MODULE 3 IMMUNO SECTION WORKSHEET QUESTIONS
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
An inflammatory response is a body’s second line of defense against pathogens. Which of the following is NOT a sign of inflammation?
Redness
Pain
Itchiness
Swelling
Heat
Loss of function
An inflammatory response is a body’s second line of defense against pathogens. Which of the following is NOT a sign of inflammation?
Redness
Pain
Itchiness
Swelling
Heat
Loss of function
Selectins are receptors that bind to sugars on the surface of cells and facilitate the rolling step of leukocyte trafficking. In one particular patient who is having recurrent bacterial infections and high leukocyte counts in their blood, researchers suspect that there may be a defect in the selectins on their cells. Immunofluorescence was done on the patient’s endothelial cells, leukocytes, and platelets to examine the presence of selectins on their surface. Images show the presence of selectins on the patient’s endothelial cells and platelets, but not on the surface of leukocytes. The patient most likely has a defect in which selectin?
L-selectin
E-selectin
M-selectin
P-selectin
D-selectin
Selectins are receptors that bind to sugars on the surface of cells and facilitate the rolling step of leukocyte trafficking. In one particular patient who is having recurrent bacterial infections and high leukocyte counts in their blood, researchers suspect that there may be a defect in the selectins on their cells. Immunofluorescence was done on the patient’s endothelial cells, leukocytes, and platelets to examine the presence of selectins on their surface. Images show the presence of selectins on the patient’s endothelial cells and platelets, but not on the surface of leukocytes. The patient most likely has a defect in which selectin?
L-selectin
E-selectin
M-selectin
P-selectin
D-selectin
Leukocyte adhesion deficiency 1 is a rare disease where white blood cells cannot move properly toward a site of infection. Which of the following is NOT a correct statement regarding the disease?
Patients have recurring bacterial infections
High neutrophil count in the blood
Defect in the Mac-1 integrin
Natalizumab can help treat LAD-1
Neutrophils can roll but do not stick
Leukocyte adhesion deficiency 1 is a rare disease where white blood cells cannot move properly toward a site of infection. Which of the following is NOT a correct statement regarding the disease?
Patients have recurring bacterial infections
High neutrophil count in the blood
Defect in the Mac-1 integrin
Natalizumab can help treat LAD-1
Neutrophils can roll but do not stick
_____________ is the process where white blood cells exit the bloodstream and travel to a site of infection in order to fight off pathogens.
Extravasation/diapedesis is the process where white blood cells exit the bloodstream and travel to a site of infection in order to fight off pathogens.
______________ are small cytokines that attract cells to the site of infection by binding to receptors on their surface. Once at the site, _____________ are heterodimer receptors present on the cells to facilitate the adhesion step of leukocyte trafficking, allowing them to stick to the surface of endothelial cells and exit the bloodstream.
Chemokines are small cytokines that attract cells to the site of infection by binding to receptors on their surface. Once at the site, integrins are heterodimer receptors present on the cells to facilitate the adhesion step of leukocyte trafficking, allowing them to stick to the surface of endothelial cells and exit the bloodstream.
______________ are leukocytes that can survey the host environment by visiting lymph nodes and the spleen, and can recirculate in the bloodstream. However, ______________ are leukocytes that cannot recirculate in the bloodstream once they reach a site of infection.
T cells are leukocytes that can survey the host environment by visiting lymph nodes and the spleen, and can recirculate in the bloodstream. However, neutrophils are leukocytes that cannot recirculate in the bloodstream once they reach a site of infection.
