MCAT Biology: Endocrine System
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
Hypothalamus
command center sitting at the base of your brain
connects your brain to your endocrine system, mostly through the pituitary gland
GnRH (Gonadotropin-Releasing Hormone)
↑ FSH & LH
Stimulates the gonads (ovaries/testes) to produce sex hormones (estrogen/testosterone) and gametes (eggs/sperm)
Negative Feedback: inhibits GnRH and FSH/LH release
GHRH (Growth Hormone-Releasing Hormone)
↑ GH
Stimulates growth, cell repair, and metabolism
Negative Feedback: inhibits GHRH and GH
TRH (Thyrotropin-Releasing Hormone)
↑ TSH
TSH goes to the thyroid → makes T3/T4, which control metabolism
Negative Feedback: inhibits TRH and TSH
CRH (Corticotropin-Releasing Hormone)
↑ ACTH
ACTH goes to the adrenal cortex → makes cortisol (stress hormone)
Negative Feedback: inhibits CRH and ACTH
High cortisol → low ACTH and CRH?
= exogenous steroids
High prolactin → low GnRH, low FSH/LH?
= prolactinoma
Hypothalamic damage → ↓ releasing hormones
panhypopituitarism
Dopamine (Prolactin-Inhibiting Factor, PIF)
↓ Prolactin
Dopamine inhibits prolactin (which stimulates milk production) — so less dopamine = more prolactin
Prolactin is not part of a negative feedback loop — instead, dopamine suppresses it directly, and high prolactin levels can actually increase dopamine over time in a regulatory way, but it's not a classic axis like the others
ADH & Oxytocin
Made in the hypothalamus but stored & released by the posterior pituitary
ADH: Water retention in kidneys (think: anti-dehydration) —> V2 receptors
Oxytocin: Uterine contractions, milk letdown, bonding
Posterior Pituitary
doesn’t make its own hormones — just releases what the hypothalamus makes
Mechanism of Hormone Types in Hypothalamus
All hypothalamic hormones are peptide hormones
→ act on membrane receptors → second messengers (fast-acting)
The pancreas has two jobs
Exocrine: Makes digestive enzymes
Endocrine: Regulates blood glucose via islets of Langerhans
Insulin
secreted by beta cells
triggered by high blood glucose (after a meal)
promotes:
glucose uptake into cells (esp. muscle & fat)
glycogen synthesis (store glucose in liver/muscles)
fat synthesis
Glucagon
secreted by alpha cells
triggered by low blood glucose (fasting/in between meals)
promotes:
glycogen breakdown (glycogenolysis)
new glucose creation (gluconeogenesis)
fat breakdown (lipolysis)
Somatostatin (GHIH = Growth Hormone Inhibiting Hormone)
delta cells
triggered by high nutrient load (glucose, amino acids, fats are high)
acts like a brake:
inhibits both insulin & glucagon
also inhibits GH and TSH in the pituitary
Type 1 Diabetes
No insulin (autoimmune β-cell destruction)
Type 2 Diabetes
Desensitized insulin receptors (Insulin resistance)
Glucagonoma
Rare tumor → too much glucagon → hyperglycemia
Insulinoma
Tumor → too much insulin → hypoglycemia
Peptide Hormones
cleaved from larger polypeptides
Golgi modifies & activates hormone
does dissolve
put in vesicles and released via exocytosis
polar —> cannot pass through membrane, so uses extracellular receptor like GPCR
common secondary messengers: cAMP, Ca2+, IP3
Example: Insulin
Steroid Hormones
made in gonads & adrenal cortex, from cholesterol
doesn’t dissolve, must be carried by proteins
non polar —> can pass through cell membrane
activate nuclear receptors (in nucleus)
direct action on DNA
Example: Estrogen, Testosterone, Cortisol
Amino-Acid Derivative Hormones
share traits from both peptide and steroid hormones
Example: Catecholamines use GPCR, Thyroxine binds intracellularly
G-Protein Coupled Receptor (GPCR)
Membrane-bound receptor that, when activated by a ligand (like a hormone or neurotransmitter), triggers a second messenger signaling cascade.
