[Safety and Infection Control] Unit 1: Safe, Effective Care Environment
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
Medical asespsis
refers to the use of precise practices to reduce the number, growth, and spread of micro-organisms (“clean technique”).
It applies to administering oral medication, managing nasogastric tubes, providing personal hygiene, and performing many other common nursing tasks.
Surgical asepsis
refers to the use of precise practices to eliminate all micro-organisms from an object or area and prevent contamination (“sterile technique”).
It applies to parenteral medication administration, insertion of urinary catheters, surgical procedures, sterile dressing changes, and many other common nursing procedures.
Before beginning any task or procedure that requires aseptic technique, health care team members must check for:
Latex allergies
Most facilities use non-latex (nitrile) gloves. However, it is the health care team’s responsibility to identify latex allergies and use items that are latex-free.
Wash hands with soap and warm water
Place hands under running water. Add soap and rub hands together vigorously for at least 15 seconds to remove transient flora and up to 2 minutes when hands are more soiled. Rinse under running water. After washing, dry hands with a clean paper towel before turning off the faucet.
If the sink does not have foot or knee pedals for turning off the water, use a clean, dry paper towel to turn off the faucet(s).
Practices that Maintain a Sterile Field
Prolonged exposure to airborne micro-organisms can make sterile items non-sterile.
Only sterile items can be in a sterile field.
The outer wrappings and 1-inch edges of packaging that contains sterile items are not sterile. The inner surface of the sterile drape or kit, except for that 1-inch border around the edges, is the sterile field to which other sterile items can be added. To position the field on the table surface, grasp the 1-inch border before donning sterile gloves.
Discard any object that comes into contact with the 1-inch border. QS
Microbes can move by gravity from a non-sterile item to a sterile item.
Do not reach across or above a sterile field.
Do not turn your back on a sterile field.
Hold items to add to a sterile field at a minimum of 6 inches above the field.
Any sterile, non-waterproof wrapper that comes in contact with moisture becomes non-sterile by a wicking action that allows microbes to travel rapidly from a non-sterile surface to the sterile surface.
Keep all surfaces dry.
Discard any sterile packages that are torn, punctured, or wet.
Sterile Unfolding Flap Order
Farthest from body
Unless the nurse pulls the top flap (the one farthest from her body) away from the body first, there is a risk of touching part of the inner surface of the wrap and thus contaminating it.
Side flap closest to surface
Next side flap
Flap closest to body
Types of Pathogens
Bacteria (Staphylococcus aureus, Escherichia coli, Mycobacterium tuberculosis)
Viruses: Organisms that use the host’s genetic machinery to reproduce (HIV, hepatitis, herpes zoster, herpes simplex virus [HSV], SARS-CoV-2 [COVID-19])
Fungi: Molds and yeasts (Candida albicans, Aspergillus)
Prions: Protein particles (new variant Creutzfeldt-Jakob disease)
Parasites: Protozoa (malaria, toxoplasmosis) and helminths (worms [flatworms, roundworms], flukes [Schistosoma])
Virulence
the ability of a pathogen to invade and injure a host.
Herpes Zoster
common viral infection that erupts years after exposure to chickenpox and invades a specific nerve tract.
Nonspecific Innate (Native)
restricts entry or immediately responds to a foreign organism (antigen) through the activation of phagocytic cells, complement, and inflammation. This occurs with all micro-organisms, regardless of previous exposure.
Nonspecific Innate (Passive)
Antibodies are produced by an external source.
Temporary immunity that does not have memory of past exposures
Intact skin, the body’s first line of defense
Mucous membranes, secretions, enzymes, phagocytic cells, and protective proteins
Inflammatory response with phagocytic cells, the complement system, and interferons to localize the invasion and prevent its spread
Specific Adaptive Immunity
allows the body to make antibodies in response to a foreign organism (antigen). This reaction directs against an identifiable micro-organism.
Specific Adaptive Immunity (Active)
Antibodies are produced in response to an antigen.
Requires time to react to antigens
Provides permanent immunity
Involves B- and T-lymphocytes
Produces specific antibodies against specific antigens (immunoglobulins [IgA, IgD, IgE, IgG, IgM])
Stages of an Infection
Incubation: interval between the pathogen entering the body and the presentation of the first finding
Prodromal stage: interval from onset of general findings to more distinct findings; during this time, the pathogen multiplies
Illness stage: interval when findings specific to the infection occur
Decline stage: interval when manifestations begin to subside as the number of pathogens decrease
Convalescence: interval when acute findings disappear, total recovery taking days to months
Health-Care Associated Infections
Formerly called nosocomial infections, these can come from an exogenous source (from outside the client) or an endogenous source (inside the client when part of the client’s flora is altered).
Often occur in the intensive care unit.
