Spinal Cord Injury
1/184
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
185 Terms
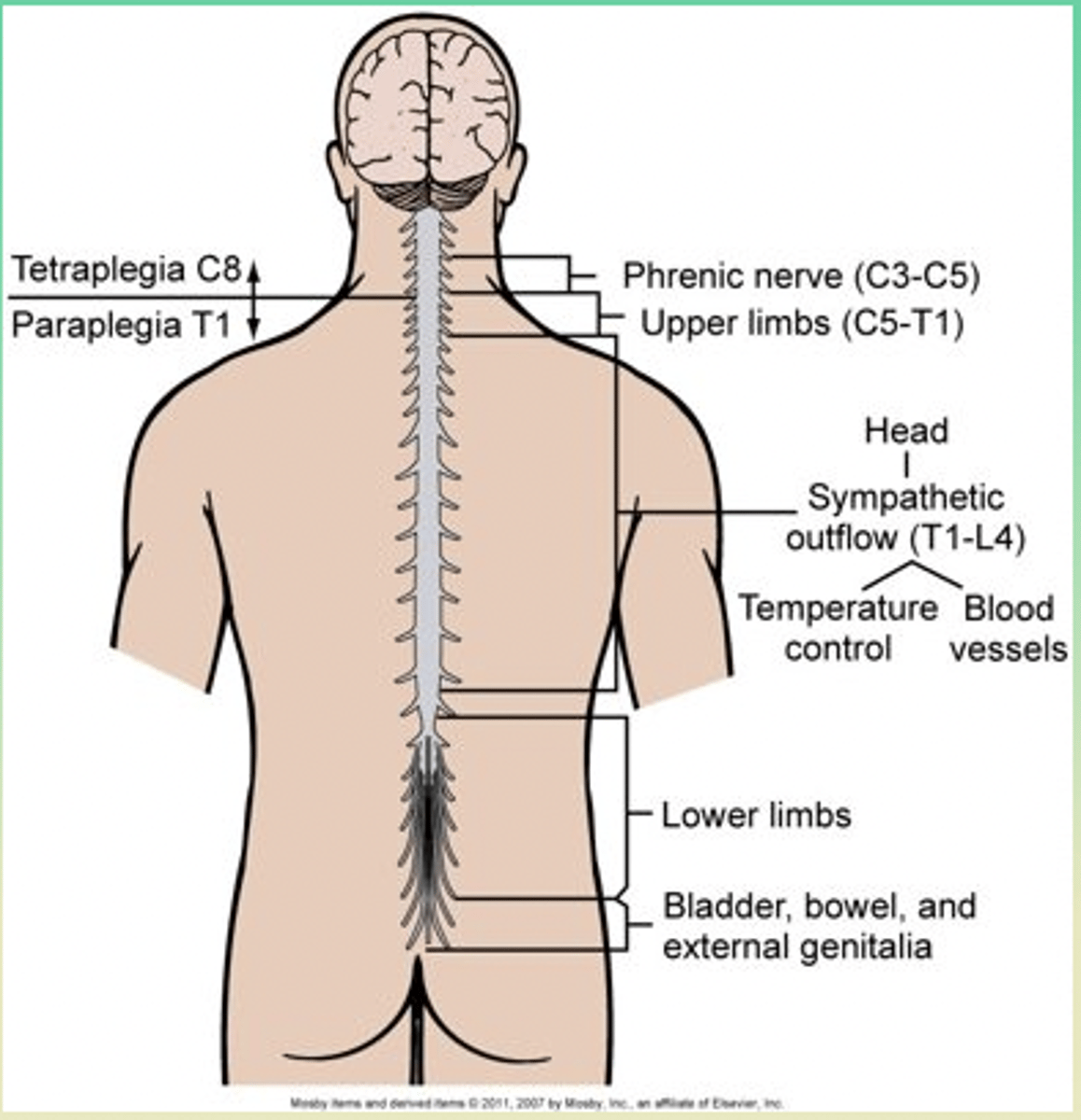
spinal cord
- major part of the CNS
- from the brainstem to lower back; ends at L2
- protected by vertebrae
-segmental spinal nerves --> sensory + motor function
spinal nerves
- spinal cord segments contain cell bodies & sensory + motor nerve fibers (______ _____)
- innervate specific region of neck, trunk, or limbs
(ie. c3-c5 segment contains phrenic nerve)
- part of PNS; enables connections between CNS (spinal cord segment) + PNS (____ ____ )
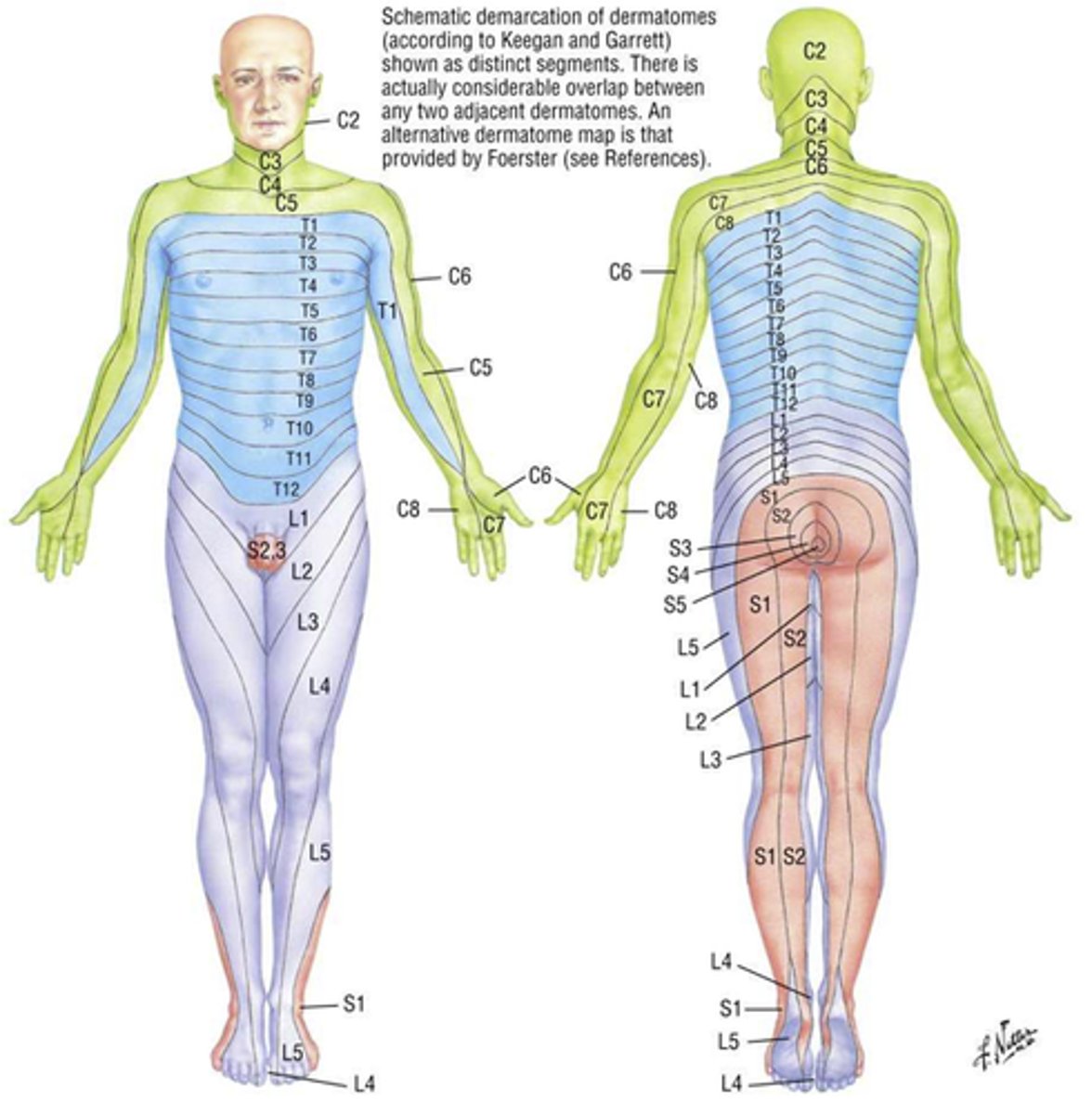
dermatome
- area of skin innervated by the sensory fibres of a spinal nerve (PNS)
- indicate the general pattern of somatic sensory innervation by spinal segments
myotome
- a muscle group innervated by the primary motor neurons of a spinal nerve (PNS)
Peripheral Nervous System
- Cranial nerves
- Spinal nerves
- Autonomic Nervous System
ANS
- involuntary functions of cv, smooth/involuntary muscle, glands
- PNS
- SNS
PNS
ANS:
- “Rest + digest” response
- Main NT → Acetylcholine
- cell bodies located in brainstem + S2-S4
- SCI does not alter function (unless brain injury + extension of cervical injury) = functioning PNS
SNS
ANS:
- “Fight or Flight” response
- Main NT → NE
- Cell bodies located from T1-L2
- dysfunction in cervical/thoracic injuries
SNS, PNS
- If ______ dysfunction (cervical/thoracic) = ++++ _______ stim w/o compensation
- manifested in sx + complications
PNS stim
- Pupil constriction
- Bradycardia + vasodilation
- Bronchoconstriction
- Increases GI motility + relaxation of GI sphincter → - stimulates elimination
- Increases gastric secretions → Saliva + HCL production
- Bladder contraction + relaxation of urinary sphincter → stimulates urination
SNS
- Pupil dilation
- Tachycardia + vasoconstriction
- Bronchodilation
- Decreases GI motility + contracts GI sphincter
- Decreases gastric secretions → Saliva + HCL production
- Bladder relaxation + contraction of urinary sphincter
spinal cord injuries (SCI)
- have a devastating effect on health and well-being
- many injured pt remain independent
