Chapter 22 Notes
0.0(0)
Card Sorting
1/12
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
1
New cards
General characteristics of the heart:
* Arteries
* Carry blood high in oxygen (excluding pulmonary arteries)
* Veins
* Carry blood low in oxygen (except for pulmonary veins)
* **Great vessels→** arteries and veins entering and leaving the heart; relatively large size
* Heart anatomy ensures that unidirectional flow of blood occurs; backflow is prevented by valves within the heart
* The heart acts like two side-by-side pumps that work at the same rate and pump the same volume of blood; one side directs blood to the lungs for respiratory gas exchange; the other directs blood to body tissues for nutrient and respiratory gas delivery
* The heart develops blood pressure by alternating cycles of the wall contraction and relaxation.
* **Blood pressure→** the force of blood pushing against the inside walls of the vessels
* Carry blood high in oxygen (excluding pulmonary arteries)
* Veins
* Carry blood low in oxygen (except for pulmonary veins)
* **Great vessels→** arteries and veins entering and leaving the heart; relatively large size
* Heart anatomy ensures that unidirectional flow of blood occurs; backflow is prevented by valves within the heart
* The heart acts like two side-by-side pumps that work at the same rate and pump the same volume of blood; one side directs blood to the lungs for respiratory gas exchange; the other directs blood to body tissues for nutrient and respiratory gas delivery
* The heart develops blood pressure by alternating cycles of the wall contraction and relaxation.
* **Blood pressure→** the force of blood pushing against the inside walls of the vessels
2
New cards
The Cardiovascular System:
* Right side of heart:
* Receives blood from body
* Pumps out to lungs
* **Pulmonary circulation:**
* Conveys deoxygenated blood from the right side of the heart through blood vessels to the lungs; oxygen is picked up; carbon dioxide realesed; the blood returns to the left side of the heart
* Pulmonary veins
* Pulmonary arteries
* Right atrium
* Right ventricle
* Left side of heart
* Receives blood from lungs
* Pumps out of body
* **Systemic circulation:**
* Moves oxygenated blood from the left side of the heart through blood vessels to the systematic cells such as those in the liver, skin, muscle, etc.
* Left atrium
* Left ventricle
* Aorta to systemic arteries
* Systemic veins
* Receives blood from body
* Pumps out to lungs
* **Pulmonary circulation:**
* Conveys deoxygenated blood from the right side of the heart through blood vessels to the lungs; oxygen is picked up; carbon dioxide realesed; the blood returns to the left side of the heart
* Pulmonary veins
* Pulmonary arteries
* Right atrium
* Right ventricle
* Left side of heart
* Receives blood from lungs