The best way to prevent HAIs is through frequent and effective hand hygiene.
A common site of HAIs is the urinary tract and these are often caused by Escherichia coli, Staphylococcus aureus, and enterococci. Other sites of HAIs are surgical wounds, the respiratory tract, and the bloodstream.
An iatrogenic infection is a type of HAI resulting from a diagnostic or therapeutic procedure.
HAIs are not always preventable and are not always iatrogenic.
Use current evidence-based practice guidelines to prevent HAIs due to multidrug-resistant organisms. QEBP
Iatrogenic infection
type of HAI resulting from a diagnostic or therapeutic procedure.
Older Client Infection Risks
slowed response to antibiotic therapy
slowed immune response
loss of subcutaneous tissue and thinning of the skin
decreased vascularity
slowed wound healing
decreased cough and gag reflexes
chronic illnesses
decreased gastric acid production
decreased mobility
bowel and bladder incontinence
dementia
greater incidence of invasive devices (a urinary catheter or feeding tube).
Older Client Expected Findings (Infection)
Have a reduced inflammatory and immune response and thus might have an advanced infection before it is identified.
Atypical findings (agitation, confusion, or incontinence) can be the only manifestations.
Expected Findings (Infection)
(dyspnea, cough, purulent sputum, and crackles in lung fields, dysuria, urinary frequency, hematuria and pyuria, rash, skin lesions, purulent wound drainage, erythema and odynophagia, dysphagia, hyperemia, enlarged tonsils, change in level of consciousness, nuchal rigidity, photophobia, headache).
Inflammation Stages
Findings during the first stage of the inflammatory response (local infection) include the following.
Redness (from dilation of arterioles bringing blood to the area)
Warmth of the area on palpation
Edema
Pain or tenderness
Loss of use of the affected part
In the second stage, the micro-organisms are killed. Fluid containing dead tissue cells and WBCs accumulates and exudate appears at the site of the infection. The exudate leaves the body by draining into the lymph system. The types of exudates are:
Serous (clear).
Sanguineous (contains red blood cells).
Purulent (contains leukocytes and bacteria).
In the third stage, damaged tissue is replaced by scar tissue. Gradually, the new cells take on characteristics that are similar in structure and function to the old cells.
Infection/Inflammation Lab Values
Leukocytosis (WBCs greater than 10,000/µL)
Increases in the specific types of WBCs (BANDS) on differential (left shift = an increase in neutrophils)
Elevated erythrocyte sedimentation rate (ESR) over 20 mm/hr; an increase indicates an active inflammatory process or infection
Presence of micro-organisms on culture of the specific fluid/area
Infection/Inflammation Diagnostic Procedures
Gallium scan: Nuclear scan that uses a radioactive substance to identify hot spots of WBCs
Radioactive gallium citrate: Injected by IV and accumulates in area of inflammation
X-rays, CT scan, magnetic resonance imaging (MRI), and biopsies to determine the presence of infection, abscesses, and lesions
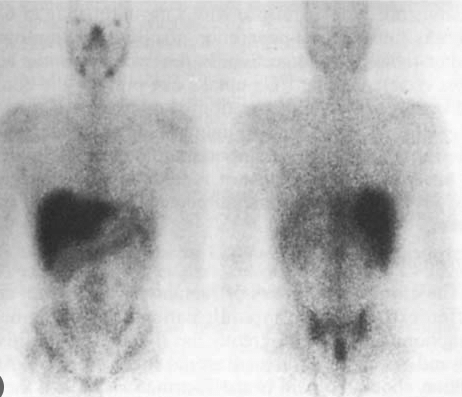
Gallium scan
Nuclear scan that uses a radioactive substance to identify hot spots of WBCs

Radioactive gallium citrate
Injected by IV and accumulates in area of inflammation
X-rays, CT scan, magnetic resonance imaging (MRI), and biopsies
determine the presence of infection, abscesses, and lesions
Good oral hygiene
decreases the protein (which attracts micro-organisms) in the oral cavity, which thereby decreases the growth of micro-organisms that can migrate through breaks in the oral mucosa.
Pulmonary hygiene
Every 2 hours
Turning, coughing, deep breathing, incentive spirometry
Indication: Immobility, COPD, etc
Decreases the growth of micro-organisms and the development of pneumonia by preventing stasis of pulmonary excretions, stimulating ciliary movement and clearance, and expanding the lungs.
Respiratory hygiene and cough etiquette
Covering the mouth and nose when coughing and sneezing.
Using facial tissues to contain respiratory secretions and disposing of them promptly into a hands-free receptacle.
Wearing a surgical mask when coughing to minimize contamination of the surrounding environment.
Turning the head when coughing and staying a minimum of 3 ft away from others, especially in common waiting areas.