- 60-70 yrs age, male 2:1 female
- highest level of injury may require full care
- divided into traumatic and non-traumatic categories
traumatic, non-traumatic
spinal cord injuries:
- _______ result of external physical impact
- _______ result of disease, infection, or tumour
Traumatic SCI
- younger; 20–30 yrs
- male 4:1 female
- cervical spine most common
- 50% r/t vehicle collisions; 30-40% falls or work r/t
initial injury (SCI)
Mechanisms:
- Cord Compression
- Penetrating Trauma
cord compression
Initial injury by _______ _______ from:
- Bone displacement (ie. blunt trauma)
- Tumor
- Abscess
- Interruption of blood supply
penetrating trauma
Initial SCI by: ________ _______
- gunshot wound
- stab wound
...
- cord wrapped in tough layers of dura; rarely torn or transected by direct trauma
- penetrating trauma = tearing and transection
primary injury
SCI
- initial mechanical injury w/ failure of spinal column (fracture or dislocation)
- imparts force to spinal cord, disrupts axons, blood vessels, and cell membranes
- initial disruption of axons as a result of stretch or laceration
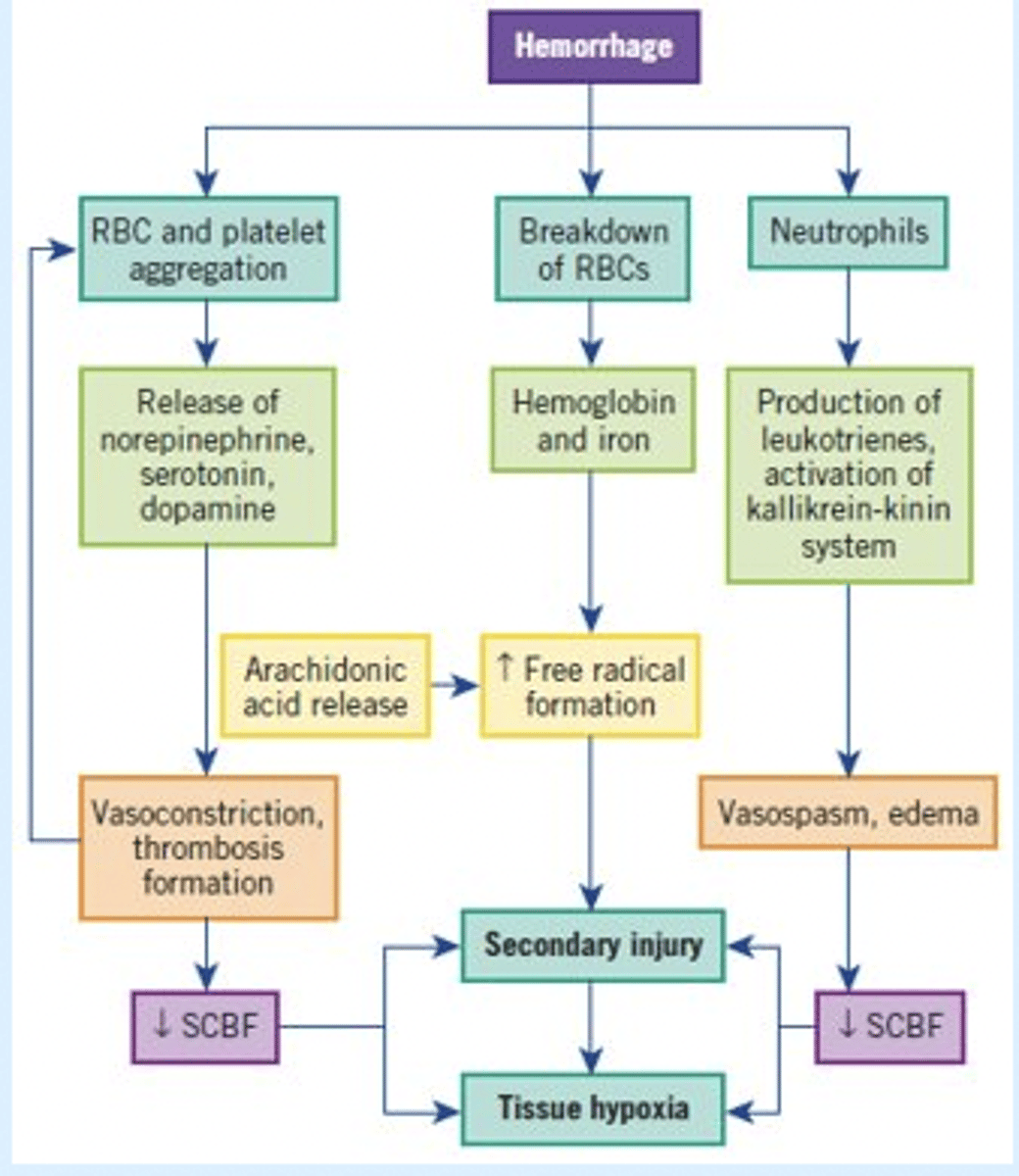
secondary injury
- Ongoing, progressive damage; occurs after initial injury
- involves vascular dysfunction, edema, ischemia, lyte shifts, inflammation, free radical accumulation + apoptotsis
secondary injury
- cell death (apoptosis) occurs + may continue for weeks-months after initial injury
- may result in permanent cord damage >24HR d/t autodestruction
petechial hemorrhage, cord ischemia
Secondary Injury: Autodestruction
- ________ _______ --> vascular disruption + hemorrhage in surrounding matter = ______ ______
- cord ischemia -> _______ (within 24 hrs) develops & extends above/below SCI = permanent cord damage
hypoxia, lactate metabolites, vasoactive substances
Secondary Injury: Autodestruction
- d/t edema + cord ischemia ________ results --> release of lactate metabolites + vasoactive substances
- _______ _____ byproduct of anaerobic metabolism --> acidosis + increases O2 demand
- ________ _______ (NE, serotonin, dopamin) --> vasopasms + further hypoxia = necrosis (limited ability to adapt to vasospasm)
....