* Pumps out of body
* **Systemic circulation:**
* Moves oxygenated blood from the left side of the heart through blood vessels to the systematic cells such as those in the liver, skin, muscle, etc.
* Left atrium
* Left ventricle
* Aorta to systemic arteries
* Systemic veins
3
New cards
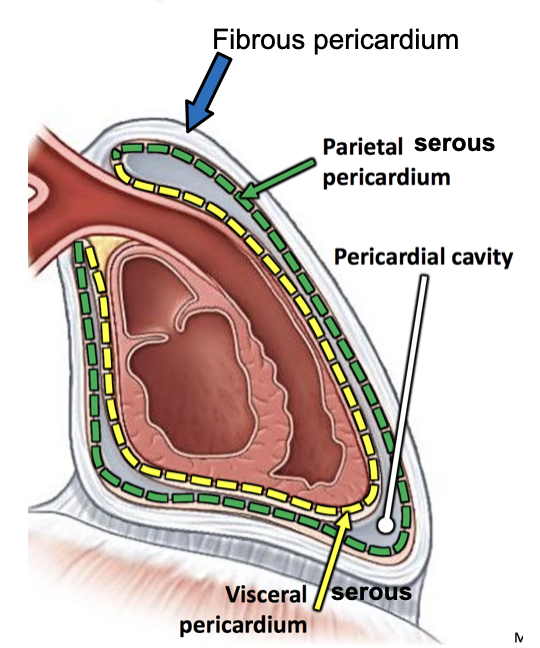
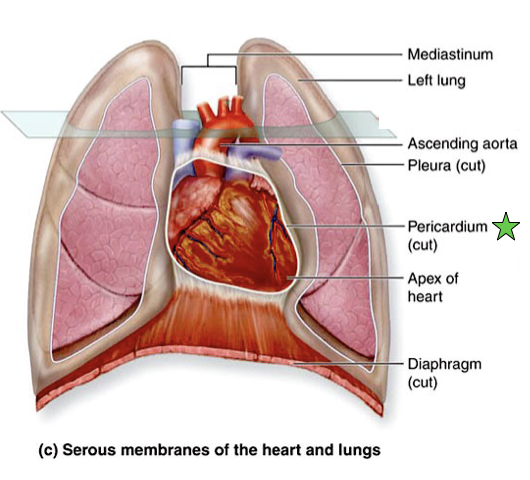
The Heart
* Sits in middle of chest, between lungs
* Surrounded by **pericardial sac** (**pericardium**)
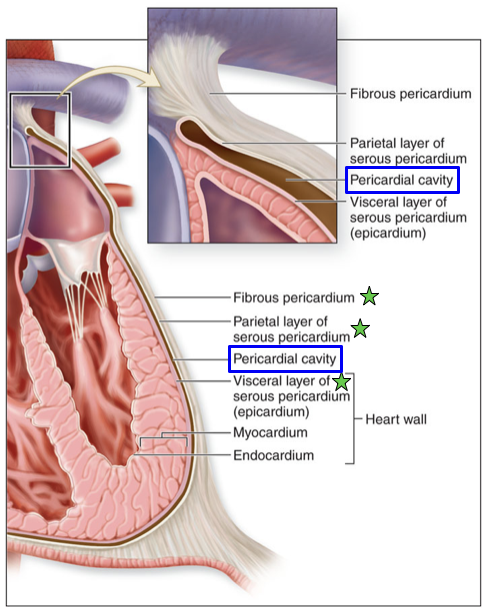
* **Fibrous pericardium**
* Outer portion of the pericardium that is made of tough, dense connective tissue
* Attached inferiorly to the diaphragm and superiorly to the base of the great vessels
* Creates a space around the heart
* Prohibits heart from moving within the thoracic cavity, and prevents the heart from overfilling with blood
* Fluid filled, protective, anti-friction
* Has multiple layers
* **Serous Membrane**
* Parietal serous pericardium
* Shiny inner surface
* Visceral serous pericardium (epicardium)
* Light reflects on membrane
* **Pericardial cavity**
* Narrow space between the parietal and visceral layers of the serous membrane
* Potential space for thin lining of serous fluid
* Too much fluid is called inflammation
* Surrounded by **pericardial sac** (**pericardium**)
* **Fibrous pericardium**
* Outer portion of the pericardium that is made of tough, dense connective tissue
* Attached inferiorly to the diaphragm and superiorly to the base of the great vessels
* Creates a space around the heart
* Prohibits heart from moving within the thoracic cavity, and prevents the heart from overfilling with blood
* Fluid filled, protective, anti-friction
* Has multiple layers
* **Serous Membrane**
* Parietal serous pericardium
* Shiny inner surface
* Visceral serous pericardium (epicardium)
* Light reflects on membrane
* **Pericardial cavity**
* Narrow space between the parietal and visceral layers of the serous membrane
* Potential space for thin lining of serous fluid
* Too much fluid is called inflammation
4
New cards
The Heart→ Superficial Anatomy
* **Base**→ the posterosuperior surface of the heart, formed primarily by the left atrium
* Superior border→ formed by the great arterial trunks (ascending aorta and pulmonary trunk), and the superior vena cava
* Inferior border→ formed by the right ventricle
* Apex
* Chambers
* Superior border→ formed by the great arterial trunks (ascending aorta and pulmonary trunk), and the superior vena cava
* Inferior border→ formed by the right ventricle
* Apex
* Chambers
5
New cards
The Heart→ Internal Anatomy
* **Epicardium**
* The outermost heart layer; aka the visceral layer
* Composed of serous membrane and areolar connective tissue
* **Myocardium**
* Middle layer of the heart wall; thickest of the layers
* Composed of cardiac muscle tissue