Performing hand hygiene after contact with respiratory secretions and contaminated objects/materials.
Airborne Precautions
Protect against droplet infections smaller than 5 mcg (measles, varicella, SARS-CoV-2, pulmonary or laryngeal tuberculosis).
Use N95, especially for TB and SARS-CoV-2
Negative pressure airflow exchange in the room of at least six to 12 exchanges per hour, depending on the age of the structure.
If splashing or spraying is a possibility, wear full face (eyes, nose, mouth) protection.
Clients who have an airborne infection should wear a mask while outside of the room/home.
Wear a gown when performing care that might result in contamination from secretions.
Negative pressure airflow exchange in the room of at least six to 12 exchanges per hour
Airborne Precaution
Droplet Precautions
Protect against droplets larger than 5 mcg and travel 3 to 6 ft from the client (streptococcal pharyngitis or pneumonia, Haemophilus influenzae type B, scarlet fever, rubella, pertussis, mumps, mycoplasma pneumonia, meningococcal pneumonia and sepsis, pneumonic plague).
Clients who have a droplet infection should wear a mask while outside of the room/home.
Wear a gown when performing care that might result in contamination from secretions.
Wear a gown when performing care that might result in contamination from secretions.
All Precautions
Protective Environment
An intervention (not type of precautions) to protect clients who are immunocompromised. This includes clients who have had an allogeneic hematopoietic stem cell transplant.
Positive airflow 12 or more air exchanges/hr.
HEPA filtration for incoming air.
Mask for the client when out of room.
Positive airflow 12 or more air exchanges/hr.
Protective Environment
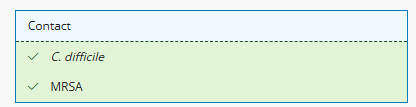
Contact precaution microbes
(respiratory syncytial virus, shigella, enteric diseases caused by micro-organisms, wound infections, herpes simplex, impetigo, scabies, multidrug-resistant organisms).
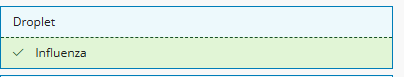
Droplet precaution microbes
(streptococcal pharyngitis or pneumonia, Haemophilus influenzae type B, scarlet fever, rubella, pertussis, mumps, mycoplasma pneumonia, meningococcal pneumonia and sepsis, pneumonic plague).
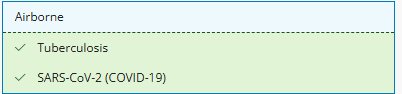
Airborne precaution microbes
(measles, varicella, SARS-CoV-2, pulmonary or laryngeal tuberculosis).
Antipyretics
Acetaminophen
Aspirin
Health care associated infections (Image)
Multidrug-Resistant Infection
Nursing Actions
Obtain specimens for culture and sensitivity prior to initiation of antimicrobial therapy.
Monitor antimicrobial levels and ensure that therapeutic levels are maintained.
Client Education
Complete the full course of antimicrobial therapy.
Avoid overuse of antimicrobials.
Treats MRSA (Methicillin-resistant Staphylococcus aureus)
Vancomycin and linezolid
Lesser known fall risks
Decreased visual acuity, generalized weakness, urinary frequency, gait and balance problems (cerebral palsy, injury, multiple sclerosis), and cognitive dysfunction.
Adverse effects of medications (orthostatic hypotension, drowsiness)
Medicare and Medicaid no longer reimburse for treating injuries resulting from falls.
Seizure Precautions
Make sure rescue equipment is at the bedside, including oxygen, an oral airway, suction equipment, and padding for the side rails
Should have a saline lock in place for immediate IV access.
Ensure rapid intervention to maintain airway patency.
Advise all caregivers and family not to put anything in the client’s mouth (except an airway for status epilepticus) during a seizure.
Advise all caregivers and family not to restrain the client during a seizure but to lower the client to the floor or bed, protect their head, remove nearby furniture, provide privacy, put them on one side with the head flexed slightly forward if possible, and loosen their clothing.
During a Seizure
Stay with the client, and call for help.
Maintain airway patency and suction PRN.
Administer medications.
Note the duration of the seizure and the sequence and type of movements.
After a seizure, determine mental status and measure oxygenation saturation and vital signs. Explain what happened, and provide comfort, understanding, and a quiet environment for recovery.
Document the seizure with any precipitating behavior and a description of the event (movements, injuries, duration of seizures, aura, postictal state), and report it to the provider.
It is inappropriate to use seclusion or restraints for:
Convenience of the staff
Punishment for the client
Clients who are extremely physically or mentally unstable
Clients who cannot tolerate the decreased stimulation of a seclusion room
When all other less restrictive means have failed to prevent a client from harming themselves or others (orientation to the environment, supervision of a family member or sitter, diversional activities, electronic devices), the following must occur before using seclusion or restraints.