Events Leading to Spinal Cord Ischemia and Hypoxia of Second Injury
extent of neuro damage
______ of _______ ________ from SCI is r/t:
- primary injury damage
- secondary injury damage
primary injury damage
Extent of neuro damage from SCI is r/t:
- Actual physical disruption of axons
secondary damage
Extent of neuro damage from SCI is r/t:
- r/t cord ischemia, hypoxia, microhemorrhage, edema
- can cause extension of SCI + permanent damage (<24HR)
- prognosis determined at 72HR or longer d/t process of _____ ____ occurring overtime
minimize/manage secondary injury
- Rapid Assessment, Intervention, Immobilization
- first 8 hrs after injury
- limit further destruction
Classified
SCI _______ by:
- Mechanism of Injury
- Skeletal level of injury
- Neurologic level of injury
- Completeness or degree of injury
mechanism of injury
- understanding ________ _ _________ is important +++
- why + how injury occured --> factors contributing to injury + mediate factors for further prevention
- also dictates sx + further investigations + goals of care + progression of injury + risk of complications + management
mechanisms of injury
Major __________ __ _______:
- flexion.
- hyperextension.
- flexion–rotation.
- extension–rotation.
- compression.
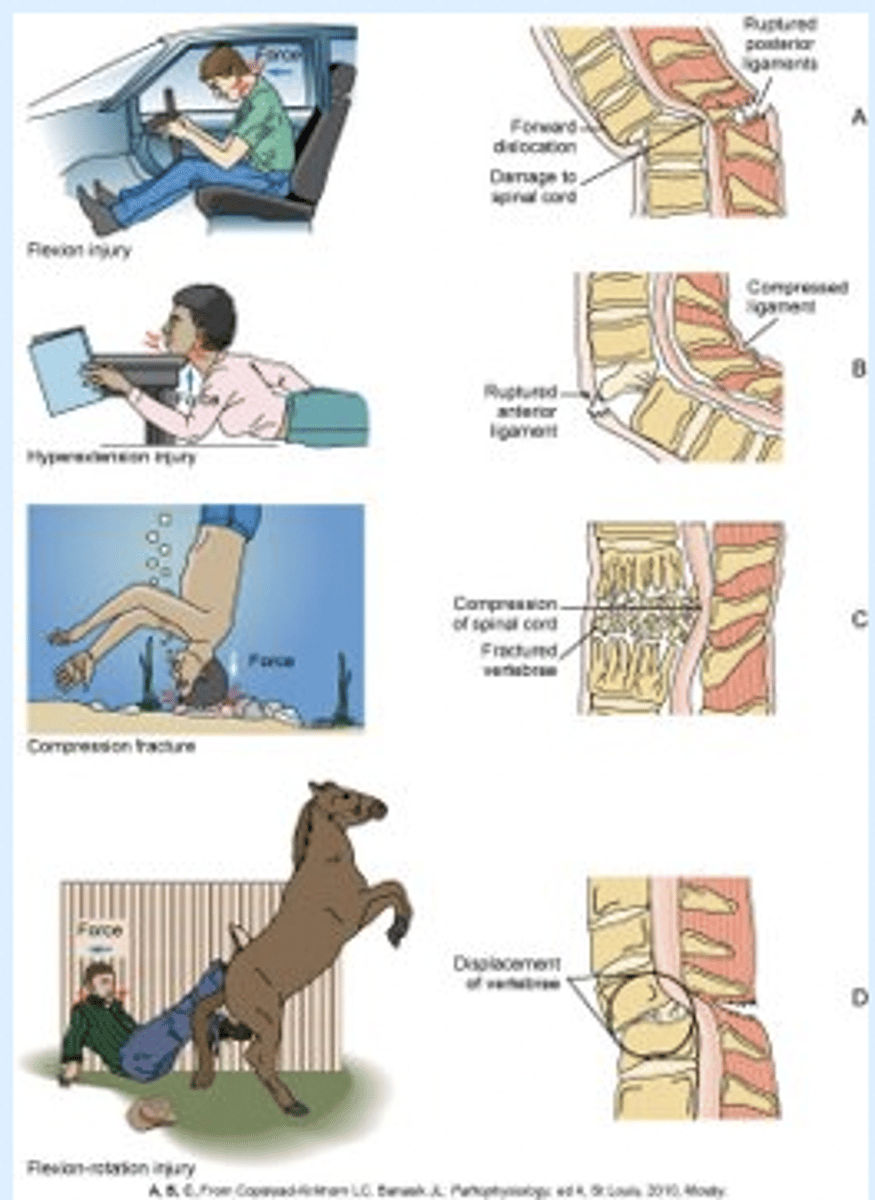
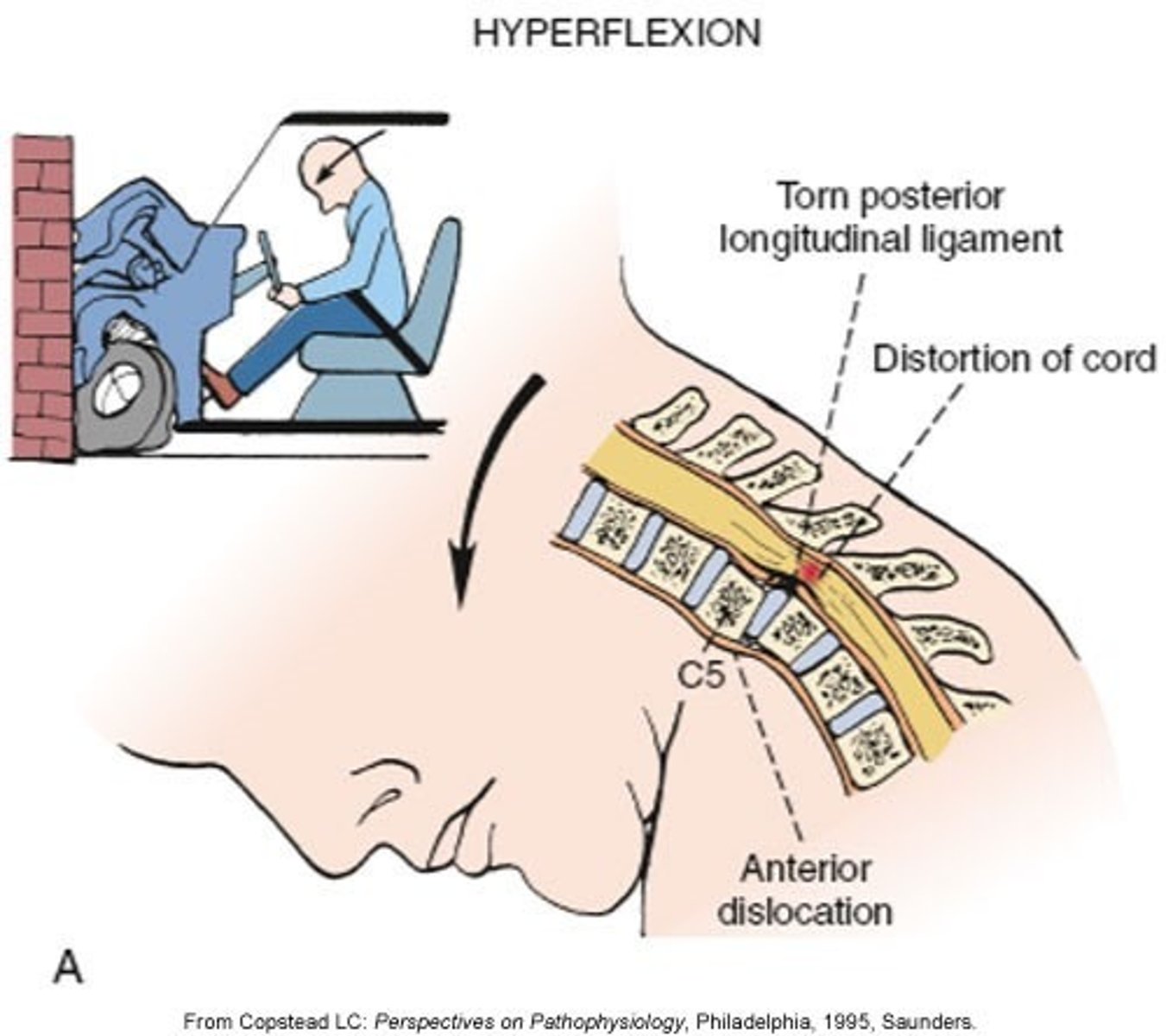
flexion injury
Major Mechanisms of SCI:
- _____ _______ of the cervical spine ruptures the posterior ligaments
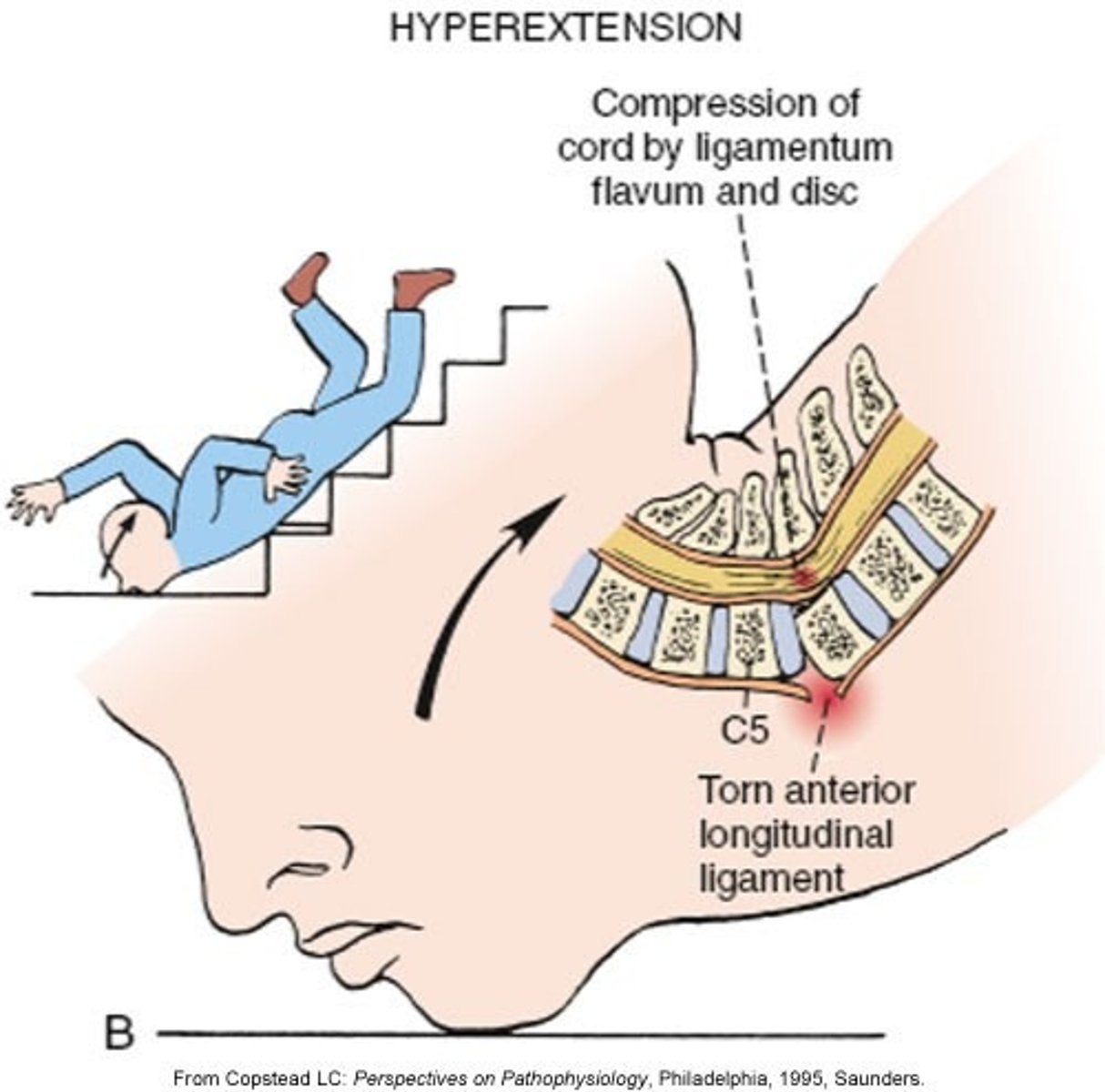
Hyperextension injury
Major Mechanisms of SCI:
- _________ _________ of the cervical spine ruptures the anterior ligaments
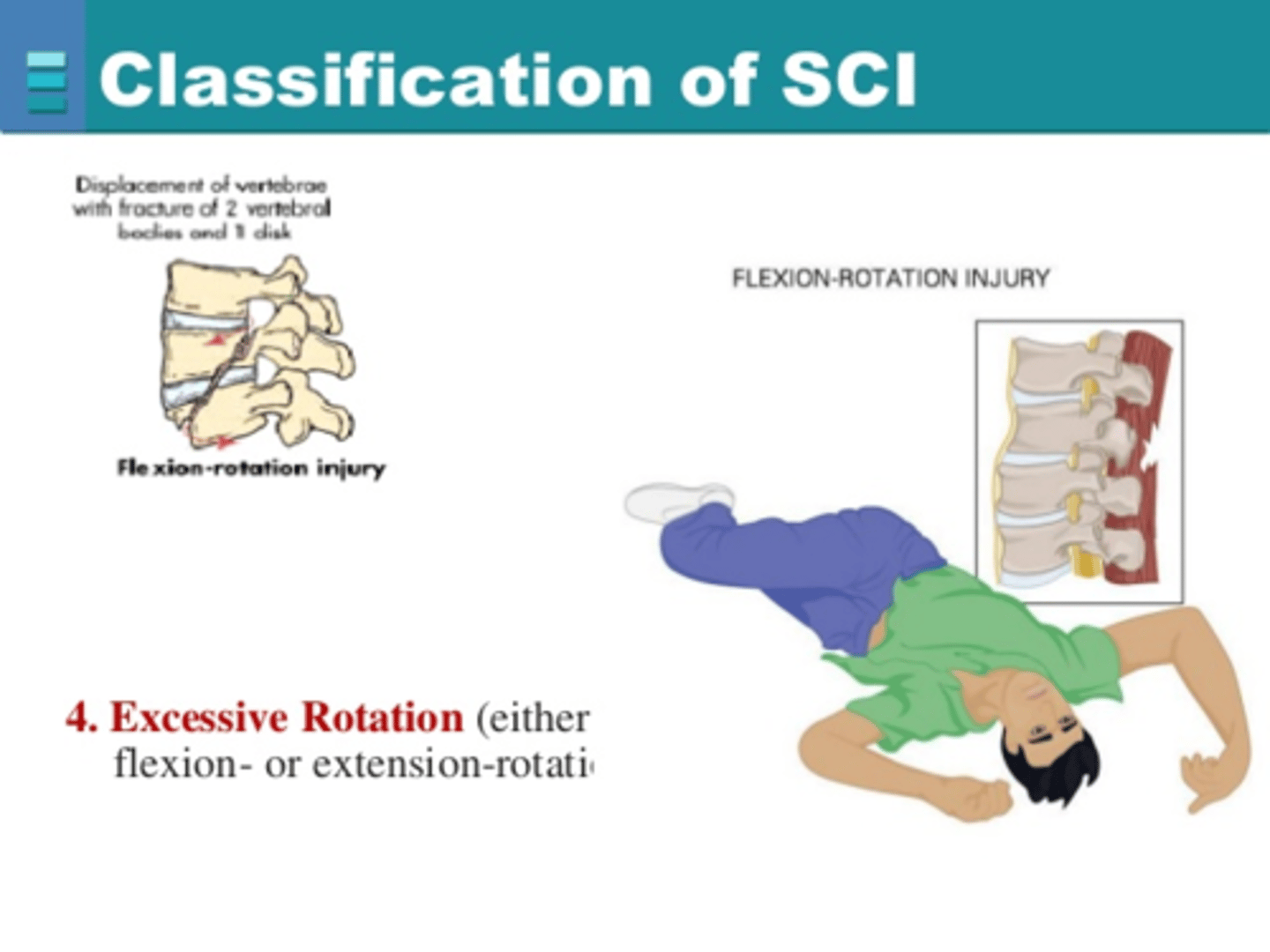
flexion-rotation injury
Major Mechanisms of SCI:
- most unstable of all injuries
