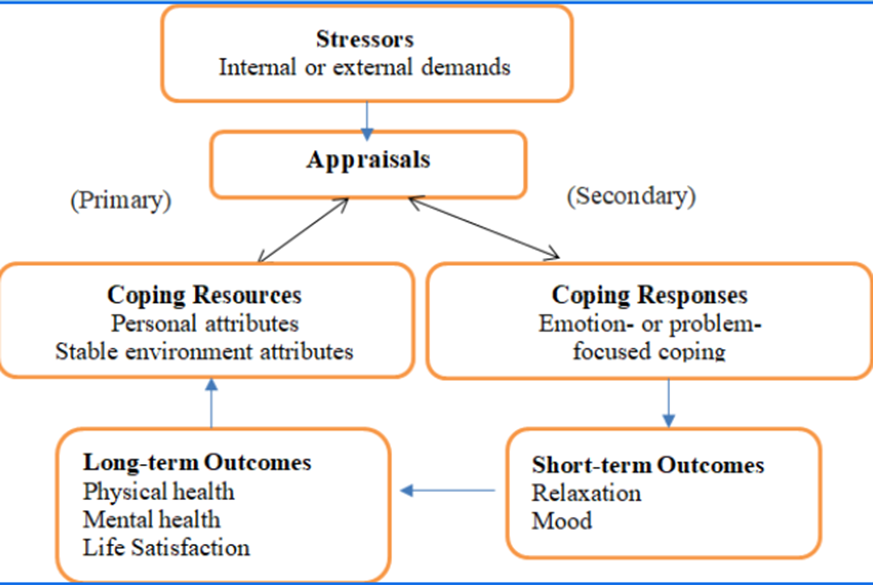
Primary Appraisal: “Is this a threat or challenge?”
Secondary Appraisal: “Do I have the tools/resources to deal with this?”
What are Jacquet’s 7 Criteria for Effective Stigmatisation?
The audience responsible for the shaming should be concerned with the transgression
There should be a big gap between the desired and actual behaviour
Formal punishment should be missing
The transgressor should be sensitive to the source of the shaming
The audience should trust the source of shaming
Shaming should be directed where possible benefits are greatest
Scrupulous implementation
Outline the Transtheoretical model of behaviour change PCPAMR
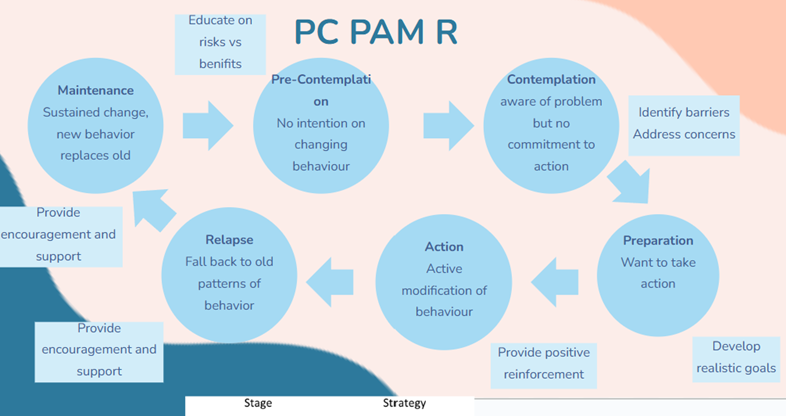
What are the pros of the transtheoretical model of behaviour change?
+ realistic as it acknowledges that change is not a linear process and that people go through stages in different ways and may relapse
+ recognises that relapse is a normal part of changing behaviour
It is important for HCPs to emphasise this and explore what a person has learned from a relapse and how this can be used to increase chances of success next time
+ useful in practice when dealing with smoking/alcohol/food/drug addictions etc, allows doctor to see if the patient is ready to change
What are the cons of the Transtheoretical model of behaviour change
could potentially become too much as a person may go through the cycle many times
- requires motivation from the patient
-not always a sequential process
-Ignores social context
- may be too late before a person enters the contemplation stage
What is the health belief model used for and what are the 5 factors part of it?
1) Perceived Susceptibility= belief of the chances of getting the illness
2) Perceived Severity= belief of the severity of the illness
3) Perceived Benefits= beliefs about what can be gained from taking action
4) Perceived Barriers= beliefs about the negative consequences of taking action
5) Self-Efficacy= confidene in their own ability to take action
What are the pros of the health belief model?
Includes common-sense constructs easy for non-psychologists to assimilate and apply
Has focused research attention on modifiable psychological prerequisites of behavior
Makes testable predictions
What are the Limitations of the health belief model?
Its common-sense framework simplifies health-related representational processes
Its theoretical components are broadly defined, and therefore different specific behaviors may not be strictly comparable
Lack of specification of a causal ordering
Neglects social factors
Name the big 5 personality traits (Psychological reasons why people respond differently to health) and what they mean
The Big Five personality traits, also known as OCEAN (Openness, Conscientiousness, Extraversion, Agreeableness, and Neuroticism), play a significant role in influencing how individuals respond to health-related situations.