Location: Cell membrane
Ligand: Typically hydrophilic (peptides, neurotransmitters)
Action: FAST and transient
Ligand binds GPCR (extracellular side)
GPCR undergoes a conformational change
On the intracellular side, it interacts with a G-protein (α, β, γ subunits)
This causes GDP → GTP exchange on the α-subunit
α-GTP dissociates from βγ complex
α-GTP then activates or inhibits a target enzyme:
Gs unit —> activates adenylyl cyclase
Gi unit —> inhibits adenylyl cyclase
Gq unit —> activates phospholipase C
Gs Pathway
Ligand binds GPCR
Gs protein activated (GDP → GTP on α-subunit)
α subunit activates adenylyl cyclase
Adenylyl cyclase converts ATP → cAMP
cAMP activates Protein Kinase A (PKA)
PKA phosphorylates targets → ↑ metabolism, transcription, glycogen breakdown
Gs Pathway common ligands
↑ cAMP, activates PKA
Glucagon → raises blood glucose
Epinephrine (β1, β2) → fight-or-flight
TSH → thyroid hormone release
ACTH → cortisol release
LH / FSH → sex hormone release
ADH (V2) → water reabsorption in kidneys
Key theme: Metabolism, stress, water balance
Gi Pathway
Ligand binds GPCR
Gi protein activated (GDP → GTP on α-subunit)
α subunit inhibits adenylyl cyclase
↓ cAMP → PKA not activated
↓ phosphorylation → ↓ cellular activity
Gi Pathway common ligands
↓ cAMP, inhibits PKA
Somatostatin → inhibits GH, TSH
Dopamine (D2) → inhibits prolactin
Gq Pathway
Ligand binds GPCR
Gq protein activated (GDP → GTP on α-subunit)
α subunit activates phospholipase C (PLC)
PLC cleaves PIP₂ → IP₃ + DAG
IP₃ triggers Ca²⁺ release from ER
Ca²⁺ + DAG activate Protein Kinase C (PKC)
PKC & Ca²⁺ → ↑ secretion, contraction, gene activity
Gq Pathway common ligands
↑ IP₃, DAG, Ca²⁺, activates PKC
GnRH → triggers LH/FSH release
TRH → triggers TSH release
Oxytocin → uterine contractions
ADH (V1) → vasoconstriction
Epinephrine (α1) → blood vessel constriction
Key theme: Reproductive hormone signaling + smooth muscle contraction
Direct Hormones
act directly on tissue/organ (ex: insulin)
Tropic Hormones
require an intermediary, they only affect endocrine tissues (ex: GnRH and LH)
Gonads
testes and ovaries
hormones: testosterone, estrogen, progesterone
controlled by the hypothalamus-pituitary-gonadal (HPG) axis
HPG Axis
Hormonal Control
Hypothalamus releases GnRH
Anterior Pituitary releases FSH & LH
Gonads release:
Testosterone (testes)
Estrogen & Progesterone (ovaries)
Testosterone
Produced by Leydig cells in the testes
Stimulated by LH
Functions:
Male sexual development (internal + external genitalia)
Muscle mass, libido, sperm production
Voice deepening, body hair
Excess testosterone → negative feedback on GnRH, FSH, and LH
Estrogen
Made by ovarian follicles, corpus luteum, and placenta (if pregnant)
Stimulated by FSH
Functions:
Female secondary sex characteristics (breasts, fat distribution)
Endometrial proliferation
Feedback regulation of FSH/LH
In pregnancy: promotes uterine growth and blood flow
Progesterone
Made by corpus luteum and placenta
Stimulated by LH
Functions:
Maintains endometrium for implantation
Inhibits uterine contractions
Thickens cervical mucus
Drops before menstruation = period begins
Mnemonic: "Pro-gestation" — keeps the uterus ready for baby
Feedback Loops of the Gonads

Anabolic Steroids
→ excess testosterone → ↓ LH/FSH → testicular atrophy, infertility
Polycystic ovary syndrome (PCOS)
→ high androgens, irregular cycles
Birth control pills
= synthetic estrogen + progesterone → constant negative feedback → no LH surge = no ovulation
Pineal Gland
Location:
Deep in the brain, between the two hemispheres, near the thalamus
Part of the epithalamus
Primary Hormone —> Melatonin
Melatonin
Derived from tryptophan (an amino acid)
Secreted in response to darkness
Regulated by light exposure via signals from the retina → suprachiasmatic nucleus (SCN) of the hypothalamus
Melatonin Functions:
Regulates circadian rhythm (your biological sleep-wake cycle)
Promotes sleepiness
Inhibits wake-promoting signals
Plays a role in seasonal reproduction in animals
Regulation:
Darkness → ↑ melatonin release
Light → ↓ melatonin release
Light inhibits the SCN → stops pineal gland from releasing melatonin
TIPS:
Melatonin does NOT knock you out like a sedative. It just makes you feel drowsy and regulates your internal clock.
