BIOL 284 exam one review
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
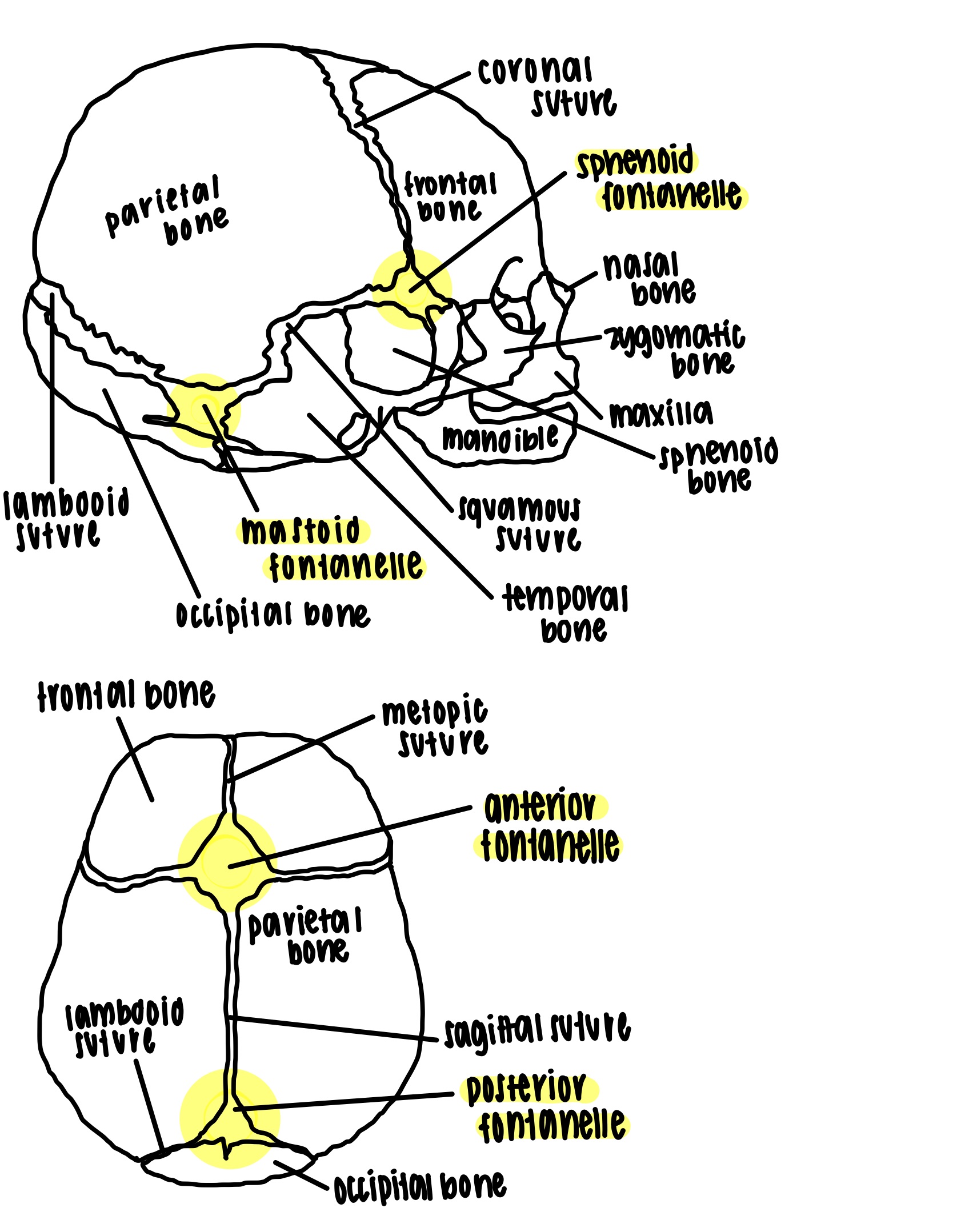
infant fontanelle
identification
sphenoid (anterolateral) fontanelle - superior to the sphenoid bone
mastoid (posterolateral) fontanelle - posterior to the temporal bone
anterior fontanelle - posterior to the frontal bone
posterior fontanelle - anterior to the occipital bone
purpose
fontanelles are spaces between unfused bone that are filled with fibrous membrane
allow for the shifting of the bones during childbirth and the growth of the brain during infancy
fontanelles typically ossify by a year old (except the anterior fontanelle which can remain present up to two years after birth)
skull reaches adult size by eight to nine years of age
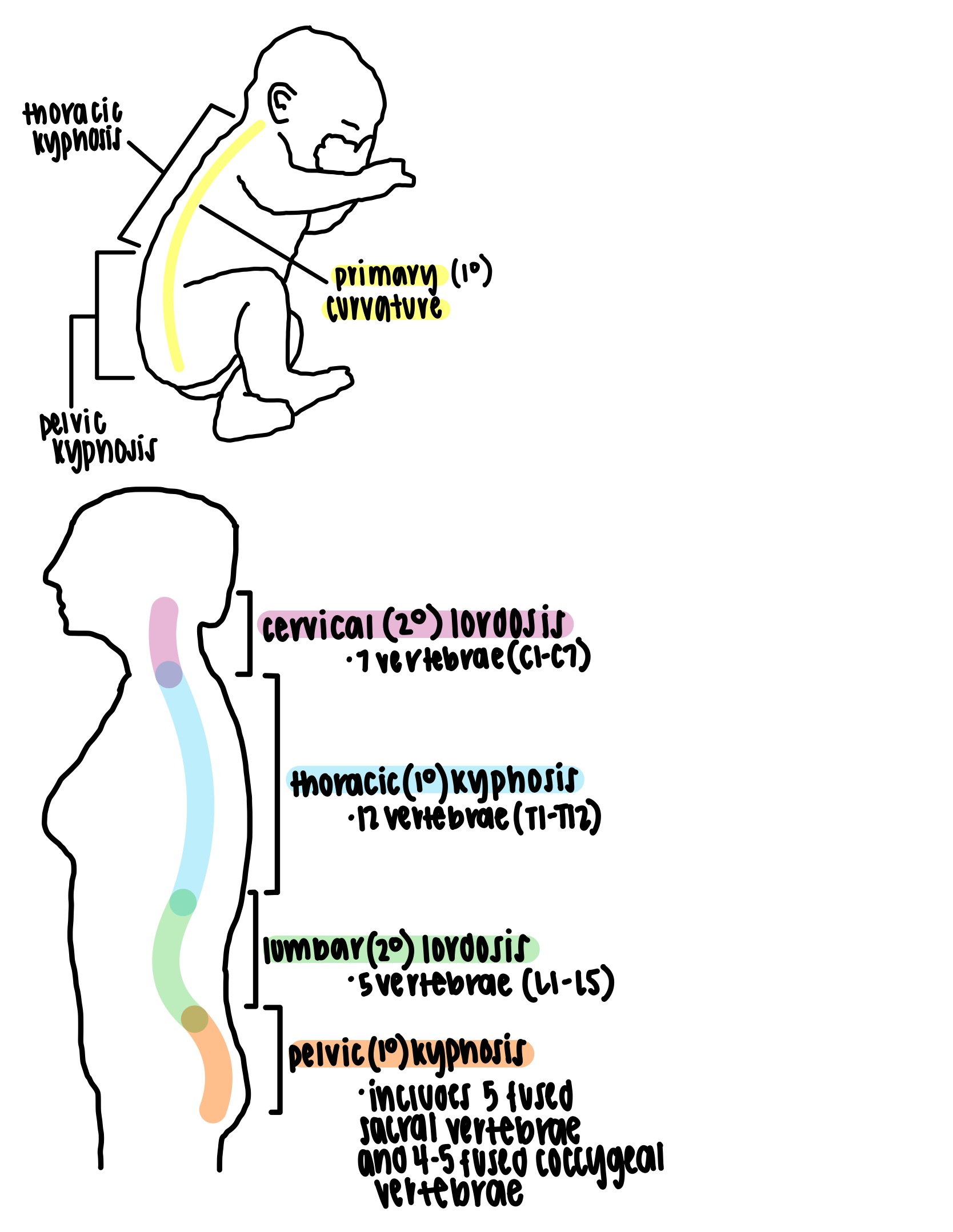
developmental curvatures of the spine
primary curvatures
present at birth
spine exhibits one continuous c shaped curve or anterior concavities (kyphoses) with thoracic and pelvic subsets
secondary curvatures
develop later - as an infant begins to crawl and lift head the cervical curvature develops and walking upright develops the lumbar curvature
spine exhibits posterior concavities (lordoses) with cervical and lumbar subsets
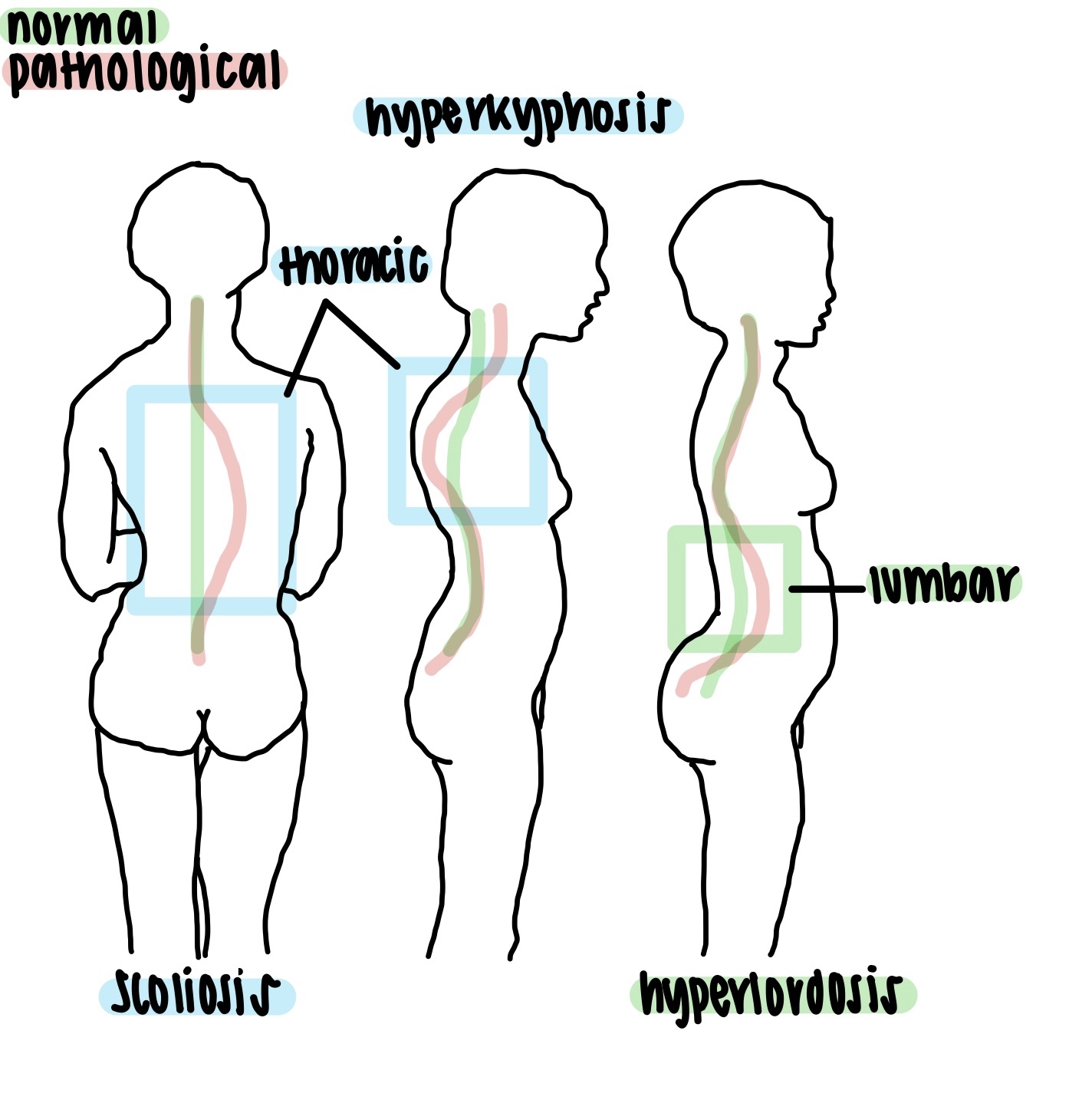
abnormal curvatures of the spine
causes -
degenerative diseases
muscle paralysis
poor posture
ergonomics
pregnancy
obesity
congenital defects
scoliosis - lateral postural drift (to the left or right)
most common abnormality
exhibits as a lateral lean with uneven shoulders
usually deviates at the thoracic level (but can also occur at the lumbar level)
more common in young girls
hyperkyphosis (hunchback) - anterior postural drift
exaggerated thoracic concavity
exhibits as anteriorly hunched shoulders
usually from osteoporosis or osteomalacia
can also be caused by wrestling or weight lifting on young and developing bodies
hyperlordosis (swayback) - posterior postural drift
exaggerated lumbar concavity that bends further anterior
exhibits as a posterior lean from the lower back that alleviates pressure on the lumbar vertebrae and compensates for increased abdominal weight
shares similar causes as hyperkyphosis
can also be caused by pregnancy or obesity
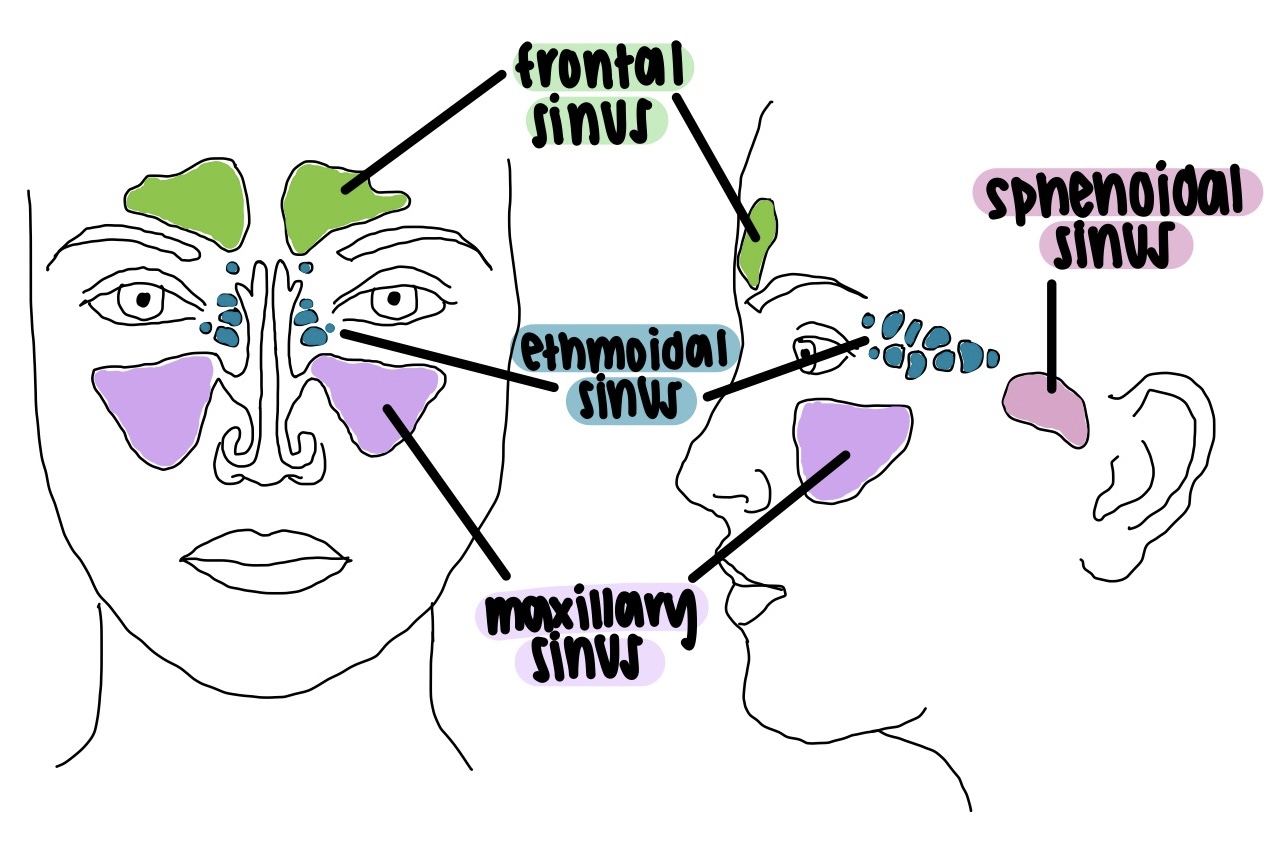
paranasal sinuses
bones containing paranasal sinuses
frontal bone (frontal sinus)
sphenoid bone (sphenoidal sinus)
ethmoid bone (ethmoidal sinus)
maxilla (maxillary sinus)
functions
connected by the nasal cavity and lined by mucous membranes
filled with air
lighten the anterior portion of the skull
act as chambers that add resonance to the voice
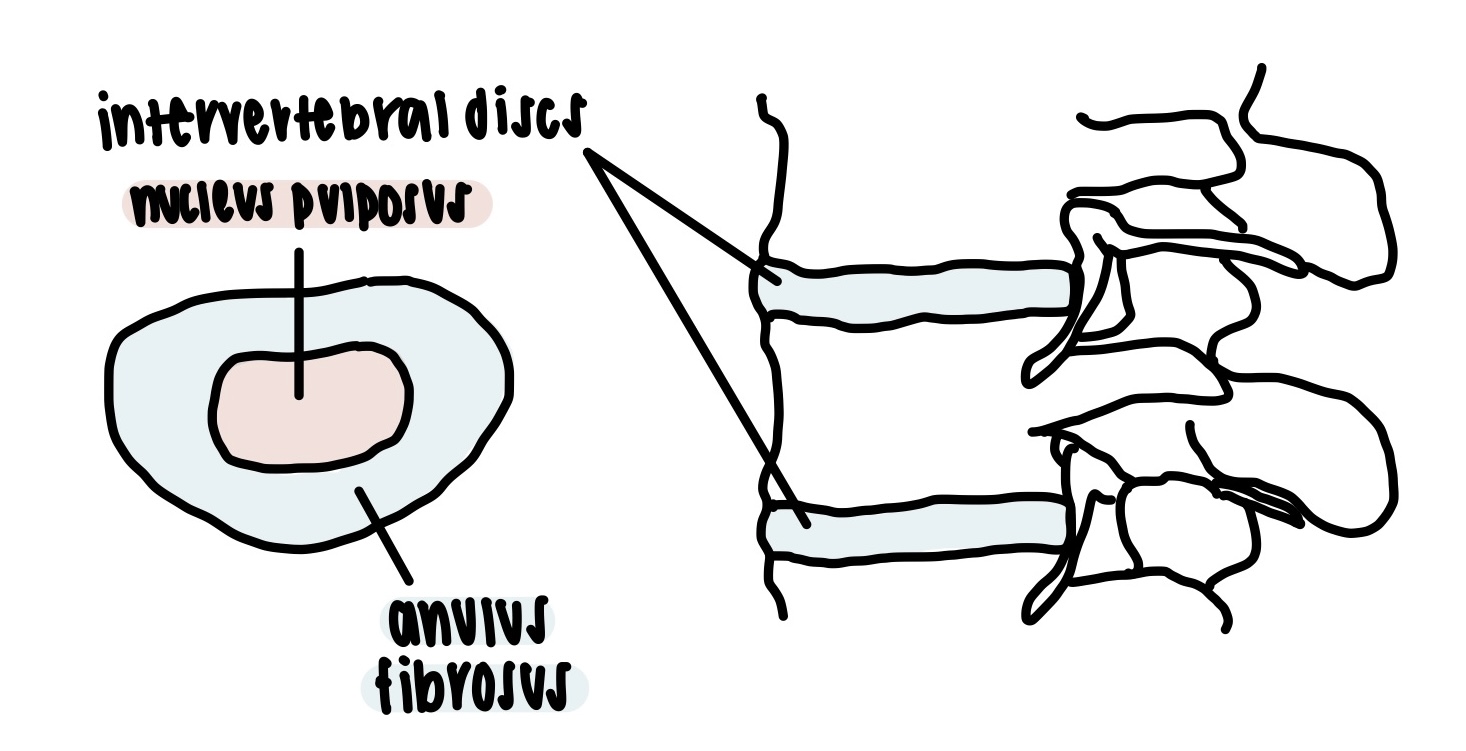
intervertebral discs
an intervertebral disc is a cartilaginous pad located between the bodies of two adjacent vertebrae
each disc consists of an inner gelatinous nucleus pulposus surrounded by a ring of fibrocartilage called the anulus fibrosus
there are twenty-three intervertebral discs with the first between C2 and C3 and the last between L5 and S1
intervertebral discs function to bind adjacent vertebrae together and support the weight of the body while allowing spinal mobility and absorbing shock
when subject to excessive stress discs can rupture (known as ruptured or herniated discs)
skeletal system functions
framework stability and support - supports the body against gravity and resistance with a rigid structure and provides scaffolding for muscles and skin
organ protection - encases vital organs (eg. central nervous system, heart, lungs, pelvic viscera, bone marrow)
movement - appendicular bones act as levers for muscle actions on limbs; breathing and neck muscles are anchored to axial bones
electrolyte balance - bone is both a storage depot and source of calcium and phosphate ions which are important for electrical and chemical currents in the tissue fluid and blood
acid and base balance - phosphate in the bone tissue buffers blood against excessive pH changes by absorbing or releasing alkaline phosphate and carbonate salts
hematopoiesis (blood formation) - red bone marrow or myeloid tissue is the chief producer of blood cells (eg. erythrocytes, leukocytes, megakaryocytes)
hormone secretion - bone cells secrete hormones that influence the secretion and action of insulin and moderate the stress response
components of the skeletal system
the living skeleton is made of active tissues that are full of cells and permeated by nerves and blood vessels
bones
organs that form the strong yet slightly flexible framework of the body
cartilage
forerunner of most bones in embryonic and childhood development
remnants of cartilage following development form articular cartilage which is hyaline cartilage without a perichondrium
articular cartilage covers interacting surfaces at the joints of mature bones
ligaments
hold bones together at the joints or articulations
general features of bones
articular cartilages
cover articular surfaces of bones in highly movable joints
allow joints to move freely with less friction which enables painless movement