Openness (O):
High Openness: Individuals with high openness are often more receptive to new information and experiences, including health-related information. They may be more likely to adopt alternative or unconventional health practices.
Low Openness: Those with lower openness might be more skeptical of new health approaches, preferring traditional or well-established methods.
Conscientiousness (C):
High Conscientiousness: Individuals high in conscientiousness tend to be organized, responsible, and disciplined. They are more likely to adhere to health regimens, follow medical advice, and engage in preventive health behaviors.
Low Conscientiousness: Those with lower conscientiousness may struggle with maintaining consistent health habits, missing appointments, or neglecting prescribed treatments.
Extraversion (E):
High Extraversion: Extraverted individuals may seek social support and engage in group activities that promote health and well-being. They might be more inclined to participate in group fitness classes or team sports.
Low Extraversion: Introverted individuals may prefer more solitary health activities or self-directed exercises. They may also be more reserved about discussing health concerns openly.
Agreeableness (A):
High Agreeableness: Agreeable individuals are generally cooperative and empathetic. They may be more likely to comply with medical advice and work collaboratively with healthcare professionals.
Low Agreeableness: Individuals with lower agreeableness may be more skeptical, independent-minded, and may question health recommendations. They might seek multiple opinions before committing to a health plan.
Neuroticism (N):
High Neuroticism: Neurotic individuals may be more prone to stress and anxiety, which can affect their health. They might engage in health behaviors as a way to alleviate anxiety or may be more vigilant about potential health threats.
Low Neuroticism: Those with lower neuroticism may be more resilient to stress and less likely to worry about health issues. However, they might also be less likely to seek help when needed.
Sociological reasons why people respond differently to health
Cultural influences: Cultural norms and values shape health behaviors. For example, some cultures may prioritize holistic approaches to health, while others may rely more on medical interventions.
Social support: The presence or absence of a strong social support system can significantly impact health behaviors. Individuals with supportive networks may be more motivated to adopt and maintain healthy habits.
Socioeconomic status: Access to healthcare resources, education, and economic factors can influence health behaviors. Lower socioeconomic status may limit access to healthcare and healthy lifestyle options.
What are the 2 Models of disability
social model of disability
medical model of disability
What is the social model of disability
The social model of disability views disability as a result of the interaction between individuals with impairments and societal barriers that hinder their full participation in society. This model emphasizes that disability is not an inherent attribute of the individual but rather a socially constructed phenomenon.
What is the medical model of disability?
The medical model of disability perceives disability primarily as a problem or deficiency within the individual that needs to be cured or managed through medical intervention.
Differences between the disability models
1. Conceptual Framework:
Medical Model: Disability is a problem of the individual, requiring medical treatment.
Social Model: Disability is a social issue, arising from environmental and attitudinal barriers.
2. Focus of Intervention:
Medical Model: Focuses on curing or managing the individual's impairment.
Social Model: Focuses on changing society to be more inclusive and removing barriers.
3. View of Disability:
Medical Model: Views disability as a negative condition that should be mitigated.
Social Model: Views disability as a natural part of human diversity and emphasizes acceptance and inclusion.
4. Role of Professionals:
Medical Model: Doctors and healthcare providers play a central role in "fixing" the disability.
Social Model: Emphasizes the role of policymakers, architects, educators, and the community in creating an inclusive society.
Pros and cons of the social model of disability
Social Pros:
Reduces stigma
Empowers disabled
Focuses on barriers
Social Cons:
Denies link between physical impairment & social disability
Reduces urgency to find cures in disabled patients
Not all disability can be helped by removal of societal barriers
Outline the Implications of these disbaility models on care
Patient centred care:
Medical Model: Health care often focuses on treating the impairment, which can lead to overlooking the broader needs and rights of the individual.
Social Model: Encourages health care providers to consider the person's social context and work to reduce barriers, promoting a more holistic approach to care.
Accessibility and Inclusion:
Medical Model: May not prioritize making healthcare facilities and services accessible.
Social Model: Stresses the importance of accessible healthcare environments and services, ensuring that all individuals can receive care without facing physical or systemic barriers.
Empowerment and Participation:
Medical Model: Can sometimes lead to a paternalistic approach, where healthcare providers make decisions on behalf of the patient.
Social Model: Advocates for the empowerment of individuals with disabilities, encouraging their active participation in healthcare decisions and promoting autonomy.
Policy and Advocacy:
Medical Model: Policy may focus more on funding medical treatments and rehabilitation services.
Social Model: Advocates for policies that address social determinants of health, such as accessible housing, education, and employment opportunities, and that promote equality and non-discrimination.
What is Maslow's hierarchy of needs? Relate this to QoL (5+1)
1. Physiological needs
2. Safety and Security needs
3. Love and Belonging Needs
4. Self esteem
5. Self actualization
-the higher up you go, the more likely QoL will be increased
What is the model of responsiblity?
