CH32: Patient with Nicotine Use Disorder
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
Learning objectives
• Recognize the health hazards associated with tobacco use.
• Identify components of tobacco products.
• Identify various alternative tobacco products.
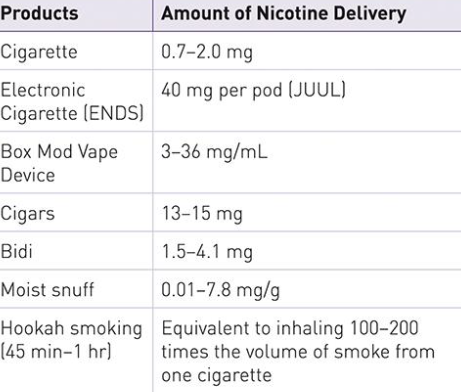
• Explain various mechanisms for nicotine delivery.
• Describe the metabolism of nicotine.
• Recognize the oral manifestations of tobacco use.
• Recognize the effects of environmental tobacco smoke (ETS).
• Assess and develop a dental hygiene care plan for the patient who uses tobacco.
• Recognize protocols for developing a tobacco cessation program.
• Identify the pharmacotherapies and behavioral therapies used for treatment of nicotine addiction.
Health Hazards/Current treads
Nicotine use is the most preventable cause of disease and premature death in the world
90% of deaths from lung cancer
There is no safe form to consume (it’s toxic!)
Types:
• Cigars
• Cigarillos
• Regular pipe
• Waterpipe (Hookah)
• Smokeless tobacco
• ENDS: Electronic nicotine delivery systems (2nd most common)
Cigarette smoking most commonly used nicotine product
Components of tobacco products and smoke
• Nicotine is an addictive psychoactive ingredient in tobacco
• Ignition causes mainstream smoke
• >90 chemicals tobacco products and smoke found to be unsafe
• Carcinogenic
Environmental tobacco smoke
• “Secondhand smoke”
• Passive or involuntary smoke nonusers are exposed to
• Most prevalent among children
• At any level it is deemed unsafe!
• Some toxic concentrations are higher in sidestream smoke than in mainstream smoke.
• Sidestream smoke: the material emitted from burning tobacco products between puffs.
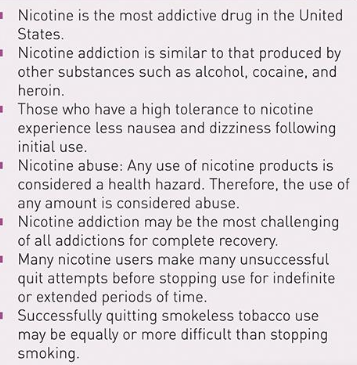
Nicotine addiction
• Addiction: “chronic, progressive, relapsing disease characterized by compulsive use of a substance”
• Tolerance-User’s need to smoke or chew the same product which can decrease the effectiveness = resulting in more product use
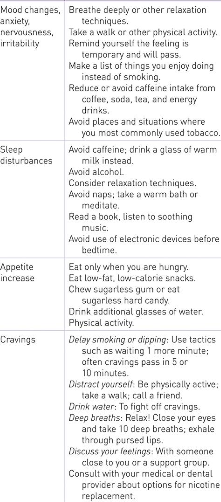
Withdrawal
Refers to “the effects of cessation of nicotine use by an individual in whom dependence is established”
Symptoms may include:
• Dysphoric or depressed mood
• Insomnia
• Irritability, frustration, anger
• Anxiety
• Difficulty concentrating
• Restlessness
• Decreased heart rate
• Increased appetite or weight gain
• Cravings for substance
• Impulsivity
• Anticipatory anhedonia
Facts:
• Patients may experience symptoms within 3 hours of quitting
• Relapse within a week is common
• Most symptoms diminish after a few weeks when relapse does not occur
• Cravings for nicotine, increased appetite, and weight gain are greatest in first 3 months after cessation
• Nicotine replacement is associated with less weight gain
Alleviating nicotine withdrawal symptoms
Metabolism of nicotine
Absorption can occur through:
• Lungs-smoked
• Skin
• Oral mucosa-smokeless
• Buccal mucosa-smokeless
• GI Tract
Metabolized by liver
Excreted in the urine
Ph levels: the more basic, the easier to absorb
• Chewing tobacco is more alkaline
Systemic effects
Cardiovascular Diseases:
• Atherosclerosis (risk factor for CHD)
• Coronary heart disease (#1 death in US)
Pulmonary Diseases:
• COPD: chromic obstructive pulmonary disease
• Emphysema-destruction of bronchial alveoli