Jet lag, insomnia, blue light exposure at night = often tied to disrupted melatonin production
Remember, melatonin is a hormone, not a neurotransmitter.
Anterior Pituitary
Controlled by the hypothalamus via releasing hormones through the hypophyseal portal system
Secretes 7 peptide hormones
Mnemonic = FLAT PEG
Tropic hormones = act on other endocrine glands → FLAT
Direct hormones = act directly on tissues → PEG
FSH (Follicle-Stimulating Hormone)
Stimulated by: GnRH
Males: stimulates spermatogenesis in Sertoli cells
Females: stimulates growth of ovarian follicles
LH (Luteinizing Hormone)
Stimulated by: GnRH
Males: stimulates Leydig cells → testosterone
Females: triggers ovulation, forms corpus luteum
LH surge → causes ovulation (mid-cycle)
ACTH (Adrenocorticotropic Hormone)
Stimulated by: CRH
Stimulates adrenal cortex → produces glucocorticoids (esp. cortisol)
Part of the stress response axis (CRH → ACTH → cortisol)
TSH (Thyroid-Stimulating Hormone)
Stimulated by: TRH
Stimulates thyroid gland → releases T3 & T4
Feedback: ↑ T3/T4 → ↓ TRH and TSH
Prolactin
Inhibited by: dopamine (PIF)
Stimulates milk production in mammary glands
During pregnancy: estrogen ↑ prolactin, but inhibits milk release
After birth: ↓ estrogen → prolactin works, nursing maintains it
Prolactin is the only anterior pituitary hormone primarily under inhibition (by dopamine)
Endorphins
Natural painkillers
Released during stress, exercise, excitement
Same pathway affected by opioids (endorphin analogs)
GH (Growth Hormone)
Stimulated by: GHRH
Inhibited by: somatostatin (GHIH)
Promotes:
Bone & muscle growth
Lipolysis
↑ Blood glucose (anti-insulin effect)
Stimulates liver to release IGF-1 (insulin-like growth factor 1)
Pathologies:
Excess GH in childhood = gigantism
Excess GH in adulthood = acromegaly
GH deficiency = dwarfism
Thyroid Gland
The thyroid makes two major categories of hormones:
T3/T4 – regulate metabolism
Calcitonin – regulates calcium levels
T3 (triiodothyronine) & T4 (thyroxine)
Made by:
Follicular cells of the thyroid
Derived from tyrosine + iodine
Function:
↑ Basal Metabolic Rate (BMR)
↑ oxygen consumption
↑ protein and lipid turnover
↑ heat production
↑ heart rate and cardiac output
Important in growth and development (especially brain!)