- ligamentous structures that stabilize spine are torn
- injury most often implicated in severe neuro deficits
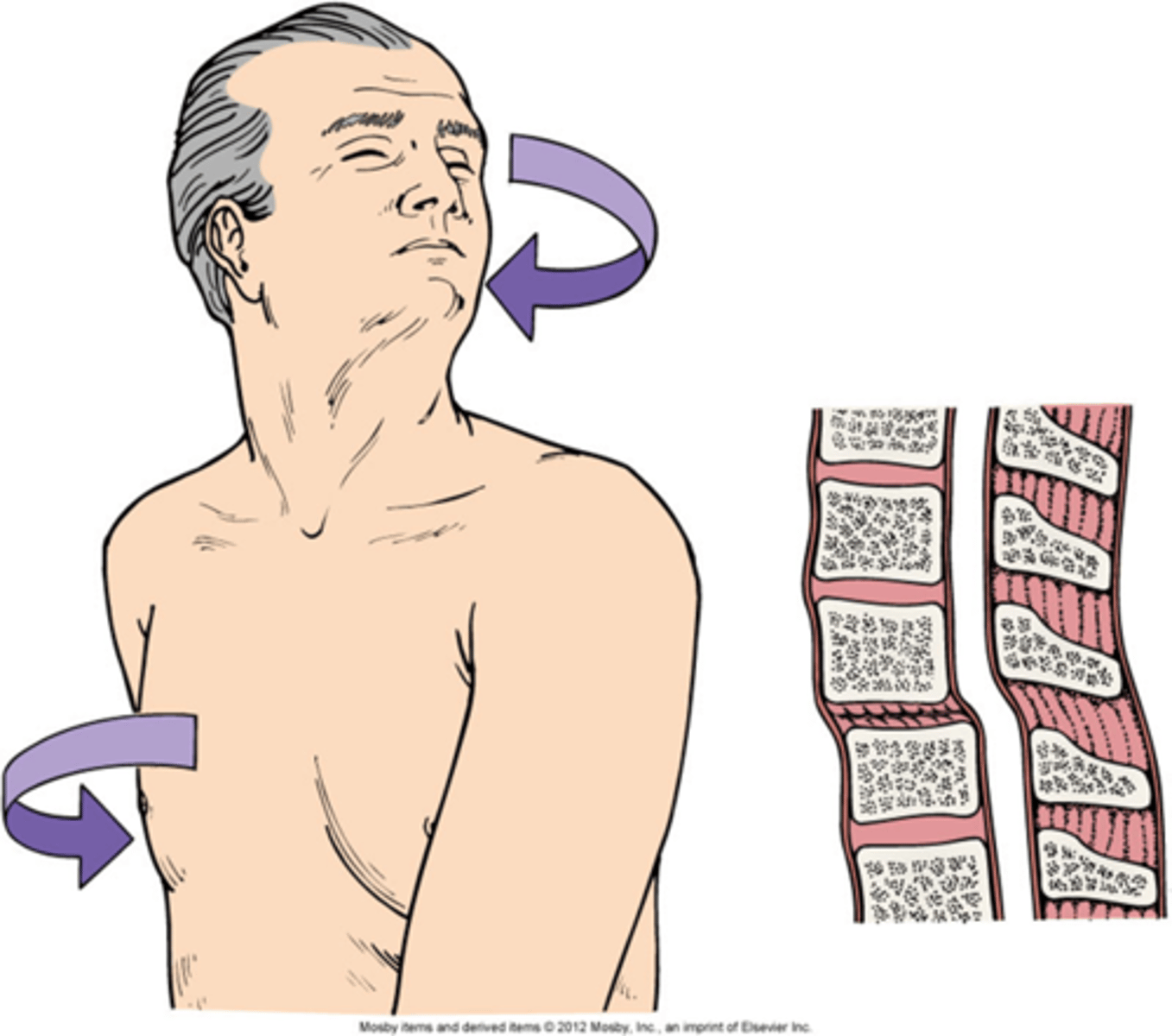
extension rotation injury
- The spine is bent backward + rotated/twisted beyond normal ROM
- ligamentous structures that stabilize spine are torn
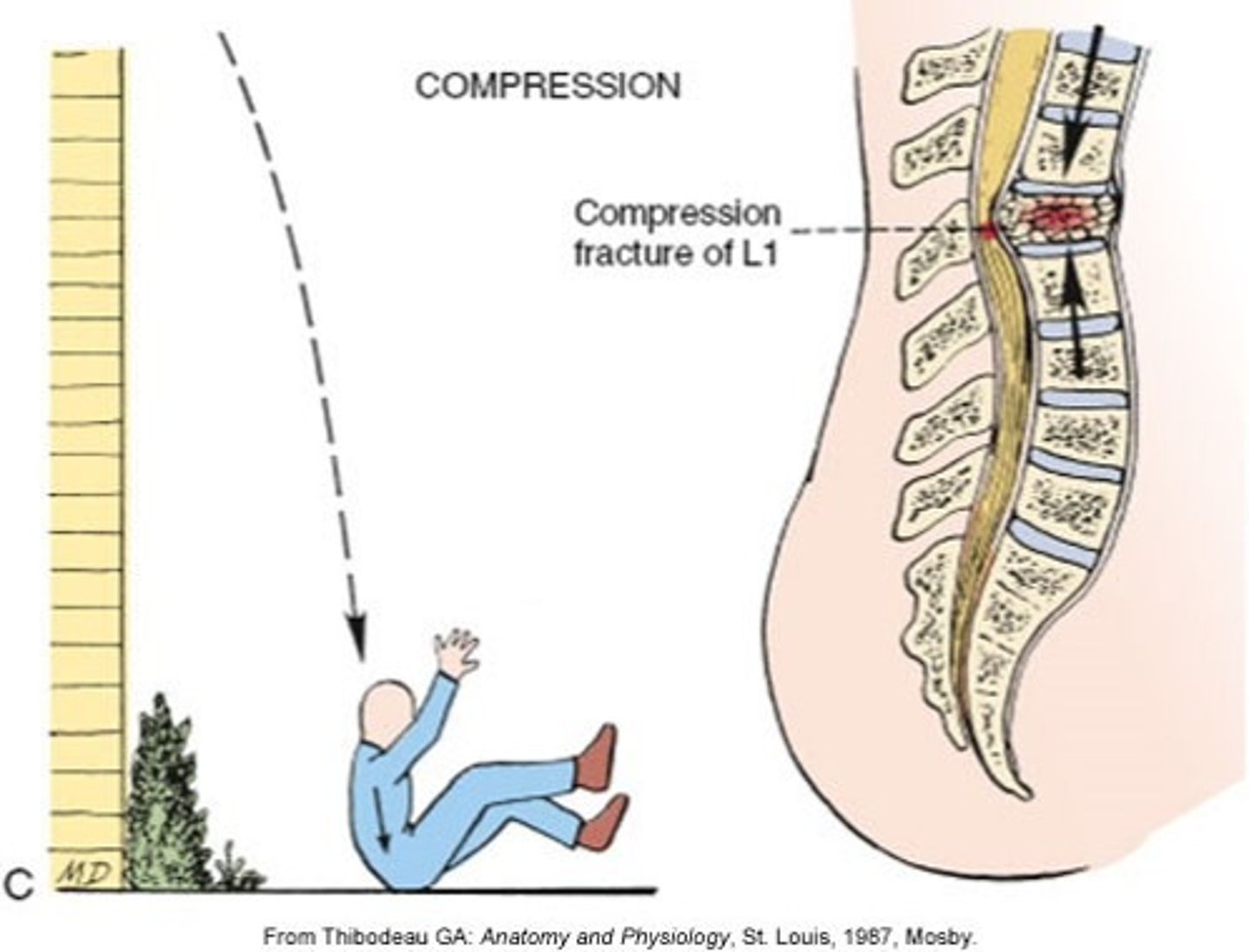
compression injury
Major Mechanisms of SCI:
- crush the vertebrae and force bony fragments into the spinal canal
level of injury
May be:
- cervical (C1-C8)
- thoracic (T1-T12)
- lumbar (L1-L2)
Skeletal level
Level of injury
- Injury at vertebral level
- where there is most damage to vertebral bones and ligaments
neurological level
SCI classifications: Level of injury
- the lowest segment of spinal cord with normal sensory and motor function bilaterally
cervical, tetraplegia, quadriplegia
- occurs if the _______ cord is involved
- Paralysis of all four extremities (_______ or ________)
C3-C5 injuries
- impact phrenic nerve
- can result in phrenic nerve damage = diaphargm paralysis
- major impact on breathing
- may need mechanical ventilation, relearn how to breath
C5-t1 injuries
- damage brachial plexus (shoulder, arm, and hand nerves)
- result in paralysis of upper limbs
medulla
consider proximity of cervical spinal cord to _________
- vital centres that control Ventilation, HR, Vasomotor function
thoracic/lumbar, paraplegia
- results if _______/______ cord is damaged.
- paralysis of lower limbs (below T1)
T1 to L4 injuries, T5
- Loss SNS innervation
- Loss Temp control (poikilothermia)
- Loss of Vasomotor tone
risk of neurogenic shock above _______
T12
- paralysis of intercostal + abdominal muscles
- affect bowel, bladder, and trunk control
...
