VPH 121: Observational Study (Eljon)
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
What is causality?
1. diseases do not occur randomly; thus, there is causation
2. causation includes temporal, spatial, health status of the population
How do we prove causation?
1. describe chain of events from cause to effect
2. study at molecular level
Steps on assessing association
1. assessment of exposure multiplied by risk indicator
2. calculation of risk or odds having a disease
Assessment of exposure
1. when checking exposure: look at outcome
2. when checking outcome: look at exposure
Risk indicators
1. risk ratio
2. odds ratio
Risk ratio
1. an example is the cumulative incidence
2. the first step is to observe the population, and then check the outcome of the exposure for new cases
Odds ratio
1. starts with disease presence
2. there no more risk of developing the disease
Assessing causation
calculates the risk/odds of having a disease
Predictive
1. at risk of disease development due to increased susceptibility
2. for example: CPV in dogs since puppies are more susceptible; thus, you have the "thought" of protecting puppies via vaccine
Diagnostic
1. ruled in via differential diagnosis
2. increased likelihood of disease development due to exposure
Management
promoting vaccination hence animals with vaccines have 5 times more protection than unvaccinated animals
Goals of epidemiology
1. describe health status
2. causality vs. association
3. predict disease occurrence
4. control disease spread
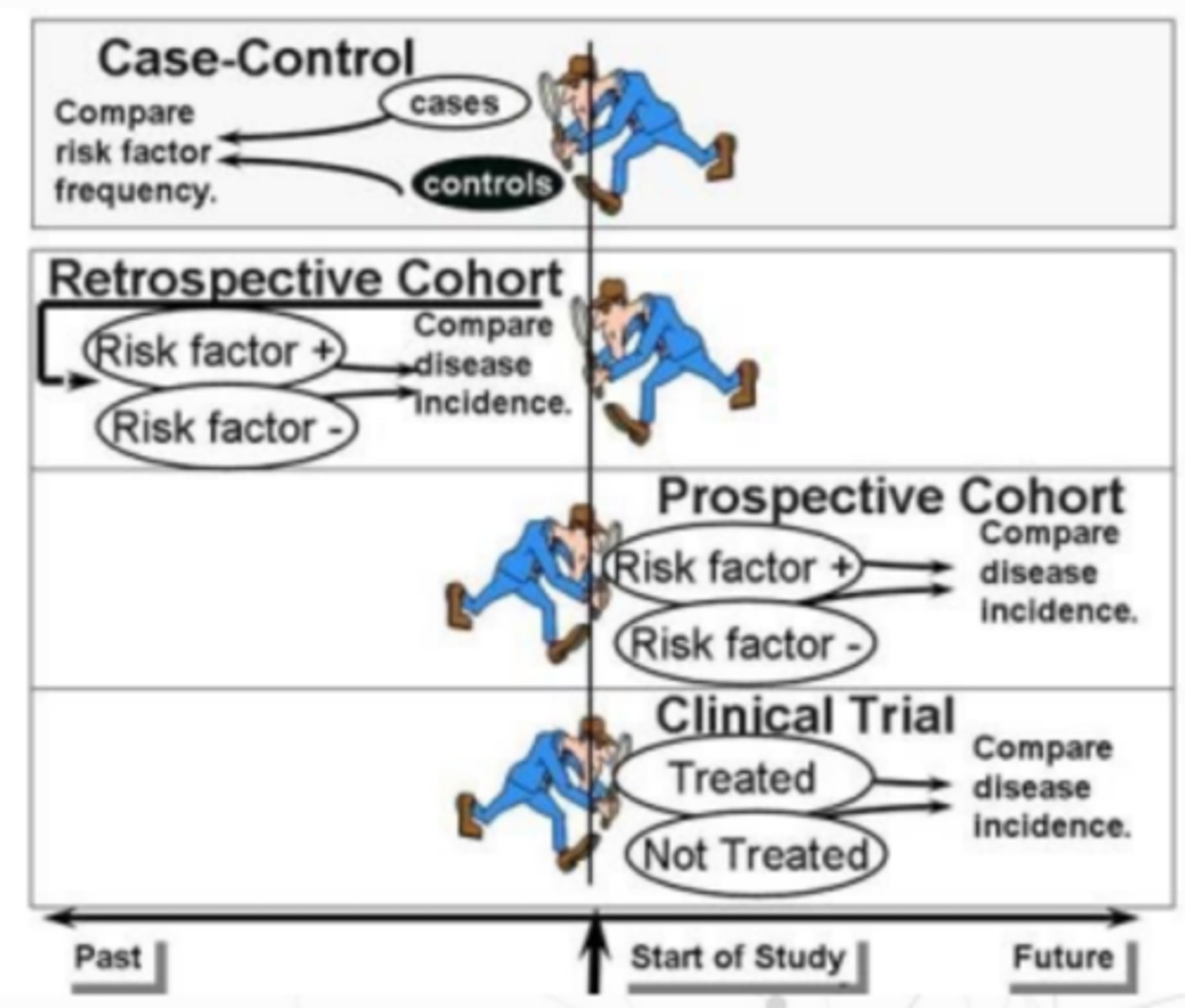
Did the researcher assign exposures?