The provider must prescribe seclusion or restraints in writing, after a face-to-face assessment of the client.
Restraint Prescription
must include the reason for the restraints
the type of restraints
the location of the restraints
how long to use the restraints
the type of behavior that warrants using the restraints.
The prescription allows only 4 hr of restraints for an adult, 2 hr for clients ages 9 to 17, and 1 hr for clients younger than 9 years of age.
Providers can renew these prescriptions with a maximum of 24 consecutive hours.
Providers cannot write PRN prescriptions for restraints.
Restraint Duration
4 hours (adult)
2 hours (9-17)
1 hour (0-9)
Can be renewed up to 24 hours
Cannot be PRN
Nursing Responsibilities (Restraints)
Assess skin integrity/care every 2 hours
Ask client/guardian to sign consent
Do not secure/tie to side rails
Loose enough to fit 2 fingers
Regularly determine the need to use restraints
Never leave client alone w/o the restraints
Documentation (Restraints)
Precipitating events and behavior of the client prior to seclusion or restraints
Alternative actions to avoid seclusion or restraints
Time of application and removal of the restraints
Type of restraints and location
The client’s behavior while in restraints
Type and frequency of care (range of motion, neurologic checks, removal, integumentary checks)
Condition of the body part in restraints
The client’s response at removal of the restraints
Medication administration
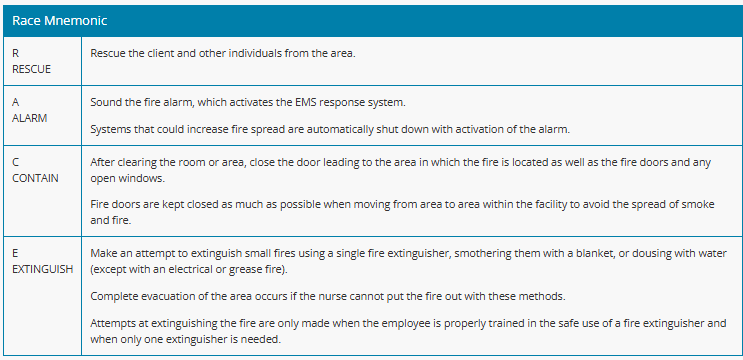
RACE (Fire Response)
R: Rescue and protect clients in close proximity to the fire by moving them to a safer location. Clients who are ambulatory can walk independently to a safe location.
A: Alarm: Activate the facility’s alarm system and then report the fire’s details and location.
C: Contain/Confine the fire by closing doors and windows and turning off any sources of oxygen and any electrical devices. Ventilate clients who are on life support with a bag-valve mask.
E: Extinguish the fire if possible using the appropriate fire extinguisher.
PASS (Fire Extinguisher)
P: Pull the pin.
A: Aim at the base of the fire.
S: Squeeze the handle.
S: Sweep the extinguisher from side to side, covering the area of the fire.
Classes (Fire Extinguishers)
Class A is for combustibles (paper, wood, upholstery, rags, other types of trash fires).
Class B is for flammable liquids and gas fires.
Class C is for electrical fires.
Class D is for metals/metal shavings.
Class K is for kitchen fires involving fats and oils.
Infants and Toddlers: Safety Guidelines
Aspiration Prevention
Keep small objects out of reach and check toys for hazards like small parts or sharp edges.
Avoid feeding infants small, hard foods like peanuts, popcorn, or whole pieces of hot dog.
Do not prop bottles during feeding or place infants in the supine position while feeding.
Use a one-piece pacifier (no strings or ribbons around the neck).
Suffocation Prevention
Follow the "Back to Sleep" rule (place infants on their backs to sleep) and encourage tummy time during the day.
Remove plastic bags and crib toys within the infant's reach; ensure crib slats are properly spaced (no more than 2 3/8 inches apart).
Avoid co-sleeping with infants; use a crib or bassinet.
Secure hazards like latex balloons, swimming pools (fenced/locked), and bathroom items (toilet lids down, doors closed).
Teach caregivers CPR and the Heimlich maneuver.
Poisoning Prevention
Store household chemicals, poisons, and medications in locked, child-proof containers.
Keep the poison control hotline accessible and dispose of expired medications safely.
Inspect for and remove lead hazards like paint chips; educate parents on preventing lead poisoning.
Falls Prevention
Keep crib and playpen rails raised and never leave infants unattended on high surfaces.
Use safety gates and install window guards.
Follow manufacturer guidelines for restraints (highchairs, swings, strollers) and discontinue use as the child outgrows them.
Transition toddlers to low beds once they start climbing.
Motor Vehicle Injury Prevention
Use a rear-facing car seat for infants and toddlers up to 2 years or until height/weight limits are exceeded; switch to a forward-facing seat afterward.