Regulation:
TRH (hypothalamus) → TSH (anterior pituitary) → T3/T4 (thyroid)
Negative feedback: High T3/T4 suppress TRH + TSH
Tip:
T4 = more stable, but less active
T3 = shorter half-life, but more potent
Calcitonin
Made by:
Parafollicular (C) cells of the thyroid
Function:
↓ Blood calcium levels by:
↑ Ca²⁺ deposition in bone
↓ Ca²⁺ absorption in blood
↓ Ca²⁺ absorption in gut
↑ Ca²⁺ excretion from kidneys
Mnemonic: Calcitonin “tones” down calcium levels in the blood
Hyperthyroidism (e.g. Grave’s disease)
↑ T3/T4 → anxiety, heat intolerance, weight loss, tachycardia
Hypothyroidism (e.g. Hashimoto’s)
↓ T3/T4 → fatigue, cold intolerance, weight gain, bradycardia
Calcitonin-secreting tumor (medullary thyroid carcinoma)
High calcitonin → hypocalcemia
Parathyroid Glands
Tiny glands located on the posterior surface of the thyroid
Secrete Parathyroid Hormone (PTH) in response to low blood calcium
PTH (Parathyroid Hormone)
Low blood calcium (Ca²⁺) = trigger for ↑ PTH secretion
Goal: Raise blood calcium levels — the opposite of calcitonin
Mechanisms of Action:
↑ Ca²⁺ resorption from bone
Stimulates osteoclast activity → breaks down bone → releases Ca²⁺ into blood
↑ Ca²⁺ reabsorption in kidneys
Less calcium is excreted in urine
↓ Phosphate reabsorption in kidneys
Prevents calcium from binding phosphate → keeps free Ca²⁺ in blood
Result: ↑ phosphate in urine
↑ Activation of vitamin D (calcitriol) in kidneys
PTH stimulates 1-α-hydroxylase → converts vitamin D → calcitriol
↑ Ca²⁺ absorption in intestines
This is indirect, via calcitriol (vitamin D)
Hypoparathyroidism
↓ Ca²⁺ → muscle cramps, tetany, seizures
Hyperparathyroidism
↑ Ca²⁺ → kidney stones, bone loss ("stones, bones, groans, and psychiatric overtones")
Chronic kidney disease
↓ vitamin D activation → ↑ PTH → secondary hyperparathyroidism
Posterior Pituitary (Neurohypophysis)
Does not make its own hormones.
Hormones are made in the hypothalamus, then stored & released by the posterior pituitary.
ADH (Antidiuretic Hormone) aka Vasopressin
Target: Kidneys (V2 receptors) & blood vessels (V1 receptors)
Retains water in the kidneys (collecting ducts)
Concentrates urine
Raises blood pressure by increasing blood volume and causing vasoconstriction
Functions:
↓ water loss in urine (by ↑ water reabsorption in collecting ducts via aquaporins)
↑ blood pressure (via vasoconstriction)
Triggered by:
↑ blood osmolarity (dehydration)
↓ blood volume/pressure
Inhibited by:
Alcohol
Low osmolarity
Oxytocin
Targets: Uterus, mammary glands, and brain
Functions:
Uterine contractions during labor
Milk ejection (not production — that’s prolactin)
Bonding and trust (mother–infant, romantic partners)
Regulation:
Positive feedback loop!
(e.g., uterine stretch → ↑ oxytocin → more contractions → more stretch…)
A patient has high plasma osmolarity and concentrated urine, this means…
ADH is likely ↑
During labor, contractions get more intense and frequent, why?
oxytocin is in a positive feedback loop
A mutation in V2 receptors leads to…
nephrogenic diabetes insipidus (ADH made but doesn't work)
Too little ADH
Diabetes Insipidus (DI)
Both types = high serum osmolarity, low urine osmolarity, increased thirst
Central DI
No ADH production (hypothalamus/post. pituitary damage)
Kidneys don’t reabsorb water → polyuria, dehydration
Nephrogenic DI
ADH is made, but kidneys don’t respond (V2 receptor mutation)
Same symptoms: dilute urine, dehydration
Too much ADH
SIADH (Syndrome of Inappropriate ADH Secretion)
Excess ADH release (often from tumors or brain injury)
Too much water reabsorbed → hyponatremia (diluted blood sodium), low urine volume, confusion/seizures
Adrenal Cortex
Makes steroid hormones (cholesterol-derived)
Split into 3 zones — each has its own hormone category
Zona Glomerulosa
→ Mineralocorticoids
Main hormone: Aldosterone
Function:
↑ Na⁺ reabsorption
↓ K⁺ reabsorption (↑ K⁺ excretion)
Water follows Na⁺ → ↑ blood volume & pressure
Triggered by:
Low blood pressure
Low Na⁺, high K⁺
Angiotensin II (RAAS system — not ACTH!)