* Contracts cardiac muscles to pump blood
* **Endocardium**
* The internal surface of the heart chamber and external surface of the heart valves
* Composed of simple squamous epithelium and an underlying layer of areolar tissue
* **Chambers**
* **Ventricles**
* Difference in appearance in 2 ventricles
* Reflects the different loads places on them in their jobs
* **Left ventricle** is thicker than the **right ventricle**; pushes blood through arteries to systematic system; right valve only pushes to lungs
* Separated by interventricular septum
* Trabeculae carneae
* **Atria (atriums)**
* Left atrium
* Receives blood from the pulmonary circulation
* Right atrium
* Receives deoxygenated blood from the systemic circulation
* Interatrial septum
* Fossa Ovalis (of septum)
* Pectinate muscles
* **Valves**
* Pulmonary Semilunar Valve
* Right Atrioventricular Valve
* Left Atrioventricular valve
* Aortic Semilunar valve
* Chordae Tendineae
* Papillary Muscles
* Prevent atrioventricular valves from everting and flipping into the atria when ventricles contract
* The outermost heart layer; aka the visceral layer
* Composed of serous membrane and areolar connective tissue
* **Myocardium**
* Middle layer of the heart wall; thickest of the layers
* Composed of cardiac muscle tissue
* Contracts cardiac muscles to pump blood
* **Endocardium**
* The internal surface of the heart chamber and external surface of the heart valves
* Composed of simple squamous epithelium and an underlying layer of areolar tissue
* **Chambers**
* **Ventricles**
* Difference in appearance in 2 ventricles
* Reflects the different loads places on them in their jobs
* **Left ventricle** is thicker than the **right ventricle**; pushes blood through arteries to systematic system; right valve only pushes to lungs
* Separated by interventricular septum
* Trabeculae carneae
* **Atria (atriums)**
* Left atrium
* Receives blood from the pulmonary circulation
* Right atrium
* Receives deoxygenated blood from the systemic circulation
* Interatrial septum
* Fossa Ovalis (of septum)
* Pectinate muscles
* **Valves**
* Pulmonary Semilunar Valve
* Right Atrioventricular Valve
* Left Atrioventricular valve
* Aortic Semilunar valve
* Chordae Tendineae
* Papillary Muscles
* Prevent atrioventricular valves from everting and flipping into the atria when ventricles contract
6
New cards
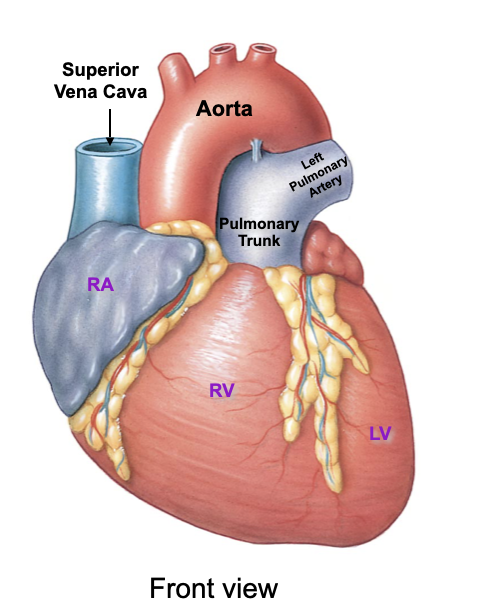
The Heart→ Attached Vessels
* Superior Vena Cava
* Drains blood from the head, neck, upper limbs, and superior regions of the trunk
* Pulmonary Trunk
* Transports blood from the right ventricle into the pulmonary circulation
* Aorta
* Conducts blood from the left ventricle into the systemic circulation
* Left pulmonary veins
* Left pulmonary artery
* Right pulmonary veins
* Inferior vena cava
* Drains blood from the lower limbs and trunk