Ensure car seats are federally approved, use a five-point harness, and are installed in the back seat.
For toddlers over 2 years or exceeding rear-facing car seat limits, use a forward-facing car seat or booster seat as per height and weight requirements.
Burns Prevention
Always test bath water and formula temperatures.
Keep pot handles turned inward and use the back burner of the stove.
Supervise faucet use and keep matches/lighters out of reach.
Cover electrical outlets and apply sunscreen (SPF 30 or higher) for outdoor protection.
Safety Guidelines for Preschoolers and School-Age Children
Drowning Prevention
Teach swimming and water safety rules.
Ensure life jackets are worn near water and use a buddy system.
Install fences around pools and supervise near water.
Motor Vehicle Injury Prevention
Use booster seats for children under 4 feet 9 inches or under 40 lbs.
Place children under 12 in the back seat if a car has a passenger airbag.
Teach proper use of seat belts, safe road behavior, and equipment safety.
Encourage playing in safe areas away from traffic.
Sex Education
Begin age-appropriate sex education for school-age children.
Firearm Safety
Keep firearms unloaded, locked, and out of reach.
Teach children to avoid guns and never stay where guns are accessible.
Store bullets separately from guns.
Play Injury Prevention
Ensure bikes are the right size, teach playground safety, and encourage play in safe areas.
Remove hazards like refrigerator doors and use protective equipment (helmets, pads).
Teach children to avoid strangers and inform parents about suspicious individuals.
Burns Prevention
Set water heaters to no higher than 120°F.
Teach the dangers of matches, fireworks, and fire.
Educate on the safe use of kitchen appliances.
Apply SPF 30+ sunscreen and dress children appropriately to prevent sunburn.
Poison
Teach child about the hazards of alcohol, cigarettes, and prescription, non-prescription, and illicit drugs.
Keep potentially dangerous substances out of reach.
Have the poison control hotline number available.
Safety Guidelines for Adolescents
Substance Use and Sexual Health
Educate on the dangers of smoking, alcohol, legal and illegal drugs, and unprotected sex.
Motor Vehicle and Injury Prevention
Ensure completion of a driver’s education course.
Set rules for passenger limits, seat belt use, and avoiding impaired driving.
Highlight risks of distracted driving (e.g., texting, eating).
Promote the use of protective sports equipment.
Monitor for signs of depression, anxiety, or behavioral changes.
Teach firearm safety and water safety (checking depth before diving).
Burns Prevention
Encourage the use of SPF 30+ sunscreen and protective clothing.
Warn against the risks of sunbathing and tanning beds.
Social Media and Online Safety
Parents should monitor, limit, and role model safe social media use.
Young and Middle-Age Adult Guidelines
Safety Concerns
Motor vehicle accidents, occupational injuries, high alcohol use, and suicide are primary concerns.
Client Education
Promote defensive driving and avoiding alcohol while driving.
Educate on the risks of high alcohol consumption, smoking, secondhand smoke, drug use, and caffeine.
Ensure home safety with smoke detectors, fire alarms, and good lighting.
Recognize signs of depression or suicidal thoughts; refer for counseling as needed.
Emphasize water safety, workplace safety, and cautious use of social media.
Encourage protection from excessive sun exposure using SPF 30+ sunscreen and protective clothing.
Older Adult Guidelines
Aging and Safety
Older adults may need to adapt to age-related changes to maintain safety and independence.
Prevention is essential as older adults often experience longer recovery times from injuries.
Reduced tactile sensitivity increases burn risk; assess home safety as needed.
Risk Factors for Falls
Physical, cognitive, and sensory changes.
Musculoskeletal and neurological changes, impaired vision or hearing.
Frequent nighttime bathroom trips due to nocturia and incontinence.
Home Safety Modifications
Remove tripping hazards (e.g., rugs, loose carpets).
Place electrical cords against walls, improve lighting, and ensure safe sidewalks.
Install grab bars in bathrooms, use nonskid mats, and provide assistive devices like shower chairs and bedside commodes.
Elements of a Home Safety Plan
Review oxygen safety measures. Because oxygen can cause materials to combust more easily and burn more rapidly, the client and family must be provided with information on use of the oxygen delivery equipment and the dangers of combustion. Include the following information in the teaching plan:
Use and store oxygen equipment according to the manufacturer’s recommendations.
Place a “No Smoking” sign in a conspicuous place near the front door of the home. A sign can also be placed on the door to the client’s bedroom.
Inform the client and family of the danger of smoking in the presence of oxygen. Family members and visitors who smoke should do so outside the home.
Ensure that electrical equipment is in good repair and well grounded.
Replace bedding that can generate static electricity (wool, nylon, synthetics) with items made from cotton.