- sx depend on the degree of paralysis
- potential for rehab depends on the level of injury
spinal cord involvement
Degree of _______ _____ ______ may be:
- complete or incomplete
complete
Degree of spinal cord involvement:
- Results in total loss of sensory and motor function below level of lesion (injury)
- transection of spinal cord + absolute paralysis below injury
- 6 types
complete
SCI w/ ________ involvement:
- central cord syndrome
- anterior chord scent syndrome
- brown saccard syndrome
- posterior chord syndrome
- cada achina syndrome
- conus medullaris syndrome
incomplete (partial)
Degree of spinal cord involvement:
- Results in mixed loss of voluntary motor activity and sensation and leaves some tracts intact
- higher capacity to regain more function
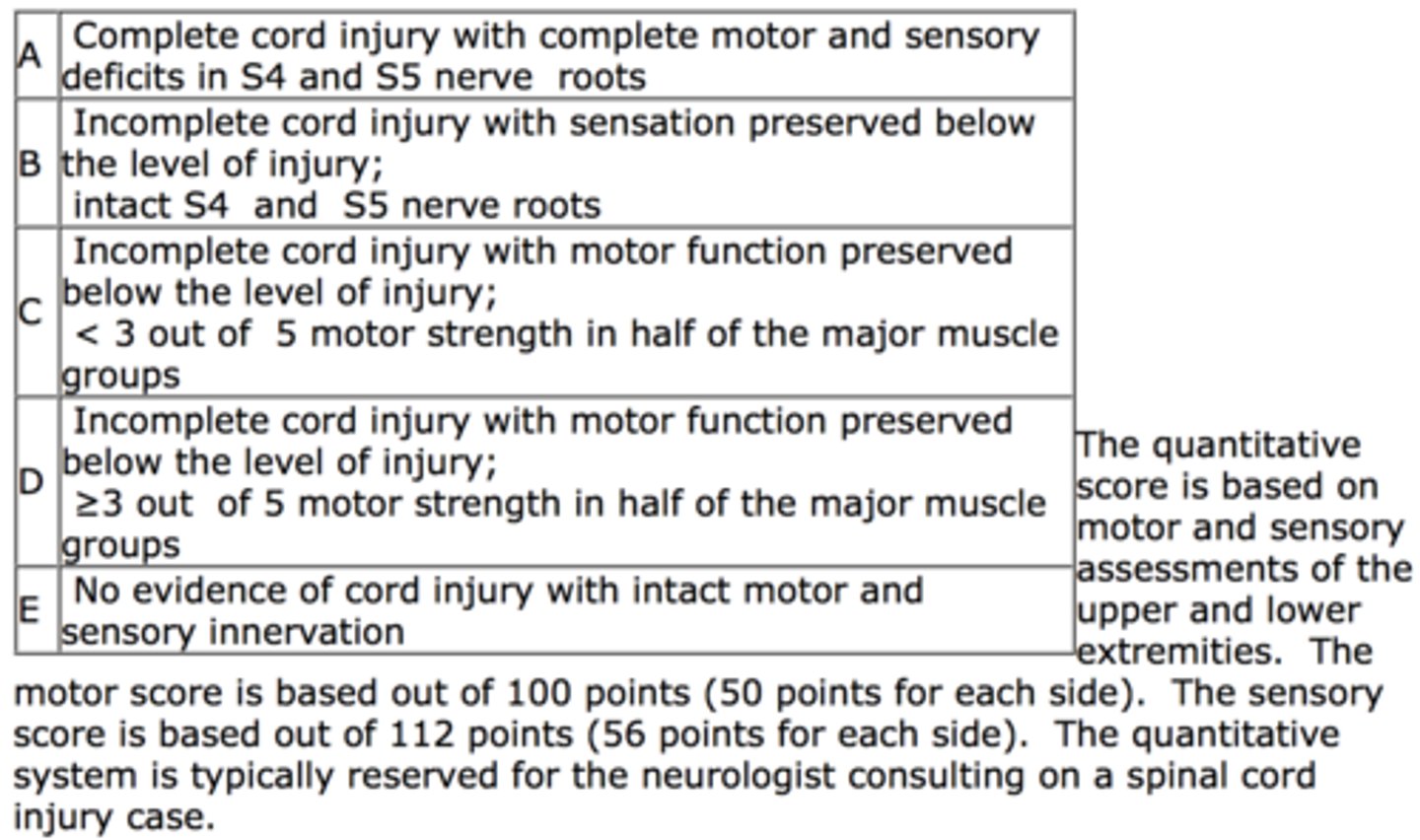
American Spinal Injury Association (ASIA) impairment scale
- used for classifying severity of impairment resulting from spinal cord injury
- very comprehensive; assess motor, sensory function + determine neuro level + completeness of injury
- used to record changes in neuro status + identifying goals for rehab
SCI manifestations
- a direct result of trauma that causes cord compression, ischemia, edema, and possible cord transection
- r/t level and degree of injury
- incomplete lesion = mixture of symptoms
higher
- ________ the injury = more serious the sequelae
- rehab goals r/t specific location of SCI
SCI manifestations
- Systemic: Neurogenic Shock
- Neuro: Paralysis, Sensory/Motor dysfunction, Spinal Shock
- Resp: r/t resp muscle functon, WOB
- CV: r/t SNS innervation, DVT
- Urinary: r/t SNS
- GI: r/t SNS
- Integ: skin breakdown/pressure ulcers
- Metabolic: temp reg, pH changes, increased demand
Neurogenic shock
- SCI above T5
- loss of vasomotor tone --> hemodynamic syndrome (massive vasodilation w/o compensation)
- acute condition --> may become irreversible & lead to death
neurogenic shock sx
- hypotension
- hypothermia
- loss of SNS innervation
w/o compensation
loss of SNS innervation
- peripheral vasodilation
- venous pooling + edema
- pulmonary edema
- decreased cardiac output + hypotension
- acute condition --> may become irreversible & lead to death
neuro
SCI Manifestations:
- paralysis r/t level of injury
- motor + sensory function below level of injury
- spinal shock
spinal shock
- temporary loss or reduction of reflexes below injury level; may mask permanent deficits
- occurs immediately following SCI; 50% of pts; lasts days to months
- hard to identify until sx reverse; return of reflexes complicates rehab
- complication: autonomic dysreflexia
return of reflexes
- Client or family may see this as return of function
- may complicate rehab
- hyperactive, exaggerated responses
- penile erections
- spasms
spasm control
- antispasmodic (ie. baclofen)
- botulin toxin for severe cases
Autonomic Dysreflexia
- serious complication of SCI above T6
- develops when reflexes return in spinal shock
- precipitated by bladder/GI contraction, skin or pain stim
- uncompensated CV rxn by SNS --> can cause seizures, stroke, MI, death
Autonomic Dysreflexia sx
- HTN (>300mgHg)
- Bradycardia (pulse <60 bpm)
- Pounding headache
- Flushing, Diaphoresis, Dilated pupils, Nausea
- Piloerection
- Nasal stuffiness
resp
SCI Manifestations:
- closely correspond to level of injury; may require ventilation
- cervical injury (above/below C4)
- thoracic injuries
- complications
above C4
SCI Manifestations: Resp
- total loss of resp muscle function; paralysis
- Laboured Breathing, Exhaustion, ABGs Deteriorate
- mechanical ventilation required to keep pt alive (ETT, TRACH) (risk of infection)
cervical injury (below C4)
SCI Manifestations: Resp Complications
- spares diaphragmatic breathing if phrenic nerve functioning (C3-C5)
- but edema + hemorrhage r/t secondary injury can affect phrenic nerve = resp insufficiency
thoracic injuries
SCI Manifestations: Resp Complications
- paralysis of abdominal + intercostal muscles --> hypoventilation
- cannot cough --> atelectasis or pneumonia
- Trach + NG enteral feeds (loss of gag reflex)
pulmonary edema
Resp Complications:
- increase in pulmonary interstitial + alveolar fluid
- may occur secondary to neurogenic shock or fluid overload in resus
T6, CV
SCI Manifestations:
- SCI above _____ --> reduces SNS innervation
- monitoring necessary
- bradycardia
- peripheral vasodilation + hypotension
- hypovolemia
bradycardia
- d/t PNS stimulation w/o SNS compensation
- +++ PNS stim = cardiac arrest (ie. suctioning or turning pt)
- Tx: atropine
atropine
- may need to be given to treat bradycardia (low HR) to increase HR + prevent hypoxemia
peripheral vasodilation, hypotension, hypovolemia
SCI Manifestations:
- _________ ________ causes decreased venous return --> decreased cardiac output + increased capacity in veins = _________ + ___________
- IV fluids + vasopressors**
DVT, PE
- _______ = common problem