* Coronary Sinus
* Drains blood from the heart wall
* Drains blood from the head, neck, upper limbs, and superior regions of the trunk
* Pulmonary Trunk
* Transports blood from the right ventricle into the pulmonary circulation
* Aorta
* Conducts blood from the left ventricle into the systemic circulation
* Left pulmonary veins
* Left pulmonary artery
* Right pulmonary veins
* Inferior vena cava
* Drains blood from the lower limbs and trunk
* Coronary Sinus
* Drains blood from the heart wall
7
New cards
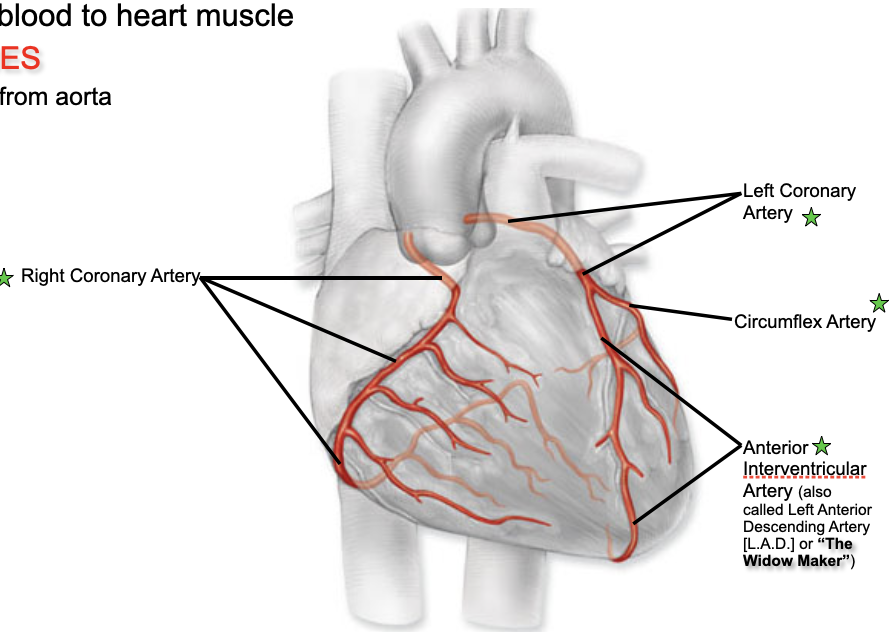
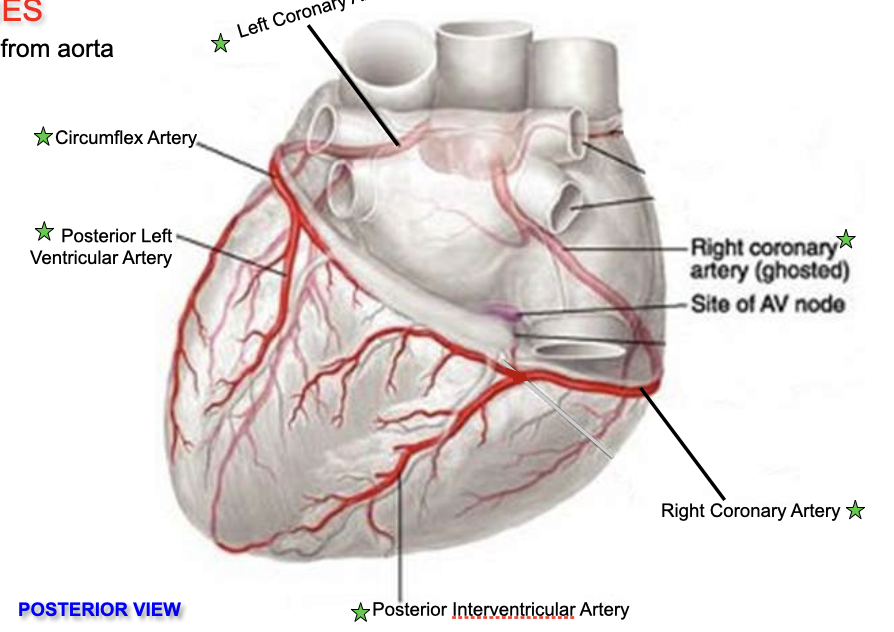
Coronary Circulation→ Arteries
* Left and right coronary arteries travel with the coronary sulcus of the heart to supply blood to the cells of the heart walls.
* Coronary arteries are considered **functional end arteries**; act like end arteries; easily blocked and can lead to dying arteries from lack of blood
* These arteries are the only branches of the ascending aorta.
* Coronary Vessels
* Provide blood to heart muscles
* **Arteries →** transports blood away from the heart; arise at aorta
* **Left Coronary Artery**
* Branches into the *anterior interventricular artery*; supplies the anterior surface of both ventricles and most of the interventricular septum
* Branches into *circumflex artery*; supplies left atrium and ventricle
* **Right Coronary Artery**
* Branches in *right marginal artery*; supplies blood to the right border of the heart
* Branches into *posterior interventricular artery*; supplies the posterior surface of both the left and right side of the heart
* *Anterior Interventricular Artery*
* *Circumflex Artery*
* *Posterior Left Ventricular Artery*
* *Posterior Interventricular Artery*
* Coronary arteries are considered **functional end arteries**; act like end arteries; easily blocked and can lead to dying arteries from lack of blood
* These arteries are the only branches of the ascending aorta.
* Coronary Vessels
* Provide blood to heart muscles
* **Arteries →** transports blood away from the heart; arise at aorta
* **Left Coronary Artery**
* Branches into the *anterior interventricular artery*; supplies the anterior surface of both ventricles and most of the interventricular septum
* Branches into *circumflex artery*; supplies left atrium and ventricle
* **Right Coronary Artery**
* Branches in *right marginal artery*; supplies blood to the right border of the heart
* Branches into *posterior interventricular artery*; supplies the posterior surface of both the left and right side of the heart
* *Anterior Interventricular Artery*
* *Circumflex Artery*
* *Posterior Left Ventricular Artery*
* *Posterior Interventricular Artery*
8
New cards
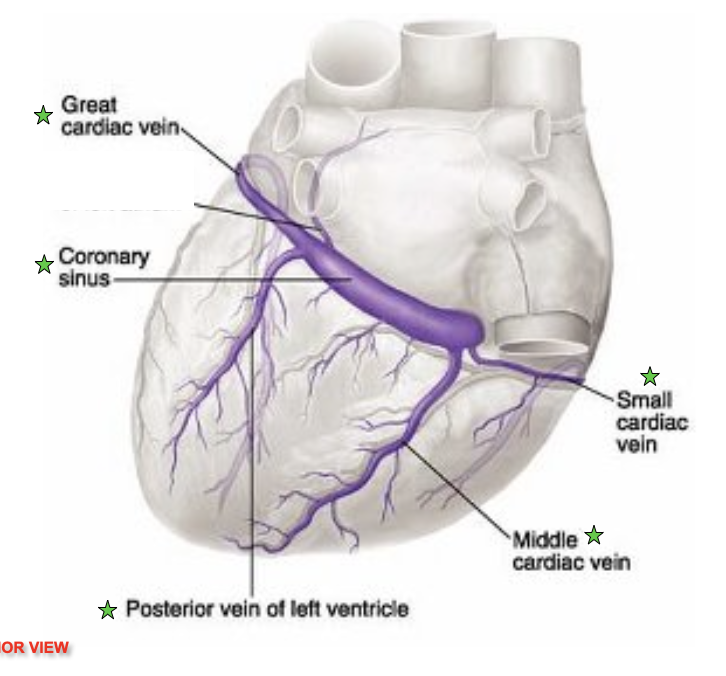
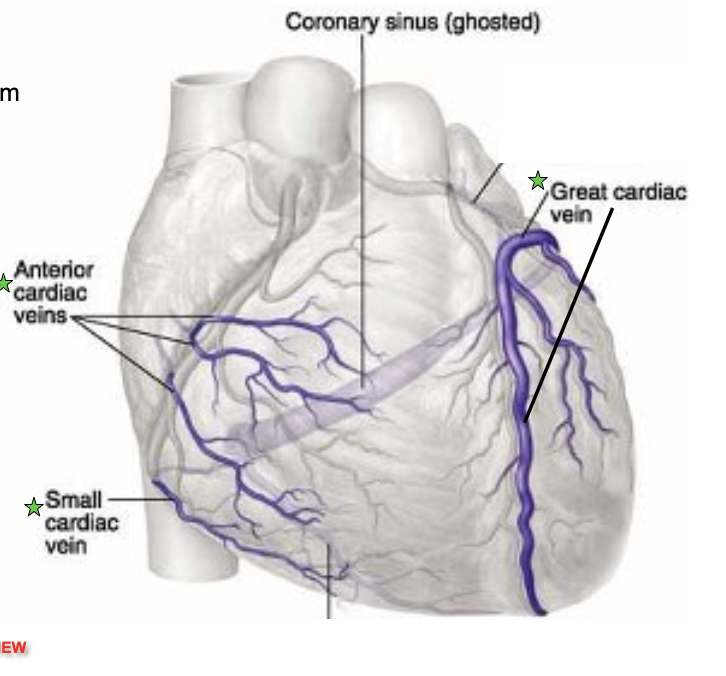
Coronary Circulation→ Veins
