Introduction to TSE's
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
What are the main characteristics of TSE diseases?
-Long incubation period
-Progressive and invariably fatal
-Holes in brain give spongiform texture
-No signs of fever
-No signs of inflammation
-No antibody response
-No signs of a pathogen with a genome
-No sign of infection
What causes TSE diseases?
Prions (infectious proteins).
What are prions?
-Host protein encoded by the PrP (Protease-resistance Protein) disease
-PrPc is the normal form and PrPSc is associated with disease
What is the difference between PrPc and PrPSc?
They have an identical amino acid structure but differ in conformation (tertiary structure).
How does PRP cause TSE disease?
-PrPSc converts PrPc to PrPsc
-PrPSc is partially resistance to proteases and hence can't be degraded
-This means that it accumulates in the brain leading to disease
-Initial production of PrPSc can be spontaneous or by process of infection
Why are prion diseases unique?
They can originate sporadically whereas all other infectious diseases are caught and passed on.
Describe the oral route of infection of prions in sheep
Entry to body through the ileal Peyer’s patch (lymphoid nodules in the ileum of small intestine).
Dissemination through 2 routes:
-Lymphoreticular system (LRS), tonsil, spleen, retropharyngeal and mesenteric lymph nodes. PrPSc is detectable in the LRS just weeks/months after infection, primarily within the follicular dendritic cells (FDCs) of primary and secondary B-cell follicles. Infection spreads from LRS through the autonomic nervous system to the central nervous system (CNS).
-Peripheral nervous system. Infection spreads through splanchnic nerves (to spine) and vagus nerve (to medulla oblongata of brain)
Describe the neuropathology of TSEs
-Neuron loss
-Astrocytic gliosis (overproduction of astrocytes in area of degeneration)
-Aggregates of PrPSc
-Spongiform change
-Vacuolation
How can we diagnose TSEs?
-Clinical signs
-Bioassay
-Histopathological detection
-Molecular detection of PrPSc
-Cyclic amplification of PrPSc from PrPc
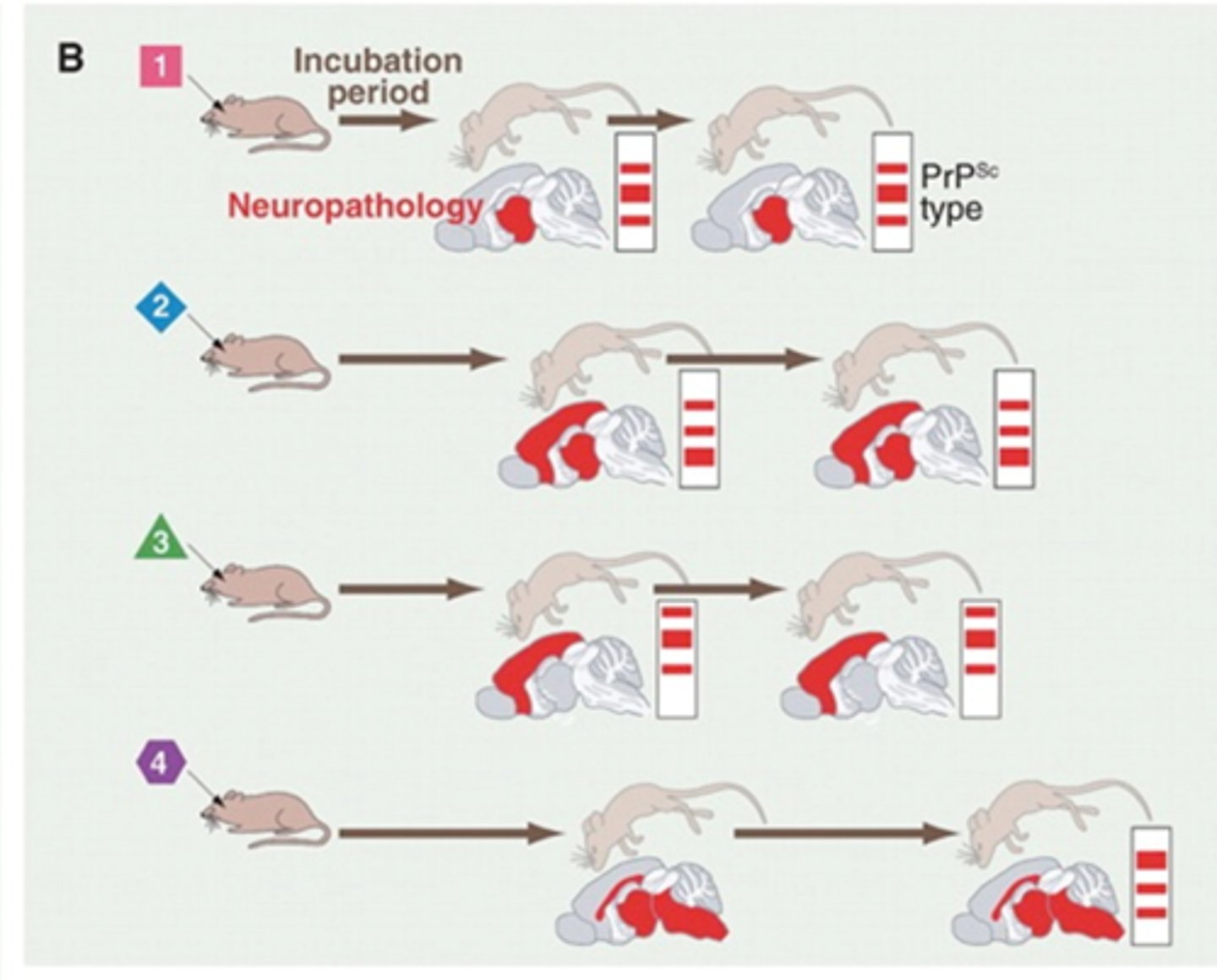
What are the key aspects that differentiate strains of TSEs?
-Incubation period
-Type, severity and distribution of brain lesions
-Western blots
What are some problems for the prion hypothesis?
-Different hosts can have the same strain but different amino acid sequences
-One host can be infected with different strains
What determines the characteristics of different TSE strains?
-Conformation of PrPSc
-Combination of glycoforms
What does a large TSE species barrier mean?
A large infectious dose of the TSE is required for inoculum.
-I.e. A large dose of mouse TSE is required to inoculate a hamster with that strain of TSE
Describe Scrapie
-Disease of sheep and goats
-Characterised by ataxia, tremors, rubbing/scratching, loss of condition and death in 1-3 months
-Endemic in UK
-Incubation of 2-5 years
-Transmission by several routes
-Progression to disease is under strong genetic control
-Occurs as different strains

Describe Bovine Spongiform Encephalopathy (BSE)
-Disease of cattle
-Characterised by ataxia, nervous or aggressive behaviour, loss of condition and death in 1-6 months
-Epidemic in UK
-Can spread to other animals incl humans
-Incubation period of 5 years or more
-Transmision by oral route
-Little evidence of host gentetic effect
-Occurs as 2 different strains
Describe Chronic Wasting Disease (CWD)
-Disease of free-ranging deer
-Only TSE of wild populations & naturally spreading
-Incubation period of 16 months
-Limited genetic control of susceptibility
-Unknown zoonotic potential

Describe Variant Creutzfeldt-Jakob Diseases (VCJD)
-Disease of humans
-Clinical signs include depression, anxiety, hallucinations, ataxia, chorea, dementia
-Causes spongiform changes and PrP-containing florid plaques in the brain
-Illness lasts ~14 mo
-Mean age of onset = 28 years