most are made of hyaline cartilage and uniquely lack perichondrium (exceptions include the menisci of the knee, the pubic symphysis, and the intervertebral discs which contain tougher fibrocartilage layers that also lack a perichondrium)
are avascular and aneural which cause difficulty with healing and the lack of perichondrium prohibits the regeneration of lost tissue
these cartilages prevent osteoarthritis which is caused by wear and tear over time
nutrient foramina
small holes in surfaces of all bones that permit blood vessels and nerves to permeate, nourish, and sustain internal bone tissue
there are many small foramina per bone but there is usually one larger nutrient foramen for the main line of the nutrient artery or vein
the foramina allow passage of nutrient vessels to and from the bone marrow in the core of the bone
types of bones
flat bones
thin and curved plates that contain a spongy layer of diploe surrounded by inner and outer tables of compact bone
protect soft organs
examples include the parietal bones, the sternum, the scapula, ribs, and hip bones
long bones
longer than wide
rigid levers acted upon by muscles that are crucial for movement
examples include the humerus, radius, ulna, femur, tibia, fibula, metacarpals, metatarsals, and phalanges
short bones
approximately equal in length and width
glide across one another in multiple directions
examples include the carpals and tarsals
irregular bones
elaborate shapes that do not fit in other bone classes
examples include the vertebrae, sacrum, the sphenoid bone, and the ethmoid bone
sesamoid bones
bones developed in tendons due to stress
a particular example is the patella
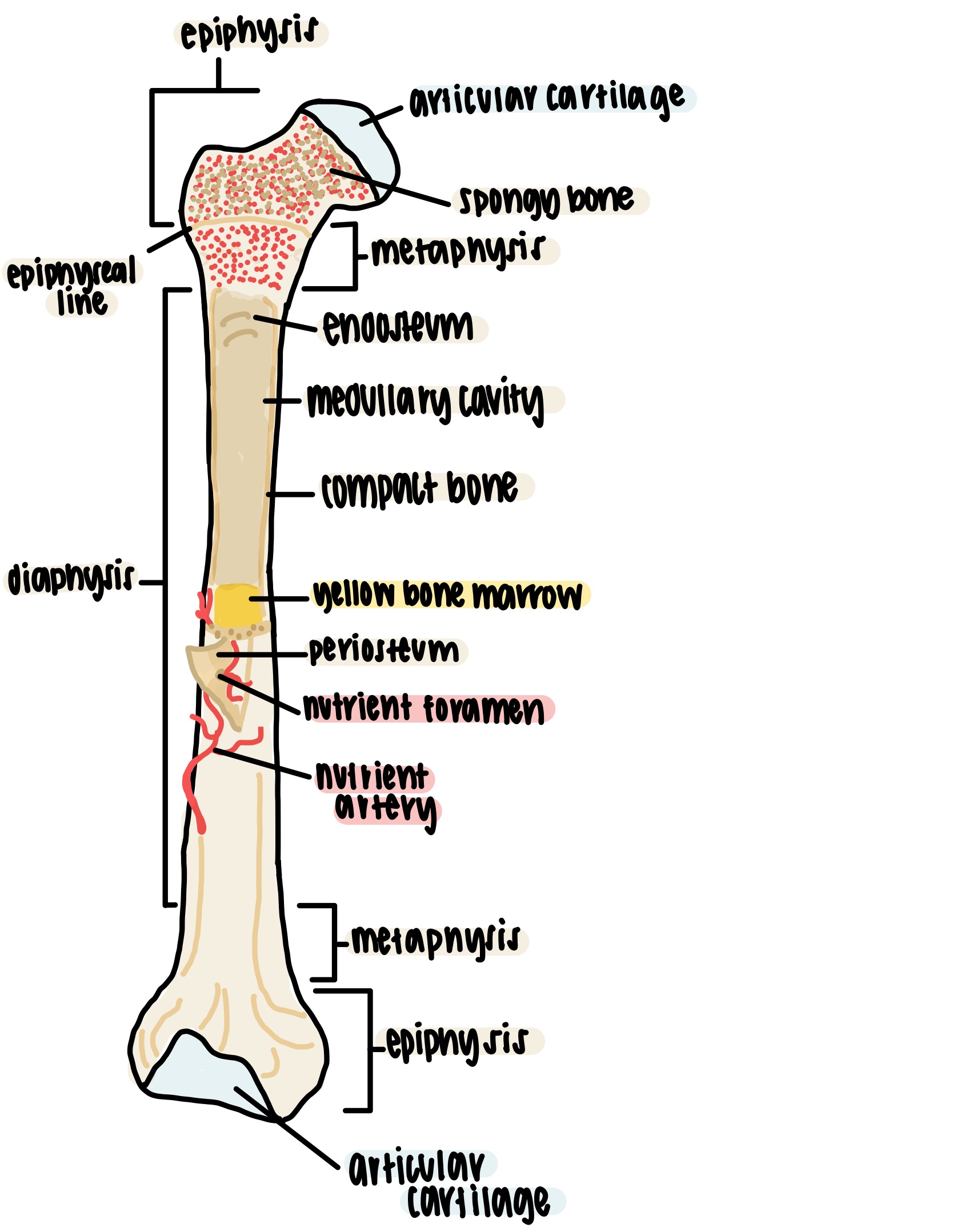
general features of long bones
diaphysis - cylinder of compact bone that provides leverage
epiphysis - enlarged ends of bone that strengthen the joint and provide added surface area for ligament and tendon attachment
epiphyseal line - slightly denser spongy bone between the epiphysis and diaphysis that is a remnant of the epiphyseal plate (areas of hyaline cartilage in the metaphysis of immature bones that enable elongation)
medullary or marrow cavity - space in the diaphysis of a long bone that contains bone marrow (mostly yellow marrow in adults)
metaphysis - area in between the diaphysis and epiphysis
periosteum - surface membrane of bone composed of two layers (an outer fibrous collagen layer and an inner osteogenic layer of osteoblasts)
endosteum - thin layer of reticular connective tissue that lines the internal marrow cavity, covers trabeculae of spongy bone, and lines the canal systems found in compact bone
compositions of bone as complex organs
bones are composed of osseous tissue which is a connective tissue with a mineralized extracellular matrix
mineralization or ossification (calcification) is the process of extracellular matrix hardening due to heavy deposition of calcium and phosphate crystals
bone organs contain various tissues (eg. osseous tissue, red bone marrow or myeloid tissue, blood, cartilage, external connective tissue, nervous tissue, yellow bone marrow or adipose tissue, and simple epithelia)
even though it appears static bone continually remodels itself and the physiology of the bones affect all other organ systems
bone membranes and their components
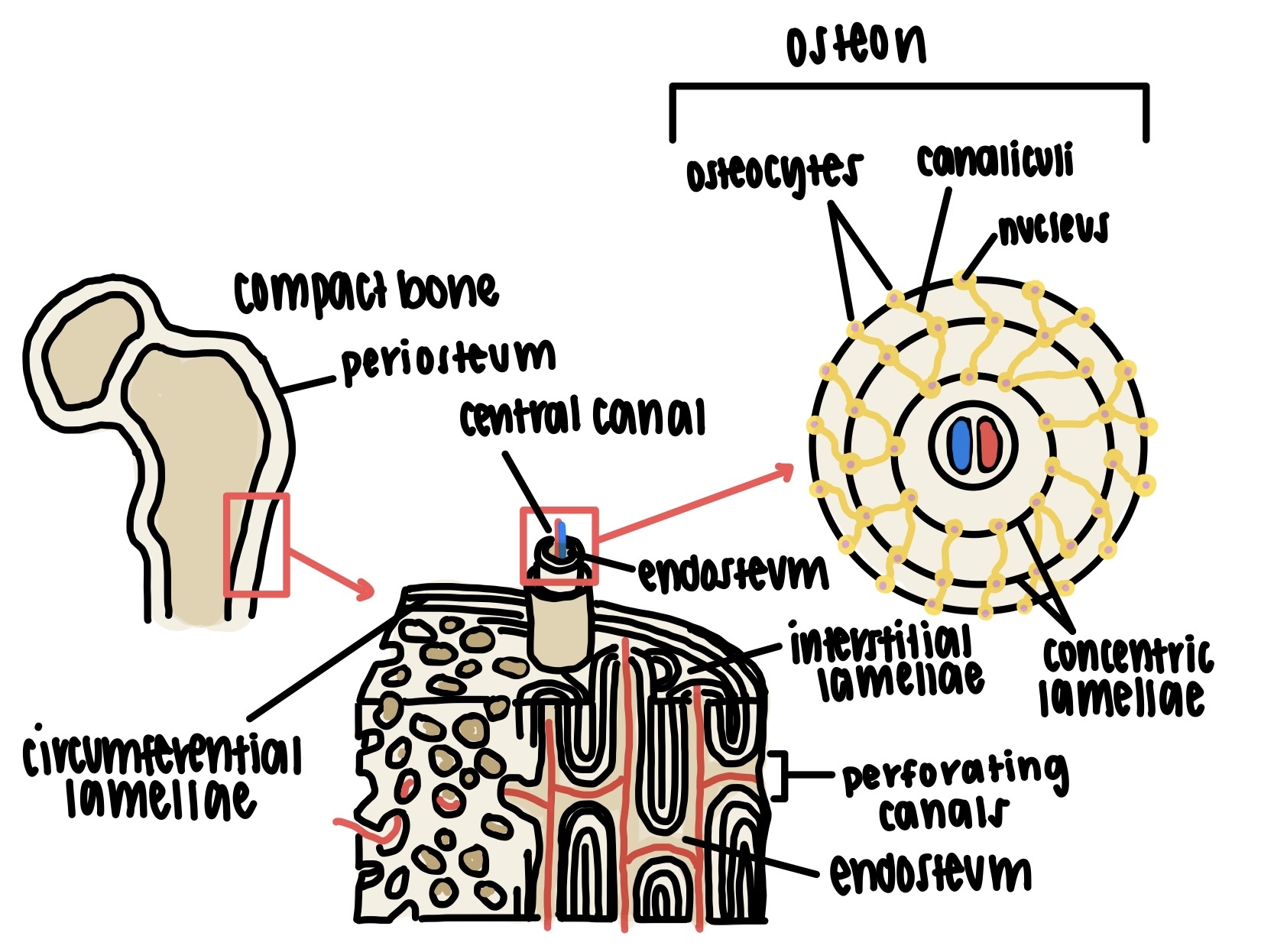
endosteum
thin reticular connective tissue lining internal bone surfaces
has cells that deposit (osteoblasts) and cells that dissolve (osteoclasts) osseous matrix
also contains hematopoietic stem cells that produce red bone marrow
found on all internal surfaces including the lining of compact bone surrounding the marrow cavity (cortical endosteum), lining of canals within compact bone osteons (osteonal endosteum), and the continuous lining of every spicule in cancellous bone (trabecular endosteum)
periosteum
dual layered external sheath that covers bone except at the articular cartilages
fibrous connective tissues of tendons and ligaments meld with the periosteum as a continuous feature
perforating or sharpey fibers penetrate into the bone matrix to provide flexibility and structural adherence which prevents delamination or tearing with injury
composed of two layers
outer fibrous layer is rich in collagen (with elastin) and vascular supplies that pass through microscopic perforating canals in bone
inner osteogenic layer contains osteoblasts which are important to thickening or circumferential growth of bone and the healing of fractures
bone cells
osteogenic or osteoprogenitor cells
derived from embryonic mesenchymal stem cells
give rise to osteoblasts and osteocytes
found in the endosteum and inner layer of the periosteum
capable of dividing and producing more bone cells and multiply continuously to produce new osteoblasts
increase osteogenesis during healing of injuries or experience of mechanical stress
osteoblasts
direct descendent of osteogenic cells
bone forming cells that synthesize a soft organic osteoid (bone like) template composed of collagen into the matrix which hardens by mineral deposition and crystallization
