MICR130 Immunology part 2 (applications + disorders) - Quiz 12/13
1/20
Earn XP
Description and Tags
Tests, adaptive immunity
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
ELISA
Enzyme Linked Immunosorbent Assay
Introduces an enzyme’s substrate (eg. detecting presence of enzyme urease / production of ammonia to test for H. pylori activity)
Anti-human antibody linked to enzyme (eg urease) introduced. Add substrate (urea) and pH indicator. Reaction will take place only if human anti-virus-antibody is present
eg. take-home pregnancy tests
Direct ELISA: detects antigen, antibody is added + patient sample with antigen added
Indirect ELISA: detects antibodies, antigen is in well + patient serum added
Fluorescent Microscopy (Fluorescent-Antibody Techniques / FA)
Identifying microbes / antibodies with fluorescent dye FTIC / TRITC
Antigens react with antibody and glow under microscope
Fluorescence Activated Cell Sorter (Fluorescent-Antibody Techniques / FA)
Fluorescent cytometry
Instrument with laser counts and separates fluorescent stained cells
eg. Can be used to count number of CD4 (helper T cells) and CD8 cells in a sample to test for the progression of AIDS for less CD4 cells
Agglutination
Detects particulate antigens (particles/cells carrying antigenic molecules) or soluble antigens adhering to particles
Antigens will link together to form visible aggregates (clumped together masses)
Direct vs Indirect agglutination
Direct: Detects antibodies against regularly large cellular antigens and clumping of these cells naturally eg. red blood cells, bacteria, fungi
Indirect / Latex agglutination: Antigen (or antibody) is attached to larger particles to improve visualization, and observing the aggregation of those, such as latex beads.
Common testing for strep
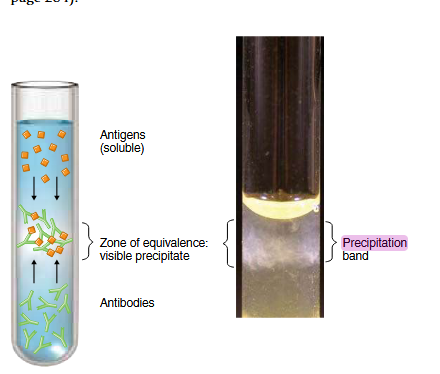
Precipitation
Detects soluble antigens with IgG or IgM antibody
Antigens and antibodies bind, creating antigen-antibody complexes that form large, insoluble lattices
Area of equivalence
Precipitation tests require an optimal ratio of antigen to antibody
Antigen/antibody placed adjacent to each other, and a cloudy line of precipitation forms in the area with the optimal ratio
Clonal Selection Hypothesis
Stem cells differentiate into B cells and are already present in body since birth
B cell encounters an antigen without T cells, producing a weak immune response (IgM / first response)
Some B cells proliferate to become memory cells, some proliferate into plasma cells (type of specialized B cell proliferates when it encounters an antigen / is selected)
B cells that proliferate into memory cells can be stimulated to become plasma cells that produce antibodies against the antigen it encountered. Same cell might class switch (produce a different antibody than IgM— eg. IgG or IgE)
Plasma cells secrete antibodies into circulation
First vs Secondary Response
First response:
IgM
Naive cells
Takes place first, weaker, less antibody
Secondary response:
Intensified immune response after first due to memory cells
Less IgM, class switching, more antibody made
(vaccination/artificially acquired immunity can be explained by this response)
HCG (hormone that produces placenta) latex inhibition agglutination test
Add urine + antibody reagent, allowing antigen + antibodies to bind
Add HCG latex beads
If HCG is present, will already be bound to the antibodies and thus antibodies will not bind to the latex particles
Inhibition (no clumping): positive / pregnant
Clumping: negative
Reagent antibodies
Specific, sensitive reagents made in animals that bind to specific molecules
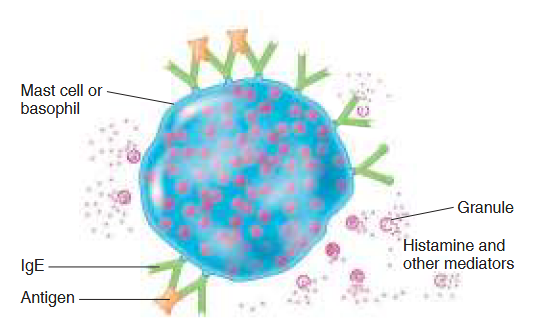
Type I hypersensitivity
What is it/what is involved, examples?
Anaphylactic
Fast acting <30 min
Reaction from IgE on basophils/mast cells binding with antigens
Antigen bridges gap between two antibodies, causing degradation (cell releases its granules + contents, including histamine)
Eg. common allergic reactions (mucousal secretions, itchy eyes), shock in systemic rx
Type II hypersensitivity
What is it/what is involved, examples?
Cytotoxic
IgG/IgM reacts with antigen to activate complement, then lyses cells
Antigens located on cell or tissue surfaces
Eg. blood transfusion reactions, erythroblastis fetalis/HDNB (hemolytic disease of newborn)
Type III hypersensitivity
What is it/what is involved, examples?
Immune complex reactions
IgG/IgM reacts with soluble antigens in serum to form an antibody-antigen complex that is deposited in tissues. Complement is activated, causing inflammatory damage
Complex circulates blood then becomes trapped in basement membrane endothelial cells. Immune complex activates complement and endothelial cells/membrane is damaged by enzymes from neutrophils
Eg. serum sickness, autoimmune conditions such as Rheumatoid arthritis, Post-Strep glomerulonephritis, Grave’s disease, Lupus, Arthus reaction (side effect of toxoid vaccines)
Type IV hypersensitivity
What is it/what is involved, examples?
Delayed cell-mediated reaction
Delayed (24-28 hours) cell-mediated (involves CD4 T cells)
Macrophage antigen presentation → T cells become memory cells then proliferate (no dermatitis during sensitization)
Dermatitis occurs upon secondary contact as memory cells release cytokines + cause inflammation
Eg. contact dermatitis (poison ivy, mango rash), PPD (purified protein derivative of tuberculosis) test
Erythroblastis fetalis and how to treat it?
Rh- mother carries Rh+ fetus then becomes immunized during her first pregnancy
During 2nd pregnancy with Rh+ fetus, mother produces antibodies that damage fetal RBCs causing jaundice and anemia
Preventable with RhoGAM: anti-Rh antibodies (blocking antibodies) to combine with the fetal Rh+ instead of her immune system to prevent mother from being immunized during 1st pregnancy
Fc region of IgE
IgE binds to mast cells via the Fc region
Mast cells have Fc-IgE receptors
Hyposensitization therapy
Desensitization therapy
Used to treat type I hypersensitivity
Patient is repeatedly immunized with small doses of allergen to try to force the immune system to synthesize IgG instead of IgE
If successful, IgG binds to allergen before IgE, thus blocking the allergic response
Blocking antibody
An antibody that binds to a specific target to prevent other molecules from binding to it
eg. IgG in hyposensitization therapy, RhoGAM
Natural antibodies
Antibodies that exist in our plasma without prior immunization
In ABO group system, individuals possess antibodies to antigens they don’t possess
Immune complexes
Soluble, circulating antigen-antibody aggregate that can fix to complement
Form under certain ratios of antigen and antibody
Type III hypersensitivities (Grave’s disease, lupus, rheumatoid arthritis, serum sickness)