Keep flammable materials (heating oil and nail polish remover) away from the client when oxygen is in use.
Follow general measures for fire safety in the home (having a fire extinguisher readily available and an established exit route if a fire occurs).
Carbon monoxide
A very dangerous gas because it binds with hemoglobin and ultimately reduces the oxygen supplied to the tissues in the body.
Cannot be seen, smelled, or tasted.
Manifestations of poisoning include nausea, vomiting, headache, weakness, and unconsciousness.
Death can occur with prolonged exposure.
Measures to prevent poisoning include ensuring proper ventilation when using fuel-burning devices (lawn mowers, wood-burning and gas fireplaces, charcoal grills).
Gas-burning furnaces, water heaters, and appliances should be inspected annually.
Flues and chimneys should be unobstructed.
Detectors should be installed and inspected regularly.
Check batteries at the same time as smoke detector batteries. Change the batteries annually on a specific date, like on a birthday.
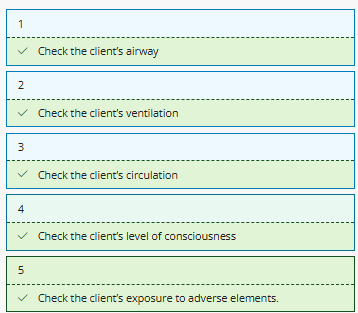
ABCDE Principle
Guides the primary survey and emergency care
Airway/Cervical Spine: This is the most important step in performing the primary survey. If a patent airway is not established, subsequent steps of the primary survey are futile. Protect the cervical spine if head or neck trauma is suspected.
Breathing: After achieving a patent airway, assess for the presence and effectiveness of breathing.
Circulation: After ensuring adequate ventilation, assess circulation.
Disability: Perform a quick assessment to determine the client’s level of consciousness.
Exposure: Perform a quick physical assessment to determine the client’s exposure to adverse elements (heat or cold).
Sprains (RICE)
Refrain from weight-bearing.
Apply ice to decrease inflammation.
Apply a compression dressing to minimize swelling.
Elevate the affected limb.
Fractures and splinting
Assess the site for swelling, deformity, and skin integrity.
Assess temperature, distal pulses, and mobility.
Apply a splint to immobilize the fracture. Cover open areas with a sterile cloth if available.
Reassess neurovascular status below the injury site after splinting.
Bleeding
Identify any sources of external bleeding and apply direct pressure to the wound site.
DO NOT remove impaling objects. Instead, stabilize the object.
Internal bleeding can require intravascular volume replacement with fluids and/or blood products, or surgical intervention.
Heat stroke
Body temperature greater than 40° C [104° F]) quickly and treat it aggressively.
Manifestations include hot, dry skin; hypotension; tachypnea; tachycardia; anxiety; confusion; unusual behavior; seizures; and coma.
The client does not sweat.
Intervene to provide rapid cooling.
Remove the client’s clothing.
Place ice packs over the major arteries (axillae, chest, groin, neck).
Apply a hypothermia blanket to promote cooling.
Irrigate the stomach and large intestine with cooling solution.
Wet the client’s body, then fan with rapid movement of air.
Do not allow client to shiver. If client shivers, cover with a sheet.
Frostnip and frostbite
Occurs when the body is exposed to freezing temperatures.
Common sites include the earlobes, tip of the nose, fingers, and toes.
Frostnip does not lead to tissue injury and can be treated by warming.
Frostbite presents as white, waxy areas on exposed skin. Tissue injury occurs.
Frostbite can be full- or partial-thickness.
Warm the affected area in a 37° to 42° C (98.6° to 108° F) water bath.
Provide pain medication.
Administer a tetanus vaccination.
Burns
Burns can result from electrical current, chemicals, radiation, or flames.
Home hazards include pot handles that protrude over the stove, hot bath water, and electrical appliances.
Remove the agent (electrical current, radiation source, chemical).
Smother any flames that are present. Perform a primary survey.
Cover the client and maintain NPO status.
Elevate the client’s extremities if not contraindicated (presence of a fracture).
Perform a head-to-toe assessment and estimate the surface area and thickness of burns.
Administer fluids and a tetanus toxoid.
Altitude Illness
Clients can become hypoxic in high altitudes. Can progress to cerebral and pulmonary edema and requires immediate treatment.
Expected Findings
Throbbing headache
Nausea
Vomiting
Dyspnea
Anorexia
Nursing Interventions
Administer oxygen.
Descend to a lower altitude.
Provide pharmacological therapy (steroids and diuretics) if indicated.
Promote rest.
BLS
Involves the CABs (Chest Compression, Airway, and Breathing) of CPR. QEBP
Assess client for a response and look for breathing. Do not take time to perform a “look, listen, and feel” assessment of breathing. If there is no breathing or no normal breathing (only gasping), call for help.