Zona Fasciculata
→ Glucocorticoids
Main hormone: Cortisol (also cortisone)
Function:
↑ blood glucose (via gluconeogenesis)
↓ protein synthesis (muscle breakdown for fuel)
↓ immune system (anti-inflammatory)
Helps body manage chronic stress
Triggered by:
ACTH (from anterior pituitary)
CRH → ACTH → Cortisol
Negative Feedback:
Cortisol feeds back to inhibit CRH and ACTH
Zona Reticularis
→ Androgens
Main product: Weak androgens (e.g., DHEA → testosterone/estrogen)
Function:
In males: minimal effect (testes take over)
In females: contributes to pubic/axillary hair, libido
Triggered by:
ACTH (minor role)
No direct feedback loop like cortisol or aldosterone
"Salt, Sugar, Sex"
From outer to inner cortex: G —> F —> R
Glomerulosa = Mineralocorticoids → Aldosterone = Salt
Fasciculata = Glucocorticoids → Cortisol = Sugar
Reticularis = Androgens → Testosterone = Sex
Cushing Syndrome
Too much cortisol (glucocorticoids)
Symptoms:
Moon face, buffalo hump, central obesity
Muscle wasting
Striae (purple stretch marks)
Hypertension
Hyperglycemia
Immune suppression
Osteoporosis
MCAT focus:
High cortisol = ↓ ACTH (if cause is adrenal tumor or steroids)
Cushing disease = pituitary tumor → ↑ ACTH
Always think: cortisol excess → catabolism + high glucose + immune suppression
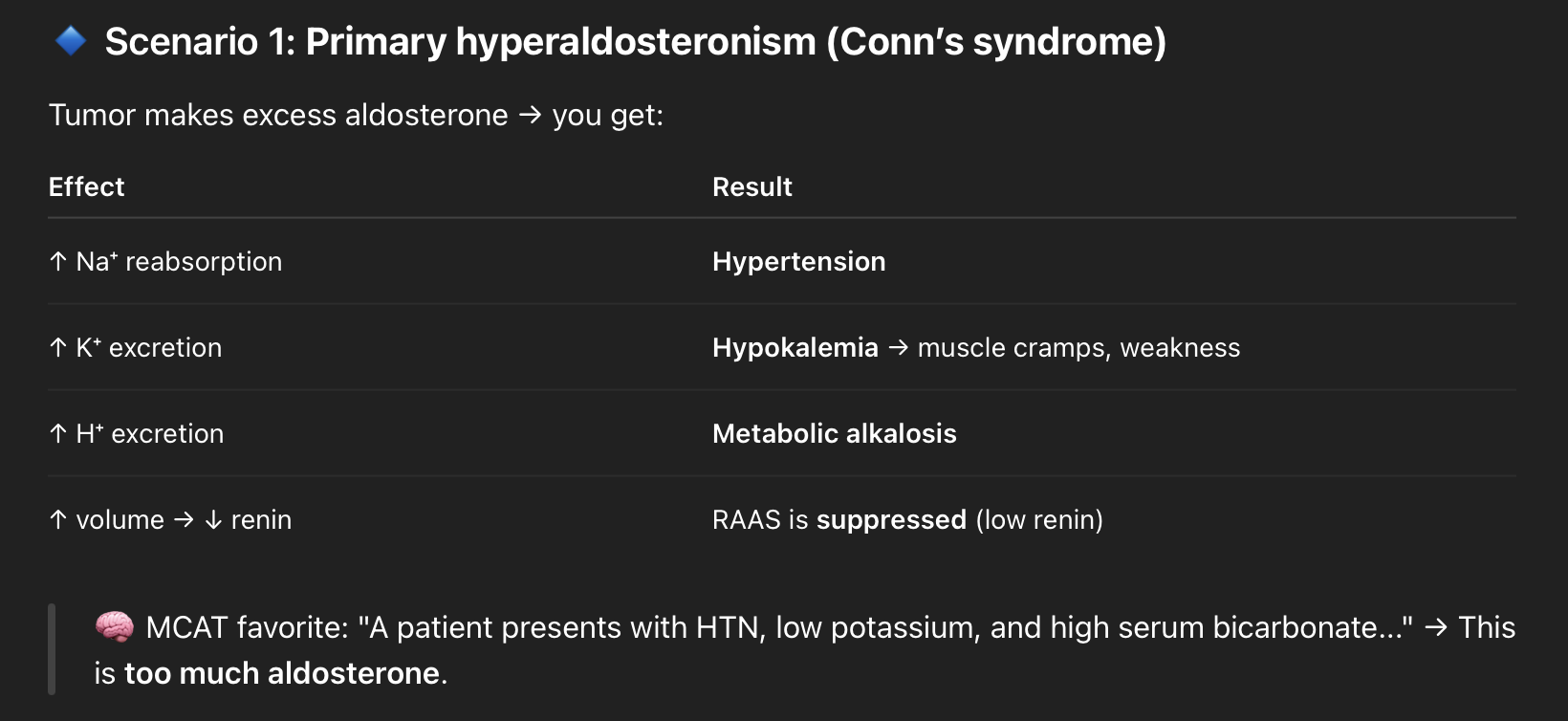
Addison’s Disease
Adrenal insufficiency (↓ cortisol & ↓ aldosterone)
Symptoms:
Fatigue, weight loss
Hypotension
Hyperpigmentation (↑ ACTH → ↑ MSH)
Hyponatremia, hyperkalemia (due to ↓ aldosterone)