- _______ = leading cause of death
- more difficult to detect --> does not exhibit usual signs such as pain+ tenderness
- assess: doppler, lower limbs, thigh girth, calf pain on dorsiflexion
GU
SCI Manifestations:
- urinary retention (acute phase) --> reflex emptying
- neurogenic bladder (areflexic, hyper-reflexic, dyssynergic)
urinary retention
SCI Manifestations:
- acute phase of SCI or spinal shock
- loss of bladder tone + reflexes for bladder emptying = _____ ______
- can cause overdistension of bladder = urine reflux into kidney --> eventual renal failure
indwelling cath
- inserted in acute phase of SCI
- remove as early as possible, once stabilized, to maintain bladder tone + decrease risk of infection
- move onto intermittent cath
reflex emptying (involuntary)
SCI Manifestations:
- after acute phase; remove cath
- bladder may become hyper-irritable
- d/t loss of inhibition from brain
neurogenic bladder
- when reflexes return in spinal shock; depending on completeness of SCI
- any type of bladder dysfunction r/t abnormal or absent bladder innervation
- May be areflexic, hyper-reflexic, dyssynergic
- Diagnose + manage dysfunction, promote bladder emptying
areflexive/flaccid bladder
Neurogenic Bladder:
- no reflex detrusor contractions
- bladder cannot empty --> distension + reflux into kidney
hyperreflexive/spastic bladder
Neurogenic Bladder:
- hyperactive reflex detrusor contractions
- bladder muscle (detrusor) contracts involuntarily during filling --> sudden urge to urinate, frequency, urgency, and urge incontinence
dyssynergic bladder
Neurogenic Bladder:
- lack coordination between detrusor contraction and urethral relaxation
- bladder muscle (detrusor) contracts + urethral sphincter muscle constricts instead of relaxing
- blocks urine outflow = high bladder pressure + potential kidney damage via reflux
GI
SCI Manifestations:
- injury above T5
- stress ulcers
- intra-abdominal bleeding
- neurogenic bowel
t5, paralytic ileus, gastric distension
SCI Manifestations:
- above ______ --> r/t decreased GI motility (SNS)
- contributes to ________ _______ + ______ _______
- TX: NG (distension) + metoclopramide
Metoclopramide
- may be used to treat delayed gastric emptying; increases gastric motility
- dopamine-receptor antagonist
stress ulcers
SCI Manifestations:
- d/t increased gastric secretion (SNS stim)
- peak 6-14 days
- high dose corticosteroids = increase risk
- Prevent: H2R blockers or PPIs
intra-abdominal bleeding
SCI Manifestations:
- difficult to diagnose (may not have pain; absence of sensory/motor function)
- *continued hypotension despite treatment
- *drop in Hgb + Hct
neurogenic bowel, t12, spinal shock
SCI Manifestations:
- d/t decreased voluntary control over bowel
- AReflexive/Reflexive bowel
- occurs in injury above _____ or _____ ______
areflexic/flaccid bowel
SCI Manifestations: Neurogenic bowel
- below T12 or in spinal shock
- decreased sphincter tone ---> inability to empty the bowel effectively without manual help
- log roll + MRP does DRE --> assess rectal tone after SCI to determine level of injury
reflexic/spastic bowel
SCI Manifestations: Neurogenic bowel
- d/t return of reflexes in spinal shock
- sphincter tone is enhanced.
- reflex emptying occurs; involuntary bowel movements when rectum is full
pressure ulcer/skin breakdown
SCI Manifestations: Integ
- result of lack of movement + loss of sensory function
- occur quickly as pts cannot sense to move or move independently
- can cause major infection or sepsis
- pt require alternating pressure mattresses
metabolic
SCI Manifestations:
- poikilothermia
- risk of acidosis/alkalosis
- monitor lytes (hypokalemia)
- wt loss & +++ nutritional needs
poikilothermia
SCI Manifestations: metabolic
- body temp adjusts to room temp; does not thermoregulate
- based on level of injury --> sweat or shiver function decreased below injury level
- SNS interruption --> prevents peripheral temp senses from reaching hypothalamus
metabolic alkalosis, lytes
SCI Manifestations:
- NG suctioning may lead to _______ ________ (d/t removal of K+ in secretions)
- monitor ________ until NG d/c + normal diet resumed
acidosis
SCI Manifestations:
- Reduced tissue perfusion may lead to _________ d/t accumulation of H+ ions and lactic metabolites (byproduct of anaerobic metabolism)
wt loss, nutrient, protein
SCI Manifestations:
- _______ _______ common; pt muscle atrophy quickly
- ________ needs greater than expected
- high ________ diet --> prevent skin breakdown + reduce muscle atrophy
DVT, PE
SCI Manifestations:
- common problem
- assess: doppler, lower limbs, thigh girth, calf pain on dorsiflexion
- _______ ________ = leading cause of death
SCI diagnostics
- CT
- MRI
- vertebral angiography
- Comprehensive Neuro Exam
CT
SCI diagnostics:
- may be used to assess stability of injury, location, and degree of bone injury
MRI
SCI diagnostics:
- gold standard for imaging neurological tissues