nonmitotic and cannot divide to form more osteoblasts
found in regenerative membranes of the endosteum and inner layer of the periosteum
contain mitochondria and endoplasmic reticula to support osteogenic role
secrete osteocalcin (allows parasympathetic nervous system to function)
osteocytes
direct descendent of osteogenic cells and osteoblasts
former osteoblasts that retire from bone formation when trapped in lacunae
interconnected by a network of canaliculi or microscopic tunnels that run through the dense mineral matrix to maintain cell viability
have cytoplasmic extensions called dendrites which project through the canaliculi and extend to other osteocytes while osteocytes close to one another communicate through gap junctions since diffusion cannot occur through bone
dissolve and deposit bony matrix in small amounts which contributes to the homeostatic regulation of bone minerals
produce biochemical relay signals to stimulate osteoblast activity when necessary
function as strain sensors as load stimulates sensory cilia on the dendrites and induces cells to secrete signals that regulate bone remodeling to adjust shape and density and adapt to stress
secrete osteocalcin (allows parasympathetic nervous system to function)
osteoclasts
descendent of leukocyte precursor cells that produce macrophages (monocytes)
bone dissolving cells
unusually large cells formed from the fusion of several cells that typically have three to four nuclei (multinucleate)
have an abundance of lysosomes that digest and break down cellular debris
have ruffled membranes that face bone surface and increase surface area for resorption efficiency
reside within pits called resorption bays
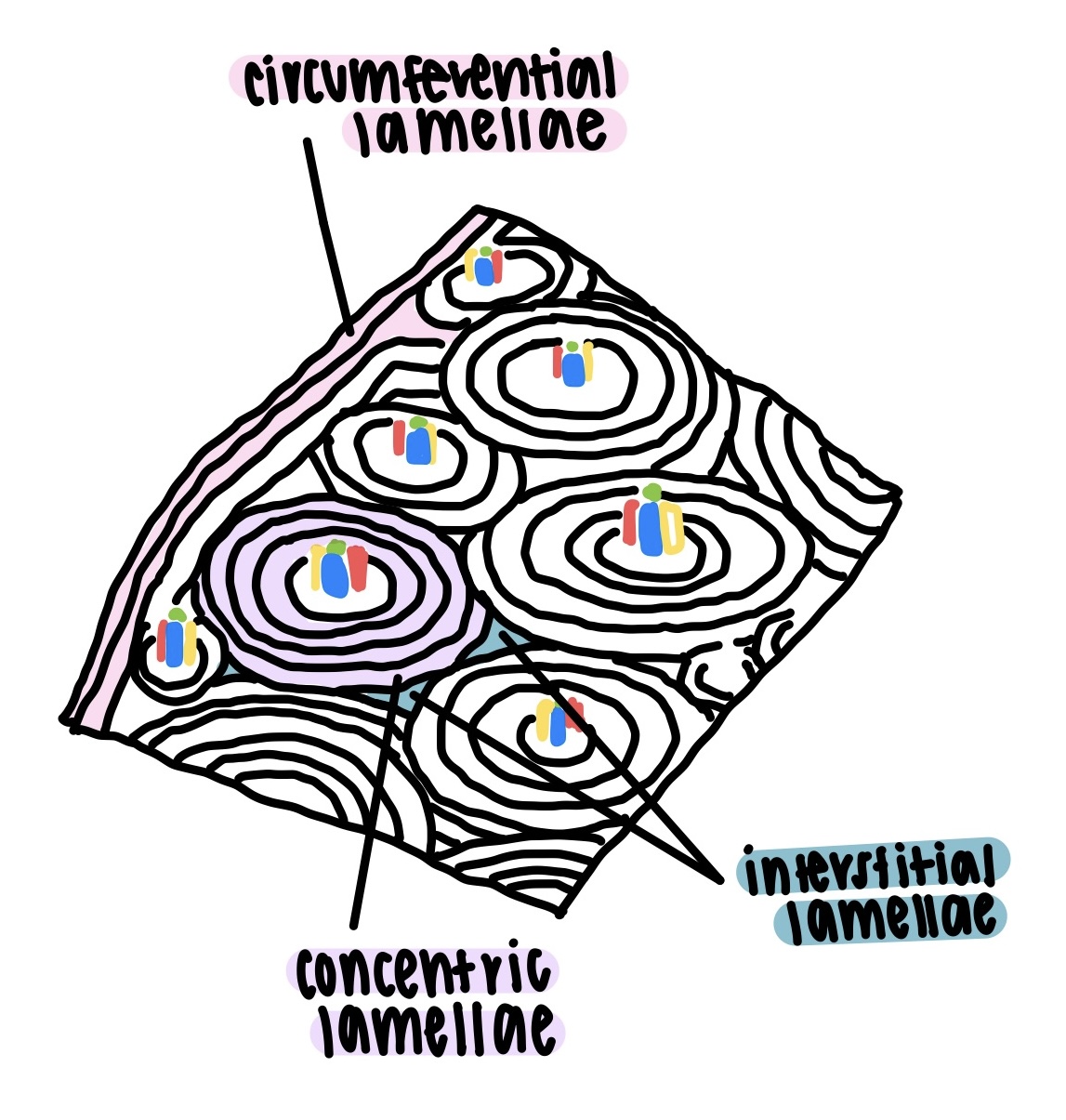
different types of lamellae
concentric lamellae
rings of matrix that surround the central canal of an osteon
interstitial lamellae
irregular regions of lamellae between osteons
circumferential lamellae
parallel layers of lamellae that form around the whole bone
components of the bone tissue matrix
matrix of osseous tissue is about ⅓ organic and ⅔ inorganic matter or minerals
bone matrix is a composite of polymer (organic) and ceramic (inorganic) components
matrix combines optimal mechanical properties of each component
organic matter
synthesized by osteoblasts
mostly collagen but includes some proteoglycans (PGs), glycosaminoglycans (GAGs), and glycoproteins
defects in collagen found in the organic matter can cause osteogenesis imperfecta or brittle bone disease which can result in serious structural problems
gives bone some degree of flexibility
bones would be brittle and prone to fracture without organic material
inorganic matter
minerals and depositions by osteoblasts
85% hydroxyapatite or crystallized calcium phosphate salt
10% calcium carbonate
5% other minerals and inorganic ions (eg. fluoride, sodium, potassium, and magnesium)
deficiencies in calcium or vitamin d can cause rickettsia in children (bones curve laterally as growth plate lacks minerals and influenced by weight) or osteomalacia in adults
structurally rigid for supporting body weight
unable to support weight and deform in shape without inorganic portion
formation of osseous tissue matrix by deposition
ossification is the detailed mineralization process that occurs in all bone tissue formation in which hydroxyapatite (calcium phosphate) and other ions are taken from the blood plasma and deposited in osteoid tissue as crystallized salts
begins in fetal ossification and continues throughout life
osteoblasts produce collagen fibers (collagenous template) that spiral the longitudinal length of the osteon and form osteoid tissue (precursor to mineralized tissue)
osteoblasts then absorb calcium and phosphate from the blood to synthesize hydroxyapatite
osteoblasts export hydroxyapatite minerals into the matrix when accumulation exceeds solubility limits (levels reach the solubility product and minerals precipitate out of solution)
minerals accumulate and cause crystals to precipitate from solution and encrust collagen fibers and serves as seed crystals for the continuing deposition of more inbound calcium phosphate crystals
this causes a brief positive feedback loop of crystallization that occurs until the bone tissue matrix is stuffed with dense mineral lattices and no more blood or other fluid can flow through the tissue
abnormal bone tissue ossification is referred to as ectopic ossification and occurs in other organs (eg. lungs, brain, eyes, muscles, tendons, arteries) which creates calculi or hardened mineral masses in an otherwise soft organ
types of osseous tissue
compact (dense or cortical) bone
dense outer shell of bone
covers cancellous bone
cancellous (spongy) bone
loosely organized bone tissue
found in the center of epiphyses and center of diaphyses of long bones and in the middle of nearly all others
called diploe in flat bones
covered by durable compact bone
are cancellous and compact bone really that different?