* **Veins→** transports blood to the heart
* Dump into coronary sinus
* Sinus dumps into right atrium
* *Great Cardiac vein*
* *Coronary sinus*
* Drains directly into the right atrium
* *Posterior vein of left ventricle*
* *Anterior cardiac veins*
* *Middle cardiac vein*
* Drains into coronary sinus
* *Small cardiac vein*
* Drains into coronary sinus
* *Great cardiac vein*
* Drains into coronary sinus
* Ventricular myocardium is compressed during contraction; most coronary flow occurs during ventricular relaxation
* Normal flow is evenly distributed; however under certain circumstance coronary flow may be reduced
* **Tachycardia→** an increased heart rate that shortens diastole
* **Hypotension→** reduces the ability of blood flow through the ventricular myocardium
* Dump into coronary sinus
* Sinus dumps into right atrium
* *Great Cardiac vein*
* *Coronary sinus*
* Drains directly into the right atrium
* *Posterior vein of left ventricle*
* *Anterior cardiac veins*
* *Middle cardiac vein*
* Drains into coronary sinus
* *Small cardiac vein*
* Drains into coronary sinus
* *Great cardiac vein*
* Drains into coronary sinus
* Ventricular myocardium is compressed during contraction; most coronary flow occurs during ventricular relaxation
* Normal flow is evenly distributed; however under certain circumstance coronary flow may be reduced
* **Tachycardia→** an increased heart rate that shortens diastole
* **Hypotension→** reduces the ability of blood flow through the ventricular myocardium
9
New cards
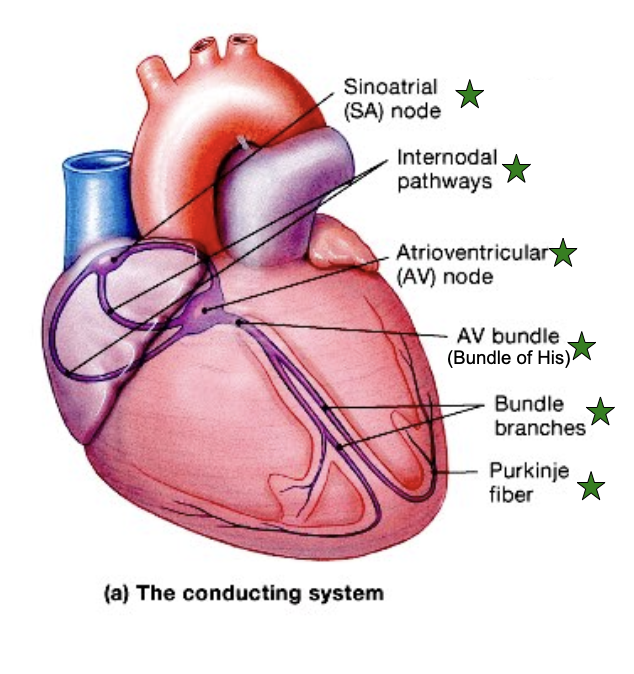
Contraction of Heart Muscles
* Angiogram
* Myocardial infarction (M.I) → Heart attack
* blocked lumen in branch of left coronary artery
* Anterior **infarct**
* Area of dying tissues due to loss of blood/oxygen supply
* Coronary Artery Bypass Graft (C.A.B.G)
* Contraction of the Heart Muscles
* Cardiac muscles cells contract as a single unit; an impulse distributes immediately and simultaneously thought the cell from the stria to the ventricles
* **Intercalated discs** have numerous desmosomes and gap junction
* **Desmosomes** prevent cardiac muscle cells from pulling apart
* **Gap junctions** provide low-resistance pathway for ions to move between adjoining cardiac muscle cells
* Allows muscle impulse to travel easily and instantaneously among cardiac muscle groups
* Intrinsic Conduction System
* Sinoatrial (SA) node
* Initiates the heartbeat; located in the posterior wall of the right atrium
* Cells act as a the **pacemaker**
* Initiates the heart impulse 70-80 times per minute
* Internodal pathways
* Atrioventricular (AV) node
* Located in the floor of the right atrium between the right AV valve and the opening of the coronary sinus
* Normally slows conduction of the impulse as it travels from the atria to the the ventricles; providing a delay between activation of the atria and ventricles