Craving salt
MCAT focus:
Primary adrenal insufficiency = problem in the adrenal cortex → ↓ cortisol + ↓ aldosterone
→ Feedback: ↑ ACTH
Common cause = autoimmune destruction of adrenal cortex
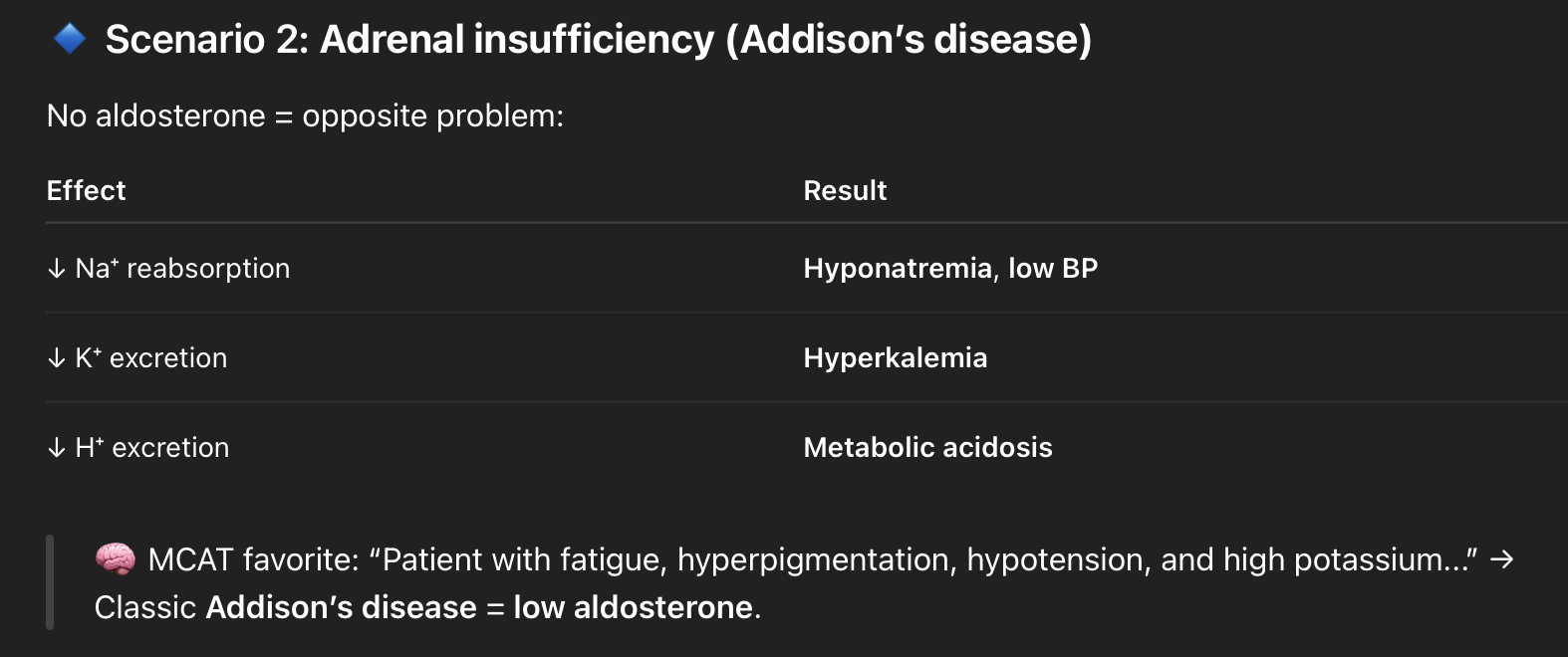
Hyperaldosteronism (Conn's Syndrome)
Symptoms:
Hypertension
Hypokalemia
Metabolic alkalosis
MCAT focus:
Excess aldosterone = ↑ Na⁺ reabsorption, ↓ K⁺
Volume overload → high BP
Potassium wasting → muscle cramps/weakness
Congenital Adrenal Hyperplasia (CAH)
most commonly 21-hydroxylase deficiency
Symptoms (varies by severity/sex):
Low cortisol
Low aldosterone
↑↑ androgens
Females: ambiguous genitalia at birth
Salt-wasting crisis (if severe aldosterone loss)
MCAT focus:
Enzyme block → ↓ cortisol → ↑ ACTH → adrenal hyperplasia + excess androgen production
↑ 17-hydroxyprogesterone (classic diagnostic marker)
Aldosterone
Released by the zona glomerulosa in response to:
↓ Blood pressure (via RAAS)
↓ Na⁺ levels
↑ K⁺ levels
In the distal tubule and collecting duct of the nephron:
↑ Na⁺ reabsorption → water follows → ↑ blood volume + BP
↑ K⁺ excretion → ↓ serum K⁺
↑ H⁺ excretion → can cause metabolic alkalosis
Scenario 3: Dehydration or blood loss
What hormone is primarily responsible for sodium reabsorption here?
Answer: Aldosterone, not ADH
↓ blood volume → triggers RAAS → ↑ aldosterone
Body compensates by reabsorbing Na⁺ + water to restore BP
Key MCAT Clues Aldosterone Is Involved
Hypertension + low K⁺ = think ↑ aldosterone
Hypotension + high K⁺ = think ↓ aldosterone