compact and cancellous bone are composed of the same osseous tissue cells in similar arrangements but cancellous bone has more surrounding space which decreases strength
osteocytes do not need central canals of regular osteons
mineral spines or spiculus join to form trabeculae (thin plates of osseous tissue) meshwork deep to compact bone
this porous cancellous bone structure lightens the load and increases mobility for survival, houses red bone marrow, increases surface area that is lined with endosteum and contributes a rich blood supply for easy access to donate and accept minerals from the blood for bone remodeling
trabecular plates are adaptive and develop greater densities along lines of mechanical stress (referred to as wolffs law)
composition and function of osseous tissue
osseous tissue in compact bone is organized into units called osteons (haversian systems)
osteons (haversian systems) consist of a central (haversian) canal that contains nerves and vasculature
central (haversian) canals (lined with endosteum) are surrounded by rings of matrix called concentric lamellae
perforating canals (lined with endosteum) pass between adjacent osteons and provide entry points for small blood vessels from the bone surface
young osteoblasts form the osseous matrix then become osteocytes that maintain the tissue in lamellae and survive by gap junctions and the canaliculi network
types and functions of bone marrow
bone marrow is soft tissue that occupies the marrow cavity of a long bone, the spaces amid the trabeculae of spongy bone, and the larger central canals
red marrow (myeloid tissue) - 50%
in nearly every bone in children
remains in the skull, vertebrae, ribs, sternum, os coxae, proximal heads of humerus, and femur in adulthood (axial skeleton)
composed of hematopoietic tissue which produces blood cells from stem cells
important for erythrocyte turnover
the transition from fetal to adult hemoglobin can cause jaundice as bilirubin is a byproduct of hemoglobin breakdown
yellow marrow (adipose tissue) - 50%
found in adults
long bone shafts contain yellow marrow
no longer produces blood cells
mainly used for energy reserves
yellow can revert to red to severe states of blood loss (eg. severe or chronic anemia)
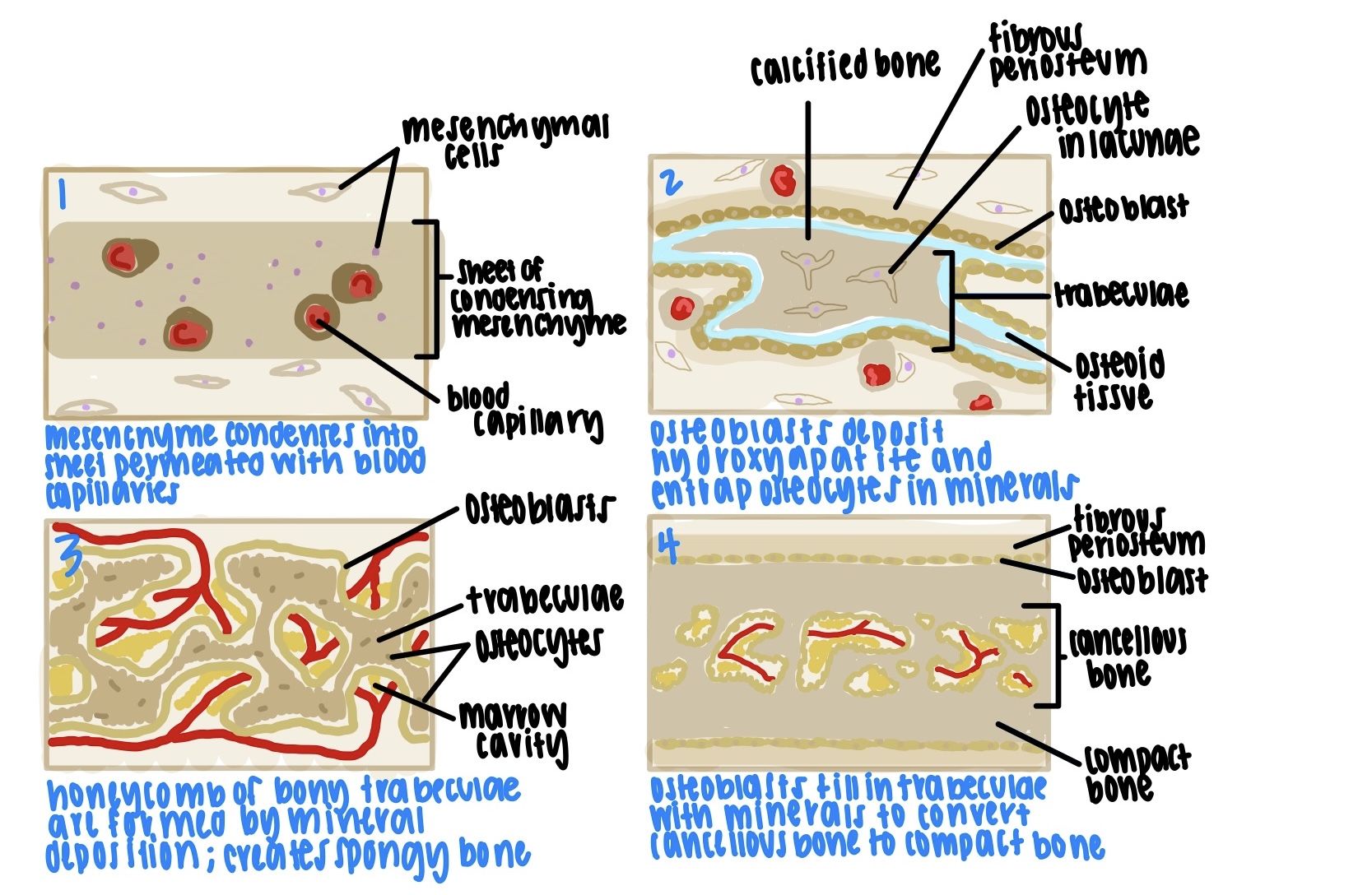
intramembranous ossification
development of bones from an embryonic template
happens quickly and early in development
occurs in the axial skeleton and most flat bones (eg. skull, ribs, sternum)
does not require a cartilage template
forms in fibrous connective tissues
occurs directly in the mesenchyme
develops inside to out
mesenchyme condenses into a soft sheet of tissue that is permeated with blood vessels and capillaries
mesenchymal cells align with the blood vessels and become osteoblasts then secrete soft collagenous osteoid tissue away from the vessels
osteoblasts deposit hydroxyapatite and other minerals on the osteoid tissue to harden the matrix
blood vessels and capillaries are compressed by minerals and osteoblasts become osteocytes in lacunae as cell bodies are surrounded by calcified matrix and periosteum begins to form
mesenchyme adjacent of the developing bone condenses and forms a fibrous periosteum on each surface and the cancellous bone becomes a honeycomb of trabeculae
osteoblasts beneath the periosteum deposit layers of bone and fill in the spaces between trabeculae
osteoblasts create a zone of compact bone on each side and thicken the bone overall while maintaining cancellous bone in the middle layer
EVERY - EMBRYONIC TEMPLATE
CHILD - CONDENSED MESENCHYME
OFTEN - OSTEOBLASTS DEPOSIT MINERALS
THROWS - TRABECULAE FORM
FITS - FILL IN TRABECULAE
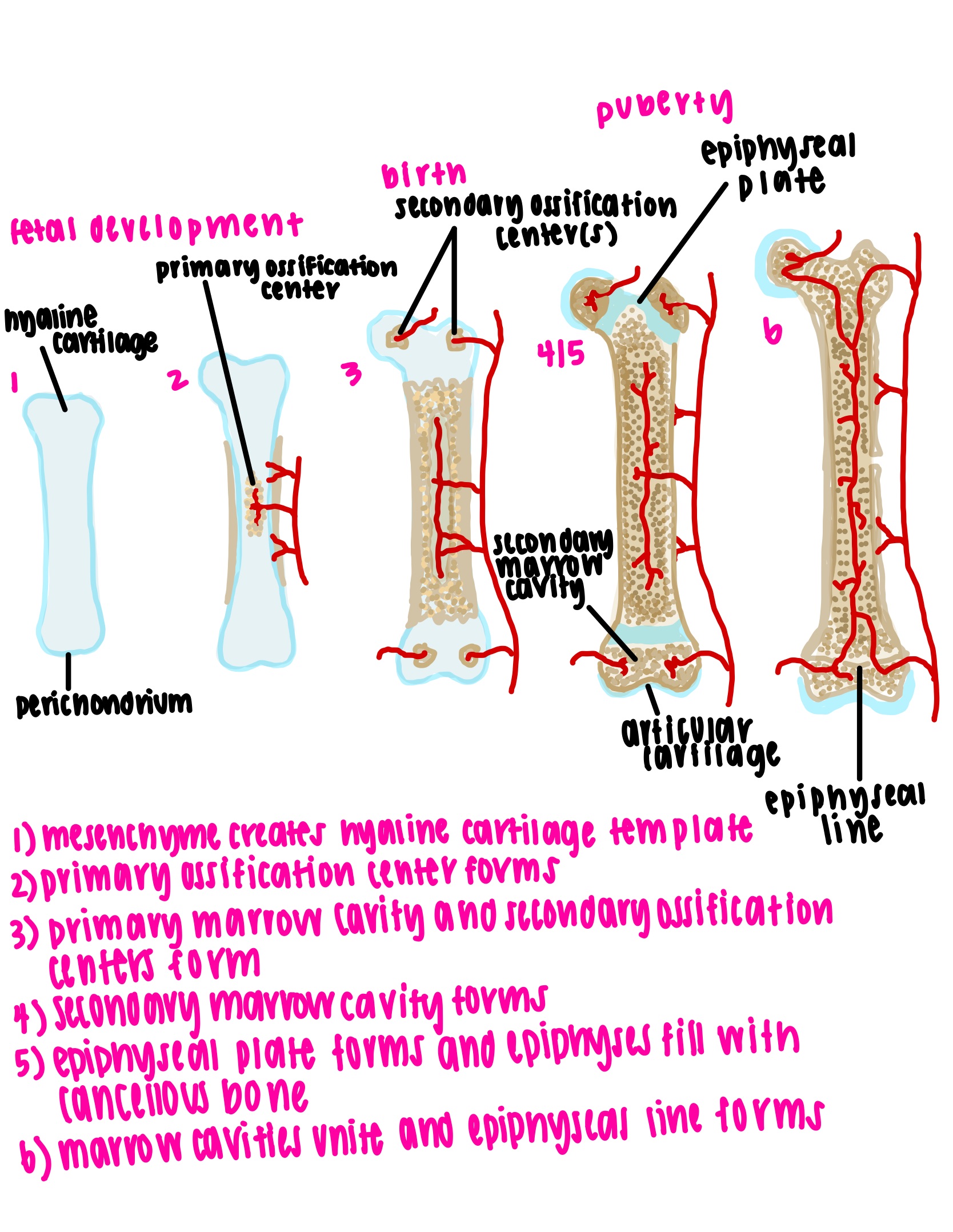
endochondral ossification
development of bones from a cartilage template
begins during fetal development and continues throughout life
requires cartilaginous model
occurs in the appendicular skeleton and most long bones (eg. limbs)
hyaline cartilage template is calcified into osseous tissue
is an interrupted procedure with a long delay
mesenchyme differentiates into a template of hyaline cartilage with a perichondrium that produces chondrocytes
the primary ossification center in the middle of the cartilage forms (diaphysis) and the perichondrium begins to produce osteoblasts (chondrocytes become osteoblasts through differentiation)
osteoblasts deposit a thin collar of bone around the middle of the cartilage model and the perichondrium is considered periosteum
primary ossification center is invaded with vasculature and turns into the primary marrow cavity and the secondary ossification center appears at the end of the cartilage model (epiphysis)
the marrow cavity is created by osteoclasts from blood vessels that digest calcified tissue and osteoblasts continue to thicken the bony collar as osteoclasts dissolve calcified cartilage
(at birth) secondary ossification center turns into the secondary marrow cavity that expands outward
primary marrow cavity continues to enlarge
(childhood) epiphyses fill with cancellous bone and ossification is suspended until puberty as an epiphyseal plate is formed
the epiphyseal plate is a thin wall of cartilage that separates the primary and secondary marrow cavities (metaphysis) which persists through childhood and serves as a growth zone for bone elongation during puberty (eventually turn into epiphyseal lines in adults which mark where the plates used to be)
(adulthood) cartilage in the epiphyseal plate is consumed to form the epiphyseal line (the bone can no longer grow in length) and primary and secondary marrow cavities unite
the gap between the epiphysis and diaphysis closes
remnant cartilage at the ends of formed bones become the articular cartilages covering each joint surface
CHILDREN - CARTILAGE TEMPLATE
HAVE - HYALINE CARTILAGE MODEL
PROBLEMS - PRIMARY OSSIFICATION CENTER
PRESENTING - PRIMARY OSSIFICATION CAVITY
SOME - SECONDARY OSSIFICATION CENTER
SAVINGS - SECONDARY OSSIFICATION CAVITY
EACH - EPIPHYSEAL PLATE
EVENING - EPIPHYSEAL LINE
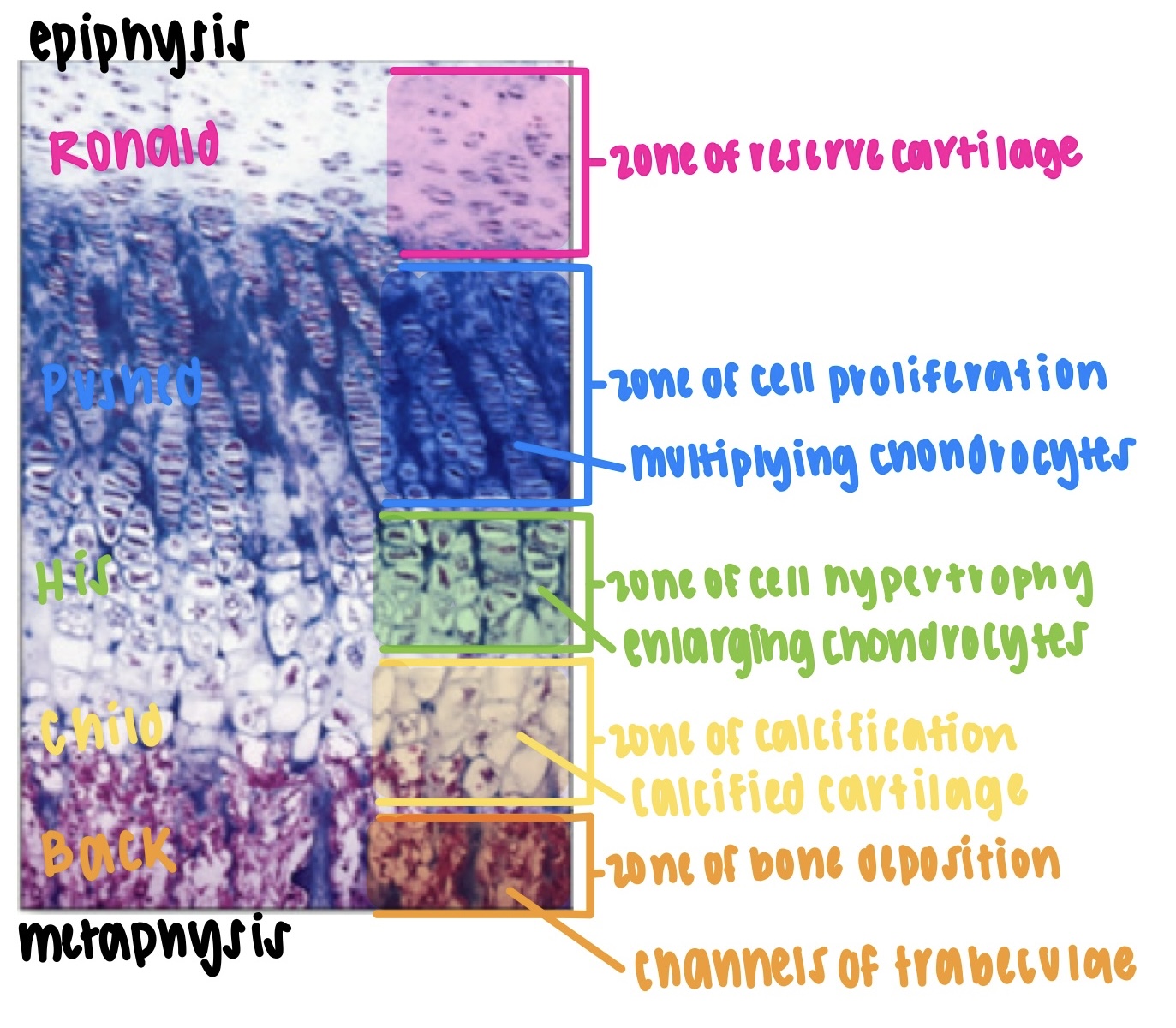
interstitial growth or bone elongation
occurs during young life (early twenties)
due to cartilage hyperplasia and hypertrophy within the epiphyseal plate
epiphyseal plates close when the cartilage is exhausted and lengthwise growth is finished
zone of reserve cartilage
region farthest from the marrow cavity
consists of typical hyaline cartilage with resting chondrocytes
zone of cell proliferation (hyperplasia)
chondrocytes multiply
consists of longitudinal columns of flattened lacunae
zone of cell hypertrophy (hypertrophy)
chondrocytes stop multiplying and begin to enlarge
walls of the lacunae thin
zone of calcification
minerals are deposited in the matrix between the columns of lacunae
cartilage calcifies
zone of bone deposition
lacunae break down and chondrocytes die by apoptosis
chondrocyte death converts columns into longitudinal channels which are invaded by blood vessels and marrow from the marrow cavity
osteoblasts line up along the walls of the channels and deposit concentric lamellae of matrix while the osteoclasts dissolve the temporary calcified cartilage
this creates a region of cancellous bone at the end of the marrow cavity facing the metaphysis and this bone remains for life
around the perimeter of the marrow cavity continual ossification converts the cancellous bone to compact bone (osteoblasts deposit bone matrix layers that become concentric lamellae of an osteon)
RONALD - RESERVE CARTILAGE
PUSHED - PROLIFERATION
HIS - HYPERTROPHY
CHILD - CALCIFICATION
BACK - BONE DEPOSITION
appositional growth or bone thickening
increase in width throughout life
occurs by deposition of new bone at the surface
osteoblasts on the deep osteogenic layer of periosteum undergo intramembranous ossification depositing osteoid tissue against compact bone
tissue calcifies and osteoblasts become osteocytes
if this occurs in parallel layers to the surface then circumferential lamellae are formed
if adjacent blood vessels in the periosteum are enveloped by a ring of new osteoid tissue then new osteons with concentric lamellae can form
osteoblasts beneath the periosteum deposit bone to form ridges around a blood vessel
the blood vessel lays in a groove between the ridges
the groove is transformed into a tunnel when the bone built on the adjacent ridges meet
the periosteum of the groove becomes the endosteum of the tunnel
osteoblasts from the endosteum deposit bone to form new concentric lamellae
the production of additional concentric lamellae fills in the tunnel and completes the formation of a new osteon
bone remodeling and mineral homeostasis
bone remodeling functions to repair microfractures, release minerals into the blood when needed, and reshape bone in response to use and disuse
wolffs law of bone : architecture of the bone is determined by the mechanical stresses placed on it
remodeling is a collaborative and precise action of osteoblasts and osteoclasts that are controlled by hormones
bony processes grow larger in response to mechanical stress
if more blood cells are needed then osteoclasts can dissolve trabeculae to widen the marrow cavity
pagets disease is caused by abnormal bone remodeling
a mature bone remains a metabolically active organ as it is involved in own maintenance of growth and remodeling
mature bone exerts a profound influence over the rest of the body by exchanging minerals with tissue fluid (eg. abnormal blood calcium disrupts the function of other organ systems especially the nervous and muscular tissues)
mineral resorption mechanism by osteoclasts
mineral resorption involves the dissolving of bone minerals for release into the bloodstream
hydrogen pumps in osteoclast membranes secrete hydrogen ions into the space between the cell and the bone surface which decreases the pH (< 4)
mineral crystals dissolve at a low and acidic pH
acid phosphatase is an enzyme that digests collagen when activated
importance of body calcium outside of bones in other systems
calcium imbalances are much more common than conditions related to phosphate although they are both vital and essential elements in living organisms
calcium is needed in neuron communication, muscle contraction, blood clotting, and exocytosis
there is approximately one kilogram of calcium in the adult body (99% in the skeleton)
there should be a normal calcium concentration in blood plasma (45% is ionized calcium which readily diffuses across capillary walls to affect other tissues while 55% is reserved calcium that is bound to plasma proteins and is electrically neutral)
calcium minerals are deposited into the skeleton and withdrawn when needed for other purposes
importance of body phosphate outside of bones in other systems
phosphate is a component of DNA, RNA, ATP, phospholipids, and biological pH buffers
the average adult has 500 to 800 g of phosphorus (85 to 90% is in the bones)
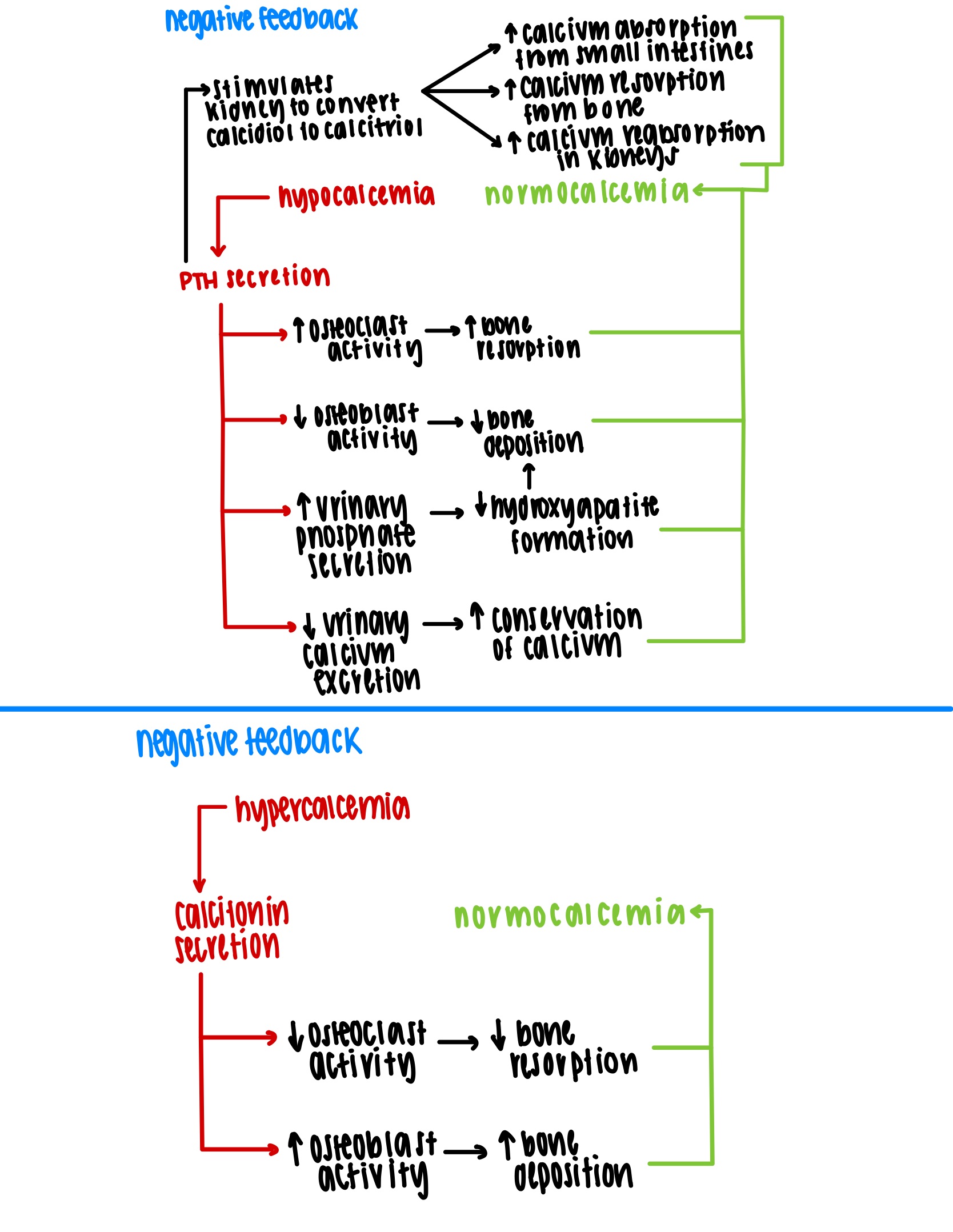
calcium homeostasis and hormonal regulation of bone mineral density
calcium homeostasis depends on a balance between intake, urinary and fecal losses, and exchanges between osseous tissue
calcium homeostasis is regulated by three hormones including (1) calcitriol or vitamin D3, (2) calcitonin, and (3) parathyroid hormone
these three hormones maintain normocalcemia
hypocalcemia (low calcium in the blood)
has a wide variety of common causes but body calcium deficiency is not one of them
causes include vitamin d deficiency, diarrhea (inability to absorb calcium because movement through the digestive tract is too quick), thyroid tumors, underactive parathyroids (hypoparathyroidism), pregnancy and lactation (second demand for calcium usage causes gestational or maternal hypocalcemia), and accidental removal of parathyroid glands during thyroidectomy surgery
calcitonin (an off switch for blood calcium)
has regular effects but appears to have become unnecessary in adult humans for normocalcemia
can be beneficial in children (high osteoclast activity) and pregnant or lactating women
can also treat pagets disease (aberrant bone remodeling)
secreted by cells of the thyroid gland and is released in response to hypercalcemia (high calcium in the blood)
lowers blood calcium concentration by (1) osteoclast inhibition (reduces osteoclast activity by as much as 70% and reduces the amount of calcium liberated from the bones) and (2) osteoblast stimulation (increases the number and activity of osteoblasts and increases calcium deposition into the skeleton)
parathyroid hormone (an on switch for blood calcium)
secreted by the parathyroid glands and is released in response to hypocalcemia