* AV bundle
* Receives muscle impulse from the AV node and extends into the interventricular septum before dividing into left and right bundles
* Left/Right Bundles
* Conduct impulse to conduction fibers called Purkinje Fibers that begin within the apex of the heart and extend through the walls of the ventricles
* Purkinje fiber
* Larger than other cardiac cells
* Rapid conduction impulses, consistent with the large size of the cells; impulse spreads immediately throughout the ventricular myocardium
* Myocardial infarction (M.I) → Heart attack
* blocked lumen in branch of left coronary artery
* Anterior **infarct**
* Area of dying tissues due to loss of blood/oxygen supply
* Coronary Artery Bypass Graft (C.A.B.G)
* Contraction of the Heart Muscles
* Cardiac muscles cells contract as a single unit; an impulse distributes immediately and simultaneously thought the cell from the stria to the ventricles
* **Intercalated discs** have numerous desmosomes and gap junction
* **Desmosomes** prevent cardiac muscle cells from pulling apart
* **Gap junctions** provide low-resistance pathway for ions to move between adjoining cardiac muscle cells
* Allows muscle impulse to travel easily and instantaneously among cardiac muscle groups
* Intrinsic Conduction System
* Sinoatrial (SA) node
* Initiates the heartbeat; located in the posterior wall of the right atrium
* Cells act as a the **pacemaker**
* Initiates the heart impulse 70-80 times per minute
* Internodal pathways
* Atrioventricular (AV) node
* Located in the floor of the right atrium between the right AV valve and the opening of the coronary sinus
* Normally slows conduction of the impulse as it travels from the atria to the the ventricles; providing a delay between activation of the atria and ventricles
* AV bundle
* Receives muscle impulse from the AV node and extends into the interventricular septum before dividing into left and right bundles
* Left/Right Bundles
* Conduct impulse to conduction fibers called Purkinje Fibers that begin within the apex of the heart and extend through the walls of the ventricles
* Purkinje fiber
* Larger than other cardiac cells
* Rapid conduction impulses, consistent with the large size of the cells; impulse spreads immediately throughout the ventricular myocardium
10
New cards
Fibrous
* The fibrous skeleton of the heart is formed from dense regular connective tissue
* Located between the atria and ventricles
* Provide **structural support** at the boundary between the atria and the ventricles
* **Forms supportive fibrous rings** to anchor the heart valves
* **Provides a rigid framework** for the attachment of cardiac muscle tissue
* **Acts as an electrical insulator**; prevents ventricles from from contracting at the same time as the atria
* Located between the atria and ventricles