If alone, activate emergency response system and get an automated external defibrillator (AED), if available, and return to the client. If a second person is available, ask the second person to activate the emergency response system and get an AED.
Check pulse. Begin CPR compressions alternated with breaths if a pulse is not detected.
Guidelines for Preventing Injury
Know your facility’s policies for lifting and safe client handling.
Have one or more staff members assist with positioning clients. Moving them up in bed is a significant cause of back pain and injury.
Plan ahead for activities that require lifting, transfer, and ambulation of a client, and ask others to be available to assist.
Prepare the environment by removing obstacles prior to the procedure.
Explain the process to the client and assistants to clarify their roles.
Be aware that the safest way to lift a client is with assistive equipment.
Rest between heavy activities to decrease muscle fatigue.
Maintain good posture and exercise regularly to increase the strength of your arms, legs, back, and abdominal muscles, so these activities will require less energy.
Keep your head and neck in a straight line with your pelvis to avoid neck flexion and hunched shoulders, which can cause impingement of nerves in your neck.
Use smooth movements when lifting and moving clients to prevent injury from sudden or jerky muscle movements.
When standing for long periods of time, flex your hips and knees by using a footrest.
When sitting for long periods of time, keep your knees slightly higher than your hips.
Avoid repetitive movements of the hands, wrists, and shoulders. Take a break every 15 to 20 min to flex and stretch joints and muscles whenever possible.
Semi-fowlers (15-45, usually 30)
This position prevents regurgitation of enteral feedings and aspiration by clients who have difficulty swallowing.
It also promotes lung expansion for clients who have dyspnea or are receiving mechanical ventilation.
Fowlers (45-60)
This position is useful during procedures (nasogastric tube insertion and suctioning). It allows for better chest expansion and ventilation and better dependent drainage after abdominal surgeries.
High-fowlers (60-90)
This position promotes lung expansion by lowering the diaphragm and thus helps relieve severe dyspnea.
It also helps prevent aspiration during meals.
Supine or dosal recumbent
The client lies on their back with the head and shoulders elevated on a pillow and forearms on pillows or at their sides. A foot support prevents foot drop and maintains proper alignment. Ensure that the vertebrae are in straight alignment without excessive flexion or extension of the head and neck.
Prone
This position promotes drainage from the mouth after throat or oral surgery, but inhibits chest expansion. It is for short-term use only.
This position helps prevent hip flexion contractures following a lower extremity amputation.
Lateral or side-lying
The client lies on their side with most of the weight on the dependent hip and shoulder and the arms in flexion in front of the body. They should have a pillow under the head and neck, upper arms, and legs and thighs to maintain body alignment.
This is a good sleeping position, but the client needs turning regularly to prevent the development of pressure ulcers on the dependent areas. A 30° lateral position is essential for clients at risk for pressure ulcers.
Lateral Semi-prone Recumbent Position
The client is on their side halfway between lateral and prone positions, with the weight on their anterior ileum, humerus, and clavicle. The lower arm is behind them while the upper arm is in front. Both legs are in flexion, but the upper leg is flexed at a greater angle than the lower leg at the hip as well as at the knee. It differs from the side-lying position in the distribution of the client’s weight.
This is a comfortable sleeping position for many clients, and it promotes oral drainage.
Orthopneic
The client sits in the bed or at the bedside with a pillow on the overbed table, which is across the client’s lap. They rest their arms on the overbed table.
This position allows for chest expansion and is especially beneficial for clients who have COPD.
Trendelenburg
This position facilitates postural drainage and venous return.
Reverse Trendelenburg
This position promotes gastric emptying and prevents esophageal reflux.
Modified Trendelenburg
The client remains flat with the legs above the level of their heart.
This position helps prevent and treat hypovolemia and facilitates venous return.
Internal emergencies
Include loss of electric power or potable water, loss of communication ability, disruption of computer information systems, and severe damage or casualties within the facility related to fire, weather (tornado, hurricane), explosion, or a terrorist act.
Readiness includes evacuation and relocation plans, procedures to notify extra personnel, safety and hazardous materials protocols, and infection control policies and practices.
External emergencies
Include hurricanes, floods, volcano eruptions, earthquakes, disease epidemics, industrial accidents, chemical plant explosions, major transportation accidents, building collapse, and terrorist acts (including biological and chemical warfare).
Readiness includes a plan for participation in community-wide emergencies and disasters.
The Joint Commission and Emergency Preparedness
Conducting two emergency preparedness drills each year.
Drills should include an influx of clients beyond those being treated by the facility. QS
Drills should include either an internal or an external disaster (a situation beyond the normal capacity of the facility).
Participating in one community-wide practice drill per year.