raises calcium blood level through various mechanisms such as (1) increasing osteoclast population, (2) decreasing osteoblast activity, (3) promoting calcium reabsorption from filtrate in the kidneys which prevents loss of calcium in the urine and reintroduces calcium to blood, and (4) promoting the synthesis of calcitriol
calcitriol (1,25 dihydroxyvitamin d3)
an activated form of vitamin d produced by the sequential action of the skin, liver, and kidneys
raises blood calcium concentration
greatly enhances calcium absorption in small intestines
increases calcium resorption from bone
promotes kidney reabsorption of calcium
without calcitriol children develop rickettsia and adults develop osteomalacia as vitamin d is essential for the adequate retrieval of dietary calcium and phosphate
osteoporosis
the most common bone disease caused by severe loss of bone mineral density (particularly in the cancellous bone since it remodels frequently)
bones lose mass and become brittle due to loss of organic matrix and minerals
pathological fractures of the hip, wrist, and vertebral column are common
often causes immobility which can lead to thrombosis and/or pneumonia
estrogen maintains bone density in both sexes and inhibits osteoclast activity
in men the adrenal glands produce the most estrogen
in postmenopausal women rapid bone loss occurs since the ovaries cease to secrete estrogen (more dangerous for women sooner than men because of this)
young female athletes with low body fat become amenorrheic due to low ovarian estrogen secretion and this loss of estrogen can lead to osteoporosis and the high mechanical stress placed on the body can lead to fractures and incapacitation
there are various clinical treatments include estrogen replacement therapy (slows bone resorption but increases risk of breast cancer, stroke, and heart disease) and forteo (parathyroid hormone derivative that slows bone loss and builds new bone but promotes bone cancer) as well as safer therapeutics including fosamax and actonel (destroy osteoclasts)
the best treatment for osteoporosis is prevention which starts with a good bone-building diet during the early years and between ages 25 and 40
other bone disorders
osteitis deformans or pagets disease
excessive proliferation of osteoclasts and resorption of excess bone with osteoblasts attempting to compensate by depositing extra bone
results in rapid and disorderly bone remodeling and weak or deformed bones
usually passes unnoticed but can sometimes cause pain and disfiguration as well as fractures
most common in males over the age of fifty
osteomyelitis
inflammation of osseous tissue and bone marrow as a result of bacterial infection
often fatal and is very difficult to treat
osteogenesis imperfecta or brittle bone disease
defect in collagen deposition that renders bones exceptionally brittle
results in fractures present at birth or occurring with extraordinary frequency during childhood
can cause tooth deformity and hearing loss due to deformity of the middle ear bones
results from mutation of any several of the collagen genes
osteosarcoma or osteogenic sarcoma
most common and deadly form of bone cancer
occurs most often in the tibia. femur, and humerus of males between the ages of 10 and 25
can metastasize to the lungs or other organs (in 10% of cases)
death typically occurs within one year if left untreated
achondroplastic dwarfism
condition in which the long bones of the limbs stop growing in childhood while the growth of other bones are unaffected
results in short stature but normal sized head and trunk
results from a failure of cartilage growth (failure of metaphysis chondrocytes in the zones of cell proliferation and hypertrophy to multiply and enlarge)
results from a spontaneous mutation that can arise anytime that DNA is replicated
the integument
the integumentary system consists of the skin and accessory organs including the hair, nails, and cutaneous glands
the integument is the largest and heaviest organ
skin can be thick or thin
thin skin covers most of the body and contains hair follicles (regardless of hair growth), sebaceous glands, and two types of sudoriferous glands (merocrine and apocrine) as well as some specialized glands
thick skin is rarer and only found in the palms, soles, palmar side (hand), and plantar side (foot) of digits as it lacks hair follicles and sebaceous glands while only containing one type of sudoriferous gland (merocrine)
serves as a barrier of resistance against trauma and infection by keratin (tough and fibrous protein that aggregates in most skin cells as keratinocytes in order to provide an anti-abrasive physical layer) and an acid mantle (sebaceous glands release sebum into the lumen of hair follicles and sudoriferous glands release moisture through the follicles or pores; the sebum and moisture combine to produce an acidic and oily mixture that traps and kills most pathogens) but the skin also has epidermal tight junctions that prevent crossing of pathogens and the dermis is an immune system surveillance region that can contain pathogens
doubly waterproofed as glycolipids on the surface of the skin form a two-way barrier preventing dehydration and dilutional hypervolemia or water intoxication
mitigates damage and protects the skin from ultraviolet radiation (melanin pigments migrate apically to disperse UV light away from living cells; melanin synthesis in basal melanocytes is a homeostatic response to UV exposure; darker skin indicates higher melanocyte activity and thus protects more effectively)
performs vitamin d synthesis (UV radiation catalyzes a critical step in the synthesis of vitamin d within the epidermis)
allows for sensation (largest sense organ that constantly informs the conscious mind of environmental conditions)
allows for thermoregulation (thermoreceptors in the skin control local changes such as hair position, blood flow changes, and perspiration control to regulate heat preservation or dissipation)
the makeup of the skin
composed of two layers including the (1) epidermis (keratinized stratified squamous epithelium) and the (2) dermis (broad connective tissue layer with areolar and dense irregular layers)
the hypodermis (adipose connective tissue) is found below the dermis and is not considered a part of the integument
epidermis
most superficial layer of skin
composed of keratinized stratified squamous epithelium
dermis
middle layer of skin
composed of collagen with some elastic and reticular fibers as produced by fibroblasts
hypodermis
mostly adipose tissue and blood vessels
thin wisps of collagen are present as they loosely tether adipocyte clusters together
function to pad the body (absorb shock and protect large resident blood vessels) and serve as an energy reservoir while also providing for thermoregulation and insulation
drugs are introduced into the hypodermis by injection as the layer is thick and highly vascular for effective systemic absorption
the epidermis
composition
composed of keratinized stratified squamous epithelium
the apical dead cells are packed with keratin and held together by glycolipid layers and desmosomes that formed while living
the living portions are avascular and rely on diffusion from vasculature beneath the basal lamina
epidermal (rete) pegs interdigitate with dermal papillae to increase nourishment and sanitation effectiveness
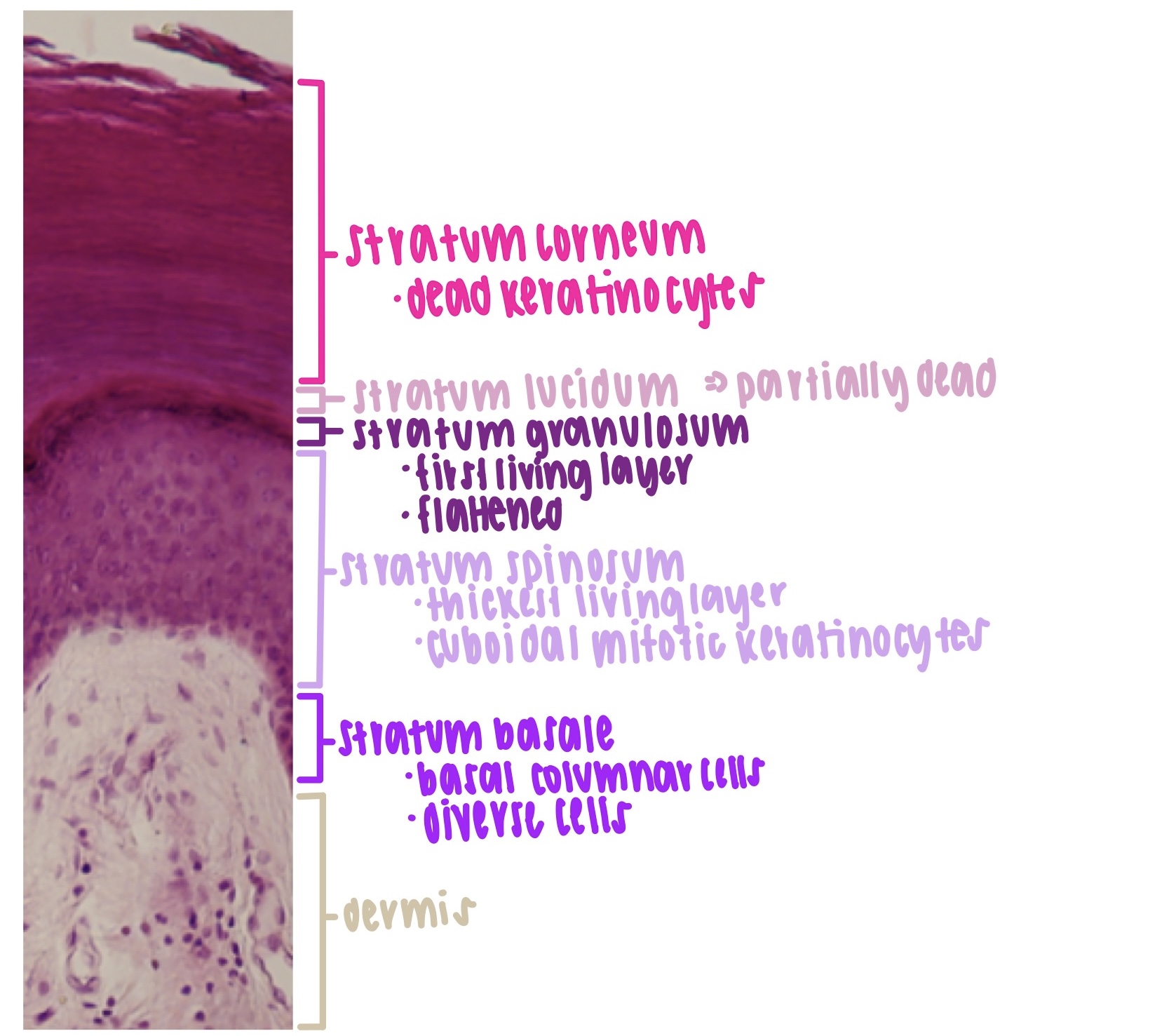
layers of the epidermis
stratum corneum
most superficial or apical stratum (dead keratinocytes)
contains up to thirty rows of dead, scaly, keratinized cells (keratinocytes)
resistant to abrasion, penetration, and water loss
forms a durable, disposable surface layer
cells are joined by corneodesmosomes that formed while living
apical cells exfoliate as dander and are replaced from below
stratum lucidum
present in both thin and thick skin but only visible in thick skin
thin translucent zone superficial to the stratum granulosum
zone of incomplete keratinization as partially keratinized dead keratinocytes appear translucent just deep to the stratum corneum
stratum granulosum
first living layer (oldest keratinocytes)
consists of three to five rows of flattened but living keratinocytes
apical most living cells in epidermis that synthesize and secret glycolipid water barrier
keratin filaments are crosslinked to increase cell rigidity and durability
easily visibly by dark keratohyalin granules
stratum spinosum
thickest living later (second thickest in thick skin but first thickest in thin skin)
migratory layer of living keratinocytes and dendritic cells
as keratinocytes migrate apically more keratin filaments aggregate and cause progressive flattening toward the surface (loss of cytoplasm and long filaments lead to spiny appearance)
deepest cuboidal keratinocytes remain capable of mitosis
stratum basale
deepest stratum (youngest keratinocytes)
single row of basal and mostly columnar cells
most diverse layer of epidermal strata containing stem cells, tactile or merkel cells, melanocytes, and living keratinocytes resting on the basal lamina and anchored by hemidesmosomes (adjacent cells adhere tightly together with desmosomes)
melanogenesis and deposition occurs
keratinocytes receive migratory orders
tactile cells are stimulated
cells of the epidermis
precursor or stem cells
perpetually dividing cells that differentiate into keratinocytes
reside and remain in the stratum basale
replenish lost keratinocytes on a continuous basis
keratinocytes
great majority of epidermal cells
synthesize keratin for barrier protection
migrate apically and die for the greater good
melanocytes
synthesize melanin to shield DNA from damaging ultraviolet light
remain in stratum basale and secrete melanin in melanosomes for deposition in nearby keratinocytes
do not migrate and divide slower (live longer) than keratinocytes
tactile or merkel cells
basal cells that transduce fine touch stimulation to dermal nerve fibers residing in the stratum basale
dendritic or langerhans cells
immune surveillance cells with phagocytic activity
interspersed with living keratinocytes in the stratum spinosum
the dermis
composition
composed mainly of collagen with some elastic fibers and reticular fibers all produced by fibroblasts
well supplied with microvasculature or small blood vessels
contain resident sweat glands, sebaceous glands, and touch receptors
dermal papillae interdigitate with epidermal (rete) pegs to increase nourishment and sanitation effectiveness
contains hair follicles and nail roots
hair follicles are invaginated epidermis and small smooth muscles called arrector pili are associated with each hair follicle which allows for contraction in response to the cold, fear, or tactile stimulation
sudoriferous (sweat) gland bodies reside in deep reticular dermis
sebaceous glands reside in dermis and empty into hair follicles
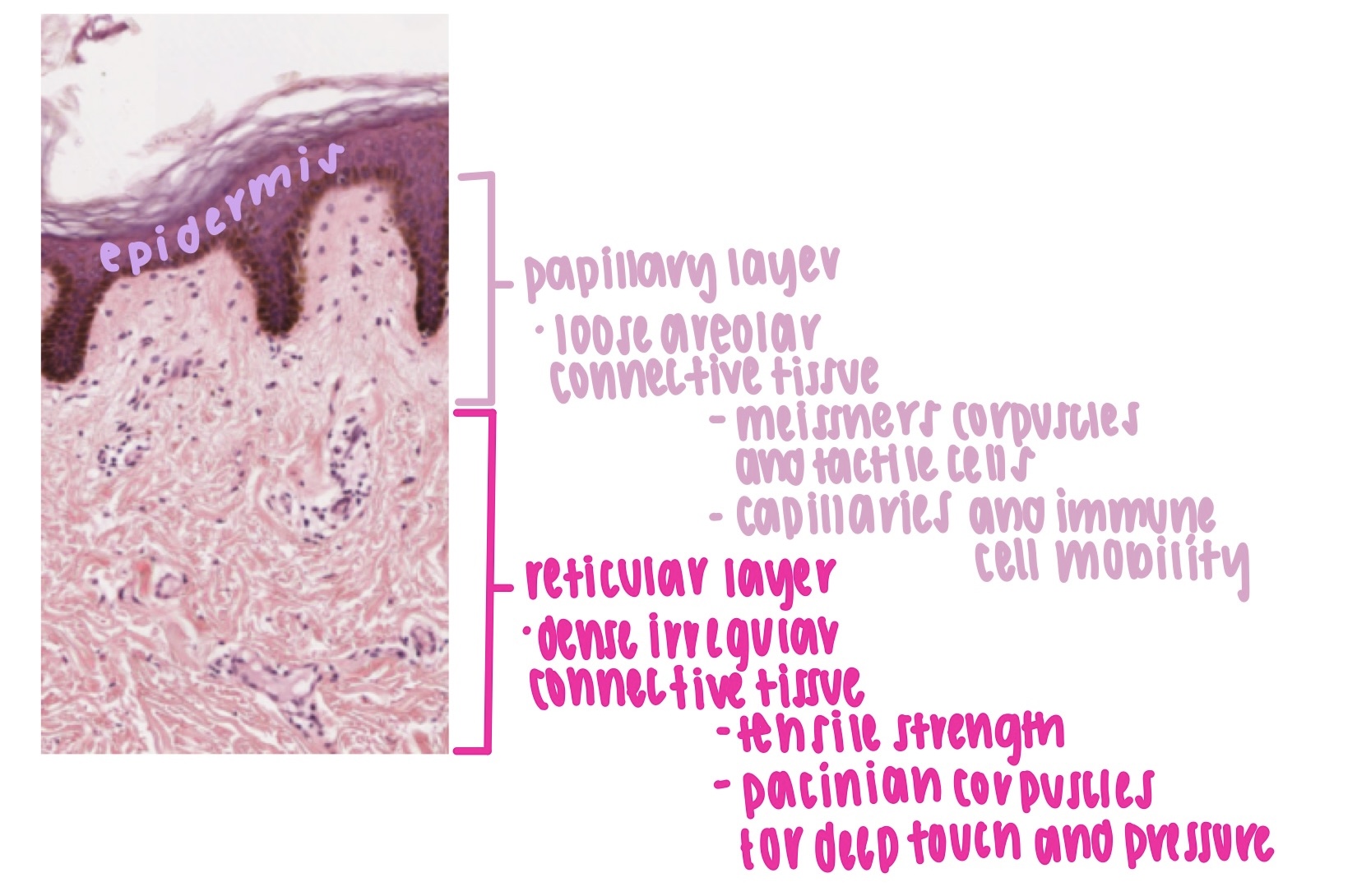
layers of the dermis
papillary layer
superficial zone of the dermis
thinner zone of loose areolar connective tissue with papillae
allows for mobility of immune cells in case of invasion
provides papillary capillary network to nourish epidermis
houses papillary touch receptors called tactile (meissners) corpuscles that reside in papillae and sense light touch (using tactile merkel cells)
reticular layer
deeper and much thicker layer of dermis
consists of dense irregular connective tissue characterized by thick and wavy collagen bundles in multiple directions
provides tensile strength in any direction which is good for unpredictable stress
stretch marks are caused by tearing in the reticular dermis
contains pacinian (lamellar) corpuscles which are deep touch and pressure receptors
dermal features
the integument has three major types of glands including (1) merocrine or eccrine sudoriferous (sweat) glands, (2) apocrine sudoriferous glands, and (3) sebaceous glands
all glands are made mostly of epithelial tissues
merocrine (eccrine) sudoriferous (sweat) glands
common and simple glands that are coiled and tubular
found throughout the body
utilize merocrine secretion (vesicular exocrine secretion mechanism)
functions to produce watery perspiration that helps cool the body
produce sweat that is slightly acidic with some ions but most ions are reabsorbed in the gland before sweat is released into the duct
apocrine sweat glands
occur only in the inguinal, anal, axillary, pectoral, and bearded area in males
utilize merocrine secretion
ducts empty into nearby hair follicles rather than the skin surface
function as scent glands that respond to stress and sexual stimulation