* Provide **structural support** at the boundary between the atria and the ventricles
* **Forms supportive fibrous rings** to anchor the heart valves
* **Provides a rigid framework** for the attachment of cardiac muscle tissue
* **Acts as an electrical insulator**; prevents ventricles from from contracting at the same time as the atria
11
New cards
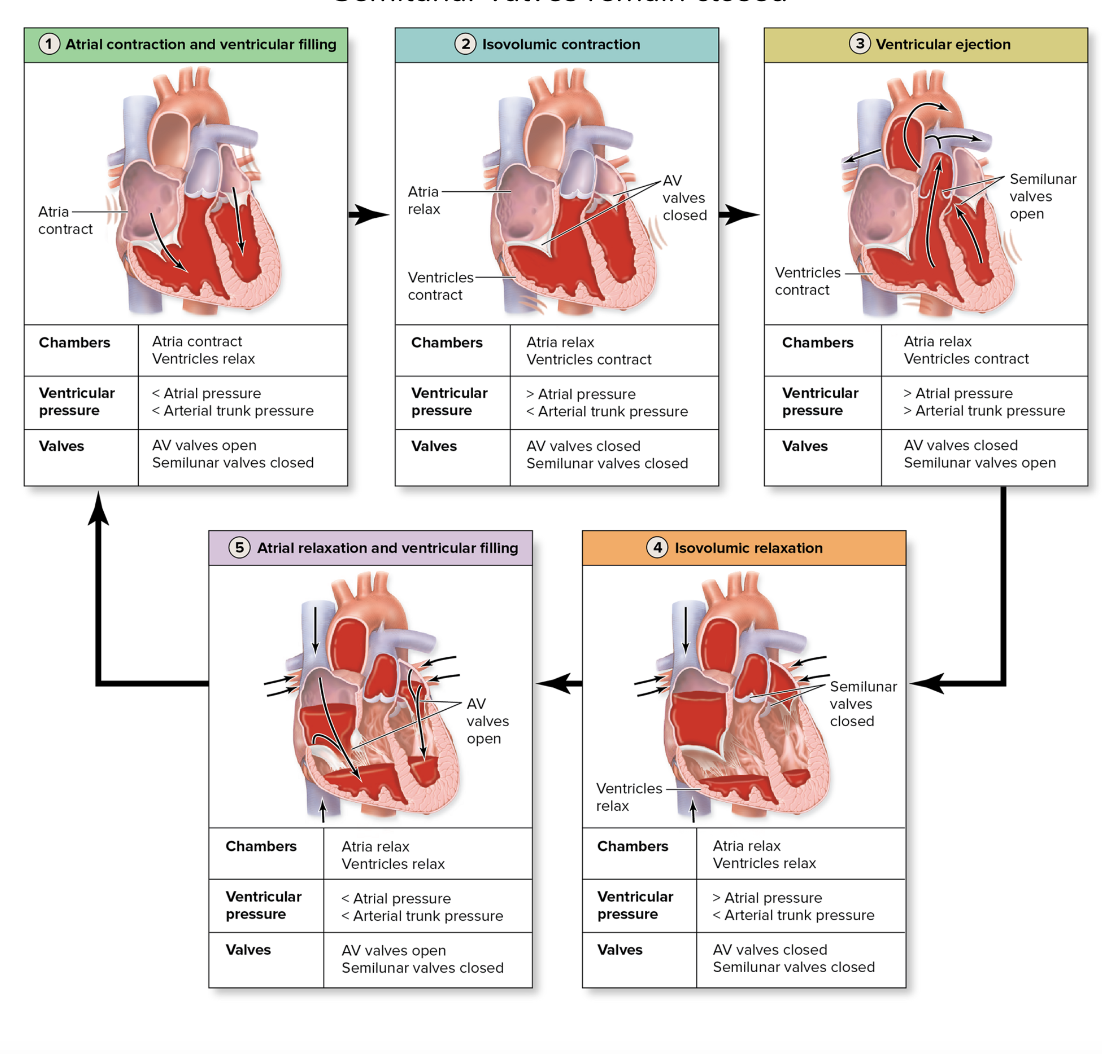
Blood Flow Through the Heart
* A cardiac cycle includes all the events within the heart from the start of one heartbeat to the initiation of the next
* **Systole→** the contraction of a heart chamber
* During this period, the contraction of the myocardium forces blood either into another chamber (from atrium to ventricle) or into a blood vessel (from ventricle into attached large artery)
* **Diastole→** the relaxation phase of a heart chamber
* During this period between contraction phases, the myocardium of each chamber relaxes; chamber fills with blood
* Steps in the Cardiac Cycle
* **Atrial contraction and ventricular filling**
* Occurs at the beginning of the cardiac cycle.
* Brief contraction of the atrial myocardium initiated by the SA node occurs
* Contraction of the atria finishes filling the ventricles through the open AV valve while the ventricles are in the diastole
* Semilunar valves remain closed
* **Isovolumic contraction**
* Occurs at the beginning of the ventricular contraction
* AV valves are forced cloths; produce “lubb” sound
* Semilunar valve remain closed
* Atria remain in diastole
* **Ventricular Ejection**
* Takes place later in the ventricular contraction; when pressure on blood in the ventricles forces the semilunar valves to open
* Blood is ejected into the arterial trunks
* Atria remain in diastole; Av valves remain closed
* **Isovolumic Relaxation**
* Occurs at the start of ventricular relaxation
* Semilunar valves close to prevent blood backflow into the ventricles; produces “dupp” sound
* The AV valve remain closed and the atria remain in diastole
* **Atrial relaxation and ventricular filling**
* Occur during the continuation of ventricular relaxation
* Atria remain in diastole
* The AV valve opens; passive filling of the ventricles from the atria begins and continues as most of the ventricular filling occurs
* Semilunar valves remain closed
* **Systole→** the contraction of a heart chamber
* During this period, the contraction of the myocardium forces blood either into another chamber (from atrium to ventricle) or into a blood vessel (from ventricle into attached large artery)
* **Diastole→** the relaxation phase of a heart chamber
* During this period between contraction phases, the myocardium of each chamber relaxes; chamber fills with blood
* Steps in the Cardiac Cycle
* **Atrial contraction and ventricular filling**
* Occurs at the beginning of the cardiac cycle.