1. yes: experimental study
2. no: observational study
Is the allocation random in the experimental study?
1. yes: randomized controlled trial
2. no: non-randomized controlled trial
Is there a comparison group in the observational study?
1. yes: analytical study
2. no: descriptive study
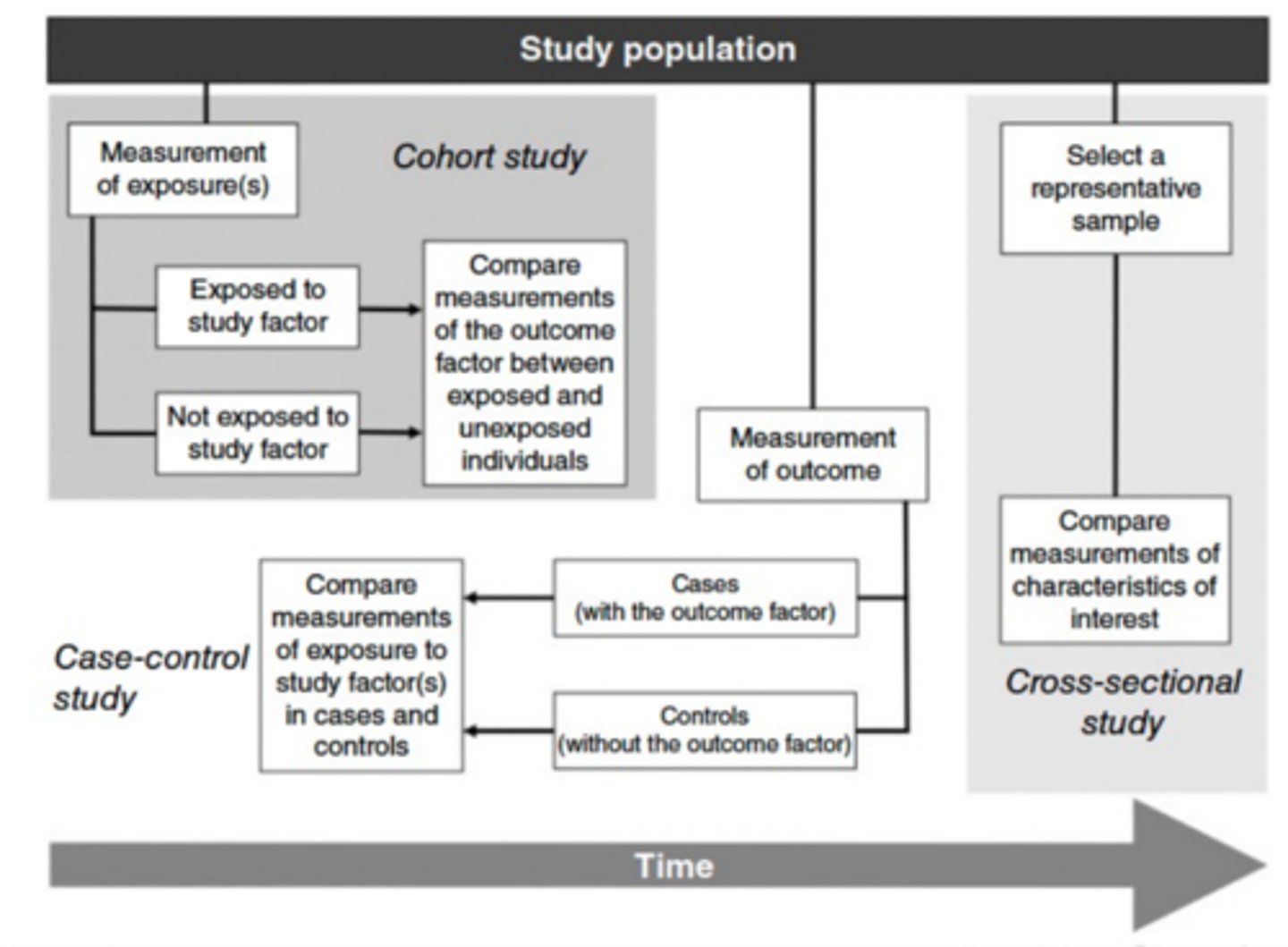
Analytical study types
1. case-control
2. cross-sectional
3. cohort
Descriptive study
1. just comparing; identifying the host and environment of the disease
2. the focus is on individual/population with "newsworthy" clinical occurrence
3. prefers unusual cases
4. more qualitative than quantitative since it only describes what happened
Descriptive study examples
1. case report
2. case series
Case report advantages
1. intensive since only focuses on 1 disease
2. detailed
Case report disadvantages
1. subjective in nature hence prone to bias
2. "focuses" on new disease
Case series
multiple and continuous unusual case occurrences
Case report examples
1. A cartilaginous choristoma in a pig liver: a case report
2. Silent histomoniasis on a brooder farm
3. CPV infection in Turkey
Cases series examples
1. Rickets: Case Series and diagnostic review of hypovitaminosis D in swine
2. Idiopathic Eosinophilic Pneumonia with Associated Pulmonary Vasculitis in Horse: A Case Series
Analytical study
there is a comparison group; comparing diseased and non-diseased populations
Assessing causation using the first three rules of Evan:
1. higher prevalence in exposed
2. higher incidence in exposed
3. exposure to a cause should be present more in a diseased population
when the animal is exposed = it has higher probability of getting diseased
Types of analytical studies
1. cohort
2. case control
3. cross sectional
Cohort study
1. most effective in assessing causal hypotheses
2. example: investigate the effect of spaying on urinary incontinence
3. starts with the cause before getting the effect
4. studies the progression of the exposed group
2 types of cohort study
prospective and retrospective
Cohort study starts with a population that has a?
similar characteristic
Cohort study answers the question?
"will the disease develop of not?"
Cohort study groups are divided into?