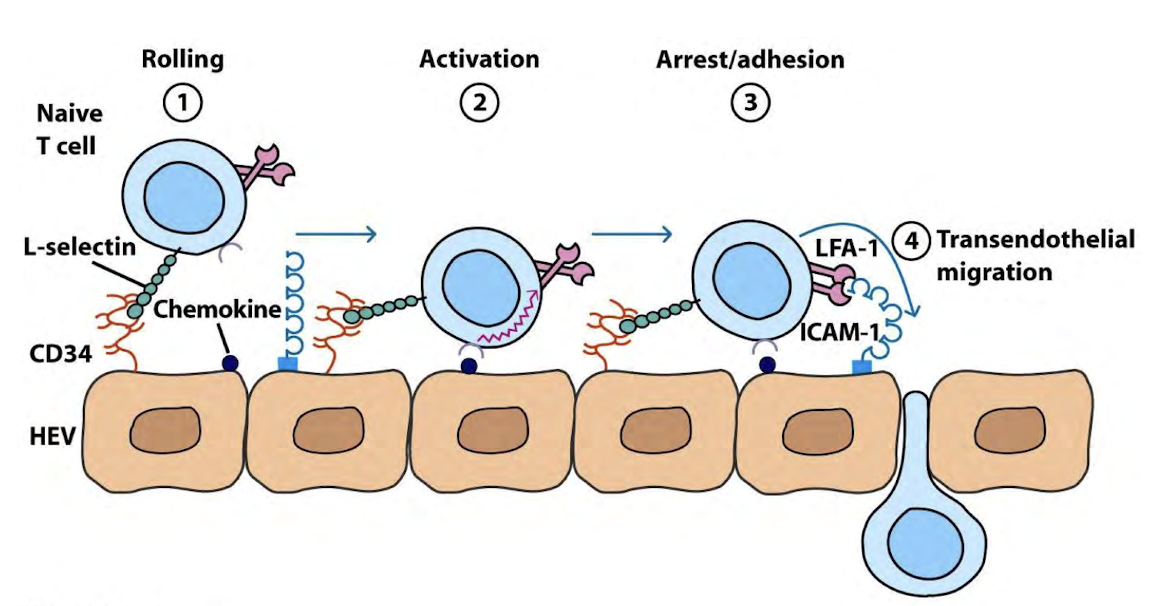
The trafficking of T cells within lymph nodes is a specific process that is different from B cells and neutrophils. Please explain the steps of this process, including the receptors and other proteins involved.
T cells utilize L-selectin to interact with sialomucin present on the surface of the high endothelial venule (HEV)
T cells use CCR7 to bind to CCL21 expressed on HEV
This binding activates integrin LFA1, causing adhesion to the HEV
Transendothelial migration occurs
A patient presents with multiple autoimmune symptoms and reduced endocrine function. Although initially suspected to have an overactive immune system, testing reveals an immunodeficiency caused by a mutation affecting self-antigen presentation in the thymus. Which of the following additional findings would most likely be present?
Absent B and T cells
Decreased number of circulating T cells
High levels of autoreactive T cells targeting endocrine tissues
Defective NADPH oxidase activity in phagocytes
Impaired class-switch recombination in B cells
Loss of complement components C1q and C4
A patient presents with multiple autoimmune symptoms and reduced endocrine function. Although initially suspected to have an overactive immune system, testing reveals an immunodeficiency caused by a mutation affecting self-antigen presentation in the thymus. Which of the following additional findings would most likely be present?
Absent B and T cells
Decreased number of circulating T cells
High levels of autoreactive T cells targeting endocrine tissues
Defective NADPH oxidase activity in phagocytes
Impaired class-switch recombination in B cells
Loss of complement components C1q and C4
Subject A who is not allergic to cats was administered with serum from subject B who is allergic to cats into the arm. Subject A was then exposed to cat fur on the arm. What do we expect to see? What is the molecule in the serum contributing to this response? Who are the scientists that discovered this component of the serum that contributes to the immune response?
No reaction, IgA, Prausnitz and Kustner
No reaction, IgG, Ishizakas
No reaction, IgE, Richet and Portier
Wheal and Flare, IgA, Richet and Portier
Wheal and Flare, IgE, Ishizakas
Wheal and Flare, IgG, Prausnitz and Kustner
Subject A who is not allergic to cats was administered with serum from subject B who is allergic to cats into the arm. Subject A was then exposed to cat fur on the arm. What do we expect to see? What is the molecule in the serum contributing to this response? Who are the scientists that discovered this component of the serum that contributes to the immune response?
No reaction, IgA, Prausnitz and Kustner
No reaction, IgG, Ishizakas
No reaction, IgE, Richet and Portier
Wheal and Flare, IgA, Richet and Portier
Wheal and Flare, IgE, Ishizakas
Wheal and Flare, IgG, Prausnitz and Kustner
A patient comes into the clinic and expresses the following:
|
Based on the information above, which of the following diagnoses is correct?
Food allergy-induced localized hypersensitivity reaction
Non-food allergy-induced systemic anaphylaxis
Food allergy-induced systemic anaphylaxis
Non-food allergy-induced localized hypersensitivity reaction
If you answered (2) or (3), what is a possible agent that could treat this patient’s condition. If you answered (1) or (4), leave this blank.