• Chronic Bronchitis: excess mucus
Cancer:
• Lung cancer, leading cause of death among cancers
• Smoking can cause various types of cancer (Table 32-2)
Tobacco Use and Other Drugs:
• Tobacco use can contribute to alcohol use
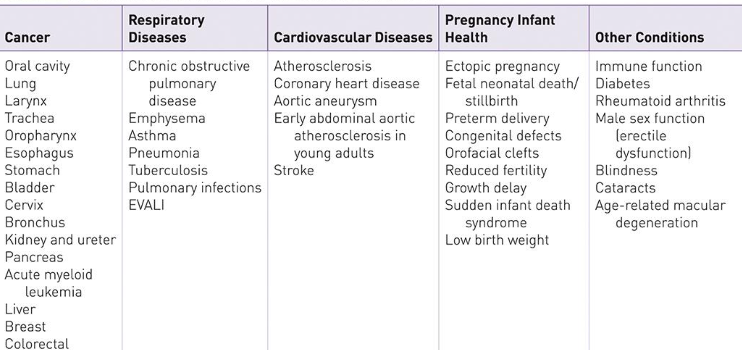
Prenatal and children
Nicotine use during pregnancy
• Miscarriage
• Low birth weight
• Placenta previa
• Preterm delivery
• Spontaneous abortion
• Stillbirth
• Orofacial clefts
ectopic pregnancy
Infancy
• Chemicals are passed down from breast milk
• ETS can cause respiratory issues and SIDs risk
Children
• ETS can affect lung development
• Secondhand smoking can cause early-onset asthma and wheezing
• Increased incidence of middle ear infections
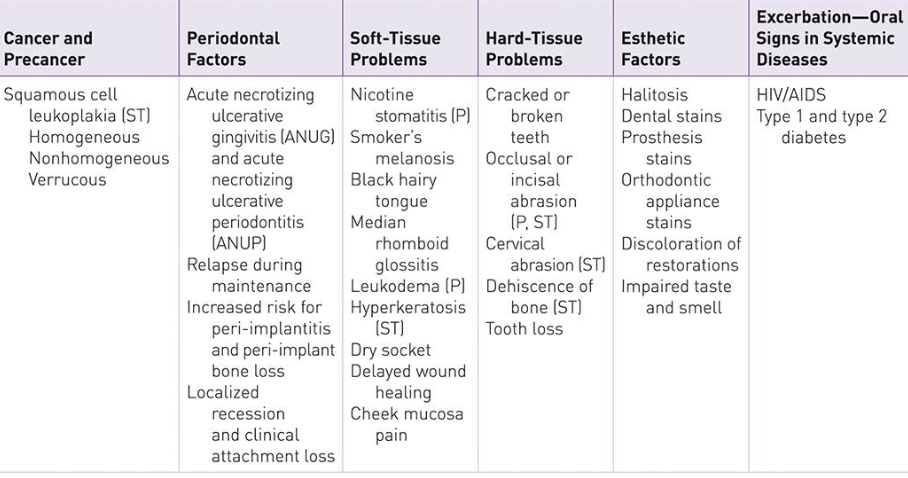
Oral manifestations of tobacco and nicotine use
Electronic cigarettes
oxidative stress=increased risk of infection and cell death to epithelium tissue
cheek and gingival mucosa pain
increased PD, vasoconstriction, RBL
Tobacco and periodontal infections
Major risk factor
Gingivitis
• Degree of inflammatory response to dental biofilm is reduced
• Nicotine use may affect treatment and therapeutic outcomes for plaque-induced gingivitis
Periodontitis in tobacco & e-cigarette users:
• Increased rate and severity of periodontal destruction
• Increased bone loss, attachment loss, and pockets depths
• Diminished gingival blood flow and gingival crevicular flow
• Increased tooth loss from periodontal causes
• Prevalence and severity may lessen with cessation
Mechanisms of periodontal destruction
Host response= lowered immune response
Impairment of revascularization:
• Disruption of immune response
• Impact on healing
• Increased risk of periodontal disease
Increased levels of inflammatory mediators and greater localized tissue destruction
Negative effect on bone metabolism
Response to periodontal treatment
• Weakened response to conventional therapy
• Negative effect on bone regeneration after periodontal therapy
• Increased risk of implant failure
• Delayed healing

Care plan
Assessment:
1. Patient History
Tobacco use status is determined
Identify use of other psychoactive drugs
Check vital signs
2. Extraoral examination
Breath and body odor
Fingers (yellow around fingertips)
Skin
Lips (wrinkles)
3. Intraoral examination
Look for oral consequences of tobacco (Table 32-3)
Clinical treatment procedures
Patients that are tobacco users may require longer and more frequent appointments due to increase of:
• Dental staining
• Calculus
• Dental caries
• Gingival inflammation
• Periodontal issues
1. Dental Biofilm Control
1st priority is self-care for daily biofilm control due increased chance of dental problems
Encourage regular dental care (brushing 2x a day, Flossing) Recommend dental products
2. Nonsurgical Periodontal Therapy
Inform patient that healing will be delayed because of tobacco use and results will vary
Tobacco cessation will help to improve results
3. Diet and Nutrition
Tobacco users may have a poor diet due to effect of tobacco use
Tobacco cessation focuses on diet as well
Reasons for quitting
2/3rds of smokers report an interest in quitting
General health awareness
Specific health problems
Effect on family
Effect of smoking on fetus
Cost
Coughing/lack of breath while exercising