exposed and unexposed
Prospective cohort study
start with today and check the outcome tomorrow
Retrospective cohort study
start with yesterday and check the outcome today
Cohort study diagram
example of a cohort study: starts with the population that drinks colostrum from infected mothers
exposed: intact female dogs, unexposed: spayed dogs
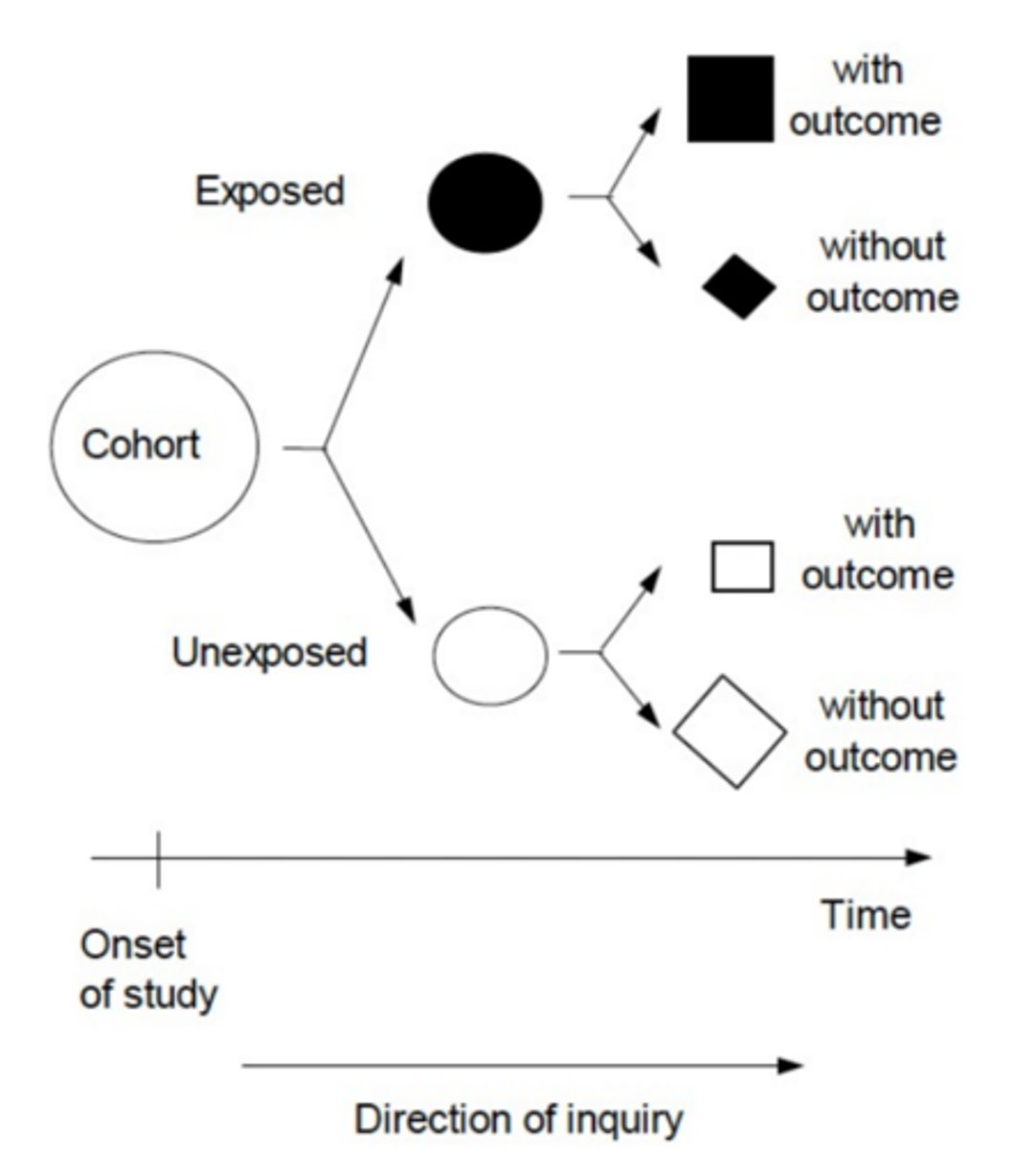
Cohort
a population with a shared characteristic (e.g. students taking VPH 121)
Cohort study advantages
1. calculation of incidence (or cumulative incidence aka "risk" since there is development of new cases in cohort studies)
2. flexible in choosing variables (no control over who is getting exposed hence, there is no bias)
3. investigate multiple outcomes and potential risk factors
4. rare exposures (since subjects are selected by their exposure status)
5. progression of the disease
6. temporal cause and effect relationship
7. second choice if experimental studies are unethical
Cohort study disadvantages
1. sampling error (since you have to select samples because you cannot sample everyone)
2. large population size for rare diseases (a small population will lead to low prevalence and incidence values)
3. long duration of follow-up
4. difficulty in follow-up
5. high cost
6. confounding variables (common when the study gets prolonged)
Sampling error in cohort studies
since subjects are selected, the sampling error can be disregarded due to overestimation or underestimation
Cohort study and cumulative incidence
1. cumulative incidence must be calculated in a cohort study
2. in a cohort study, the more appropriate measure to compute is the risk
Cohort and experimental study
similar; but there is a "control " in experimental studies
Relative risk
the ratio between cumulative incidence or risks between the exposed and unexposed groups
Relative risk answers the question?