A patient comes into the clinic and expresses the following:
|
Based on the information above, which of the following diagnoses is correct?
Food allergy-induced localized hypersensitivity reaction
Non-food allergy-induced systemic anaphylaxis
Food allergy-induced systemic anaphylaxis
Non-food allergy-induced localized hypersensitivity reaction
A possible agent that could treat this patient’s condition: epinephrine.
A major cause of secondary hypersensitivity cases is HIV infection. Let’s review the process by which HIV infects a T cell:
HIV attaches to T cell by binding to _______ and a coreceptor: _______ or _______
HIV enters the cell and unfolds, releasing its RNA genome
__________, a viral enzyme, converts the RNA genome into DNA
__________, another viral enzyme, to cut the T cell DNA and integrate the viral DNA (provirus) into the genome
A major cause of secondary hypersensitivity cases is HIV infection. Let’s review the process by which HIV infects a T cell:
HIV attaches to T cell by binding to CD4+ and a coreceptor: CCR5 or CXCR4
HIV enters the cell and unfolds, releasing its RNA genome
Reverse transcriptase, a viral enzyme, converts the RNA genome into DNA
Integrase, another viral enzyme, to cut the T cell DNA and integrate the viral DNA (provirus) into the genome
A student needs your help in describing IgE-mediated allergic reactions. Help them by filling in the following blanks:
An allergen is recognized by a B cell and displayed on MHCII
MHCII/Allergen is recognized by __________________ cell (HINT: the polarizing cytokine for this cell is IL-4)
The cell in (b) secretes cytokines like IL-4 and IL-5 causing the class switching to ________ (which class of Ig)
This Ig in (c) binds to Fc receptors known as ____________ present on ____________ cells (granulocyte often found in connective tissue).
Upon secondary exposure to this allergen, cross-linking of the Fc receptor described in (d) causes degranulation of the cell described in (d). List three contents that are released by these cells:
__________________________
__________________________
__________________________
A student needs your help in describing IgE-mediated allergic reactions. Help them by filling in the following blanks:
An allergen is recognized by a B cell and displayed on MHCII
MHCII/Allergen is recognized by T-Helper 2 cell (HINT: the polarizing cytokine for this cell is IL-4)
The cell in (b) secretes cytokines like IL-4 and IL-5 causing the class switching to IgE (which class of Ig)
This Ig in (c) binds to Fc receptors known as FcεRI present on mast cells (granulocyte often found in connective tissue).
Upon secondary exposure to this allergen, cross-linking of the Fc receptor described in (d) causes degranulation of the cell described in (d). List three contents that are released by these cells:
Histamine
Leukotrienes / Prostaglandins
Cytokines
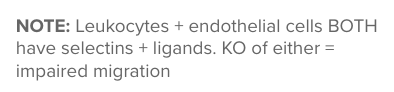
USING THIS AS WORD BANK:
Severe Combined Immunodeficiency (SCID), Bare-Lymphocyte Syndrome, DiGeorge Syndrome, Hyper IgM Syndrome (X-linked), Wiskott-Aldrich Syndrome (WAS)
Thymic developmental defects due to deletion on chromosome 22 (including TBX1): ____ | |
Mutation in early lymphocyte development gene such as RAG1/2 or Artemis; causes absent T cells and absent or diminished B and NK cells: ____ | |
CD40L deficiency leads to defective T–B cell interaction and isotype switching: ____ | |
Defect in MHC class I or II expression; leads to lack of CD4+ or CD8+ T cell activation: ____ | |
Mutation in WASP, a gene that encodes a cytoskeletal protein important in HSCS, causes thrombocytopenia and recurrent bacterial infections: ____ |
Thymic developmental defects due to deletion on chromosome 22 (including TBX1): DiGeorge Syndrome | |
Mutation in early lymphocyte development gene such as RAG1/2 or Artemis; causes absent T cells and absent or diminished B and NK cells: Severe Combined Immunodeficiency (SCID) | |
CD40L deficiency leads to defective T–B cell interaction and isotype switching: Hyper IgM Syndrome (X-linked) | |
Defect in MHC class I or II expression; leads to lack of CD4+ or CD8+ T cell activation: Bare Lymphocyte Syndrome | |
Mutation in WASP, a gene that encodes a cytoskeletal protein important in HSCS, causes thrombocytopenia and recurrent bacterial infections: Wiskott-Aldrich Syndrome (WAS) |
Innate immune deficiencies are often the result of a defect in phagocytosis. Describe the general steps of phagocytosis, and identify the stages where defects can result in specific immunodeficiencies discussed in class.