produce thick and milky sweat with fatty acids
develop at puberty and release pheromones (humans produce pheromones but lack the organ to detect them)
sebaceous (oil) glands
flask shaped glands with short ducts that open into a hair follicle
found throughout the body
composed of stratified cuboidal epithelium
utilize holocrine secretion
the cell is replaced by mitosis at the base of the gland
produces oily sebum
function to keep skin and hair from becoming dry and brittle
ceruminous glands
simple and coiled tubular glands that exist only in the external ear canal
true apocrine gland
combines sebum and exfoliated cells to form cerumen (earwax)
function to keep the eardrum pliant, waterproof the ear canal, kill bacteria, and hinder foreign particle entry
mammary glands
milk producing glands that develop only during pregnancy and lactation
found in the breasts
true apocrine gland
rich secretions released by ducts that open into the nipple
mammary ridges or milk lines are two rows of mammary glands found in most mammals
the hypodermis
mostly adipose tissue and blood vessels
thin wisps of collagen are present as they loosely tether adipocyte clusters together
function to pad the body (absorb shock and protect large resident blood vessels) and serve as an energy reservoir while also providing for thermoregulation and insulation
drugs are introduced into the hypodermis by injection as the layer is thick and highly vascular for effective systemic absorption
life cycle of a keratinocyte
keratinocytes are produced deep in the epidermis by the mitosis of stem cells in the stratum basale
some of the deepest keratinocytes in the stratum spinosum also continue dividing
mitosis ceases once epidermal cells migrate two to three cells away from the dermis as mitosis requires an abundant supply of oxygen and nutrients which are acquired from blood vessels in the nearby dermis
as new keratinocytes form the older ones are pushed toward the apical surface of the epidermis
in 30 to 40 days keratinocytes make way to the surface and exfoliate or flake off
keratinocyte migration is slower in old age and faster in skin that has been injured or stressed (accelerates keratinocyte multiplication and can result in calluses or corns which are accumulations of dead keratinocytes)
as keratinocytes are pushed upwards by dividing cells below they flatten and produce more keratin filaments and lipid filled lamellar granules
in the stratum granulosum these granules (1) release a protein called filaggrin which binds the cytoskeletal keratin filaments together into coarse and tough bundles, then (2) cells produce a tough layer of envelope protein beneath the plasma membrane which creates a nearly indestructible protein sac around keratin bundles and (3) lamellar granules release a lipid mixture that spreads out over the cell surface to waterproof it which creates a (4) barrier that cuts keratinocytes off from the supply of nutrients below which causes cell death and leaves the tough waterproof sac with bundles of keratin that creates the epidermal water barrier
the stratum corneum contains compact layers of dead keratinocytes and keratinocyte fragments
dead cells exfoliate off as dander which can accumulate
dandruff is composed of clumps of dander stuck together by sebum
skin discoloration as diagnostic observations
cyanosis
blue or grey hue of the skin and mucous membranes
caused by oxygen deficiency in circulating blood
most visible in the lips and oral mucosa as well as the tongue but also be seen in the palms and under the fingernails
can result from conditions that prevent blood from picking up a normal load of oxygen in the lungs such as airway obstructions, drowning, choking, lung diseases including emphysema and respiratory arrest, cold weather, and cardiac arrest
erythema
abnormal redness of the skin
common sign of infection and inflammation
results from increased blood flow in dilated cutaneous vessels or by dermal pooling of red blood cells that have escaped abnormally permeable capillaries
can be narrowly circumscribed (around a mosquito or tick bite) or spread more broadly
pallor
pale or ashen color
occurs when there is little blood flow through the skin or when the blood has low oxygen levels
reveals dermal collagen
noticeable in face and palms
can result from emotional stress, low blood pressure, circulatory shock, cold temperatures, or severe anemia
albinism
genetic lack of melanin
results in milky white hair and skin and blue grey eyes
caused by a recessive, nonfunctional tyrosinase allele that prevents the synthesis of melanin from the amino acid tyrosine
jaundice
yellowing of the skin and whites of eyes
cause by high levels of bilirubin (hemoglobin breakdown product) in the blood
the liver and spleen convert hemoglobin to bilirubin which the liver excretes in the bile
when the liver is not developed enough (such as with cancer, hepatitis, cirrhosis, and prematurity) bilirubin cannot be disposed of efficiently and it accumulates
hematoma
otherwise known as a bruise
mass of clotted blood showing through the skin
typically caused by accidental trauma or blows to the skin
can be indicative of hemophilia, metabolic or nutritional disorders, and physical abuse
tissue growth and developmental mechanisms
hyperplasia
tissue growth through cell multiplication (division)
primary form of tissue growth during gestation, infancy, and childhood (also important in adolescence)
hypertrophy
enlargement of preexisting cells
characterizes muscle growth through exercise and the accumulation of body fat
neoplasia
development of a tumor (neoplasm)
can be benign and stop growing
can be malignant and continue growing (forms cancer)
both benign and malignant neoplasms are composed of abnormal and dysfunctional tissue
benign neoplasms include skin moles, cysts, scars and keloids, as well as static organ tumors
malignant neoplasms become carcinomas of various organs
metaplasia
changing from one type of mature tissue to another
an example is that of pseudostratified columnar epithelium in the bronchi of smokers which converts to stratified squamous epithelium (allows for greater protection from damage but reduces mucus production and movement)
classification of tissues
epithelial tissue
all epithelia are avascular and depend on diffusion from deeper tissues with a blood supply for nutrition and sanitation
consist of a layer or layers of densely packed and adherent cells with little room for extracellular matrix
high cells to matrix ratio (lots of cells and little matrix)
contains a basal lamina (basement membrane) which is the only visible matrix found in epithelial tissues
the basal lamina is a protein sheet (containing collagen, laminin, and fibronectin) attached to the basal surface of the epithelium and functions to anchor the epithelium to underlying (connective) tissues
cover internal and external surfaces and usually lie superficial to connective tissues
line the internal lumen of hollow organs as part of the mucous membranes or mucosa
line internal body cavities and resident organs as part of serous membranes or serosa
form most glands and ducts (single or multiple layers of tissue can develop as a circular tube with an epithelial layer lining the tube)
apical or outermost surfaces of epithelial tissues are exposed to the environment or an internal space
serve as selective exchange membranes and as barriers
adhere tightly to one another and to their basement membrane which prevents free and unwanted passage and protects underlying tissue
tend to be more resilient than deeper tissues
shapes
squamous
thin and flat (plate like)
wider than they are tall
cuboidal
square or rounded (cube like)
as tall as they are wide
columnar
tall and narrow (stalk like)
taller than they are wide
types
simple epithelia
single layer of cells
consist of four types including (1) simple squamous, (2) simple cuboidal, (3) simple columnar, and (4) pseudostratified columnar
stratified epithelia
multiple layers of cells
consists of four types (omit two) including (1) stratified squamous and (2) transitional or urothelium
connective tissue
tissues in which cells usually occupy less space than the extracellular matrix
low cells to matrix ratio (little cells and lots of matrix) compared to epithelium
most connective tissue cells are not directly adjacent as cells are separated by substantial matrix (including ground substance and fibers)
some are highly vascular while others are avascular
types
connective tissue proper (lamina propria)
include two dense or fibrous subtypes and three loose subtypes
supportive connective tissues
three cartilage and three bone types
fluidic connective tissues
blood
epithelial tissue
simple epithelia
simple squamous epithelium
characteristics
single layer of thin and flat cells
bulges where the nucleus is located
function
thin layer permits rapid diffusion or selective transport
can secrete lubricating substances
locations
mesothelia of pleura
serosa or serous membranes of stomach and intestines
endothelium (luminal lining of blood vessels and heart)
glomerular capsule (inner layer of filtration structure in the kidneys)
kidney tubules
alveoli (air sacs in the lungs)
pericardium
peritoneum
mesenteries
simple cuboidal epithelium
characteristics
single layer of square or rounded cells
spherical and centrally placed nuclei
function
absorption and secretion
production of protective mucous coat
movement of respiratory mucus
locations
renal (kidney) ducts and tubules
hepatic (liver) ductules for bile secretion
thyroid follicles
pancreatic ducts
mammary gland ducts
salivary gland ducts
bronchioles
simple columnar epithelium
characteristics
single layer of tall and narrow cells
can have goblet cells and microvilli brush border (goblet cells are bulbous clear cells involved in the bulk secretion of mucus that produce an aqueous mixture containing mucin proteins and ions as well as acids and bases)
function
bulk absorption and bulk secretion
secretions usually contain a very high mucus content
locations
luminal lining of the gastrointestinal tract
gastric mucosa
small intestine mucosa
colonic mucosa
rectal mucosa
gallbladder tubules
uterus and uterine tubes
pseudostratified ciliated columnar epithelium
characteristics
single layer of cells that appears multilayered
all cells touch the basement membrane
ciliated on apical surface with a few interspersed goblet cells
function
secrete and propel mucus
locations
respiratory mucosa
nasal to bronchial mucosa
portions of the male urethra
stratified epithelia
keratinized stratified squamous epithelium
characteristics
multiple cell layers with dead compact cells
keratin filled flat cells on the surface that are dead and lack a nucleus
can exfoliate and be replaced by deeper layers
function
resist abrasion and penetration
prevent infections as a barrier pathogens
minimize fluid loss
locations
found only in the epidermis
particularly in the palms and soles
nonkeratinized stratified squamous epithelium
characteristics
multiple cell layers that lack dead surface cells
cells do not exfoliate
function
mildly resist abrasion and penetration
prevent infections as a barrier to pathogens
must be constantly moistened
locations
oral mucosa
esophageal mucosa
anal mucosa
vaginal mucosa
tongue
transitional epithelium or urothelium
characteristics
round surface cells of different shapes and sizes
can be binucleated
can possess umbrella cells that cover more than one cell
thick when relaxed and thin when stretched
function
stretches to allow filling of urinary bladder
protect underlying tissues from osmotic damage by urine
locations
localized to urinary system
ureters
urinary bladder
proximal urethral mucosa
renal canal
types of body membranes
membranes line external and luminal surfaces as well as body cavities and their resident viscera
cutaneous (external) membrane or the skin
largest membrane in the body
utilized for protection
the superficial portion contains keratinized stratified squamous epithelium (epidermis) while the deep portion contains areolar connective tissue (papillary dermis)
mucous (luminal) membranes
mucous membranes (mucosa) line the surface of hollow organs that open into an internal lumen
the superficial portion contains an epithelial tissue layer (simple or pseudostratified columnar with goblet cells or nonkeratinized stratified squamous) that often has cilia or microvilli while the deep portion contains the lamina propria (usually areolar connective tissue) and muscularis mucosa (smooth muscle that moves the mucosa)
serous (cavity) membranes