Na⁺ and water move together, K⁺ goes opposite
No change in glucose (that’s cortisol’s lane)
Adrenal Medulla
Location: the inner part of the adrenal gland (surrounded by the cortex)
Function:
Releases catecholamines:
Epinephrine (adrenaline)
Norepinephrine (noradrenaline)
These are tyrosine-derived amino acid hormones, and they act FAST via GPCRs
Triggers:
Sympathetic nervous system activation (via preganglionic acetylcholine release)
Emotional or physical stress
Low blood sugar, exercise, trauma
Adrenal Medulla: Epinephrine
Main hormone secreted by adrenal medulla (about 80%)
Acts on β1, β2, α1 receptors
Effects:
↑ Heart rate (β1)
↑ BP (vasoconstriction via α1 + vasodilation via β2 in skeletal muscle)
↑ Bronchodilation (β2)
↓ Histamine release (anti-allergy effect)
↑ Glucose (via glycogenolysis & gluconeogenesis)
*associate epinephrine with stress, asthma treatment, and metabolic boosts
Adrenal Medulla: Norepinephrine
Mainly acts on α1 and β1 receptors
Effects:
↑ Vasoconstriction (↑ BP) via α1
↑ Heart rate via β1
Less effect on bronchodilation than epinephrine
*NE in questions about vasoconstriction and blood pressure maintenance
Pheochromocytoma
Tumor of the adrenal medulla → excess catecholamines
Classic symptoms:
Episodic hypertension
Sweating
Tachycardia
Palpitations
Anxiety, panic attacks
Diagnosed by: ↑ metanephrines / catecholamine breakdown products
Catecholamines
amino acid–derived, but act like peptide hormones — bind surface receptors (GPCRs) and act fast