how many times more (or less) likely are exposed individuals to get the disease compared to the unexposed individuals
RR > 1
high likelihood of association
RR = 1
no association
RR < 1
not an exposure, protective effect
Prospective and retrospective cohort studies diagram
Attributable risk
absolute measure of excess risk in the exposed from the unexposed group
Attributable risk formula
AR = AR exposed - AR unexposed
AR > 0
excess absolute risk
AR = 0
absence of additional risk (there is still a risk but there is no additional)
AR < 0
not a risk factor, protective factor
Case control study selects?
diseased and disease-free populations
Case control study is effective in studying diseases with?
low incidence and conditions with long follow-up
Case control study has no measure of disease frequency because?
sampling is chosen due to disease presence
Case control study is the opposite of cohort study since?
we will start with the outcome and check previous exposures
Prospective case control study
non-existent; a case control study will always be retrospective
Case control study
1. incidence and prevalence cannot be computed since there are no new cases and there is a predetermined population
2. example: investigate the risk factors for those with urinary incontinence
3. an example of a longitudinal study since there is a duration of time
4. studies diseased vs. disease-free populations
Case control study starts with?
outcome then checking the history of the exposed and unexposed groups
Case control study answers the question?
"what happened?"
Case control study advantages
1. rare diseases
2. diseases with long incubation or latent periods
3. fast conduct
4. low cost (since less time is spent and records are used instead; thus, there is no follow-up)
5. few subjects are required (looks at outcome already)
6. available records
7. absence of risk
8. multiple exposures
Case control study disadvantages
1. sampling error
2. poor quality of records
3. difficulty in validation
4. no control on variables
5. selecting a control group
6. no assessment of temporal sequence (since the effect came first before the cause; opposite of the natural course of diseases)
7. rare exposures (since the cases already happened, hard to assess exposure)
8. limited to one outcome
Case control study odds ratio
ratio between odds of disease in exposed and unexposed groups
OR > 1
highly associated
OR = 1
not associated
OR < 1
less association
Cross-sectional study
1. random selection and examination of a population at
one point in time
2. describing disease occurrence at the time of collection
3. only type of study that is not longitudinal
4. records can be used (similar to case control studies)
A cross-sectional study can be challenging when investigating causal hypotheses, because?
there is no cause in the equation since cross-sectional study only checks the outcome prevalence
Cross-sectional study has no idea about the?
possible exposures that happened in the past
What type of study is: "How many developed urinary incontinence in dogs from Batong Malake during October 2023? What are possible risk factors?"
cross-sectional study
2 MULTIPLE CHOICE OPTIONS
Prevalence of cross-sectional studies is?
computed since there is a need for the number of diseased animals at a certain time
Cross-sectional study advantages
1. estimation of prevalence (in larger populations) or positivity rate (in smaller populations)
2. fast conduct
3. moderate cost (since it only identifies animals with the disease)
4. records can be used occasionally
5. no risk to subjects (except for the subject involved in sample collection)
6. multiple exposures and outcomes
Cross-sectional study disadvantages
1. rare diseases and exposures (since there will be low prevalence)
2. diseases with short duration (checking the disease at one period of time; the result would turn out with low prevalence)
3. uncontrolled extraneous variables (no idea of what happened before and after)
4. estimation of incidence (not monitored into time)
5. temporal pattern (since it can be non-established)
6. poor quality of records
Cohort study flow
cohort group -> exposure -> outcome
Case control flow
outcome -> exposure
Cross-sectional study flow
absent = the exposure and outcome happens at the same time since it is cross-sectional
Analytical study diagram
Descriptive study diagram