serous membranes (serosa) line the surfaces of body cavities and resident organs
produce serous fluid obtained from blood plasma to lubricate organs and cavity walls
thin membrane consisting of a simple squamous epithelium (mesothelium) and a slight layer of areolar connective tissue
intercellular junctions
cells must cooperate to form a healthy barrier tissue
most cells of a barrier tissue share via intercellular junctions
intercellular junctions exist between neighboring cells and maintain the tissue layer so the tissues can live long and prosper
tight (occluding) junctions - create a seal
a region of plasma membrane from two adjacent cells fused by adhesion proteins
form a zone that completely seals off lateral intercellular spaces near the apical side of the membrane which makes it impossible for most substances to pass between cells
most but not all epithelia have tight junctions
desmosomes (anchoring junctions) - provide structural support
patches that hold cells together
resist mechanical stress and keep cells from pulling apart
hooklike and j shaped proteins arise from cytoskeleton traverse transmembrane grooves and latch on to one another
hemidesmosomes (half desmosomes) - anchor cells to basal lamina
latch the basal surface of epithelium to the basal lamina and functions to resist epithelial layer delamination from underlying tissues
gap (communicating) junctions - allow direct communication and substance exchange
pores that equilibrate internal conditions between cells of an epithelial tissue
allow for free diffusion of ions, glucose, amino acids, and other small solutes through the cytoplasm of adjacent cells
a ring like connexon arranged in segments (like that of an orange) forms a water filled pore with size exclusion properties
glands and modes of secretion
glands are mostly made of epithelial tissue and function to secrete substances for use elsewhere in the body or for release and elimination from the body
exocrine glands (excreting)
maintain contact with the internal and external body cavities via a duct or epithelial tube that conveys products to the surface
external exocrine glands include sudoriferous, mammary, ceruminous, sebaceous, and lacrimal glands
internal exocrine glands include goblet cells, mucus glands, digestive glands, and renal tubules
endocrine glands (secreting)
ductless glands that do not reach the surface of the body
examples include the thyroid, adrenal, thymus, and pituitary glands
merocrine (eccrine) secretion
most common form of secretion
vesicular exocytosis deposits endocrine or exocrine products into a duct, vessel, or other fluidic space
include tear, sweat, and pancreatic glands, goblet cells, melanocytes, and all endocrine glands
apocrine secretion
decapitation secretion
apical surface fragments release membrane bound chunks of exocrine product into a duct
include ceruminous and mammary glands
not apocrine sudoriferous glands (perform merocrine secretion)
holocrine secretion
suicide secretion
exocrine gland cells accumulate a product and the entire cell breaks away to disintegrate in the duct
the secretion is a mixture of cell fragments and synthesized substance
include sebaceous and tarsal or oil glands of the eyelids
connective tissue
—
connective tissue proper (lamina propria)
cellular makeup
fibroblasts are the most abundant cells that function to produce structural protein fibers such as collagen and elastin as well as the ground substance of the extracellular matrix
resident immune cells protect the tissue from infection
macrophages phagocytize pathogens and debris and trigger immune responses recruiting leukocytes from the blood
mast cells secrete heparin to inhibit clotting and histamine to dilate blood vessels and increase blood flow which leads to swelling and inflammation
extracellular makeup
fibers are made by fibroblasts
type one collagenous fibers are made of collagen and are the tough, thick, slightly flexible and stretch resistant fibers of tendons, ligaments, and the deep dermis of skin
elastic fibers are made of elastin and are thin, highly flexible, and branched to allow for stretch and elastic recoil
reticular fibers are made of thin, type three collagen strands that compose a thin branching collagen network with glycoproteins and forms a framework for immune cells to reside upon
ground substance is a gelatinous to rubbery consistency and contains glycosaminoglycans (GAGs; polysaccharides of amino sugars that draw in water to provide gelatinous consistency to ground substance), proteoglycans (PGs; large molecules incorporating GAGs that create strong structural bonds between cell membrane proteins, cell cytoskeletons, and extracellular matrix fibers to support tissue integrity), and adhesive glycoproteins (membrane bound proteins that bind cells to fibers and/or PGs to support tissue integrity)
subtypes of connective tissue proper
these subtypes include dense or loosely organized fibers made up of mostly collagen, abundant vasculature, and seemingly empty space (ground substance appears empty)
dense subtypes have a lot of type one collagen and less ground substance visible than loose subtypes
dense subtypes vary in orientation of fibers
dense regular connective tissue
all tendons and ligaments
tendons attach muscle to bone and transfer muscular tension to bones
ligaments bind bones together and resist stress
densely packed and parallel
often wavy with slender fibroblast nuclei
avascular
dense irregular connective tissue
lower (reticular) dermis
capsules around the liver, kidney, and spleen viscera
fibrous sheaths around cartilage and bones
microvasculature
densely packed but running in random directions
withstand stress applied in unpredictable directions and imparts durability to tissues
—-
loose subtypes have less collagen with other fibers mixed in and more ground substance or empty space between cells
loose subtypes vary in types of fibers
areolar connective tissue
upper (papillary) dermis
underlying epithelia, surrounding blood vessels, nerves, esophagus, trachea, fascia, mesenteries, visceral pericardium, and pleura
made of elastic fibers (thin strands) and type one collagen (thick strands)
contain fibroblasts and a lot of ground substance
loosely organized fibers with abundant blood vessels
nearly epithelial layer rests on a layer of areolar tissue (extensive vasculature in areolar tissue brings fresh blood to nourish and filter avascular epithelia by diffusion)
contains a ready supply of infection fighting leukocytes that move about freely in areolar tissue
reticular connective tissue
spleen, lymph nodes, thymus, and bone marrow
made of type three collagen reticular fibers
—
cartilaginous connective tissue
more rubbery and flexible than bone but more rigid than other connective tissues
avascular with uniform cellular makeup
cells begin as chondroblasts that produce a matrix of type two collagen and chondroitin
chondroblasts become chondrocytes as they mature and trap themselves in lacunae
all cartilage begins as hyaline cartilage (smooth and glassy and uniform appearance of a type two collagen matrix) but few locations are later modified into elastic cartilage or fibrocartilage
perichondrium is a sheath of collagen fibers, fibroblasts, and chondroblasts that surrounds most hyaline and elastic cartilage (but not fibrocartilage and articular hyaline cartilage)
perichondrium contains a reserve population of cells that contribute to cartilage growth and repair throughout life
hyaline cartilage
smooth and glassy appearance due to fineness of type two collagen fibers relative to type one fibers
flexibility eases joint movement and allows for some expansion or constriction while rigidity maintains a patent airway and gives shape to facial features
articular cartilages are hyaline cartilage (joint surfaces at the ends of long bone)
costal cartilage and the respiratory tract (tracheal rings, bronchial plates, laryngeal and nasal cartilages)
the most abundant form of cartilage
elastic cartilage
modified hyaline cartilage with additional elastin secreted into the cartilage matrix
more flexible cartilage that is able to stretch and recoil to original shape due to elastic fibers
limited to the external ear and the epiglottis of the larynx
special stain for elastic fibers turns them deep purple
fibrocartilage
modified hyaline with coarse bundles of type one collagen secreted into cartilage matrix
more fibrous appearance in which chondrocytes form linearized rows
resist compression and absorb shock but has limited flexibility
does not regenerate due to a lack of perichondrium
limited to the interpubic disc, knee menisci, articular disc of the jaw, and intervertebral discs
tissue injury and repair
tissue regeneration is the replacement of dead or damaged cells by the same type of cells as before
regeneration restores normal organ function
fibrosis is the replacement of damaged tissue with scar tissue
fibrosis does not restore normal function
basic understanding of stem cells
tissues can change types within certain limits
stem cells exist but are not equal
member cell differentiation occurs when unspecialized tissues of an embryonic, stem, or precursor cell become specialized and mature cell types
differentiation is the specialization of a cell into one of a specific type which reduces flexibility in what the cell can do
an example of this include embryonic mesenchymal cells which differentiate into muscle, bone, and cartilage
differentiation is most prominent in youth but occurs in adults as well
embryonic stem cells (ESCs) are totipotent in early stages because of unlimited developmental plasticity but the inner cells become pluripotent and cannot become accessory or pregnancy organs but can become anything else
adult stem cells (ASCs) are multipotent cells that can develop into multiple cell lines but some are unipotent and can produce one mature cell type
relationship between surface area and volume
when cells grow the volume increases more than the surface area
surface area is proportional to the square of cell diameter
volume is proportional to the cube of a cell diameter
interaction with the extracellular environment occurs on the cell surface and allows for processes such as oxygen absorption, glucose uptake, and carbon dioxide efflux
matters as organelle viability is at risk in a larger cell (if a cell grows too large the surface area becomes insufficient to support the cell machinery through inadequate environmental interaction)
matters also because structural integrity is at risk in a rapidly growing and larger cell (if the volume of a cell increases abruptly before the membrane can grow to compensate the cell may rupture)
functions of different organelles
nucleus
largest organelle that is visible with a microscope
enclosed in a double membrane called the nuclear envelope which is perforated with nuclear pores
the nuclear lamina is inside the nuclear envelope and is a densely fibrous but narrow zone composed of intermediate filaments
contains nucleoplasm which has chromatin (genetic material) and nucleoli (produce ribosomes)
endoplasmic reticulum
system of interconnected channels called cisterns enclosed by a membrane
the rough endoplasmic reticulum is covered in ribosomes and functions to synthesize and fold proteins that are secreted from the cell or packaged in organelles
the smooth endoplasmic reticulum lacks ribosomes and perform detoxification as well as steroid production and lipid manufacture
ribosomes
small granules of protein that read messenger RNA and assemble amino acids into proteins specified by the code
golgi complex
small system of cisterns that synthesize carbohydrates and finish protein and glycoprotein synthesis
lysosomes
package of enzymes that hydrolyze macromolecules and substrates
peroxisomes
contain different enzymes that use molecular oxygen to oxidize organic molecules and neutralize free radicals
proteasomes
hollow cylindrical complexes of proteins that destroy unwanted proteins
mitochondria
organelles specialized for the synthesis of ATP
centrioles
short cylindrical assembly of microtubules that contribute to cell division
functions of different membrane proteins
transmembrane proteins pass completely through the phospholipid bilayer and protrude from it on both sides
peripheral proteins do not protrude into the phospholipid bilayer but adhere to either the inner and outer face of the membrane
receptor
binds to chemical messengers and transport them into the cell
usually specific for one particular messenger
enzyme
breaks down a chemical messenger and terminates the effects
carries out final stages of starch and protein digestion