1. Awareness of risk: By being aware of the risk, parents are more likely to address themselves and redefine their responsibilities
2. Reproduction seen as problematic
3. Redefining elements: Situation is perceived differently, especially within the family, which can lead to decreased support. Responsibility becomes problematic.
4. Establishing self as responsible decision maker: Parents have a choice to accept the risk, modify the risk, or avoid the risk. This depends on the relationships which are prioritised.
What are the different models of addiction?
Disease Approach
Moral Code
Genetic approach
Choice model
Exposure Model
Experimental Model
What is the disease approach to addiction?
Progressive & chronic disease which is uncontrollable & requires treatment – aims to reduce stigma.
What is the Moral Code to addiction?
Result of weakness and people are addicted due to a matter of choice → increases stigma.
What is the Genetic Approach to addiction?
Genetically predisposed to certain addictive behaviours. Excludes environmental & social influence
What is the choice model of addiction?
Refers to addiction as an action of choice meaning people can choose to stop & start as they decide.
What is the Exposure Model to addiction?
Regular consumption has led to metabolic dependency & so need to use with increasing dose to receive effect.
What is the Experimental Model of addiction?
Phase of experimenting
Outline the PRIME theory?
-brings together what we know about motivation in one model
-includes our innate reactions, habits, drives, desires, goals, plans and so on
-goal is to improve our ability to explain, predict and influence behaviour
-'p.r.i.m.e', which stands for plans, responses, impulses, motives and evaluations
· PLANS- Your intention to do something - Mental representations, future action, degrees of commitment
· EVALUATION- Evaluate beliefs to make a decision
· MOTIVES- Conscious desires - what you want
· IMPULSES/INHIBITIONS- Conscious urges
· RESPONSES- Start / stop / modify actions

What are the 3 central ideas of the prime theory?
-it is wants and needs at each moment that drive our behaviour.
-our intentions and beliefs about what is good or bad only influence our actions if they create sufficiently strong wants and needs at the relevant moment.
-our image og our ourselves and how we feel about that, our identity, is a potentially very strong source of wants and needs which can be enough to overcome ones arising from biological drives such as hunger
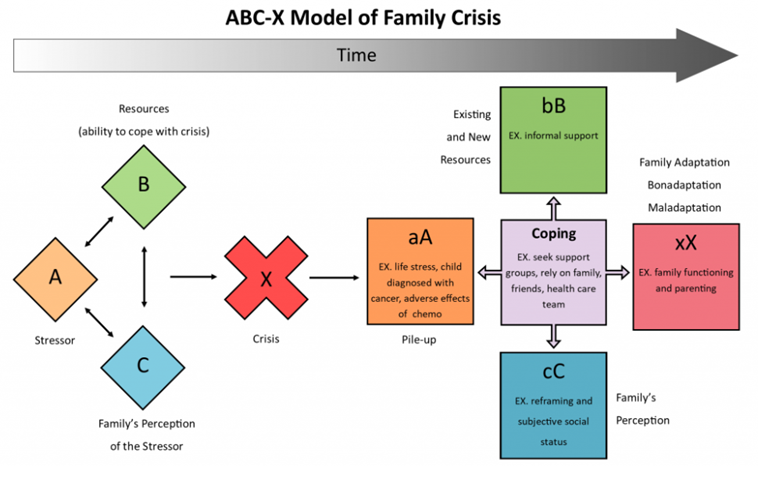
Outline the ABCX model of family crisis
· PLANS- Your intention to do something - Mental representations, future action, degrees of commitment
· EVALUATION- Evaluate beliefs to make a decision
· MOTIVES- Conscious desires - what you want
· IMPULSES/INHIBITIONS- Conscious urges
· RESPONSES- Start / stop / modify actions
Outline Transactional Model of Stress & Coping (Lazarus & Folkman)
Stress is a dynamic relationship between a person and their environment.
One becomes stressed when demands outweigh resources.
1. Primary Appraisal - is anything at risk? How bad is it?
2. Secondary Appraisal - internal & external locus coping options.
3. Coping - problem/emotion-focussed.
Name and explain 5 Stages of Grief
5 Stages of Grief - DABDA
1. Denial: patient does not want to acknowledge what is happening; protective emotion.
2. Anger: acknowledges illness but anger persists; “why me?”, “why now?”.
3. Bargaining: making deals with self to feel better; “what if I didn’t do X?”, “if I act this way I’ll feel better.”
4. Depression: crushing sadness; diagnosis no longer denied.
5. Acceptance: Illness is accepted and incorporated within life and self-identity.
Outline DNARA
1. Denial: denies having the illness.
2. Normalising: classes symptoms as normal which neutralises threat but not disease.
3. Avoidance: avoids situation which may exacerbate problem; potentially causes social exclusion.
4. Resignation: totally consumed by illness; highly dependent on others.
5. Accommodation: patient acknowledges and deals with problems illness presents.