* Brief contraction of the atrial myocardium initiated by the SA node occurs
* Contraction of the atria finishes filling the ventricles through the open AV valve while the ventricles are in the diastole
* Semilunar valves remain closed
* **Isovolumic contraction**
* Occurs at the beginning of the ventricular contraction
* AV valves are forced cloths; produce “lubb” sound
* Semilunar valve remain closed
* Atria remain in diastole
* **Ventricular Ejection**
* Takes place later in the ventricular contraction; when pressure on blood in the ventricles forces the semilunar valves to open
* Blood is ejected into the arterial trunks
* Atria remain in diastole; Av valves remain closed
* **Isovolumic Relaxation**
* Occurs at the start of ventricular relaxation
* Semilunar valves close to prevent blood backflow into the ventricles; produces “dupp” sound
* The AV valve remain closed and the atria remain in diastole
* **Atrial relaxation and ventricular filling**
* Occur during the continuation of ventricular relaxation
* Atria remain in diastole
* The AV valve opens; passive filling of the ventricles from the atria begins and continues as most of the ventricular filling occurs
* Semilunar valves remain closed
12
New cards
Heart Sounds
* Caused by closing of valves
* Changes in normal sound can be diagnostic
* **Heart murmur**
* First indication of heart valve problems
* Result of turbulence of the blood as it passes through the heart
* May cause valvular leakage, decreased valve flexibility, or misshapen valve
* **Valvular insufficiency**
* Occurs when one or more of the cardiac valves leaks because the valve cusps do no close tightly enough
* May be caused by inflammation or disease
* **Valvular Stenosis**
* Scarring of the valve cusps so that they become rigid or partially fused and cannot completely open
* Narrows and presents resistance to the flow of blood, decreasing chamber output
* Often the affected chamber undergoes hypertrophy and dilates
* Primary cause is **rheumatic heart disease**
* Changes in normal sound can be diagnostic
* **Heart murmur**
* First indication of heart valve problems
* Result of turbulence of the blood as it passes through the heart
* May cause valvular leakage, decreased valve flexibility, or misshapen valve
* **Valvular insufficiency**
* Occurs when one or more of the cardiac valves leaks because the valve cusps do no close tightly enough
* May be caused by inflammation or disease
* **Valvular Stenosis**
* Scarring of the valve cusps so that they become rigid or partially fused and cannot completely open
* Narrows and presents resistance to the flow of blood, decreasing chamber output
* Often the affected chamber undergoes hypertrophy and dilates
* Primary cause is **rheumatic heart disease**
13
New cards
Electrical Activity in the Heart
* Stepwise progress of Electrical Impulse
* **Step 1:** SA node activity and atrial activation begin (elapsed time=0)
* **Step 2: Atrial Depolarization**; Stimulus spreads across the atrial surfaces and reaches the AV node (elapsed time= 50 msec)
* **Step 3:** There is a 100-msec delay at the AV node. Atrial contraction begins (elapsed time= 150 msec)
* **Step 4:** The impulse travels along the interventricular septum within the AV bundle and the bundle branches to the purkinje fibers and, via the moderator band, to the papillary muscles of the right ventricle (elapsed time= 175 msec)
**Step 5:** ventricular depolarization; The impulse is distributed by Purkinje fibers and relayed throughout the ventricular myocardium. Atrial contraction is completed, and ventricular contraction begins (elapsed time =225 msec)
* **Step 1:** SA node activity and atrial activation begin (elapsed time=0)
* **Step 2: Atrial Depolarization**; Stimulus spreads across the atrial surfaces and reaches the AV node (elapsed time= 50 msec)
* **Step 3:** There is a 100-msec delay at the AV node. Atrial contraction begins (elapsed time= 150 msec)
* **Step 4:** The impulse travels along the interventricular septum within the AV bundle and the bundle branches to the purkinje fibers and, via the moderator band, to the papillary muscles of the right ventricle (elapsed time= 175 msec)
**Step 5:** ventricular depolarization; The impulse is distributed by Purkinje fibers and relayed throughout the ventricular myocardium. Atrial contraction is completed, and ventricular contraction begins (elapsed time =225 msec)