prevents excessive stimulation of a cell
carrier
transmembrane protein that binds to solutes and transfers them to the other side of the membrane
some carriers are pumps as ATP is consumed in the process
ion channel
constantly open and allows ions to pass into and out of the cell
passages that allow water and hydrophilic solutes to move through the membrane
leak channels are always open and allow materials to pass through continually
gated ion channel
opens and closes to allow ions through only at certain times
ligand gated channels respond to chemical messengers
voltage gated channels respond to changes in electrical potential or voltage across a plasma membrane
mechanically gated channels respond to physical stress on a cell
cell identity marker
a glycoprotein acting as a cell identity marker that distinguishes the cells of the body from foreign cells
enables the immune system to tell which cells belong to the body and which are foreign invaders
cell adhesion molecule (CAM)
binds one cell to another
cells adhere to one another and to extracellular material
surface extensions of the membrane
microvilli
extensions of the plasma membrane that primarily serve to increase surface area
best developed in cells specialized for absorption (eg. simple columnar epithelial cells of the intestines and kidneys)
can be dense and appear as fringe brush border on the apical cell surface
cilia
hairlike processes (eg. ciliated pseudostratified columnar epithelia) that primarily serve to propel substances especially mucus
nonmotile cilia adopt sensory roles
nonmotile cilia are found in the inner ear, retina of the eye, the kidney, and the plasma membrane
motile cilia are numerous but less widespread than nonmotile cilia
motile cilia are found in the respiratory tract, uterine (fallopian) tubes, internal cavities (ventricles) of the brain, and short ducts (efferent ductules) associated with the testes
active versus passive transport
active transport
mechanisms that consume adenosine triphosphate (ATP) for energy
include active transport and vesicular transport
active transport has a slower rate than passive
active transport is more saturable than passive transport
primary active transport is the process in which a carrier moves a substance up the concentration gradient using energy from ATP (eg. sodium potassium pump which outputs three sodium ions and intakes two potassium ions upon consumption of one ATP)
passive transport
mechanisms that do not require adenosine triphosphate (ATP) expenditure by the cell
include filtration and (simple and facilitated) diffusion as well as osmosis
simple versus facilitated transport
simple (direct) diffusion
net movement of particles from a place of high concentration to a place of lower concentration as a result of constant and spontaneous motion
nonpolar and hydrophobic (lipid soluble) substances and gases can diffuse directly through the lipid bilayer of the cell membrane
the cell cannot control permeability of simple diffusing substances as the limiting factor is the availability of nonpolar surface area
facilitated diffusion (carrier mediated) transport
diffusion through protein channels or pumps
carrier mediated transport of a solute down the concentration gradient
use membrane proteins to transport substances from one side of the membrane to the other
includes passive facilitated diffusion as well as active transport
cells control permeability by regulating channel protein abundance (expression) or by opening and closing channels (gating)
solutes that use this form of transport include water and charged, hydrophilic solutes
carriers exhibit specificity as transport proteins are specific for a class of certain ligands and the solute binds to a specific receptor site on the carrier protein
carriers exhibit saturation and as the solute concentration rises the rate of transport increases but only to an extent or the transport maximum (more solute does not increase rate)
transport maximum and saturation
the transport maximum (saturation point) is the point in which carriers are saturated and excess solute does not increase the rate of transport
otherwise referred to as the maximum biological diffusion rate
all carriers and channels or pumps for solute transport are occupied simultaneously and further increases in the concentration gradient to do not increase the rate of transport
simple diffusion is the least saturable (greatest transport maximum)
ungated and passive facilitated diffusion is the second saturable
gated and passive facilitated diffusion is the third saturable
active transport is the most saturable (lowest transport maximum)
factors affecting the rate of diffusion and transport
temperature
an increase in temperature results in an increase in kinetic energy and an increase in diffusion and transport rate
molecular weight
an increase in size results in a decrease in kinetic energy and a decrease in diffusion and transport rate
larger molecules move slowly through a medium
steepness of concentration gradients
the greater the difference between the two concentrations the greater the rate of diffusion and transport
membrane permeability
an increase in permeability results in an increase in diffusion and transport rate
cells can adjust permeability by adding or removing channel proteins and by opening or closing membrane gates
membrane surface area
an increase in surface area makes more membrane available for the diffusion of particles
in simple diffusion an increase in the lipid bilayer surface area increases the diffusion and transport rate
in facilitated diffusion an increase in expressed and open channel proteins increases the diffusion and transport rate
types of transporters
uniport transporters carry only one type of solute
symport transporters perform cotransport and move two or more solutes through a membrane simultaneously and in the same direction
antiport transporters perform countertransport and move two or more solutes through a membrane in the opposite direction
secondary active transport
requires an energy input to move a solute up the concentration gradient
depends indirectly on adenosine triphosphate (ATP)
uses energy stored in an electrochemical gradient to move a different molecule against the gradient
fueled by primary transport
osmosis and tonicity
osmosis
net flow of water from one side of a selectively permeable membrane to another
crucial to water distribution or fluid balance in the body
the usual direction of net movement is from the watery side with a lower solute concentration to the less watery side with a higher solute concentration
aquaporins are channel proteins specialized for water and can increase the rate of osmosis
reverse osmosis is a process in which a mechanical pressure applied to one side of the system can override osmotic pressure and drive water through a membrane against the concentration gradient
tonicity
the ability of.a solution to affect the fluid volume and pressure a cell
a hypotonic solution has a lower concentration of nonpermeating solutes than the intracellular fluid which causes cells to swell and burst (lyse)
a hypertonic solution has a higher concentration of nonpermeating solutes than the intracellular fluid which causes cells to lose water and shrivel (crenate)
an isotonic solution has an equal solute concentration to that of the intracellular fluid which prevents changes. incell volume or shape
bulk transport
vesicular transport
move large particles and droplets of fluid or numerous molecules at once through the membrane in bubble like vesicles
endocytosis
vesicles bring matter into a cell
exocytosis
vesicles release matter from the cell
phagocytosis
referred to as cell eating
process of engulfing particles such as bacteria and dust and cellular debris
vesicles are called phagosomes
pinocytosis
referred to as cell drinking
process of taking in droplets of extracellular fluid containing molecules of some use to the cell
vesicles are called pinocytotic vesicles
receptor mediated endocytosis
more selective form of phagocytosis or pinocytosis
enables a cell to take in specific molecules from the extracellular fluid with a minimum of unnecessary matter
particles in the extracellular fluid bind to specific receptors on the plasma membrane
the receptors cluster and the membrane sinks in to create a pit coated with a peripheral membrane protein called clathrin
the pit pinches off to form a clathrin coated vesicle in the cytoplasm
clathrin serves as an address label on the coated vesicle that directs it to an appropriate destination in the cell and informs other structures in the cell what to do with the vesicle
receptor mediated exocytosis
process of discharging material from a cell
a secretory vesicle in the cell migrates to the surface and docks on the peripheral proteins of the plasma membrane
these proteins pull the membrane inward and create a dimple that eventually fuses with the vesicle and allows it to release the contents
transcytosis
material is capture on one side of the cell and released on the other
diffusion by filtration through a tissue membrane
passive movement of smaller and dissolved particles across the tissue layers by physiological forces or physical pressure in a selectively permeable fashion
examples include the filtration of nutrients through gaps in the blood capillary walls and the filtration of wastes from the blood in the kidneys while holding back blood cells and large proteins
typically occurs in a simple squamous tissue
hierarchy of life
atoms (smallest unit of life; small particles with unique chemical identities)
molecules
macromolecules
organelles (microscopic structures of a cell that carry out individual functions)
cells (smallest units that carry out all basic functions of life)
tissues (masses of similar cells and cell products that form a discrete region of an organ and performs a specific function)
organs (structures composed of two or more tissue types that work together to carry out a particular function)
organ systems (group of organs with unique collective functions)
organisms (most complex; single and complete individual)
homeostasis
homeostasis refers to the ability to maintain internal stability
involves the physiological ability to detect change and activate mechanisms that oppose it to maintain relatively stable internal conditions
the state of the body fluctuates (dynamic equilibrium) within a limited range around a set point
negative feedback
negates and reverse change to keep variable close to set point
maintains or restores steady state
activate mechanisms to reverse or mitigate change
receptor cells respond to a stimulus and the integrating or control center makes decision on how to respond to the stimulus
the effector organ is activated and restores conditions to the set point
example - brain regulation of body temperature
if too warm the blood vessels dilate (vasodilation) in the skin and sweating begins (heat losing mechanism)
if too cold the blood vessels constrict (vasoconstriction) and shivering begins (heat gaining mechanism)
positive feedback
repeated feedback loop in which change produces more of the change until the stimulus goes away
disrupt steady state or alter the set point
produces rapid changes in appropriately healthy situations (eg. childbirth; blood clotting; fever)
opposes the inertial qualities of homeostasis
example - childbirth
fetal propulsion to the cervix stimulates nerve endings
stimulated nerves trigger release of oxytocin
oxytocin stimulates stronger uterine contraction to propel fetus towards the birth canal
increases stimulation of cervical nerve endings
increases surge of oxytocin causing the positive feedback loop to be repeated until child is born
example - blood clotting
platelets adhere to injured area
activated platelets release chemicals that activate and attract more platelets
initiates cascade of enzymatic reactions to form a clot
clot forms and seals the wound
releases more chemicals that further activate platelets and enhance the clotting process
gradients and flow
a gradient is a difference in chemical concentration, electrical charge, physical pressure, temperature, or another variable between one point and another
if matter moves from a high to low point it flows down the gradient
if matter moves from a low to high point it flows up the gradient
chemicals flow down concentration gradients
charged particles flow down electrical gradients
ions governed by a combination of concentration and electrical charge flow down electrochemical gradients
heat flows down a thermal gradient