Categories of triage during mass casualty events
Emergent or Immediate Category (Class I): Highest priority is given to clients who have life-threatening injuries but also have a high possibility of survival once they are stabilized.
Urgent or Delayed Category (Class II): Second-highest priority is given to clients who have major injuries that are not yet life-threatening and can usually wait 30 min to 2 hr for treatment.
Nonurgent or Minimal Category (Class III): The next highest priority is given to clients who have minor injuries that are not life-threatening and do not need immediate attention.
Expectant Category (Class IV): The lowest priority is given to clients who are not expected to live and are allowed to die naturally. Comfort measures can be provided, but restorative care is not.
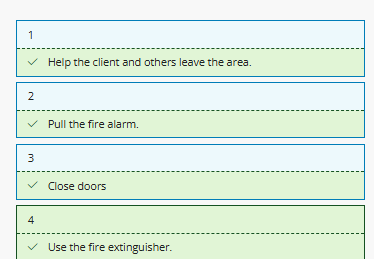
Fire Emergency
If evacuation of the unit is necessary, horizontal (lateral) evacuation is done first. Vertical evacuation to other floors is done if client safety cannot be maintained.
If a nurse discovers a fire that threatens the safety of a client, use the RACE (Rescue, Alarm, Contain, and Extinguish) mnemonic to guide the order of actions.
Turn supplemental oxygen off for clients who can safely tolerate room air.
Ask ambulatory clients to assist removing clients who are in wheelchairs.
RACE Mnemonic (image)
Severe Thunderstorm/Tornado Precautions
Draw shades and close drapes to protect against shattering glass.
Lower beds to the lowest position and move away from the windows.
Place blankets over all clients who are confined to beds.
Close all doors.
Relocate as many ambulatory clients as possible into the hallways (away from windows) or other secure location designated by the facility.
Do not use elevators.
Monitor for severe weather warnings using television, radio, or Internet.
Chemical Incidents
Take measures to protect self and to avoid contact.
Assess and intervene to maintain the client’s airway, breathing, and circulation. Administer first aid as needed.
Remove the offending chemical by undressing the client, removing all identifiable particulate matter. Provide immediate and prolonged irrigations of contaminated areas.
Irrigate skin with running water, with the exception of dry chemicals (lye or white phosphorus). In the case of exposure to a dry chemical, brush the agent off of the client’s clothing and skin.
Gather a specific history of the injury, if possible (name and concentration of the chemical, duration of exposure).
In the event of a chemical attack, have knowledge of which facilities are open to exposed clients and which are only open to unexposed clients.
Follow the facility’s emergency response plans (personal protection measures, the handling and disposal of wastes, use of space and equipment, reporting procedures).
Radiologic Incidents
The amount of exposure is related to the duration of the exposure, distance from source, and amount of shielding.
The facility where victims are treated activates interventions to prevent contamination of treatment areas (floors and furniture are covered, air vents and ducts are covered, radiation-contaminated waste is disposed of according to procedural guidelines).
Wear water-resistant gowns, double glove, and fully cover their bodies with caps, shoe covers, masks, and goggles.
Wear radiation or dosimetry badges to monitor the amount of their radiation exposure.
Survey clients initially with a radiation meter to determine the amount of contamination.
Decontamination with soap, water, and disposable towels occurs prior to entering the facility. Water runoff is contaminated and contained.
After decontamination, resurvey clients for residual contamination. Continue irrigation of the skin until the client is clean of all contamination.
A nurse on a medical-surgical unit is informed that a mass casualty event occurred in the community and that it is necessary to discharge stable clients to make beds available for injury victims. Which of the following clients should the nurse recommend for discharge?
Select all that apply.
A client who is dehydrated and receiving IV fluid and electrolytes
A client who has a nasogastric tube to treat a small bowel obstruction
A client who is scheduled for elective surgery
A client who has chronic hypertension and blood pressure 135/85 mm Hg
A client who has acute appendicitis and is scheduled for an appendectomy
A client who is scheduled for elective surgery
A client who has chronic hypertension and blood pressure 135/85 mm Hg
Bomb Threat
Extend the conversation as long as possible.
Listen for distinguishing background noises (music, voices, traffic, airplanes).
Note distinguishing voice characteristics of the caller.
Ask where and when the bomb is set to explode.
Note whether the caller is familiar with the physical arrangement of the facility.
If a bomb-like device is located, do not touch it. Clear the area and isolate the device as much as possible by closing doors, for example.
Notify the appropriate authorities and personnel (police, administrator, director of nursing).
Cooperate with police and others. Assist to conduct a search as needed, provide copies of floor plans, have master keys available, and watch for and isolate suspicious objects (packages and boxes).
Keep elevators available for authorities.
Remain calm and alert and try not to alarm clients.