Treatment methods for nicotine cessation
1) Self-help (unassisted)
2) Assisted strategies
Self-help interventions
The following methods are used singularly or most commonly in conjunction with one another:
“Cold Turkey”
Reduce # of nicotine exposures
Join a family member or friend
OTC nicotine replacement aids
Transitioned to a “light” version of cigarettes
Fewer than 1 in 10 report success in this cessation
Assisted strategies for nicotine addiction
Counseling
Interventions by oral health professionals
Pharmacotherapies
Table 32-5 (list of FDA-approved first line pharmacotherapies)
Combination
Counseling and pharmacotherapy
Pharmacotherapies used for treatment of nicotine addiction
1) Nicotine Replacement Therapy
Objective is to prevent withdrawal symptoms and to promote nicotine cessation
Nicotine Gum-transmucosal delivery: nicotine is release while chewing
Nicotine Patch- Transdermal delivery
Nicotine Inhaler- Transmucosal delivery
Nicotine Nasal Spray- Nasal Mucous Membrane delivery
Nicotine lozenge- Transmucosal delivery
2) Nicotine Free Therapy
Bupropion SR-reduce cravings
Varenicline Tartrate (see table 32-5)
Tobacco cessation program
An essential compound to create an oral healthcare plan for patients that use tobacco
Requires multiple appointments, repeated interventions, and multiple attempts from the patient
Use Motivation Interviewing
Person-centered
Goal-directed method of communication
Strengthen intrinsic motivations for change
5 As of Smoking Cessation
Ask
Advise
Assess
Assist
Arrange
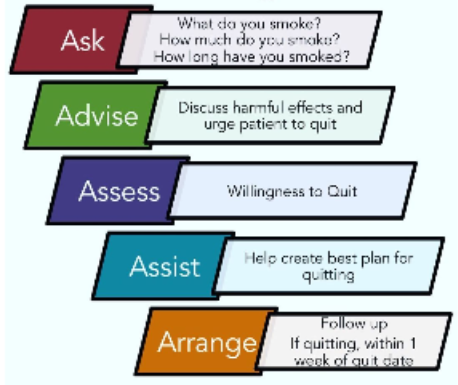
Ask
Health History
Present questions carefully and without judgment
Obtain patient’s confidence and trust
Recognize the type of tobacco product used
don’t assume children and teens don’t smoke
Advise
Advise every patient about nicotine use
Never users or former users: praise their behavior
Current user: Stop-Look-Listen
Stop now: advise the patient to stop and the importance of
stopping
Show: hand patients a mirror to observe the oral examination
Listen: ask the patient their opinion about quitting and why
Assess
Asking the patient if they are ready to quit
If yes: if additional treatment is needed refer to next step
If no: use the 5 R’s
Relevance-why do/do they not want to quit
Risks
Rewards
Roadblocks
Repetition-reinforcement
Assist
Set a quit date (within two weeks)
Encourage the patient to tell their family and friends!
Provide practical counseling
Pharmacotherapy
Provide educational therapy
Support patient
Remove all nicotine products, encourage total abstinence, review past quit attempts (triggers, what worked), provide local/state quit number, inform combo of medication and counseling is beneficial, pamphlets + support groups
Arrange
Follow-up with the patient
Contact patient before quit date and 1 week after quit date
Answer questions that patient might have
1st, 2nd, 3rd month of cessation intense withdrawal so follow up
If relapse, let them reflect and affirm
Documentation
Careful and complete documentation is important for every patient!
Including:
Tobacco history: current and/or past use
Age, ethnicity, gender, periodontal, and dental status, IOEO exam findings
Patient interests/confidence and motivation/readiness to quit
Previous quit attempts and techniques
Options for cessation provided and referrals