Bonus: Explain how such defects can lead to granuloma formation.
Phagocytosis overview:
Recognition: Phagocytes bind pathogens via PRRs or opsonins (complement, antibodies).
Engulfment: Pathogen is internalized into a phagosome.
Fusion: Phagosome fuses with lysosome to form a phagolysosome.
Killing: NADPH oxidase (Phox proteins) generates reactive oxygen species (ROS) to destroy microbes.
Digestion: Pathogen is degraded and expelled from the cell.
Defects causing immunodeficiency:
Chediak–Higashi Syndrome: Defect in Step 3
Defective LYST gene → failed phagosome-lysosome fusion → pathogens survive inside phagocytes.
Chronic Granulomatous Disease (CGD): Defect in Step 4
Defective Phox proteins → no ROS production → phagocytes can’t kill pathogens → chronic bacterial/fungal infections.
Bonus – Granulomas:
In CGD, phagocytes can’t control the infection so more immune cells are recruited to the infection site, which triggers chronic inflammation. Macrophages and other immune cells cluster to wall off infection sites, forming granulomas.
There are several reasons why allergies happen and none of them seem to be too far off or correct. One of them is the hygiene hypothesis. Describe the hygiene hypothesis. Based on your explanation of it, in regions that have high helminth infestation incidence, do we expect more or less cases of hypersensitivities? Why?
The hygiene hypothesis states that living in increasingly hygienic environments is causing our immune systems to dysregulate itself resulting in allergies, asthma, and autoimmunities.
In regions that have high helminth infestation incidence, we expect avoidance of TH2 cell dominance as a result of TH2 cell employment against helminth infection. As such, we would expect less cases of hypersensitivity due to less dysregulation of TH2 activity resulting in activity against allergen.
Outline the time course of the Type I hypersensitivity reaction. There are three main phases. When does each phase occur? What is each phase mediated by? What are the major symptoms or clinical outcomes of each phase?
Early Response: occurs within minutes of allergen exposure
Mediated by mast cell granule release
Symptoms:
Bronchoconstriction & Mucus Secretion in Lungs (leukotrienes and prostaglandins)
Vasodilation (Histamine, Lipid Mediators)
Late Phase Reaction: occurs hours after initial allergen exposure
Characterized by a result of the recruitment of cells
Cytokine production (whether pre-packaged or via transcription/translation) causes influx of neutrophils, eosinophils, and TH2 cells
Symptoms:
More inflammation → tissue damage
Third Phase: 3-4 days post-exposure
Characterized by massive eosinophil infiltration and basophils
Secrete additional cytokines and proteases that recruit more cells
Symptoms:
Results in tissue damage
Neutrophils are a part of the _________ immune system
They are the most abundant leukocyte
They are also classified as _________________ as they possess granules that can degranulate
Play a key role in inflammation
Neutrophils are a part of the INNATE immune system
They are the most abundant leukocyte
They are also classified as GRANULOCYTES as they possess granules that can degranulate
Play a key role in inflammation
Neutrophils kill by three mechanisms …
Degranulation
____________ (mxn of action utilized by APCs)
____________ (involves decondensed chromatin release)
Neutrophils kill by three mechanisms …
Degranulation
Phagocytosis (mxn of action utilized by APCs)
NETosis (involves decondensed chromatin release)
Question: A recently discovered mutation results in no expression of the gene that codes for the L-selectin. What is the most likely effect of this mutation?
No transendothelial migration
Less transendothelial migration due to presence of E-selectin
Less transendothelial migration due to presence of P-selectin
No difference in transendothelial migration
1. No transendothelial migration
(remember that leukocytes + endothelial cells BOTH have selectins + ligands. KO of either = impaired migration)
MATCH Function to Selectin, Chemokine or, Integrin!
Plays a critical role in leukocyte slowing along the vascular trail | |
Heterodimer that plays a critical in leukocyte adhesion to the vascular trail | |
Drives the leukocyte towards the site of infection/injury via utilization of the leukocytes’ GPCR | |
Natalizumab targets this, preventing the neutrophil from reaching the site of infection | |
Activates (e.g. CCR7) integrin |
Plays a critical role in leukocyte slowing along the vascular trail | SELECTIN |
Heterodimer that plays a critical in leukocyte adhesion to the vascular trail | INTEGRIN |
Drives the leukocyte towards the site of infection/injury via utilization of the leukocytes’ GPCR | CHEMOKINE |
Natalizumab targets this, preventing the neutrophil from reaching the site of infection | INTEGRIN |
Activates (e.g. CCR7) integrin | CHEMOKINE |
THE ISHIZAKAS (1960S)
Experiment #1 — Is there something in the serum?
Purified serum from patients with allergies and separated fractions of this serum (by size)
Ig fractions of serum from allergic individuals were injected into volunteers
These volunteers were then given allergen-> called it “E”
See if reaction (wheal and flare) is present
Results:
Reaction was present
Conclusion: an Ig fraction was responsible for causing the allergic reaction->called the “E” reagin (now known as IgE)
Follow-up Question: Which Ig is responsible for this reaction?
THE ISHIZAKAS (1960S)
Follow-up Question: Which Ig is responsible for this reaction?
E
RAGWEED ALLERGEN

TYPE II HYPERSENSITIVITIES
Two Phases
Phase I (Sensitization): Cell-surface Ag cause production of IgG or IgM via normal mechanisms
Phase II (Pathology): Subsequent exposure results in IgG or IgM binding resulting in cell lysis via …
Complement Dependent Cytotoxicity: activation of classical complement pathway
Antibody Dependent Cell Cytotoxicity: binds to Fc receptors on ___________ (IgG!)
Opsonization → Phagocytosis (less common)
TYPE II HYPERSENSITIVITIES
Two Phases
Phase I (Sensitization): Cell-surface Ag cause production of IgG or IgM via normal mechanisms
Phase II (Pathology): Subsequent exposure results in IgG or IgM binding resulting in cell lysis via …
Complement Dependent Cytotoxicity: activation of classical complement pathway
Antibody Dependent Cell Cytotoxicity: binds to Fc receptors on NK CELLS (IgG!)
Opsonization → Phagocytosis (less common)
Question: A novel protein called erythrocyte antibody factor (EAF) is present on RBCs and is recognized by anti-IgG antibodies. Upon her ___________ pregnancy, the mother is found to have anti-EAF antibodies. Assuming the fetus to be EAF+, what will most likely happen to the fetus?
First; polycythemia
First; anemia
First; no symptoms
Second; polycythemia
Second; anemia
Second; no symptoms
4. SECOND: POLYCYTHEMIA
Maternal IgG forms after the first pregnancy; in the second it crosses the placenta and destroys EAF+ fetal RBCs → fetal anemia
Injecting Ag into individual with high levels of anti-Ag Abs will result in formation of ________________________ → exacerbated inflammatory response
Discovered in 1903 after Arthus repeatedly injected horse serum into rabbits and observed symptoms of edema and gangrene
Injecting Ag into individual with high levels of anti-Ag Abs will result in formation of IMMUNE COMPLEXES→ exacerbated inflammatory response
Discovered in 1903 after Arthus repeatedly injected horse serum into rabbits and observed symptoms of edema and gangrene
TYPE I, II, III, IV
Description | Hypersensitivity |
Mediated by T Cells and Macrophages: |
|
IgG binding to donor blood cell Ag causing RBC lysis: |
|
Arthus Reaction: |
|
Mediated by IgE and Mast Cell Degranulation: |
|
Result of inefficient immune complex clearance: | |
Farmer’s Lung: |
|
TYPE I, II, III, IV
Description | Hypersensitivity |
Mediated by T Cells and Macrophages: | TYPE IV |
IgG binding to donor blood cell Ag causing RBC lysis: | TYPE II |
Arthus Reaction: | TYPE III |
Mediated by IgE and Mast Cell Degranulation: | TYPE I |
Result of inefficient immune complex clearance: | TYPE III |
Farmer’s Lung: | TYPE III |
TYPES OF TRANSPLANTS
Histocompatibility determines rejection → “histocompatible” grafts share sufficient antigen similarity, decreasing change of rejection. Goal of transplantation is to …
1)
2)
TYPES OF TRANSPLANTS
Histocompatibility determines rejection → “histocompatible” grafts share sufficient antigen similarity, decreasing change of rejection. Goal of transplantation is to …
Minimize graft rejection
Prevent suppressing entire immune response